Tumor small intestine
-
Upload
kansal007 -
Category
Health & Medicine
-
view
144 -
download
0
Transcript of Tumor small intestine

TUMOR SMALL INTESTINE
BY-DR SUMIT KR KANSAL JUNIOR RESIDENT 2ND YEAR DEPARTMENT OF SURGERY
MODERATER : DR UMANG MITHAL

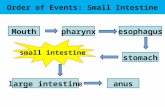
Small Intestine

Anatomy
A. Duodenum: Retro-peritoneal Supplied by the celiac artery & SMA
B. Jejunum: Occupies upper left of the abdomen Thicker wall and wider lumen than the
ileum Mesentery has less fat and forms only 1-2
arcadesC. Ileum:
Occupies the lower right; has more fat and forms more arcades
Contains Payer’s patches Ileum & jejunum is supplied by the SMA

Venous drainage:• Through sup. Mesenteric vein
Lymphatics:• Lymph drainage occur through
lymphatic vessel• Lymhmesenteric LNcisterna
chylithoracic ductLt subclavian vein
Nerve supply:• Parasympathetic- vagus• Sympathetic- splanchnic




Tumors of the small intestineClassification
• Non-neoplastic polyps Hamartomatous polyps (Juvenile & Peutz-Jeghers polyps) Inflammatory polyps Lymphoid polyps
• Neoplastic ( epithelial) polyps Benign polyps (adenoma) Malignant lesions Adenocarcinoma Carcinoid
• Mesenchymal lesions GI stromal tumors (benign & malignant) Others ( lipoma, neuroma, angioma, Kaposi sarcoma)
• Lymphoma Diffuse large cell lymphoma. MALT cell lymphoma.

Epidemology of SI Tumors• Sites of the highest risk are the duodenum, for adenocarcinomas, and the ileum, for
carcinoids and lymphomas. • In industrialized countries, small bowel cancers are predominantly adenocarcinomas; • In developing countries, lymphomas are much more common.• The incidence of small bowel cancer rises with age and has generally been higher
among males than among females. • The risk factors for small bowel cancer include Dietary factor Cigarette smoking, Alcohol intake, Medical conditions -Crohn's disease, familial adenomatous polyposis,
cholecystectomy, peptic ulcer disease, and cystic fibrosis.• The protective factors may include rapid cell turnover, a general absence of bacteria,
an alkaline environment, and low levels of activating enzymes of precarcinogens.

Site– Adenocarcinomas - proximal small bowel.– other malignant lesions - in the distal intestine.– Adenomas - are found in the duodenum, 30% are found in the jejunum, and 50%
are found in the ileum.– Lipomas - are most common in the ileum – Leiomyoma - smooth muscle origin– Hemangiomas - the jejunum is the most commonly affected small bowel
segment. – PeutzJeghers syndrome - The entire jejunum and ileum are the most usual
portions of the gastrointestinal tract involved with these hamartomas.
Carcinoid tumors and lymphomas are more frequent than adenocarcinoma and leiomyo-sarcoma.

SMALL-BOWEL NEOPLASMS• BENIGN– Adenomas are the most common benign neoplasm of the small intestine. – Other benign tumors include fibromas, lipomas, hemangiomas,
lymphangiomas, and neurofibromas.• Majority of small bowel neoplasm are benign• Adenomas, lipomas, hemangiomas, neurogenic tumors • Frequently asymtomatic & identified incidentally• Can present with intersusception, small bowel obstruction, bleeding,
anaemia• Inv: capsule endoscopy & small bowel endoscopy• Symptomatic lesion can be treated by small bowel resection & anastomosis.
05/01/2023

Leiomyomas • Leiomyomas, are the most common symptomatic benign
neoplasms of the small bowel.• As the origin of these tumors has become clearer,
pathologists have shifted from designations such as leiomyoma or leiomyosarcoma to the term stromal tumors (i.e., GISTs). And benign GISTs are three to four times more common than malignant GISTs.
• Currently, these tumors are thought to arise from the interstitial cell of Cajal and made up of spindle (70%) and epithelioid (30%) cells
• >90% GISTs express CD117, the c-kit proto-oncogene protein that is a transmembrane receptor for the stem cell growth factor, and 70% to 80% express CD34, the human progenitor cell antigen.

Leiomyoma

AdenomasThree primary types: True adenomas Villous adenomas Tubulovillous• Mostly asymptomatic some times present with bleeding and
obstruction with most occurring singly and found incidentally.• The malignant potential of these lesions is reportedly between
35% and 55%.• Treatment is determined by location and adenoma type. Jejunum and ileum - segmental resection. duodenal adenomas - duodenal resection by
pancreaticoduodenectomy sporadic adenomas - pancreas-preserving duodenectomy
(endoscopic or open polypectomy can be performed if technically feasible.)

• Typically,characterized by the Spigelman classification Screening endoscopy with a forward- and side-viewing endoscope is performed at regular intervals with biopsy of all
• Frequency of endoscopic screening is 1 to 3 years, depending on the Spigelman classification
PARAMETER 1 2 3
No Of Polyp 1-4 5-20 >20
Size in mm 1-4 5-10 <10
Histology Tubular tubulovillous villous
Degree of dysplasia
mild moderate Severe
Stage 0 - 00 pointsStage 1 - 1-4 points Stage 2 - 5-6 pointsStage 3 - 7-8 pointsStage 4 - 9-12 points.

Diagnosis• . Diagnosis can usually be accomplished by endoscopy
and biopsy, and• symptomatic lesions in an accessible region should be
resected by simple excision. • There is no malignant potential for Brunner gland
adenomas

Lipomas • Also included in the category of stromal tumors.• present as single intramural lesions located in the submucosa.• occur in the sixth and seventh decades of life and are more
frequent in men. • Less than one third of these tumors are symptomatic • manifestations are obstruction and bleeding from superficial
ulcerations. • The treatment of choice for symptomatic lesions is excision.• have no malignant potential, when found incidentally, should
be removed only if simple resection.

LIPOMA

Hemangiomas • Developmental malformations as submucosal proliferation of
blood vessels at any level of the gastrointestinal tract. the jejunum is the most commonly affected small bowel
segment.
• Can 3% to 4% of all benign tumors of the small bowel and are multiple in 60% of patients.
• if inherited disorder known as OslerWeber-Rendu disease.• Can present in the lung, liver, and mucous membranes.• The most common symptom of small bowel hemangiomas is
intestinal bleeding.• Angiography and 99mTc–red blood cell scanning are the most
useful diagnostic studies. • Intraoperative trans illumination and palpation can be helpful• Resection of involved segment to be done.


Peutz-Jeghers Syndrome
• Hamartomas of the small bowel occur as part of the PeutzJeghers syndrome
• 1- to 2-mm, brown or black spots located in the entire jejunum and ileum are the most usual portions of the gastrointestinal tract involved with these hamartomas;
• however, 50% of patients may also have rectal and colonic lesions, and 25% of patients have gastric lesions.
Symptoms• recurrent colicky abdominal pain,
Sign• Intermittent intussusception. • Lower abdominal pain associated with a palpable mass.• Hemorrhage as a result of autoamputation of the polyps

Hamartoma

SMALL-BOWEL NEOPLASMS• MALIGNANT– The small intestine is frequently affected by metastases from or local invasion
by cancers originating at other sites.– Primary small-bowel cancers are rare• Adenocarcinomas: comprise 35–50 percent of all cases• carcinoid tumors comprise 20–40 percent• lymphomas comprise approximately 10–15 percent. • Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal
tumors arising in the small intestine and comprise up to 15 percent of smallbowel malignancies.
05/01/2023 Shwartz

SMALL-BOWEL NEOPLASMS• Clinical Presentation– Most small-intestinal neoplasms are asymptomatic until they become large.– Small-bowel obstruction is the most common mode of presentation. – Hemorrhage is the second most common mode of presentation.– Physical examination may reveal an abdominal mass or signs of intestinal
obstruction. – Fecal occult blood test may be positive. Cachexia or ascites may be present with
advanced disease.– Lesions in the periampullary location can cause obstructive jaundice or
pancreatitis.
05/01/2023 Shwartz

Malignant neoplasm:Histologic types:
Tumor type Cell of origin Frequency Predominant Site
adenocarcinoma Epithelial cell 35 – 50% Duodenum
carcinoid Enterochromaffin cell
20 – 40% Ileum
lymphoma lymphocyte 10 – 15% Ileum
GIST (gastrointestinal stromal tumors)
? Interstitial cell of Cajal
10 – 15% -

• Adenocarcinomas constitute about 50% of the malignant tumors of the small bowel in most reported series.
• The peak incidence is in the seventh decade of life, and most series show a slight male predominance.
• Tumors of the duodenum tend to present somewhat earlier than those occurring in the most distal intestine, with symptoms of jaundice and chronic bleeding.
• Adenocarcinomas of the jejunum and ileum usually produce symptoms that may be more nonspecific and include vague abdominal pain and weight loss.
• Most common CA of small bowel• Most common in duodenum and proximal jejunum half
involve the ampulla of Vater.
Adenocarcinoma

• These are most commonly found in the duodenum, except in patients with Crohn's disease, in whom most are found in the ileum.
• Lesions in the periampullary location can cause obstructive jaundice or pancreatitis.
• Adenocarcinomas located in the duodenum tend to be diagnosed earlier in their progression than those located in the jejunum or ileum, which are rarely diagnosed prior to the onset of locally advanced or metastatic disease.
• Clinical features: anaemia, GI bleeding, intususception, obstruction
• As with adenocarcinomas in other organs, survival of patients with small bowel adenocarcinomas is related to the stage of disease at the time of diagnosis

Pathophysiology• (1) dilution of environmental carcinogens in the liquid chyme present in the small-
intestinal lumen• (2) rapid transit of chyme, limiting the contact time between carcinogens and the
intestinal mucosa. • (3) a relatively low concentration of bacteria in small-intestinal chyme and,
therefore, a relatively low concentration of carcinogenic products of bacterial metabolism.
• (4) mucosal protection by secretory IgA and hydrolases such as benzpyrene hydroxylase that may render carcinogens less active.
• (5) efficient epithelial cellular apoptotic mechanisms that serve to eliminate clones harboring genetic mutations.

Large circumferential adenocarcinoma of the jejunum

– Risk factors• Consumption of red meat• Ingestion of smoked or cured foods• Crohn disease• Celiac sprue• Peutz-Jeghers syndrome. • Familial adenomatous polyposis (FAP)– nearly 100 % cumulative lifetime risk of developing duodenal adenomas
that have the potential to undergo malignant transformation. – The risk of duodenal cancer in these patients is more than 100-fold than in
the general population

TNM Classification• T – Primary Tumour• TX Primary tumour cannot be assessed • T0 No evidence of primary tumour • Tis Carcinoma in situ• T1 Tumour invades lamina propria or submucosa • T2 Tumour invades muscularis propria • T3 Tumour invades through muscularis propria into subserosa or into non-peritonealized perimuscular tissue (mesentery or retroperitoneum3) with extension 2
cm or less• T4 Tumour perforates visceral peritoneum or directly invades other organs or structures (includes other loops of small intestine, mesentery, or retroperitoneum
more than 2 cm and abdominal wall by way of serosa; for duodenum only, invasion of pancreas)
• N – Regional Lymph Nodes • NX Regional lymph nodes cannot be assessed • N0 No regional lymph node metastasis • N1 Regional lymph node metastasis
• M – Distant Metastasis • MX Distant metastasis cannot be assessed • M0 No distant metastasis• M1 Distant metastasis
• Stage Grouping• Stage 0 - Tis N0 M0 • Stage I - T1 N0 M0 T2 N0 M0 • Stage II - T3 N0 M0 T4 N0 M0 • Stage III -Any T N1 M0 • Stage IV -Any T Any N M1

Diagnosis•Due to absence or nonspecific symptoms these lesions are rarely diagnosed preoperatively.
•Laboratory tests are nonspecific EXCEPT I. Elevated serum 5-hydroxyindole acetic acid (5-HIAA) levels
in carcinoid syndrome. II. Elevated carcinoembryonic antigen (CEA) levels in
adenocarcinomas, but only in the presence of liver metastases.
• Contrast radiography of the small intestine may demonstrate benign and malignant lesions

• Enteroclysis -sensitivity of 90% in the detection of small-bowel tumors and is the test of choice, particularly for tumors located in the distal small bowel.
• Upper GI with small-bowel follow-through examinations sensitivities ranging from only 30 to 44%.
• CT scanning has low sensitivity for detecting mucosal or intramural lesions, can demonstrate large tumors and is useful in the staging of intestinal malignancies.
• Angiography or radioisotope-tagged red blood cell (RBC)
scans-Tumors associated with significant bleeding
• Flexible endoscopy in diagnosing duodenal lesions, and colonoscope in the terminal ileum for visualization and biopsy of ileal neoplasms.

Contrast radiograph demonstrating a lesion in the proximal jejunum determined to be an adenocarcinoma of the small intestine at the time of surgery

CT scan demonstrating a small-bowel loop in the left upper quadrant with an irregularly thickened wall and areas of ulceration (arrow). This lesion proved to be a jejunal adenocarcinoma

Lymphoma
1. Primary lymphoma 2. Secondary lymphoma [ Metastatic ]
Primary lymphomas arise with in the lymphoid tissue of GI tract.
• 1- 5 % of all GI malignancies are lymphomas.• Secondary lymphomas are brought to GIT from
lymphomas primarily arising some where else in the body.
• Lymphoma may involve the small intestine primarily or as a manifestation of disseminated systemic disease.

• Primary small-intestinal lymphomas are most commonly located in the ileum, which contains the highest concentration of lymphoid tissue in the intestine
• Lymphomas constitute 7% to 25% of small bowel malignant tumors in the adultin children younger than age 10 years, they are the most common intestinal neoplasm.
• Risk of devloping in patient withceliac disease and immunodeficiency states (e.g., AIDS).
• small intestine lymphomas are usually large, with most larger than 5 cm; they may extend beneath the mucosa
• Microscopically, there is often diffuse infiltration of the intestinal wall.

• Symptoms of small bowel lymphoma include pain, weight loss, nausea, vomiting, and change in bowel habits. Perforation may occur in up to 25% of the patient.
• Primary lymphomas commonly arise in the stomach and small intestine and carry better prognosis.

primary lymphoma of the ileum with tumor.

The treatment of adenocarcinomas and lymphomas of the small bowel is
• wide resection including regional lymph nodes .This may require pancreaticoduodenectomy (Whipple operation) for duodenal lesions.
• surgical resection for cure is not possible. Therefore, palliative resection should be performed to prevent further complications of bleeding, obstruction, and perforation.
•If this is not possible, bypass of the involved segment may provide relief of symptoms
TREATMENT

A, Malignant tumors should be resected with a wide margin of normal bowel and a wedge of mesentery to remove the immediate draining lymph nodes.
B, End-to-end anastomosis of the small bowel and repair of the mesentery

GISTs: (gastrointestinal stromal tumors)
Most common mesenchymal tumors arising in the small bowel70% arises from the stomach followed by the small bowel15% of small bowel malignancies
Formerly classified as: 1. Leiomyomas2. Leiomyosarcomas3. Smooth muscle tumors of the intestine.
• 60% to 70% of GISTs are located in the stomach.• The small intestine is the second most common site,
containing 25 to 35% of GISTs.• There appears to be no regional variation in the prevalence of
GISTs within the small intestine.• GISTs have a greater propensity to be associated with overt
hemorrhage than the other small-intestinal malignancies

•A defining feature of GIST is its expression of the receptor tyrosine kinase KIT (CD117).
•Pathologic KIT signal transduction is believed to be a central event in GIST pathogenesis.
•The majority of GISTs have activating mutations in the c-kit protooncogene, which cause KIT to become constitutively activated, presumably leading to persistence of cellular growth or survival signals.
•Because the interstitial cells of Cajal normally express KIT, these cells have been implicated as the cell of origin for GISTs.

Small bowel leiomyosarcoma (malignant gastrointestinal stromal tumor) with hemorrhagic necrosis

Treatment: Small-intestine GISTs:• Segmental resection • If preoperatively diagnosed, lymphadenectomy should not
be done, for rarely associated LN metastases.• Resistant to conventional chemotherapy• Adjuvant treatment -Imantinib mesylate (Gleevec):
− Formerly known as ST1571− 80% of unresectable lesions showed clinical benefits− 50 – 60% showed evidence of reduction in tumor
volume.

− blocks the unregulated mutant c-kit (CD117) tyrosine kinase. Imatinib mesylate also inhibits the Bcr-Abl and platelet-derived growth factor (PDGF) receptor tyrosine kinases.
− Role as neoadjuvant and adjuvant under evaluation

METASTATIC NEOPLASM• Metastatic tumors involving the small bowel are much more
common than primary neoplasms. • The most common metastases to the small intestine are those
arising from other intra-abdominal organs, including the uterine cervix, ovaries, kidneys, stomach, colon, and pancreas.
• Small intestinal involvement is by either direct extension or implantation of tumor cells. Metastases from extra-abdominal tumors are rare but may be found in patients with adenocarcinoma of the breast and carcinoma of the lung.
• Cutaneous melanoma is the most common extra-abdominal source to involve the small intestine, with involvement of the small intestine noted in more than half of patients dying from malignant melanoma.

Symptoms• Anorexia• weight loss• anemia,• bleeding • partial bowel obstruction. Treatment- is palliative resection to relieve symptoms or,
occasionally, bypass if the metastatic tumor is extensive and not amenable to resection

A, Barium radiograph shows “target lesions” consistent with metastatic melanoma of the small bowel (arrow).
B, Specimen demonstrating metastatic melanoma to the small bowel.

Carcinoid tumor.
Literally, carcinoid means carcinoma like.
•These are named carcinoid because these resemble in biological behavior with carcinoma i.e., they have the ability to metastasis though very slowly but the neoplastic cells forming the tumors, microscopically do not appear typically malignant.
•These tumors arise from the diffuse components of endocrine system that are present in different parts of the body.
•These tumors are now called “well-differentiated neuroendocrine tumors.

•Carcinoids of the small bowel arise from enterochromaffin cells found in the crypts of Lieberkühn also known as argentaffin cells because of their staining by silver compounds
•Carcinoid tumors may be derived from the foregut (respiratory tract, thymus), midgut (jejunum, ileum and right colon, stomach, and proximal duodenum), and hindgut (distal colon and rectum).
•Foregut carcinoids characteristically produce low levels of serotonin (5-hydroxytryptamine) but may secrete 5-hydroxytryptophan or adrenocorticotropic hormone.
•Midgut carcinoids are characterized by having high serotonin production.
.

•Hindgut carcinoids rarely produce serotonin but may produce other hormones, such as somatostatin and peptide YY.
•The malignant potentials are directly related to• Site of origin.• Depth of penetration in the wall of the gut.• Size of the tumor
•The gastrointestinal tract is the most common site for carcinoid tumors.
•Carcinoid tumors may arise from GI tract, tracheobronchial tree, lungs, pancreas, biliary tract and even liver.
•Most of the carcinoid arise from GI tract, and more than 40 % occur in the small intestine. small bowel carcinoids are seen in fifth decade of life

•All carcinoid tumors are potentially malignant.
•After the appendix, the small intestine is the second most frequently affected site in the gastrointestinal tract.
•In the small intestine, carcinoids almost always occur within the last 2 feet of the ileum.
•Carcinoid tumors have a variable malignant potential and are composed of multipotential cells with the ability to secrete numerous humoral agents the most prominent of which are serotonin and substance P.
•In the gastrointestinal tract, more than 90% of carcinoids are found in three sites: the appendix (45%), the ileum (28%), and the rectum (16%)
.

Carcinoid syndrome. 25-50% carcinoid tumor develops carcinoid syndrome.
1. Diarrhea2. Flushing3. Hypotension4. tachycardia 5. fibrosis of endocardium and valves of the right
heart.• GI carcinoid produce carcinoid syndrome only when these
metastasize to liver but it is not necessary for extra intestinal carcinoid

SITE CASESAVERAGE METASTASIS (%)
CASES OF CARCINOID SYNDROME
Esophagus 1 0Stomach 93 (2%) 23 8Duodenum 135 (4%) 20 4Jejunoileum 1032 (28%) 34 91Meckel's diverticulum 42 (1%) 19 3
Appendix 1686 (45%) 2 6Colon 91 (2%) 60 5Rectum 592 (16%) 18 1Ovary 34 6 17Biliary tract 10 30 0Pancreas 2 1Total 3718 136
Distribution of Gastrointestinal Carcinoids: Incidence of Metastases and of Carcinoid Syndrome

Diagnosis
• Carcinoid tumors of the small intestine are rarely diagnosed preoperatively.
• Barium radiographic studies of the small bowel may exhibit multiple filling defects as a result of kinking and fibrosis of the bowel.
• Angiography and high-resolution ultrasonography can provide information on mesenteric involvement as well as hepatic involvement.
• Carcinoid tumors produce serotonin which metabolized in the liver and the lung to the pharmacologically inactive 5-hydroxyindoleacetic acid (5-HIAA). Elevated urinary levels of 5-HIAA measured over 24 hours with high-performance liquid chromatography are highly specific

• CT is useful in detecting hepatic and lymph node metastases and the extent of bowel wall and mesenteric involvement.
•Advantage of the fact that many of these tumors possess somatostatin receptors is somatostatin receptor scintigraphy using 111In-labeled pentetreotide
• The plasma concentration of chromogranin A, a protein made in the secretory granules, which is elevated in more than 80% of patients with carcinoid tumors is the test of choice , the lack of specificity limits its usefulness as a sole marker.
• Still the combination of 24-hour urine 5-HIAA and serum chromogranin A levels provides the best biochemical diagnostic accuracy.
•Positron emission tomography (PET) scan A PET scan is another imaging test that uses low levels of radioactivity to look for tumors.

• Capsule endoscopy Test doesn’t really use an endoscope.The patient swallows a capsule (about the size of a large vitamin pill) that contains a light source and a tiny camera. Like any other pill, the capsule goes through the stomach and into the small intestine. As it travels (usually over about 8 hours), it takes thousands of pictures. These images are transmitted electronically to a device worn around the person’s waist, while he or she goes on with normal daily activities. The pictures can then be downloaded onto a computer, where the doctor can watch them as a video. The capsule passes out of the body during a normal bowel movement and is discarded.
• Double balloon enteroscopy A special endoscope that is made up of 2 tubes, one inside the other. First the inner tube, which is an endoscope, goes forward about a foot, and then a balloon at its end is inflated to anchor it. Then the outer tube goes forward to near the end of the inner tube and it is then anchored in place with a balloon. This process is repeated over and over, letting the doctor see the intestine a foot at a time. This procedure done under general anesthesia . The main advantage of this test over capsule endoscopy is that the doctor can take a biopsy if something abnormal is seen.

Barium radiograph of a carcinoid tumor of the terminal ileum demonstrates fibrosis with multiple filling defects and high-grade partial obstruction (arrows).

A-Carcinoid tumor of the distal ileum demonstrates the intense desmoplastic reaction and fibrosis of the bowel wall.
B -Mesenteric metastases from a carcinoid tumor of the small bowel.

T1 Lam propria/ submucosa and < 1 cm T2 Muscularis propria or > 1 cm T3 Jejunal, ileal: subserosa. Ampullary, duodenal: pancreas or retroperitoneum` T4 Perforates serosa; adjacent structures
Stage I - T1 N0 Stage IIA - T2 N0 IIB - T3 N0Stage IIIA - T4 N0 IIIB - Any T N1 Stage IV -Any T Any N M1
TNM FOR CARCINOID TUMOR OF SMALL INTESTINE

TREATMENTThe treatment of carcinoid tumors requires a multidisciplinary approach, and combined modalities may be the best option
Surgical debulking, Hepatic artery embolization or chemoembolization, Medical therapy
•The treatment of patients with small bowel carcinoid tumors is based on tumor size and site and presence or absence of metastatic disease
•Primary tumors of less than 1 cm in diameter without evidence of regional lymph node metastasis, a segmental intestinal resection is adequate.

•Patients with lesions larger than 1 cm, with multiple tumors or with regional lymph node metastasis, regardless of the size of the primary tumor, wide excision of bowel and mesentery is required.
•Lesions of the terminal ileum are best treated by right hemicolectomy. •Small duodenal tumors can be excised locally.•Extensive lesions may require pancreaticoduodenectomy.• In addition to treatment of the primary tumor, it is important that the abdomen be thoroughly explored for multicentric lesion.

Chemotherapy: The role of chemotherapy is confined predominantly to patients with metastatic disease who are symptomatic and unresponsive to other therapies
30 -50% response»Cyclophosphamide»5-fluorouracil»Streptozocin
Octreotide: - analogues of somatostatin most effective for management of symptoms of carcinoid syndrome.
Interferon-α (IFN-α)- decreases in urinary 5-HIAA levels in 42% of patients and tumor regression in 15%.
Serotonin receptor antagonists have been used with limited success- Ketanserin and cyproheptadine.
Result in some tumor regression in up to one third of the patients. The duration of response, however, is short lived

Prognosis
• Carcinoid tumors have the best prognosis of all small bowel tumors,
– Resection of a carcinoid tumor localized - 100% survival rate.
– Five-year survival rates are about 65% among patients with regional disease and
– 25% to 35% among those with distant metastasis– Elevated level of chromogranin A, which was found to be
an independent predictor of an adverse prognosis.