Small Intestine - MicrobeWiki.pdf
-
Upload
mahmoud-abdel-rahman -
Category
Documents
-
view
257 -
download
2
Transcript of Small Intestine - MicrobeWiki.pdf
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 1/13
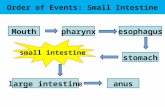
The Small Intestine (in order from stomach to the large intestine):
Duodenum, Jejunum, and Ileum.[1
Small Intestine
From MicrobeWiki, the student-edited microbiology resource
This is a curated page. Report corrections to Microbewiki (mailto:[email protected]) .
This article is concerned with the microbes residing in one particular niche: the small intestine of the digestive tract.Although most of the human flora (the term used for the bacteria living in the human body) is found in the colon, thereare a good number of microbes found in the small intestine. The following article will discuss the different bacteria thatcontribute to normal functioning and diseased states of the small intestine, with a focus on that of humans.
Contents
1 Introduction
2 Description of the niche2.1 Duodenum
2.2 Jejunum2.3 Ileum
2.4 Protection against bacteria
3 Adjacent communities3.1 Stomach
3.2 Large Intestine
3.3 Conditions under whichthe environment changes
4 Resident microbes
4.1 Which microbes arepresent?4.2 Functions of flora[2]
4.2.1 Protective
4.2.2 Structural4.2.3 Metabolic
5 Microbial Adventures: Vol. 16 Microbial diseases of the smallintestine
6.1 Peptic Ulcers fromHelicobacter Pylori[31]]6.2 Tropical Sprue
6.3 Small Intestine BacterialOvergrowth6.4 Other Diseases
7 Current Research and Discoveries8 Conclusion9 References
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 2/13
The lymphoid appearance of the Peyer's patch under
electron microscope [15
Introduction
The human body is not only made up of human cells, but is also comprised of bacterial cells. In fact, microorganisms, ormicrobes, are so abundant that there are about ten times as many bacteria as there are human cells; while there are 100trillion human cells, there are 1000 trillion bacteria cells [12]. It is estimated that there are 500 to 100,000 species ofbacteria living in the human body [12]. These microbes reside on the skin and mucus surfaces of human tissue, but notwithin tissues[10].
Some of the bacteria in the body can be beneficial by helping the host obtain and breakdown nutrients, while others canbe infectious, causing harm to the host. The microbes living in the host are known as normal bacteria and have beendubbed microbiota [11]. However, there are several that indeed benefit the human (a relationship of mutualism), whilethere are some bacteria that are harmful to the host (a parasitic relationship). Parasitic bacteria can cause many differenttypes of disease, and are thus also considered pathogenic bacteria. As this article is looking at the small intestine,different microbial diseases of the small intestine will be reviewed. It is interesting to note that the growth of pathogenicbacteria can be controlled via means of competitive exclusion provided by the presence of useful bacteria provides[13]; this demonstrates the importance of studying the interaction between different microorganisms in a niche, whichwill be covered later in this article.
Description of the niche
The small intestine is the site where most of the nutrient absorption occurs such as minerals, sugars, and amino acids.After food has been broken down in the stomach by strong hydrochloric acid, the pyloric sphincter opens and food getpushed into small intestine by peristalsis. There are three major structural parts of the small intestine, duodenum,jejunum, and ileum. Throughout these sections, finger-liked structure called villi increase surface area that helps theabsorption of nutrients. The concentration of bacterial activity in the small intestine is around 1 million per milliliter [28].The microbial processes it undergoes is limited proteolysis and saccharolysis, toxin and SCFA production[25].
Duodenum
The duodenum is a hollowed tube that is situated betweenthe stomach and the jejunum. The duodenum is the shortestsection of the small intestine; it is 26cm long, on average. Itis mostly responsible for digesting chyme, the food bolusthat was created by the churning motion of the stomach.Since it doesnt have the thick mucus lining like thestomach, the duodenum cannot tolerate the low pHintroduced by the chyme. In order to neutralize the pH, theliver secretes bile and pancreas secretes bicarbonate intothe duodenum and brings the pH of duodenum up toaround 5 and 6 range, a much more tolerable pH forprotein and enzymes to function. Enzymes such as lipase,trypsin and chymotrypsin are also secreted into theduodenum to aid digestion. The bacterial density in this
section of the small intestine reaches 101 to 103 CFU(Colony Forming Units) /mL and flourishes with gram-positive cocci and rods[2].
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 3/13
Image of the Paneth cell under the
1BAS 2 Image Analyzer.[20
Jejunum
The jejunum is 2.5m long, and is the site of absorption. The pH is 7-8 (slightly alkaline). The jejunum is situated rightafter the duodenum and it is about 10 feet long with pH between 7 and 8 [21]. Goblet cells are most numerous injejunum, although they exist throughout small intestine. The primary functions of these cells are to secrete mucus. Mucusprovides protection against pH, stress, and microorganisms by trapping them [22]. As a result of this, the bacterial
density rise to 104-107 CFU/mL and obtains various microbes such as Enterococcus faecalis, lactobacilli, diphtheroids,and the yeast Candida albicans.[25]
Ileum
The ileum is the last section of the small intestine. Like the jejunum, it is also around 10 feet long and its pH lies between
7 and 8. The bacterial density here is also 104-107 CFU/mL and has a microbe community similar to that of the colon.The Ileum is responsible for most of the food and liquid absorption, and the unabsorbed matter and waste products arepassed into the large intestine.[21]] One unique feature of the ileum is the dominance of Peyers patch, a form oflymphoid tissue. The main function of these Peyers patches is to provide leukocytes, part of the immune system, tofight against foreign microorganisms [1] (http://www.siumed.edu/~dking2/erg/giguide.htm) .
Protection against bacteria
Functionally similar to neutrophils, the most abundant form of white blood cellin human, paneth cells on the crypt in the lumen of the small intestine providehost defense against harmful bacteria by primarily secreting antibacterialmolecules defensins, or alpha-defensins when exposed to both Gram positiveand negative bacteria. Defensins kills the bacteria cells by disrupting theirmembrane function. Defensins peptides contain hydrophobic and positively-charged regions that can interact with bacterias negatively phospholipidsmembrane by forming pores. This leads to the weakening of the membraneand causing lysis of the bacterial cell. Since most bacteria have higherconcentration of negatively charged membrane than normal vertebrae cellmembrane, they interact well with defensins positively charged regions andsparing the normal vertebrae cells that are needed for normal metabolicfunctions. Paneth cells also secrete lysozyme and phospholipase A2, which both have antimicrobial functions as well.With the addition of these two agents, paneth cells not only have the ability to kill bacteria, but even fungi and someenveloped viruses as well [14].
Adjacent communities
Stomach
The stomach is located directly above the small intestine, and it is separated from the duodenum by the pyloricsphincter. As mentioned above, the duodenum has a neutral pH, which is needed because inside the stomach, gastricjuice is secreted in order to provide the acidic environment needed to convert the inactive pepsinogen to the activepepsin. As the chyme (the semi-digested foodstuff) enters the duodenum, bile is secreted by the liver through the bileduct, to neutralize the acidic pH from the stomach.
Large Intestine
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 4/13
Fluorescent image of gut bacteria .[28
The colon is connected to the other end of the small intestine, at the ileum. It contains an incredibly large number of
bacteria, at a concentration of 1011-1012 CFU/mL; the highest concentration found in any ecosystem. The coloncontains 400 different types of species which is mostly anaerobic, gram-positive and gram-negative cells. The largeintestine absorbs water, minerals, and organic acids. The microbial processes it undergoes is proteolysis, saccharolysis,toxin and SCFA production [2].
Conditions under which the environment changes
The physical conditions of the small intestine can change if there is diarrhea, ulcers, or infections. For example, one mayhave to take medications like antacid due to conditions such as heart burn or acid reflux into the esophagus. However,one side effect of taking such medication is the decrease of acidity of stomach acid due to neutralization of hydrochloricacid with carbonate from antacid. The result of this is that stomach cannot effectively kill the bacteria that enters thebody, which increase the vulnerability of the gastrointestinal tract to bacterial infection [30]. These will be detailed in thediseases section below.
Resident microbes
Which microbes are present?
The intestinal tract of human body has tentimes as many microbial organisms than therest of the body cells in the body [9]. Thereare up to 100,000 primarily aerobicorganisms per milliliter found in the smallintestine, and there are at least 500bacterial species present inside the intestinaltract [9]. The bacterial environment of thejejunum, the middle section of the smallintestine located after the duodenum,consists mainly of gram-positiveStreptococci and Lactobacilli [6]. Researchdone on several healthy volunteers showedthe presence of Streptococci, Lactobacilli,Staphylococci, and fungi in the intestinaltract [6]. In the ileocaecal valve,Bacteroides and coliform bacteria are thedominant bacteria present there, in additionto anaerobic Lactobacilli [6]. In the ileum, the last section of the small intestine, the bacterial presence is varied, due tothe backwash contamination of the colon [6].
Functions of flora[2]
Protective
The natural flora of the small intestine protect the host by taking up space inside the small intestine. Their presence inthe small intestine prevents pathogens from obtaining a foothold in the niche.
Normal bacteria stimulate the growth of the intestinal lining and the immune system of the intestine.
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 5/13
Lactobacillus bacteria.[23
The natural flora of the small intestine provides competition for nutrients againstpathogens, making it more difficult for pathogens to grow.
The natural flora of the small intestine produces anti-bacterial products to eliminatecompetition such as pathogens.
Structural
The natural flora in the small intestine makes up part of the intestinal barrier.
The natural flora of the small intestine is critical in the natural development of theimmune system.
Metabolic
The natural flora of the small intestine protect the host by metabolizing carcinogens in dietary foods.
The natural flora of the small intestine provide the host with synthesized vitamins, such as biotin and folate.
Help produce vitamin K, which is absorbed and used by the host.
The bacteria are important even for the muscular activity of the small intestine. Without bacteria, there is reducedmuscular activity.
Microbial Adventures: Vol. 1
It was a dark and churning night in the stomach of Bob. Lactobacillus lounged around in the folds of the stomach,waiting for the churning to stop. It had been churning for hours with no end in sight. Then, as suddenly as the churningstarted, it stopped. LB, as he was known among his fellows, stepped out from the folds and surveyed the environment.The harsh acid environment was held back by only his spore coatings. No, he decided. This was not the place togerminate, I wouldn't last long in this environment. He decided to stay inside his spore, ready to spring forth when themoment was right.
Before he could return to the safety of the fold he had been hiding under, the stomach began to undergo peristalsis, theundulating motion of the stomach rippled across the landscape throwing LB to and fro. He was thrown across thePyloric Sphincter. There he blacked out.
LB suddenly awoke to the rushing river of bile released by the gall bladder. If LB had a mouth, he would have beenspitting out the bile, luckily he did not have a mouth. The bile crashed into the partially digested fat around him, causingthe fat to emulsify! Around him a pool of bicarbonate began to form, causing the acids from the stomach to beneutralized. I must be in the duodenum, LB rationalized. This place is much more habitable than the stomach, but its abit too volatile for me!
LB floated along with the gentle flow of food and other spores, some of the spores eventually decided they liked thisenvironment and decided to stay. It wasn't his place to make judgements on other microbe's choices, so he wishedthem well and moved along.
It wasn't long before LB arrived to find himself at a bustling city! It was the largest collection of microbes LB had everseen. The city had looked like it had started at a center point and had expanded outward, a colony had once settledhere and had eventually grew into the wonder LB saw before him. Nearby LB heard one microbe say to another "Ah,
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 6/13
Helicobactor pylori under the
transmission electron microgram. .[26
the Jejunum. You will never find a more wretched hive of scum and villainy." The words of this other microbe were veryconvincing, and LB decided against germinating in this town. He had overheard rumors of a place even larger and moredensely packed than even the jejunum, they were whispers of the colon. LB wished to see the sight whose verydescription was uttered with secrecy and reverence.
LB stayed packed in his spore and continued to move along, hopeful to see the colon. He traveled a long while andeventually landed in the ileum. The ileum was not the metropolis he had heard about. In fact, it was nearly the same sizeas the jejunum. The conditions here were more pleasant than the duodenum and the jejunum. Doubt gripped LB, he feltthe legendary metropolis slip away. LB had given up hope, LB decided that the ileum would be the place to stay togerminate, replicate, and produce lactic acid. The food was plentiful and the neighborhood was friendly.
Little did he know that the metropolis he was looking for was the colon, and it was just a bit further down the tract.Fortunately for LB, this place made him happier than he would ever be if he had indeed traveled to the colon to livethere. For if he had traveled to the colon, he would not have wanted to live there, it is an incredibly crowded place,more so than LB's wildest dreams.
Microbial diseases of the small intestine
Pathogenic bacteria in the small intestine are the cause of a variety of diseases. Specific species of bacteria areresponsible, but the balance of bacterial numbers is also important. The human host thus has enzymes specialized inregulating the numbers should they get too high or low, but the small intestine is still at risk for disease.
Peptic Ulcers from Helicobacter Pylori[31]]
Peptic ulcers are sores in the lining of the stomach or the duodenum of thesmall intestine. They have two different causes: infection by the bacteriaHelicobacter pylori (H. pylori), or long-term use of NSAIDs (nonsteroidalanti-inflammatory agents) such as aspirin. Contrary to popular belief,stress and spicy food do not cause peptic ulcers; instead, they merelyexacerbate the severity of preexisting ulcers. Once an ulcer develops,abdominal discomfort is the most common symptom, and is sometimesaccompanied by nausea, weight loss or poor appetite.
The bacteria H. pylori is a spiral-shaped, gram-negative microaerophileproteobacterium that inhabits the stomach and duodenum. Once a personcontracts H. pylori, it attacks the stomach and duodenum by targeting theprotective mucus coating. Since mucus usually protects the stomach fromthe acid, acid can now reach the underlying sensitive lining and break itdown. H. pylori is specially adapted to the acidic environment of thestomach due to the secretion of protective neutralizing enzymes, specifically urease, and its spiral shape allows forburrowing and embedding into the intestinal lining. Contrary to popular belief, peptic ulcers are actually predominant inthe duodenum rather than the stomach. Since the duodenum has a neutral pH environment, H. pylori is not limited toacidic environments; it has merely adapted to survive in the stomach, and instead changes its living conditions byregulating urease [32].
Surprisingly, H. pylori infection usually does not lead to ulcers; while 20 percent of people under 40 years old areinfected, only 10 percent of people actually suffer from peptic ulcers at some point in their lives. It is believed that thebacterium is transferred through food or water, but the exact method of spreading is still unknown; as a result,prevention is very difficult, and researchers are currently working on developing a vaccine [29].
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 7/13
Ulcer .[29
The diagnosis of H. pylori-induced ulcers begins with first identifying a stomach ulcer by performing an endoscopy or anupper gastrointestinal series (an X-ray taken after the patient drinks barium to highlight the organs on the film). Next, H.pylori will be diagnosed through a variety of tests: blood, breath, stool and tissue sample. For the blood test, they detectthe presence of antibodies to the bacteria. For the breath test, a urea solution containing a special carbon atom isingested, and if the bacteria is present, the urea breaks down to release the carbon, which is measured. A test on thefecal matter can also be performed, which is also known as the Helicobacter pylori antigen test (HpSA). Finally, thetissue test is saved until the very end because it is the most invasive; a biopsy sample is removed with the endoscope,and either the urease test, a histology test, or a culture test is taken.
Treatment of H. pylori peptic ulcers can take the form of drugs that either target theulcers or target the bacteria. Those that strictly treat the ulcers both suppress acidsecretion and protect the stomach lining, such as histamine receptor-2 (H2)blockers and proton pump inhibitors. Antibiotics are taken to kill the H. pylori. It isnot wise to use only one type of medication; to date, it is recommended to undergoa 2-week course of triple therapy, which involves taking two antibiotics to kill theH. pylori, an acid suppressor or a stomach-lining protector. This method has beenproven to be effective for over 90 percent of patients suffering from this ailment.The only downside to this treatment is that many pills have to be taken at once.There are also variations to triple therapy: dual therapy (antibiotic, acid suppressor)and quadruple therapy (two antibiotics, an acid suppressor, and a stomach-liningprotector).
Tropical Sprue
One of the infectious disorders of the small intestine is tropical sprue. Although there is no precise definition of thisdisorder as of yet, some scientists define it as malabsorption of two or more test substances of people living in thetropics" [6]. Symptoms of tropical sprue usually include macrocytic anemia, or abnormally enlarged erythrocytes, dueto a malabsorption of folate and vitamin B12 [7]. In early stages of this disease, the ileum and jejunum specifically areaffected due to the malabsorption of xylose, glucose, fat, vitamin B12, and folate. After a duration of four months, themucosa in the small intestine shows partial villous atrophy. Since the villi are the main components of the small intestinethat is used for the absorption of nutrients, the absorptive qualities of the small intestine are limited in a patient withtropical sprue, leading to malabsorption of essential nutrients. Though there is no specific known cause of tropicalsprue, there is little doubt that it is caused by a severe, acute gastrointestinal infection. No specific microorganism hasbeen identified as the sole cause of tropical sprue, however. Patients with tropical sprue often have a colonization ofcoliform bacteria in the small intestine. Studies have shown that patients with tropical sprue in areas such as North India,Puerto Rico, Haiti, and in Europeans travelling in India contain coliform bacteria in the jejunum. The bacteria in theintestines of the European travelers included Alcaligenes faecaelis, Enterobacter aerogenes, and the hafnia species [6].Other patients were infested with Klebsiella pneumonia, Escherichia coli, and Enterobacter cloacae. In one study inVellore, India, coliform bacteria were present in 29 of 33 patients with tropical sprue [6]. Additional studies in animalshave shown that colonization of Enterobacteria in the small intestine causes changes in mucosal structure of the villi.Several experiments have been conducted on rabbit jejunum. Coliform bacteria are usually aerobes or facultativeanaerobes, and they contain toxins that increase fluid secretion in the intestines. Another experiment conducted onrabbit jejunum has shown that Klebsiella pneumonia, when entered into the jejunum, decreases xylose absorption whileshortening and blunting the villi, inhibiting absorption [6]. Similar results have been shown with a different strain ofbacteria, Enterobacter cloacae, is also entered into the jejunum [6].
The standard treatment of tropical sprue is a dosage of tetracycline and folic acid for at least six months [6]. Thistreatment fixes the mucosal structure of the villi of the small intestine, resolving malabsorption , resulting in patientshaving increased appetite and weight gain. If there is evidence of vitamin B12 malabsorption in the body during tropicalsprue, a vitamin B12 replacement is added as a remedy. Though full recovery is expected, people who stay in the
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 8/13
tropical areas where this disease is endemic, have a good chance of falling into a relapse [6]. If this disease is untreated,death eventually occurs, with the victim dying extremely malnourished. However, tropical sprue can be fatal inextremely young or old victims, even with treatment.
Tropical sprue is mostly prevalent in tropical areas, however, not all of these areas have cases of tropical sprue. Thismay be due to dietary differences of the inhabitants in these regions. There has been a study linking the amount of long-chain unsaturated fatty acids consumed to the occurrence of tropical sprue in the population [6].
Small Intestine Bacterial Overgrowth
Small intestine bacterial overgrowth (SIBO), also known as small bowel bacterial overgrowth (SBBO), is a conditionof the small intestine, defined as an increase in the number of bacteria in the upper gastrointestinal tract [9]. It can becaused by any condition that interferes with the muscular activity in the small intestine that can allow bacteria to multiply[8]. SIBO can result in villous atrophy and mucosal inflammation, altering the absorptive functions of the small intestine[9]. The main cause of SIBO is thought to be mainly bacterial. The production of enterotoxins by facultative anaerobesinjures the intestinal surface while aerobic bacteria produce enzymes and metabolic products that cause epithelial injury.Symptoms of SIBO result mainly from malabsorption, and these symptoms include combinations of cramping, diarrhea,dyspepsia, and weight loss. In addition, anemia can result from malabsorption caused by occult blood loss, vitamin B12deficiency, or both [9].
The diagnosis of SIBO usually starts with a clinical exam. The presence of 105 or more colony units of non-pharyngealbacteria, usually coliforms, suggest SIBO [9]. Screening tests, which include urine ladicans, serum D-lactic acid, andthe glucose breath hydrogen test, are also used. The most common of these, the glucose breath hydrogen test, works asan increase in the hydrogen production in the breath after glucose consumption usually means that there is a significantsmall intestine bacterial fermentation of carbohydrates [9].
Treatment is usually given when the symptoms become too severe, and they usually depend on the species of bacteriainvolved and the severity of the symptoms. Most treatments include the use of oral antibiotics, which reduce the numberof bacteria in the intestinal tract. Surgery may be needed for anatomical anomalies such as diverticula, which arepouches in the colon that provide bacteria with a safe area in which to multiply. The most popular antibiotic used ismetronidazole [9]. Trimethoprim-sulfamethoxazole, aminoglycosides, spectrum penicillins, and cephlasporins are usuallyused against facultative anaerobes [9]. If a patient has increased symptomatic activity, increased dosage may beadministered. Sulfasalazine or corticosteroids may be used if there is an increased inflammatory response, however,dosage is based only on bacterial response [9].
A new and upcoming treatment used to combat SIBO is the use of bacterial substitution, which utilizes probioticbacteria to replace existing bacteria, since the probiotic bacteria can eliminate pathogenic bacterial infections [9]. Theseprobiotic bacteria have a beneficial effect on the small intestine. The probiotic bacteria commonly used are able tocontrol the growth of pathogenic bacteria such as Salmonella typhimurium, Shigella sp, Clostridium difficile,Ampylobacter jejuni, and Escherichia coli, and in addition, are able to offer protection against Gardnerella vaginalitis,Bacteroides bivius, Candida albicans, and Chlamydia trachomatis. Lactic acid bacteria such as Lactobacillus GG andActobacillus plantarum 299V are able to inhibit many gram-negative bacteria by removing toxic substances in the smallintestine and stimulating the immune system [9].
Other Diseases
Crohn's Disease[2] (http://www.asm.org/microbe/index.asp?bid=59965)
Salmonellosis[3] (http://www.ncbi.nlm.nih.gov/pubmed/18589722?ordinalpos=15&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum)
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 9/13
Streptococcus gordonii observed under
Transmission electron micrograph .[27
Irritable Bowel Syndrome[4] (http://www.ncbi.nlm.nih.gov/pubmed/18700692?ordinalpos=1&itool=EntrezSystem2.PEntrez.Pubmed.Pubmed_ResultsPanel.Pubmed_RVDocSum)
Current Research and Discoveries
1. Proliferation and Apoptosis of the Enterocyte is influenced by Bacteria
Prior studies have shown that the small intestines have undergone morphological changes, such as the crypt depth andvillous height, after inoculating germ-free pigs with different types of bacteria. Two gnotobiotic experiments wereperformed where 16 piglets were allocated into 4 types of treatment groups: Germ-Free, monoassociation withLactobacillus fermentum, Escherichia coli, or sow feces. The piglets were reared for 14 days of age where the intestinaltissue and enterocytes were collected each day for histology, gene expression, and protein analysis. Quantitative PCRwas used to measure proliferating nuclear cell antigen and it was concluded that the Escherichia coli and not theLactobacillus fermentum helped stimulate an increase apoptosis and cell proliferation. Thus, only by the death of thereceptors and commensal bacteria were the enterocyte able to have a significant turnover[3].
2. Commensal Bacteria increase invasion of intestinal epithelium
Researchers from Harvard Medical School have discovered that the bacteria in the small intestine may help promotethe invasion of typhoid. The beneficial bacteria located in the small intestine produce a compound that assist inredistributing the protein on the cells surface, which resides on the lining of intestine. This triggers epithelial celltrafficking of a protein, therefore serving as a receptor for the pathogenic bacteria. As a result, the cells become moresusceptible to infection of Salmonella enterica serovar Typhi[4].
3. Diversity of Intestinal Bacterial in Maturing Chicken
Bacterial flora in the ilea and ceca of chickens are analyzed bystudying 1,230 partial 16S rRNA gene sequences. BacterialDNA was isolated using density gradient centrifugation. Studiesshow that the microbes that live in the ileum consist of: 68.5%Lactobacillus, 11% Clostridiaceae, 6.5% Streptococcus, and6.5% Enterococcus. The large amount and variety of bacteria inthe intestine make it difficult to distinguish the function of eachone; however, overall that intestinal bacterial affect: nutrition,immune responses, pathogenesis of intestinal disease, anddegradation of mucus. The bacterial community in birds isaffected by diet, age, and antibiotics. Overall, results showedthat as the bacterial community started out as a stablecommunity in the ileum and cecum. However, as the chickensmatured, the bacterial community becomes more complex andincreasingly differs between the ileum and cecum, which showsthat each region develops its own unique set of microbes[16].
4. Regulation of Intestinal Angiogenesis by Microbes via Paneth Cells
Using three-dimensional imaging, researchers at the Washington University School of Medicine studied the impact ofintestinal angiogenesis on the microbes in the small intestine of mice. Angiogenesis, the growth of new blood vessels,takes place in the complex network of blood vessels in small intestinal villi. However, the villi is also the site where gutmicroorganisms, or microbiota, live. This experiment studies the differences between the villi in germ-free mice and micewith Bacteroides thetaiotaomicron colonies during or after postnatal gut development approximately a ten day period.
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 10/13
Studies have shown that Bacteroides thetaiotaomicron is of the major microbes that reside in both mouse and humangut. This experiment focuses on Paneth cells, which defend the host against microbes by secreting antibacterial peptidesthat affect the microbes in the lumen, or interior of the blood vessels. The results show that microbes function inbreaking down carbohydrate polymers by facilitating lumen breakdown of dietary macromolecules so that the host doesnot have to cleave the various linkages in their food themselves. Symbiosis is observed since the host is able to gainmore nutrients, while microbes are provided a safe niche with a plentiful carbon source[17].
5. Microbial Symbiosis prevents Intestinal Inflammatory Disease
Symbiosis between microbes and their human host can be observed by microbes preventing intestinal inflammatorydisease. One of the main microbes this experiment focuses on is Bacteroides fragilis, which protects its human hostagainst colitis, a chronic inflammation of the membrane lining the gastrointestinal tract, caused by Helicobacterhepaticus, a commensal bacterium. Although colitis is mainly affects the large intestine, in some rare cases it affects theileum as well since it precedes the large intestine. In order for Bacteroides fragilis to be beneficial to its host, it mustexpress polysaccharide A, or PSA, which affects the interleukin-10-producing CD4 T cells; otherwise Helicobacterhepaticus will continue to grow and cause inflammatory disease. It is shown that purified PSA can prevent gutpathology. This experiment gives purified PSA to mice and measures the changes of the inflammatory disease. Micewithout Helicobacter hepaticus had a very mild colitis, while mice with Helicobacter hepaticus developed severe colitis.When purified PSA was given to the diseased mice, they were almost completely protected against the Helicobacterhepaticus, and the disease level was reduced to match those who did not develop colitis. Thus, Bacteroides fragilis isjust one example of a symbiosis relationship where a single bacterial organism promotes human health; and suggests thatthere are others yet to be discovered[18].
6. Effects of Dietary Fat Source and Antibiotics and Age on Bacterial in the Ileum of Chickens
PCR with denaturing gradient gel electrophoresis (DGGE) studies how different fat sources in the diets of broilerchickens affected the microbial community in the ileum of the chickens at different ages. DGGE involves molecularfingerprinting which separates polymerase chain reaction (PCR)-generated DNA products. This experiment differs fromprevious experiments, which only focused on the cecum, by examining the parts of the small intestine the jejunum andileum, which are largely responsible for nutrient absorption. The experiment focuses only on the ileum, but notes that thesame micro flora exist in both sites. In addition, instead of studying the effects of dietary carbohydrate sources, itfocuses on dietary fat sources by feeding the chickens with either soy oil or lard and tallow mix and an antibioticsupplement (avilamycin and salinomycin mix). Salinomycin antibiotic inhibits the growth of C. perfringens. The resultsconfirmed that the microbial communities were affected by both factors: the chickens dietary fat source withantibiotics as well as the age of the chickens. As the chickens aged, there was an increase in Streptococcusalactolyticus, enterobacteria, and Clostridium perfringens. The different dietary fat sources primarily affectedLactobacillus salivarius and Clostridium perfringens. Results show that soy oil has a higher solubility which help thedispersion of antibiotics in the small intestine; thus, indirectly affects the microbial communities that live there.Clostridium perfringens, which was affected by both age and dietary fat sources, also exhibited different strains inresponse to the factors[19].
7. Why the immune system doesnt attack the small intestine
Researchers from the Dana Farber Cancer Institute and Shannon Turley, PhD, recently identified a group of lymphnode cells that instruct the immune system to leave healthy tissue alone. They have found that cells that are not generallythought of as part of the immune system actually help protect against microbe attacks in the intestine. Since the lymphnodes are found throughout the body, they suppress a variety of autoimmune diseases, which normally results fromimmune system assault on healthy tissue. In order to distinguish the normal and foreign cells, small proteins are located
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 11/13
on the cell surface called antigens. Thus the dendritic cells exposed the antigens of normal neighboring cells, which in-turn puts the immune system at ease. Turley discovered that dendritic cells are not essential in creating tolerance in Tcells but instead tolerance is produced by stomal cells from nearby lymph nodes[24].
Conclusion
A wide variety of microbes reside on the mucus surfaces of the small intestine. From these 500 bacterial species, manyof these microbial communities are beneficial for the host by: aiding in nutrient absorption, stimulating growth, providingprotection against pathogens, producing antibiotics, and even aiding in muscular activity of the small intestine. However,some microbes are parasitic and cause diseases. Despite the large number and diversity of microbes that inhabit thesmall intestine, current research and studies on the small intestine gradually provide more insight on the specific functioneach microbe, which can lead to the development of new drugs and treatments for diseases.
References
[1] Bentley-Hibbert, Dr. Stuart. Small Intestine [The small intestine is the portion of the digestive system mostresponsible for absorption of nutrients from food into the bloodstream. The pyloric sphincter governs the passage ofpartly digested food from the stomach into the duodenum. This short first]. Digital image. MedlinePlus MedicalEncyclopedia. 25 Oct. 2006. ADAM. 26 Aug. 2008.
[2] O'Hara, Ann M., and Fergus Shanahan. "The gut flora as a forgotten organ." European Molecular BiologyOrganization 7 (2006): 688-93.
[3] Willing, B. P., and A.G. Van Kessel. "Enterocyte proliferation and apoptosis in the caudal small intestine isinfluenced by the composition of colonizing commensal bacteria in the neonatal gnotobiotic pig." Journal of AnimalScience 2527th ser. 85 (2007): 3256-266.
[4] Lyczak, J.B. "Commensal Bacteria Increase Invasion of Intestinal Epithelium by Salmonella enterica SerovarTyphi." INFECTION AND IMMUNITY 71 (2003): 6610-614.
[5] Baker, S.J. "Tropical Sprue." British Medical Bulletin 28 (1972): 87-91.
[6] Glynn, Judith. "Tropical sprue--its aetiology and pathogenesis." Journal of the Royal Society of Medicine 79 (1986):599-606.
[7] Westgaard, Henrik. "Tropical Sprue." Current Treatment Options in Gastroenterology 7 (2004): 7-11.
[8] Lee, Dennis, and Jay W. Marks. "Small Intestine Bacterial Overgrowth." MedicineNet Inc..
[9] Vanderhoof, Jon A., Rosemary J. Young, Nancy Murray, and Stuart S. Kaufman. "Treatment Strategies for SmallBowel Bacterial Overgrowth in Short Bowel Syndrome." Journal of Pediatric Gastroenterology & Nutrition 27 (1998):155-60.
[10]http://www.textbookofbacteriology.net/normalflora.html
[11]Samuel Baron MD; Charles Patrick. Davis (1996). "Bacteriology": Chapter 6. Normal Flora. University of TexasMedical Branch at Galveston.
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 12/13
[12]Sears CL (2005 Oct;11). "A dynamic partnership: celebrating our gut flora". Anaerobe (5):247-51: 247251.Academic Press.
[13]Salminen S, Gueimonde M, Isolauri E (2005). "Probiotics that modify disease risk". J Nutr 135 (5): 1294 8.PMID 15867327.
[14]Wilson CL, Ouellette AJ, Satchell DP, etc: Regulation of intestinal alpha-defensin activation by themetalloproteinase matrilysin in innate host defense. Science 286:113-117, 1999.
[15]Nagi/Babiuk, A. M. "Preparation, purification and characterization of bovine Peyer's patch leukocytes." PudMedCentral. Apr. 1988. Canadian Veterinary Medical Association. 29 Aug. 2008.
[16]Lu, Jiangrang, Umelaalim Idris, Barry Harmon, Charles Hofacre, John J. Maurer, and Margie D. Lee. Diversityand Succession of the Intestinal Bacterial Community of the Maturing Broiler Chicken. Applied and EnvironmentalMicrobiology 11th ser. 69 (2003): 6816-824.
[17]Stappenbeck, Thaddeus S., Lora V. Hooper, and Jeffrey I. Gordon. Developmental regulation of intestinalangiogenesis by indigenous microbes via Paneth cells. Proceedings of the National Academy of Sciences 99 (2002):15450-5455.
[18]Mazmanian, Sarkis K., June L. Round, and Dennis L. Kasper. A microbial symbiosis factor prevents intestinalinflammatory disease. Nature 453 (2008): 620-25.
[19]Knarreborg, Ane, Mary Alice Simon, Ricarda M. Engberg, Bent Borg Jensen, and Gerald W. Tannock. Effectsof Dietary Fat Source and Subtherapeutic Levels of Antibiotic on the Bacterial Community in the Ileum of BroilerChickens at Various Ages. Applied and Environmental Microbiology 68 (2002): 5918-924.
[20]Elmes/Stanton/Howells/Lowes. "Relation between the mucosal flora and Paneth cell population of human jejunumand ileum." PudMed Central. Nov. 1984. BMJ Group. 29 Aug. 2008.
[21]"Anatomy and Function of the Gastrointestinal Tract." University of Missouri Health Care. University of Missouri.29 Aug. 2008 .
[22]Gartner & Hiatt. "Jejunum." Histology Lab. University of Medicine and Dentistry of New Jersey. 29 Aug. 2008.
[23] "Getting To Know "Friendly Bacteria"" NCCAM, National Institutes of Health 12 (2006).
[24] Turley, Shannon, and Dana Farber Cancer Institute. "Why doesn't the Immune System attack the Small Intestine?"Bright Surf. 10 Jan. 2007. The Resource for Science Institution. 27 Aug. 2008
[25]Gibson, Glenn R., and Robert A. Rastall. "When We Eat, Which Bacteria Should We Be Feeding?" AmericanSociety of Microbiology May 2004: 1-8.
[26]Dai, GuoFei. "Bactericidal and Morphological Effects of NE-2001, a Novel Synthetic Agent Directed againstHelicobacter pylori." Pubmed Central. Aug. 2005. American Society for Microbiology (ASM). 29 Aug. 2008.
-
6/11/2014 Small Intestine - MicrobeWiki
http://microbewiki.kenyon.edu/index.php/Small_Intestine#Duodenum 13/13
[27]Stinson, Murray. "Invasion and Killing of Human Endothelial Cells by Viridans Group Streptococci." PubmedCentral. May 2003. American Society for Microbiology (ASM). 29 Aug. 2008.
[28]Gibson/Rastall. "When We Eat, Which Bacteria Should We Be Feeding?" American Society for Microbiology.May 2004. American Society for Microbiology (ASM). 29 Aug. 2008.
[29]"Peptic Ulcer." Medline Plus. National Institute of Health. 29 Aug. 2008.
[30]"Antacids and Heartburn." Antacid and Heartburn. Cleveland Clinic. 29 Aug. 2008.
[31]"H. pylori and Peptic Ulcer." National Digestive Diseases Information Clearinghouse. National Institute of Health.29 Aug 2008
[32] "Regulation of Urease for Acid Habitation." George Sachs, David R. Scott, David L. Weeks, MarinaRektorscheck, and Klaus Melchers.
Edited by Ellis Chiu, Janet Kwok, Kevin Lee, Susan Lee, Martin Tang, Adnan Vahora, students of Rachel Larsen(mailto:[email protected])
Retrieved from "http://microbewiki.kenyon.edu/index.php?title=Small_Intestine&oldid=63834"Category: Curated Pages
This page was last modified on 29 April 2011, at 20:07.