small intestine imaging
-
Upload
sumer-yadav -
Category
Health & Medicine
-
view
103 -
download
1
Transcript of small intestine imaging

1
Small intestine imaging
dr sumer yadav

2

3
Indications for small bowel investigations
• Investigation of non-specific symptoms such as pain,distension,bloating,diarrhoea
• Suspected inflammatory bowel disease,includingexclusion of small bowel disease in Crohn’s colitis
• Partial small bowel obstruction• Obscure G I bleeding,iron deficient anaemia or bleeding
per rectum with normal upper G I endoscopy and colonoscopy
• Definition of anatomy,of fistulas or malrotation • Exclusion of malignancy,for example,complicating
coeliac disease

4
Difficulty in investigation
• Median lengthof 5.7m• Difficult to visualise by location and anatomy• Investigations must traverse proximal or distal
gut,and then negotiatea tortuous course• Movement,with consequent artefact• Radiation dose• Patient acceptability of for example,NG
tubes,MRI scanners• Low yield due to inappropiate referrals• Interpretation of images

5
KEY POINT 1
• The small bowel is difficult to image and studies of all techniques are limited by the lack of a gold standard reference and agreed criteria for referral

6
Techniques
• Conventional radiography• Bariummeal follow through& enteroclysis• Sonography• CT-CT enteroclysis,CTenterography• MRI-MRenteroclysis• Capsule endoscopy• Enteroscopy –push enteroscopy,push-pull
enteroscopy[also called double-balloon] and intraoperative enteroscopy

7
Conventional Xrays
• Preferred initial radiographic investigation• Diagnostic in 50-60%• Radiographs done are 1.Supine Abdomen-bladder should be emptied before the
film and film should include area from diaphragm to hernial orifices
2.Chest Radiograph- superior to erect abdomen to detect pneumoperitoneum
Chest disease may mimic SBO 3.Erect Abdomen-air fluid level are seen .normal two may
be seen at D-Jflexure and terminal ilenm

8
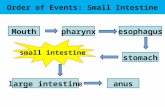
Difference between large & small intestine
• large bowel small bowel
• Haustra present absent
• Valvulae
conniventes absent present
loops pheripheral central

9
SBO IN FPA

10
FPA
Centrally placed small bowel loop
Valvulae conniventes

11Rigler’sign

12
Barium meal follow through
• 500 ml of 42%w/v barium mixture is ingested,fluroscopic and over head radiographs at 15-30 minutes intervals,continue till ileoceacal valve,when barium has reached caecum,with targeted fluroscopy of special area of interest.
• Manual palpation of the abdomen facilitates movement of contrast and assesment of fixation of bowel loops.

13
Figure

14
Figure
• X-ray image from a small bowel series showing a right inguinal hernia.

15
Saddle bags

16
Classic radiographic string sign

17
Ca cecum invading terminal ileum

18
Lymphoma mid ileum

19
carcinoid

20
• Radiograph from double-contrast upper GI showing a normal duodenum.

21
• Radiographic appearance of Crohn's disease of the terminal ileum. Nodularity, ulceration, narrowing, and irregularity ...

22
Aphthoid ulceration of terminal ileum (small arrows)- Note also "cobblestoning" (larger arrows).

23
Typical features of Crohn's disease of the distal ileum including fissure ulcers (small arrows), longitudinal ulcers (arrowhead), "cobblestoning" (open arrows), aphthoid ulcers (curved arrow) and stricturing. ic=ileocaecal valve

24
Crohn 's disease of distal ileum with stricturing and sacculation on the antimesenteric aspect (curved arrows), and fissure ulcers (small arrows). Open arrow points to ileo-caecal valve

25
Backwash ileitis" due to ulcerative colitis. Note features of chronic ulcerative colitis in right colon, patulous ileocaecal valve, dilated distal ileum with granular mucosa.

26
Chronic ileocaecal tuberculosis. The caecum and ascending colon are retracted craniad and are fibrotic. scarred and saccilated (curved arrows). The terminal ileum in this patient is relatively patulous (straight arrows) and probably nodular. v=ileocaecal valve.

27
Nodular filling defects in small bowel of AIDS patient (same of which are arrowed) are consistent with the submucosal deposits of Kaposi sarcoma. Disease was present elsewhere in the bowel. Although unverified in this patient, the thickened folds and pa or coating probably represent co-existent opportunistic infection - most likely cryptosporidium.

28
Small bowel non-Hodgkin's lymphoma. Enteroclysis examination demonstrates a segment of ileum in the right iliac fossa with wall thickening, destruction of the normal fold pattern and aneurysmal ulceration (arrowed) and mass effect

29
Benign lymphoid hyperplasia of distal ileum. Ileocaecal valve is arrowed.

30
Jejunal diverticulosis on enteroclysis examination. Multiple moderate-sized and large diverticula present.

31
Meckel's diverticulum (arrowed) demonstrated on enteroclysis in a young patient with recurrent melaena.

32
Multiple band adhesions of small bowel in left iliac fossa causing retraction, tenting and fixation of several adjacent loops.

33
Acute small bowel ischaemia. Small bowel barium study shows partial functional obstruction, proximal to diffuse spastic narrowing of ileum with thickened folds and thick walls. There is a ''picket fence" pattern in places (arrowed). c=colon.

34
Small bowel ischaemia. Same patient as slide 33 CT after intravenous contrast. Note "target" sign in thickened ileal loops in right iliac fossa (arrowed), oedema in adjacent mesentery and fluid filled obstructed bowel to left of midline. Bowel had returned to normal a few weeks later on follow up contrast study (patient then asymptomatic).

35
Advntages
• Relative ease of cocept and its execution,the availability of equipment and expertise,the acceptence to the patient,and a relatively lower radiation dose

36
Disadvantage
• Limited ability to distinguish abnormalit,given that there may be many overlying loops of small intestine
• Length of examination
• Lack of complete distention of small bowel

37
Small bowel enteroclysis
• The intubation and infusion of small bowel by barium,challenges the distensibility of bowel wall,exagerating the effects of mild or subclinical obstruction,demonstrates mucosal detail more readily
• Technique –infusion of 30-40%w/v at 60-90mi/min after duodenal intubation.
• Double contrast enteroclysis infusion of 60-95%w/v barium,followed by infusion of air/methyl cellulose to distend lumen leaving a thin coating of barium.

38
Advantages
• Shorter examination time
• Better distension
• Greater positive and negative for a wide range of S B pathology,including strictures,adhesions and intrinsic SB disease[eg sprue]

39
Disadvantage
• Patient discomfort
• Higher radiation dose
• Gastroduodenal disease may not be seen
• More experienced radiologist required

40
Key point 2
• Barium contrast studies are widely avilable but yield is low

41
Ulrtasonograpny
• Trans abdominal ultrasound• Advantages• 1.cheap• 2.quick• 3.acceptable to patient• 4.no ionising radiation-important in Crohn’s
disease patient who may require many investigations over a life time.due to this popular wiyh paediatricians
• 5.extraluminal information• 6.dynamic changes

42
• Disadvantage
• 1.operator dependent modality
• 2.lack of standardisation
• 3.less useful in obese[images are better in children] or in the presence of large volumes of bowel gases

43
Studies with of USG• Studies concentrated for use in crohn’s disease• It shows bowel wall thickening,presence of mesenteric fat wrapping.These
are used as marker of disease activity• Other sign includes pattern of vascularisation,presence of free peritoneal
fluid and mesenteric lymphadenopathy• Direct extra luminal information-presence of abscesseswhich may be
missed with small bowel contrast studies• Compared with small bowel follow through of the ileum,ileal bowel wall
thickening of more than 2.5 mm gave comparative sensitivity of 75%,specificity of 92% and P P value of 88%
• Sup. Mesenteric artery doppler does not corelate with disease severity• Small bowel follow through is more sensitiveand still indicated on strong
clinical grounds in spite of normal USG result• There is lack of agreed definition of the bowel wall thickening that may be
considered abnormal• Other disease processes, such as ileal TBand backwash ileitis of UC

44
New development in USG
• Supplementation with oral contrast
• USG after distention of the small bowel with PEG electrolyte balanced solution
• In this method greater length of diseased bowel recognised and detection of jejunal lesions other wise missed with plain USG
• By Calabrese et al
• cont.

45
• Pareante et al used nonabsorbable anechoic contrast to distend bowel with proven crohn’s disease
• In this stricture was better seen
• Authors that USG with contrast may be first-line investigation and comparable with small bowel enema

46
Doppler USG
• Evaluate changes seen in vasculature with bowel inflamation
• Incresed vascularity is seen in the bowel
• Sup. Mesenteric artery images may indicate disease activity
• But there are small no. of studies there fore the role of Doppler USG is still to be established

47
• Ultrasound showing blood flowing from intestines into liver. Image on the left: routine. On the right with power Doppler.

48
Ultrasound of thickened bowel. Relatively hypoechoic thick walls (arrowed) with echogenic lumen. Appearances are non-specific - in this case, Crohn's disease of the ileum

49
Ultrasound image demonstrates pelvic abscess and enterocutaneous fistula complicating Crohn's disease. Abscess (arrows) contains internal echoes. Hyperechoic foci (arrowhead) represent gas in bladder (b) wall.

50
Same patient as previous slide. CT of pelvis demonstrates thickened loop of ileum (small arrows), fistula to bladder (arrowhead) and gas in bladder wall (curved arrow) and in non-dependent aspect of bladder itself. More cranial image better showed associated abscess.

51
• An ultrasound miniprobe (20 MHz) is placed in the ascending part of the partly water-filled jejunal lumen in a patient with CD. The layers of the wall are seen and also an erosion/superficial ulcer (b) can be observed. The edge of the lesion is indicated

52
Key point 3
• USG may be very useful and acceptable in identifying terminal ileitis,particularly in children ,but its use is very observer-dependent and expertise in bowel USG is not widely available.

53
CT scan
C T has central role in imaging abdomen
CT can depict bowel thickening,fistulas,abscesses and lymphadenopathy
• Bowel wall assessment during different phases of scanning with i.v. contrast allows assesment of perfusion
• Intramural gas may be detected• MDCT can reconstruct images in any angle

54
C T SCAN
• Advantages
• 1.quick
• 2.acceptable to most of the patient
• 3. major advantage is –provide extraluminal information over luminal contrast studies

55
Disadvantages
• Ionising radiation
• It is static rather than dynamic .This make differentiation b/w skip lesionsand peristalsis difficult
• Artefact which may arise from the lack of physiological distension

56
CT ENTEROCLYSIS
• Newer more specific technique for small bowel
• Require same nasojejunal intubation and small bowel distension with contrast as barium enteroclysis
• More quick
• Ability to follow the progression of contrast is lacking

57
indicatinos
• Suspected malignancy
• Known inflamatory bowel disease
• Occult G I bleed
• Low grade small bowel obstruction
• Refractory coeliac sprue

58
Studies with CT ENTEROCLYSIS
• It demonstrated fistula which was not shown by other modality
• Aid in the diagnosis of ileoceacal TB by demonstrating necrotic mesenteric lymph node
• In refractory coeliac sprueit demonstrated ulceration,lymphoma,adenocarcinomaof jejunum
• Boudiaf et al• cont.

59
• Important-early crohn’s disease may be better demonstrated on small bowel enema
• In patients with very high index of suspicion,use of both tests may be appropiate
• More abnormality detected with CTenteroclysis than small bowel enema,but principally with extra luminal manifestation
• Minordi et al

60
CT ENTEROGRAPHY• Generic term for C T investigation where small bowel is distended
with orally ingested contrast as opposed to that delievered by nasojejunal tube
• Primary reason for abandoning the naso jejunal tube is patient acceptibility
• Enterography may prove itself as effective as enteroclysis• Oral contrast agent used –water,methylcellulose,PEG,dilute barium
solution• The advantage of oral hyperhydration to achieve small bowel
distensibility is that in future it could be added to the general CTabd/pelvis for abdominal pain of uncertain etiology
• Mazzeo et al

61
CT with free air and bowel loop

62
• Enterovesical fistulas

63

64
Key point 4
• CT enteroclysis shold be at least as good as small bowel enema,and will provide extraluminal informatiom.
• Images are static and repeated studies expose to ionising radiation

65
M R Imaging
• Give extra luminal information and permit multiplanar reformatting without ionising radiation
• Preferable in children and reproductive age group
• Distinguish active disease with fibrosis• Definition of tissue planes is better than CT• Real time functional information may be
obtained with MR fluroscopy and this is a distinct advantage over CT

66
• Contrast by physiological luminal content
• Purposeful distention by drinking or by enteroclysis
• Positve gadolinium based or negative iron based contrast used in MR entroclysis
• MR demonstrate In crohn’s disease –muralulcer,fistulas,pseudopolyp,thickening,stenosisand pre-stenotic dilatation

67
Disadvantage
• Patient compliance-many patient fails to complete the scan
• Long timeaffect image quality,as artefact may be produced by peristalsis
• vomiting and rectal evacuation

68
CT V/S MR
• CT in the absence of luminal distention is not sensitive for excluding small bowel pathology

69
MR V/S CONVENTIONAL RADIOGRAPHY
• No difference in finding of mural No difference in finding of mural ulceration,pseudopolyp,stenosis,pre stenotic ulceration,pseudopolyp,stenosis,pre stenotic dilatation or fistuladilatation or fistula
• More exrta luminal information with MR More exrta luminal information with MR enteroclysis in crohn’s disease as enteroclysis in crohn’s disease as abscesses,lymphadenopathy,small bowel abscesses,lymphadenopathy,small bowel separation and colonic lesionseparation and colonic lesion
• Studies say that MR enteroclysis may be inferior Studies say that MR enteroclysis may be inferior in detecting subtle lesionsin detecting subtle lesions
• EUR RADIOLOGY 2006EUR RADIOLOGY 2006

70
KEY POINT 5
• MR enteroclysis may be equivalent to other imaging modalities, but with the advantage of dynamic imaging and no ionising radiation

71
Enteroscopy
• Imp. Both diagnostic and therapeutic• Ileoscopy as part of colonoscopy• Push enteroscopy-Enteroscope which traverse
the proximal jejunum. Max. distance covered 150 cm
• Push-pull or Double Balloon enteroscopy visualise entire small bowel
• Good result in obscure GI bleed• Mucosal visualisation better than capsule
endoscopy

72
Disadvantages
• Invasive
• Risks of bleeding & perforation
• Lower patient acceptibility
• Limited expertise

73
Key point 6
• Push enteroscopy permits therapeutic intervention but has limited reach.Double Balloon enteroscopy may overcome this but is very invasiveand not widely available

74
Capsule endoscopy
• Direct luminal visualisation is aceived by the patient swallowing a capsule containing a video camera,microchip and transmitter,with images transmitted to a receiver worn by the patient
• Important complication-impactation which may require surgical removal.impactation rate 0.75%
• Contra indicated in stricturing Crohn’s disease,in implanted pace maker,in swallowing disorder
• Patency capsule-capsules with a lactose body which dissolves after 40 h to confirm the patency of the lumen
• Biopsy is not possible at present• More small bowel pathology may be seen, leading to
further investigations, not all of which may be necessary

75
• It is of note thay,in patients with suspected crohn’s disease,capsule endoscopy did not give rise to a significantly greater yield over any modality,whereas it did in the known Crohn’s disease patient.
• This is most likely to be due to the heterogeneity of patients labelled as ‘suspected Crohn’s disease’
• There is lack of consensus as to what constitutes Crohn’s disease on capsule endoscopy.
• It may be hard to distinguish b/w Crohn’s disease and NASID induced enteropathy
• Overall impression is that capsule endoscopy produces a greater yield.
• Take home message is- it may be powerful in promoting its uptake in G I world

76
Advantage
• Direct mucosal visualisation
• Patient acceptibility
• Lack of ionising radiation

77
Disadvantages
• Cost
• Reporting time
• Impaction
• Difficult to localise the lesion
• High miss rate

78
The capsule

79
Inner workings of capsule

80
Scanner

81
Key point 7
• The evidence points towarss capsule endoscopy being superior to other imaging modalities in known Crohn’s disease.however,it is not used in those with stricturing Crohn’s disease patients due to risk of capsule retention.Its usefulness in the patient with suspected Crohn’s disease is less clear.

82
Implication for practice• A department should be encoureged to ultrasound the terminal ileum of patient who
present with irritable bowel syndrome-type symptoms,in whom it is desiredto exclude inflammatory bowel disease.
• Ultrasound should be performed by G I radoiologist expert in the field of bowel sonography.
• Next tier of investigation should be CT enterography or enteroclysis,which should replace barium enteroclysis,as result are similar but the latter is more comprehensive.
• Rigorous audit shold accompany the change in practice,to ensure standards remain high and that results are as good as enteroclysis.
• For Crohn’s disease patient who may require repeated investigations over many years,MR enteroclysis should be developed
• Finally ,capsule endoscopy should be available for investigation of lesions such as angiodysplasia which are not seen on cross-sectional imaging.
• Recommendations for the investigation of obscure G I bleeding have been largely established and are likely to comprise upper and GI endoscopy,followed by a repeat UGI endoscopy as lesions are found at enteroscopy that would be within reach of the initial study. This can be followed by capsule endoscopy, then enteroscopy

83
Key point for clinical practice• The small bowel is difficult to image and studies of all techniques are limited by the
lack of a gold standard reference and agreed criteria for referral.• Barium contrast studies are widely available but yield is low.• USG may be very helpful and accepyable in identifying terminal ileitis,particularly in
children,but its use is very observer-dependent and expertise in bowel ultrasound is not widely available.
• CT enteroclysis should be at least as good as small bowel enema,and will provide extraluminal information.images are static and repeatwd studies,such as Crohn’s patient might expect during a life time,may result in considerable exposure to ionising radiation.
• MR enteroclysis may be equivalentto other imaging modalities,but with the advantage of dynamic imaging and no ionising radiation.
• Push enteroscopy permits therapeutic intervention but has limited reach.Double balloon enteroscopy may overcome this but is very invasive and not widely available.
• The evidence points towards capsule endoscopy being superior to other imaging modalities in known Crohn’s disease although it cannot be used in a large subsection of Crohn’s disease patients due to stricturing with consequent risk of capsule retention.Its usefulness in suspected Crohn’s disease is less clear.

•Thanks
84