Identification of novel target genes involved in Indian Fanconi anemia patients using microarray
-
Upload
rama-shanker -
Category
Documents
-
view
213 -
download
0
Transcript of Identification of novel target genes involved in Indian Fanconi anemia patients using microarray

Gene 531 (2013) 444–450
Contents lists available at ScienceDirect
Gene
j ourna l homepage: www.e lsev ie r .com/ locate /gene
Short Communication
Identification of novel target genes involved in Indian Fanconi anemiapatients using microarray
Pavithra Shyamsunder a, Kripa S. Ganesh a, Prasanna Vidyasekar a, Sheila Mohan b, Rama Shanker Verma a,⁎a Stem cell and Molecular Biology Laboratory, Department of Biotechnology, Indian Institute of Technology Madras, Chennai 600 036, Indiab Registry for Fanconi Anaemia in India (REFAIN), Durgabai Deshmukh General Hospital and Research Center, Durgabai Deshmukh Road, Chennai 600 028, India
Abbreviations: FA, Fanconi anemia; BM, Bone marrDiepoxybutane; HNSCC, Head and neck squamous cecrosslinks; ATXN3, Ataxin-3; ETS1, v-ets avian erythroblasto1; ARID4A, AT rich interactive domain 4A (RBP1-like); ROSSuperoxide dismutase; AML, Acute myeloid leukemia; Cleukemia; NK, Natural killer.⁎ Corresponding author at: Department of Biotec
Technology Madras, Chennai 600036, Tamil Nadu, Indfax: +91 44 22 57 4102.
E-mail address: [email protected] (R.S. Verma).
0378-1119/$ – see front matter © 2013 Elsevier B.V. All rhttp://dx.doi.org/10.1016/j.gene.2013.08.082
a b s t r a c t
a r t i c l e i n f oArticle history:Accepted 24 August 2013Available online 11 September 2013
Keywords:MicroarrayFanconi anemiaOxygen sensitivityHematological abnormalitiesImpaired immunity
Fanconi anemia (FA) is a genetic disorder characterized by progressive bonemarrow failure and a predispositionto cancers. Mutations have been documented in 15 FA genes that participate in the FA–BRCA DNA repair path-way, a fundamental pathway in the development of the disease and the presentation of its characteristic symp-toms. Certain symptoms such as oxygen sensitivity, hematological abnormalities and impaired immunity suggestthat FA proteins could participate in or independently control other pathways as well. In this study, we identified9 DNA repair genes that were down regulated in a genome wide analysis of 6 Indian Fanconi anemia patients.Functional clustering of a total of 233 dysregulated genes identified key biological processes that included regu-lation of transcription, DNA repair, cell cycle and chromosomal organization. Microarray data revealed the downregulation of ATXN3, ARID4A and ETS-1, which were validated by RTPCR in a subsequent sample set of 9 IndianFA patients. Herewe report for thefirst time a gene expression profile of Fanconi anemia patients from the Indianpopulation and a pool of genes that might aid in the acquisition and progression of the FA phenotype.
© 2013 Elsevier B.V. All rights reserved.
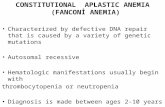
1. Introduction
Fanconi anemia (FA) is a rare autosomal or X-linked recessive(Taniguchi and D'Andrea, 2006) chromosomal instability syndromecharacterized by multiple congenital abnormalities, bone marrow(BM) failure, aplastic anemia, cancer/leukemia susceptibility, and cellu-lar hypersensitivity to clastogens such as cisplatin,mitomycin C (MMC),diepoxybutane (DEB), and melphalan. Treatment with these agentscauses increased chromosome breakage in cells derived from patientswith FA (D'Andrea and Grompe, 1997). FA patients are also susceptibleto solid tumors, such as head and neck squamous cell carcinoma(HNSCC), gynecological squamous cell carcinoma (SCC), esophagealcarcinoma, liver tumors, brain tumors, skin tumors and renal tumors.
The prevalence of FA is estimated to be 1 to 5 cases per million andheterozygous carrier frequency is estimated to be 1 in 300, althoughthe actual frequency is probably higher (Orkin et al., 2009). The medianage at diagnosis is 6.5 years for male patients, and 8 years for female pa-tients, although the age at diagnosis ranges from 0 to 48 years. Themale
ow; MMC, Mitomycin C; DEB,ll carcinoma; ICL, Interstrandsis virus E26 oncogene homolog, Reactive oxygen species; SOD,MML, Chronic myelomonocytic
hnology, Indian Institute ofia. Tel.: +91 44 2 257 4109;
ights reserved.
to female ratio is 1.24 (Taniguchi and D'Andrea, 2006). FA can be dividedinto fifteen andmore complementation groups that include—A, B, C, D1,D2, E, F, G, I, J, K, L, M and N (Dokal, 2012). Proteins encoded by FAgenes (FA proteins) include an ubiquitin ligase (FANCL/PHF9/POG),a monoubiquitinated protein (FANCD2), a helicase (FANCJ/BACH1/BRIP1), a protein with helicase motifs and a nuclease motif (FANCM)and a well-known breast/ovarian cancer susceptibility protein(FANCD1/BRCA2). FA proteins (including BRCA2) and another well-known breast/ovarian cancer susceptibility protein, BRCA1, cooperatein a common DNA repair process the “Fanconi Anemia–BRCA pathway”which is required for cellular resistance to DNA interstrand crosslinks(ICL). Furthermore, molecular and functional interaction of FA proteinswith specific DNA repair proteins namely ATM(ataxia telangiectasiamu-tated), NBS (Nijmegen breakage syndrome), RAD 51 alongside manyother DNA repair proteins ascertains the role of FA proteins in DNA dam-age (Kennedy and D'Andrea, 2005). However, symptoms like type 2 dia-betesmellitus (Golubnitschaja et al., 2006; Pácal et al., 2011), café-au laitspots (Novellino et al., 1999) and other clinical manifestations are notentirely explained by DNA repair deficiency in FA (Pagano et al., 2005),suggesting a role for FA proteins in regulating functions beyond DNA re-pair. This also suggests the presence of other proteins that may interactwith FA proteins or independently control certain pathways in FA. Awell-accepted method of understanding the development and progres-sion of a variety of diseases has been through the use of genome-wideexpression array analysis. A genome wide expression array yields dataabout candidate genes that may be involved in disease acquisition andprogression. The focus of this study was to elucidate the molecularbasis of the phenotypic symptoms exhibited by FA patients using

Table 1Primer sequences.
Gene symbol Sequence Annealing tm
ATXN3 60 °CFP 5′ AGCTGAGCACACACTGGATG 3′RP 5′ CTTGCACTGGCATCTTTTCA 3′ARID4A 60 °CFP 5′ TGGTGGATTGTGGCAGTAAA 3′RP 5′ TCAGGTAGGCAGGCTCATCT 3′ETS-1 60 °CFP 5′ TGGAGTCAACCCAGCCTATC 3′RP 5′ TCTGCAAGGTGTCTGTCTGG 3′GAPDH 60 °CFP 5′ GAAGGTGAAGGTCGGAGT 3′RP 5′ GAAGATGGTGATGGGATTTC 3′
445P. Shyamsunder et al. / Gene 531 (2013) 444–450
microarray analysis. Previous studies with Indian FA patients have con-centrated on chromosomal analysis. A study with 33 FA patients, re-vealed spontaneous chromosome breakage in 63.64% of patients,malignancies in 27.27% and chromosomal abnormalities in 55.5%(Korgaonkar et al., 2010a). Chromosomal breakage analysis in 195 pedi-atric patients revealed 17% of patients with classical FA, 4% with somaticmosaicism, 13% with high frequency of chromosomal breakage andwithout clinical features, and 66%with suspected FA but had no chromo-somal breakage and clinical features of FA (Korgaonkar et al., 2010b). Thecurrent study reports the first ever genome wide expression study forIndian FA samples and details, for the first time, down regulation ofthree target genes ATXN3, ARID4A and ETS-1. The dysregulation ofthese genes can provide explanations for oxygen sensitivity (Paganoet al., 2011), certain aberrant hematological defects (Butturini et al.,1994) and impaired immunity (Myers et al., 2011) associated with FA.
2. Materials and methods
2.1. Sample collection
Peripheral blood was collected from 15 Fanconi anemia Indian pa-tients from Andhra Mahila Sabha Hospital, Chennai, according to theIndian Council of Medical Research (ICMR) New Delhi guidelines withthe consent of the patients. All samples used for the study were charac-terized for the hypersensitivity to DNA damaging agentmitomycin C bythe clinician prior to sample collection. The clinical features of thepatients are provided in Supplementary information (Supplm data 1).Peripheral blood was also collected from 3 individuals with no symp-toms of FA who served as control for the current study. Samples werecollected in sterile PAXgene Blood RNA tubes (PreAnalytix GmbH,Switzerland) and stored at−20 °C until further processing.
2.2. RNA isolation
Total RNA was isolated from the samples using PAXgene Blood RNAisolation kit according to the manufacturer's instructions (PreAnalytixGmbH, Switzerland). Total RNAwas quantified bymeasuring the absor-bance at 260 nm using a PerkinElmer Lambda 650 UV/VIS spectropho-tometer (PerkinElmer, USA).
2.3. Oligonucleotide array analysis of RNA samples
RNA was amplified using Express Art mRNA amplification kit microversion (Artus GmbH, Germany). Amplified RNA was labeled with Cy3Post-Labeling Reactive Dye Pack (GE Healthcare UK limited, UK). La-beled RNA was fragmented and purified using Express Art Amino allylmRNA amplification kit and YM10 columns (Millipore, USA). 10.0 mgof the labeled amplified RNA was used for hybridization with theHuman 40K (A + B) OciChip array. Hybridization was performedusing the automated hybstation HS 4800. The hybridized chips werescanned using an Affymetrix 428TM array scanner at three differentPMT gains. The interest was to determine probes (genes) that were dif-ferentially expressed (DE) between the normal and FA samples. Athreshold log fold change (LFC) of 3.0 was fixed to attain an FDR ofless than 0.05 and accordingly the DE genes were obtained. The statisti-cal analysis was carried out using the R package and the biological anal-ysis was carried out using GenowizTM software (Ocimum Biosolutions,USA).
2.4. Functional clustering and gene ontology analysis
The differentially expressed genes obtained through the aforemen-tioned comparisons were functionally clustered under different geneontology (GO) terms using the microarray analysis software — DAVID(The Database for Annotation, Visualization and Integrated Discovery)(Huang da et al., 2008). The terms were categorized into biological
process, molecular function and cellular component. For each GOterm, the p-value was calculated. A term with p b 0.05 was consideredto be enriched with genes. The p-value was calculated as thehypergeometric probability to get so many probes/probesets/genes foraGO term, under the null hypothesis that theywere picked out random-ly from the microarray. The lower the p-value, the more significant theGO term.
2.5. Real time PCR amplification
Total RNA (1.6 μg) was reverse transcribed from oligo-dT primers(NEB, USA) and the resulting cDNA was amplified by PCR using gene-specific primers (MWG biotech, Germany). Real time PCR was carriedout using a DyNAmo ColorFlash SYBR Green qPCR Kit (Thermo, USA)on an Eppendorf mastercycler, ep realplex (Eppendorf, Germany). Atwo-step cycling protocol was performed consisting of a single 7 min-ute cycle at 95 °C, followed by 40 cycles of 10 s at 95 °C, and 30 s at60 °C. Melting curve analysis was performed after amplification tocheck for thepresence of any spurious amplification or for the formationof primer dimers. Relative mRNA expression was determined by nor-malization against the expression of a housekeeping gene, glyceralde-hyde 3-phosphate dehydrogenase (GAPDH). The primer sequenceshave been listed in Table 1.
3. Results
3.1. Identification of differentially expressed genes
Microarray analysis was carried out on 6 FA patient blood samples.Microarray analysis resulted in the identification of 233 commonlydysregulated genes. Out of the 233 genes, 52 were upregulated and181 were downregulated. This list included 9 DNA repair genes, 54genes involved in the regulation of transcription, 11 chromosome orga-nizing genes and 14 genes regulating cell cycle. The entire dysregulatedgene list is available in the supplementary data (Suplm data 2).
3.2. Gene ontology/functional enrichment analysis to identify dysregulatedprocesses
Gene ontology/functional enrichment analysis was utilized to iden-tify the involvement of differentially expressed genes in various biolog-ical processes and molecular functions using DAVID (Huang da et al.,2008). This analysis clustered genes into a variety of functional groups(Fig. 1, Table 2) with regulation of transcription, DNA repair, cell cycleand chromosomal organization being of utmost significance. Table 3 de-picts the fold changes of genes functioning in regulation of transcription,DNA repair, cell cycle and chromosomal organization.

Table 2Functional enrichment of dysregulated genes.
Biological process Counta p-value %a
Regulation of transcription 54 3.69E-06 23.17Intracellular transport 18 0.001136 7.72Protein transport 19 0.002244 8.15Cellular component disassembly 5 0.002926 2.14DNA repair 9 0.014927 3.86Tricarboxylic acid cycle 3 0.027191 1.28DNA metabolic process 12 0.027522 5.15Membrane organization 10 0.028143 4.29Chromosome organization 11 0.04699 4.72Regulation of cell activation 6 0.047512 2.57Mesoderm formation 3 0.061627 1.28Cell cycle 14 0.097139 6
a Count represents the number of geneswithin each biological process; % represents thefraction of genes within each biological process with reference to a total number of 233dysregulated genes.
446 P. Shyamsunder et al. / Gene 531 (2013) 444–450
3.3. Microarray data validation
Microarray data of the 6 samples (FAP1-6) was validated using qPCRfor three differentially expressed genes: ATXN3, ARID4A and ETS-1 in adifferent set of 9 Indian FA samples (P1-9). GAPDHwas used as an inter-nal control. Expression levels of ATXN3, ARID4A and ETS-1 validated themicroarray data (Fig. 2).
4. Discussion
Genome wide expression analysis was used to identify candidategenes that are dysregulated in FA patients from the Indian population.Our study revealed various genes and processes that may influencethe phenotypic symptoms of FA. We report, for the first time, thedysregulation of 54 transcription factors, 9 DNA repair genes, 11 genesinvolved in chromosomal organization and 14 cell cycle genes in FA pa-tients (Fig. 3) in our genomewide screen. Thefindings of themicroarrayanalysis led us to hypothesize that several genes apart from the FA pro-teins may influence basic processes like DNA repair and cell cycle pro-gression which are affected in FA patients. The absence of a functionalFA protein has been linked to the clinical and phenotypic symptomsexhibited by FA patients. We have also identified additional candidategenes like ATXN3, ARID4A and ETS-1 that might cause or exacerbatethe symptoms attributed to a defective FA–DNA repair pathway.Amongst the dysregulated genes identified, ATXN3, ARID4A and ETS-1served as interesting targets as these genes could explain ROS sensitiv-ity of FA cells (Pagano et al., 2011), hematological abnormalities(Butturini et al., 1994) and impaired immune function presented byFA patients (Myers et al., 2011).
4.1. FA and ROS sensitivity
A plethora of symptoms characterize Fanconi anemia, of which thesensitivity of FA cells to oxidative stress (Pagano et al., 2011) andredox imbalances (Du et al., 2008) play a pivotal role in the clinicalman-ifestation of the disease. Although the established role of FANC proteinsis believed to be DNA repair (Kennedy and D'Andrea, 2005), there isstrong evidence suggesting that the FA proteins could be involved inguarding the cell against oxygen toxicity or at least preventing the accu-mulation of exogenous molecules (Korgaonkar et al., 2010a). Levels ofreactive oxygen species (ROS) are excessive in awide variety of diseases(Halliwell et al., 1992). Amongst the ROS produced by living cells, O2⁎−is a type of ROS that is proinflammatory in nature and damages cells.Certain ROS mediate cell functions like proliferation and programmed
Fig. 1. Gene ontology analysis of dysregulated genes— Gene ontology analysis was carried outeach biological process. Genes were functionally enriched using DAVID software.
cell death by regulating intracellular signaling cascades (Haddad,2002). A key cellular component that guards the cell against the effectsof O2⁎− is Superoxide dismutase (SOD). The enzyme functions bytransforming O2⁎− into Hydrogen peroxide(H2O2) and thus preventingthe formation of peroxynitrite (ONOO−) and hydroxyl radical (HO)(Afonso et al., 2007). The downregulation of SOD2 has been shown toincrease the levels of mitochondrial O2⁎− (Morten et al., 2006). FA pro-teins that function in DNA repair are also known to interact with pro-teins that are involved in redox related functions like GST (Cumminget al., 2001) and cytochrome P4502E1 (CYP2E1) (Futaki et al., 2002).Korkina and Kumari et al. demonstrated that ROS levels were higherin freshly collected leucocytes from patients and in the mitochondriaof FA cells (Korkina et al., 1992; Kumari et al., 2013) and three indepen-dent studies have reported that FA blood cells exhibit lowered levels ofSOD (Joenje et al., 1979; Kumari et al., 2013; Yoshimitsu et al., 1984),hinting at the presence of a regulatory mechanism controlling SOD ex-pression. One of the regulators of SOD expression is ATXN3. This regula-tory effectwasdemonstrated bymeans of anATXN3knockdownmodel.In this model, knock down of ATXN3 subsequently resulted in loweredlevels of SOD2 (Araujo et al., 2011). Our genome wide screen of FA pa-tients revealed downregulation of ATXN3. FA cells exhibit increased ox-ygen sensitivity (Pagano et al., 2011) and lowered levels of SOD (Joenjeet al., 1979; Yoshimitsu et al., 1984). Considering the results of theATXN3 knock down model, we believe that the lowered levels ofATXN3 as obtained through our screen could contribute towards
for the 233 differentially expressed genes. Figure depicts the number of genes involved in

447P. Shyamsunder et al. / Gene 531 (2013) 444–450
increased sensitivity of FA cells to ROS. Thus, ATXN3 could be one of theregulatory molecules that work concomitantly with the other FA genesin guarding the genome against oxygen toxicity. While studies have
Table 3Microarray fold changes observed for dysregulated genes functioning in significant biological p
Genesymbol
Gene name Unigene FAP1
ARID4A AT rich interactive domain 4A (RBP1-like) Hs.161000 −2.088234ATXN3 Ataxin 3 Hs.532632 −2.664803ETS1 v-ets erythroblastosis virus E26 oncogene
homolog 1 (avian)Hs.369438 −4.092708
BCOR BCL6 corepressor Hs.659681 −1.139996CCNT1 Cyclin T1 Hs.279906 −2.246266CHD2 Chromodomain helicase DNA binding protein 2 Hs.220864 −2.838614CNOT2 CCR4-NOT transcription complex, subunit 2 Hs.133350 −2.894902CNOT4 CCR4-NOT transcription complex, subunit 4 Hs.490224 −2.069109CRK v-crk sarcoma virus CT10 oncogene homolog (avian) Hs.638121 −1.980451CSDE1 Cold shock domain containing E1, RNA-binding Hs.69855 −5.225931CTNND1 Catenin (cadherin-associated protein), delta 1 Hs.166011 −1.878359HDAC3 Histone deacetylase 3 Hs.519632 −0.908127JRKL Jerky homolog-like (mouse) Hs.105940 −1.229229KLF4 Kruppel-like factor 4 (gut) Hs.376206 −0.647018LIMD1 LIM domains containing 1 Hs.193370 −0.825771MBD1 Methyl–CpG binding domain protein 1 Hs.405610 −0.982658MDM2 Mdm2 p53 binding protein homolog (mouse) Hs.484551 −1.191055MED12 Mediator complex subunit 12 Hs.409226 −0.798645MED6 Mediator complex subunit 6 Hs.497353 −1.556077MEF2C Myocyte enhancer factor 2C Hs.649965 −2.041590MTERF Mitochondrial transcription termination factor Hs.532216 −1.205538MYNN Myoneurin Hs.507025 −1.684755KAT6A K (lysine) acetyltransferase 6A Hs.491577 −2.835789NFX1 Nuclear transcription factor, X-box binding 1 Hs.413074 −2.274711NFYA Nuclear transcription factor Y, alpha Hs.10441 −0.721893NR2C2 Nuclear receptor subfamily 2, group C, member 2 Hs.555973 −1.318492NRIP1 Nuclear receptor interacting protein 1 Hs.155017 −1.090576PHTF2 Putative homeodomain transcription factor 2 Hs.203965 −0.960236PMS2P3 Postmeiotic segregation increased 2 pseudogene 3 Hs.659871 −2.164776PRDM2 PR domain containing 2, with ZNF domain Hs.371823 −1.051003PRKAR1A Protein kinase, cAMP-dependent, regulatory,
type I, alpha (tissue specific extinguisher 1)Hs.280342 −3.409387
RFC1 Replication factor C (activator 1) 1, 145 kDa Hs.507475 −1.437767SAFB2 Scaffold attachment factor B2 Hs.655392 −1.623107SFPQ Splicing factor proline/glutamine-rich Hs.355934 −4.763948SMARCC1 SWI/SNF related, matrix associated, actin dependent
regulator of chromatin, subfamily c, member 1Hs.476179 −2.39639
SSBP3 Single stranded DNA binding protein 3 Hs.658676 −1.181881SUPT16H Suppressor of Ty 16 homolog (S. cerevisiae) Hs.213724 −3.299234SUPT6H Suppressor of Ty 6 homolog (S. cerevisiae) Hs.250429 −1.818026TMF1 TATA element modulatory factor 1 Hs.267632 −2.756142TMPO Thymopoietin Hs.11355 −1.352596TRPS1 Trichorhinophalangeal syndrome I Hs.657018 −1.840082TTF2 Transcription termination factor, RNA polymerase II Hs.486818 −1.689048XRN2 5′–3′ exoribonuclease 2 Hs.255932 −3.094427ZBTB1 Zinc finger and BTB domain containing 1 Hs.605143 −1.988054ZMYND11 Zinc finger, MYND-type containing 11 Hs.292265 −2.281413ZNF143 Zinc finger protein 143 Hs.523471 −0.610100ZNF189 Zinc finger protein 189 Hs.50123 −0.945426ZNF192 Zinc finger protein 192 Hs.57679 −1.882509ZNF224 Zinc finger protein 224 Hs.585869 −1.670326ZNF263 Zinc finger protein 263 Hs.611475 −1.474178ZNF354C Zinc finger protein 354C Hs.272328 −1.001033ZNF485 Zinc finger protein 485 Hs.147440 −1.074190CEP110 Centriolar coiled coil protein 110 kDa Hs.653263 −2.392417CKAP2 Cytoskeleton associated protein 2 Hs.444028 −1.248540CUL3 Cullin 3 Hs.372286 −3.661268HUWE1 HECT, UBA andWWE domain containing 1 Hs.136905 −1.668632MCM8 Minichromosomemaintenance complex component 8 Hs.597484 −0.759321MPHOSPH6 M-phase phosphoprotein 6 Hs.344400 −1.051056MRE11A MRE11 meiotic recombination 11 homolog A
(S. cerevisiae)Hs.192649 −1.513986
PAFAH1B1 Platelet-activating factor acetylhydrolase 1b,regulatory subunit 1 (45 kDa)
Hs.77318 −2.735348
POLH Polymerase (DNA directed), eta Hs.655467 −0.865089PPP5C Protein phosphatase 5, catalytic subunit Hs.654604 −1.267057RAD52 RAD52 homolog (S. cerevisiae) Hs.410355 −1.372267UVRAG UV radiation resistance associated gene Hs.728868 −2.663826
a RT — Regulation of transcription, CC — Cell cycle, DR— DNA repair, CO— Chromosomal or
revealed the role of ROS in the FA phenotype, RNS, nitrosative stressmay also be another hallmark worth exploring in the future (Paganoet al., 2013).
rocesses.
FAP2 FAP3 FAP4 FAP5 FAP6 Functiona
4 −1.8814225 −2.6952906 −2.4275098 −3.8181794 −3.8967519 RT, CO5 −2.8560681 −3.150746 −2.9082077 −3.7393537 −3.9834485 RT, DR
−4.1299314 −4.1350837 −4.8303757 −4.0425625 −4.16098 RT
5 −0.7037759 −2.4459937 −2.2662945 −1.7982032 −1.4580443 RT, CO8 −2.2150784 −3.4145777 −3.7996588 −6.037102 −6.1391745 RT, CC5 −3.4455738 −3.8617468 −3.7852848 −3.3884482 −3.285871 RT, CO7 −2.9599395 −1.745224 −1.6148648 −1.2874866 −1.3241405 RT
−2.0576768 −2.988181 −2.5086281 −2.983029 −2.937101 RT1 −2.3040824 −3.6022077 −2.8751872 −2.5895712 −3.6518314 RT6 −3.2928753 −1.3346844 −1.3652673 −1.0836091 −1.2957387 RT3 −1.4631181 −4.5063562 −5.0104012 −5.4775863 −5.8052955 RT8 −1.0579424 −3.5581834 −3.3086352 −1.3419857 −2.2663174 RT, CC, CO9 −1.3720741 −4.4163322 −4.340958 −4.5027514 −4.072406 RT9 −0.6433077 −1.3697188 −1.3520951 −1.061784 −2.6196897 RT8 −1.2499804 −3.9692376 −5.070657 −4.085126 −4.913678 RT9 −0.6718884 −2.7590778 −2.5483532 −1.7366831 −2.3630772 RT8 −1.3518295 −1.8929324 −1.8817682 −5.939037 −5.14754 RT, CC5 −0.9275179 −2.5297499 −1.4504995 −1.7511351 −2.6985128 RT5 −1.1943803 −2.1636772 −2.1833315 −2.0736606 −2.3324292 RT2 −2.095941 −1.5725875 −1.5910478 −2.2946625 −1.1648741 RT7 −0.8175936 −2.708548 −2.6939423 −2.041026 −1.9039416 RT3 −1.7255974 −2.148846 −1.6326177 −1.5640934 −1.9892774 RT7 −3.0045652 −1.3772879 −0.9933968 −1.9256244 −2.091951 RT, CO1 −1.8757906 −0.8616953 −1.5426261 −1.8838735 −1.62391 RT3 −0.8053327 −2.2710748 −1.6756492 −2.3338935 −2.1837924 RT9 −1.4832335 −1.4082527 −1.2675412 −3.1266198 −3.1214888 RT6 −1.3725276 −2.7412448 −2.3659058 −1.1863141 −0.813828 RT6 −1.5217209 −2.706872 −2.7262647 −3.1478033 −3.1622567 RT8 −2.1994643 −1.584861 −1.89592 −2.3920372 −1.741571 RT, DR
−0.6481133 −1.3523777 −1.2353115 −1.1318169 −1.3344331 RT6 −3.2220068 −2.0842462 −1.4994707 −2.3852787 −2.7978168 RT
5 −1.7300186 −0.8110757 −1.0781198 −1.0431266 −0.8183808 RT, CO, DR9 −1.0178995 −1.835352 −1.8898158 −0.9453516 −0.7466931 RT4 −4.1773624 −3.9869478 −4.022042 −4.3315268 −4.0402308 RT, DR
−2.3536997 −1.9486163 −2.3160958 −1.7731533 −1.3023686 RT, CO
4 −1.3957362 −1.1231089 −2.9222317 −3.2321935 −3.4770856 RT−3.450623 −3.1630425 −3.701679 −3.6621096 −3.7621841 RT, CO, DR
1 −1.9685874 −1.9490142 −1.8085268 −1.3239937 −1.2504492 RT, CO1 −3.154498 −2.6024256 −2.387364 −3.5527754 −3.8389387 RT3 −2.0067801 −2.5897183 −2.8365726 −4.4237757 −4.360162 RT6 −1.6186805 −4.011957 −3.2441294 −2.5762646 −3.3779342 RT8 −1.5673528 −4.595577 −4.0857687 −3.9160326 −2.6046264 RT6 −2.0169272 −2.1364152 −1.5267248 −1.0351906 −2.9206352 RT8 −2.0683093 −2.6538742 −3.547709 −2.886253 −3.7151854 RT
−2.3172812 −2.4929187 −3.3524187 −3.2515028 −3.1219494 RT, CC8 −1.0869212 −1.8461668 −1.5537093 −1.7527261 −2.227175 RT5 −1.3029137 −2.1524434 −1.572439 −2.182274 −2.4836807 RT7 −1.3200936 −5.3963485 −5.1017914 −7.45697 −7.812148 RT7 −1.633368 −2.9632657 −2.898582 −2.5219958 −2.4418943 RT3 −0.7494359 −3.4036043 −3.5644054 −1.1062346 −1.7896869 RT3 −0.9885936 −5.4903374 −5.414627 −6.8843 −6.4973564 RT6 −1.5120106 −2.6228955 −3.6198347 −2.7269094 −2.6004796 RT4 −2.3456988 −3.079011 −2.3998573 −3.200707 −3.3882103 CC9 −1.3526568 −3.409547 −3.4089396 −2.8354964 −2.5187504 CC7 −2.6796284 −5.468642 −5.107132 −5.872275 −5.8860626 CC
−1.9072194 −2.1330204 −2.4220853 −1.9308553 −2.5556498 CO2 −0.9311252 −2.0144038 −3.4816597 −1.502178 −1.1706347 RT, CC4 −0.745841 −4.80761 −4.2019186 −3.702878 −3.7931986 CC6 −1.5531545 −2.3768024 −3.1562812 −4.266412 −3.9324493 CC, DR, CO
2 −2.6822934 −1.1477141 −0.6715474 −1.1534762 −1.6222134 CC
4 −1.3602586 −4.11924 −4.592596 −4.5615735 −3.721238 DR4 −0.8399777 −3.7891712 −4.8423033 −2.530812 −3.7116804 CC7 −1.6867933 −2.1181064 −2.370849 −2.7214417 −1.7899549 DR, CC, CO5 −2.751512 −4.8178444 −4.064264 −3.8162055 −4.969411 DR
ganization.

448 P. Shyamsunder et al. / Gene 531 (2013) 444–450
4.2. FA and hematological abnormalities
Hematological abnormalities are exhibited by themajority of FA pa-tients. The abnormalities include, pancytopenia, bone marrow failure,MDS and AML (Butturini et al., 1994). Production of proinflammatorycytokines like TNF-α and IFN-γ are abnormally high in the serum andbone marrow of FA patients (Dufour et al., 2003; Matsushita et al.,2011; Schultz and Shahidi, 1994) and this could contribute to the hema-topoietic defects in FA. The other gene identified in our screen ARID4A,which was downregulated in all the patient samples is known to affectcertain hematological functions. The involvement of ARID4A in hemato-logical abnormalities is based on a study that utilized an ARID4A knockdownmouse model. These mice exhibited dysregulated hematopoiesis,anemia followed by CMML, which ultimately progressed into AML indi-cating that ARID4A may serve as a leukemic suppressor (Wu et al.,2008). Few of the hematological abnormalities exhibited by ARID4Aknock down mice have also been observed in FA patients, suggestingthat ARID4Amay be one of the genes involved in themaintenance of he-matopoiesis and its absence could contribute to the hematological ab-normalities observed in FA.
Fig. 2. The Fanconi anemia network— Functional clus
4.3. FA and impaired immunity
Several reports have suggested lowered activity and number of im-mune cells in FA patients. Froom et al. established that FA patientsdisplayed lowered activity of Natural killer (NK) cells (Froom et al.,1987). While Petridou and Barrett showed that the NK cell numberand activity were significantly reduced in FA patients (Petridou andBarrett, 1990). A study by Meyers et al., showed lowered number ofNK cells with blunted cytotoxic function in FA patients. They also sug-gested that immune impairment in FA patients encompassed abnormal-ity in cytotoxic T cell function and defective B cell compartment (Myerset al., 2011). Castello et al., also demonstrated a quantitative defect inthe B cell compartment. This defect wasmore severe in FA homozygouspatients (Castello et al., 1998). Korthof et al. have also reported similarobservations alongside lowered serum levels of IgG and IgM (Korthofet al., 2013).
The Ets family of proteins regulates developmental processes in re-sponse to extracellular signals (Oikawa and Yamada, 2003). ETS-1 isover-expressed in lymphoid cells and regulates the transcription oflymphoid-specific genes (Anderson et al., 1999; Bassuk and Leiden,
tering of the genes downregulated in FA patients.

Fig. 3. Microarray data validation — Real time PCR analysis of ATXN3, ARID4A and ETS-1 in 9 Indian FA patient samples.
449P. Shyamsunder et al. / Gene 531 (2013) 444–450
1997). ETS-1 is important for maintaining the cellularity of the thymusand for efficient thymocyte development (Bories et al., 1995;Muthusamy et al., 1995). ETS-1 −/− mice had reduced peripheral Tcell numbers and mature T lymphocytes were highly susceptible to ap-optosis in vitro. Development of functional NK cells was established tobe regulated by ETS-1 (Barton et al., 1998). ETS-1 knock down miceexhibited impaired development of B cell precursors and inactivationof the ETS-1 gene affected varied aspects of B cell development andfunction (Eyquem et al., 2004). Our genome wide screen identified thedownregulation of the ETS-1 gene, which was validated by RT-PCR in9 Indian FA patients. The lowered levels of ETS-1, as observed in ourstudy could potentially affect the immune components like NK-cellsand B-cells in FA.
Being the first report of a genome wide expression profile of Indianpatients, the identification of several dysregulated genes is significant,as this array of genes, or part of it, may serve as potential markers forFanconi anemia in the Indian population. The identified genes are in-volved in central processes that are impaired in FA cells such as tran-scription, chromosomal organization, DNA repair and cell cycle
Fig. 4. Dysregulated target genes and their possible manifestations in FA.
progression. Three target genes were found to be dysregulated, whichmay potentially contribute towards the phenotypic features of FA pa-tients. Fig. 4 represents the involvement of these 3 genes — ATXN3,ARID4A and ETS-1 in the phenotypic manifestations of FA patients.With this study, we put forward the possibility that ATXN3 may be in-volved in the regulation of ROS levels, ARID4A in the regulation of he-matological functions and ETS-1 in the regulation of immune function,providing a primer for further studies to confirm the actual role andfunctions of these genes in FA.
Conflict of interest
The authors state that there is no conflict of interest.
Acknowledgment
This work was supported by a grant to R.S.V. by the Department ofBiotechnology (DBT — BT/PR11268/MED/12/416/2008). P.S. and P.V.wish to thank the Council of Scientific and Industrial Research, Indiafor their senior research fellowship.
Appendix A. Supplementary data
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.gene.2013.08.082.
References
Afonso, V., Champy, R., Mitrovic, D., Collin, P., Lomri, A., 2007. Reactive oxygen species andsuperoxide dismutases: role in joint diseases. Joint, Bone, Spine 74, 324–329.
Anderson, M.K., Hernandez-Hoyos, G., Diamond, R.A., Rothenberg, E.V., 1999. Precise de-velopmental regulation of Ets family transcription factors during specification andcommitment to the T cell lineage. Development 126, 3131–3148.
Araujo, J., et al., 2011. FOXO4-dependent upregulation of superoxide dismutase-2 in re-sponse to oxidative stress is impaired in spinocerebellar ataxia type 3. Hum. Mol.Genet. 20, 2928–2941.
Barton, K., et al., 1998. The Ets-1 transcription factor is required for the development ofnatural killer cells in mice. Immunity 9, 555–563.
Bassuk, A.G., Leiden, J.M., 1997. The role of Ets transcription factors in the developmentand function of the mammalian immune system. Adv. Immunol. 64, 65–104.
Bories, J.C., et al., 1995. Increased T-cell apoptosis and terminal B-cell differentiation in-duced by inactivation of the Ets-1 proto-oncogene. Nature 377, 635–638.
Butturini, A., Gale, R.P., Verlander, P.C., Adler-Brecher, B., Gillio, A.P., Auerbach, A.D., 1994.Hematologic abnormalities in Fanconi anemia: an International Fanconi Anemia Reg-istry study. Blood 84, 1650–1655.
Castello, G., Gallo, C., Napolitano, M., Ascierto, P.A., 1998. Immunological phenotype anal-ysis of patients with Fanconi's anaemia and their family members. Acta Haematol.100, 39–43.

450 P. Shyamsunder et al. / Gene 531 (2013) 444–450
Cumming, R.C., Lightfoot, J., Beard, K., Youssoufian, H., O'Brien, P.J., Buchwald, M., 2001.Fanconi anemia group C protein prevents apoptosis in hematopoietic cells throughredox regulation of GSTP1. Nat. Med. 7, 814–820.
D'Andrea, A., Grompe, M., 1997. Molecular biology of Fanconi anemia: implications for di-agnosis and therapy. Blood 90, 1725–1736.
Dokal, I., 2012. Heightened DNA damage response impairs hematopoiesis in Fanconi ane-mia. Haematologica 97, 1117.
Du,W., Adam, Z., Rani, R., Zhang, X., Pang, Q., 2008. Oxidative stress in Fanconi anemia he-matopoiesis and disease progression. Antioxid. Redox Signal. 10, 1909–1921.
Dufour, C., et al., 2003. TNF-alpha and IFN-gamma are overexpressed in the bonemarrowof Fanconi anemia patients and TNF-alpha suppresses erythropoiesis in vitro. Blood102, 2053–2059.
Eyquem, S., et al., 2004. The development of early and mature B cells is impaired in micedeficient for the Ets-1 transcription factor. Eur. J. Immunol. 34, 3187–3196.
Froom, P., Aghai, E., Dobinsky, J.B., Quitt, M., Lahat, N., 1987. Reduced natural killer activityin patients with Fanconi's anemia and in family members. Leuk. Res. 11, 197–199.
Futaki, M., et al., 2002. The FANCG Fanconi anemia protein interacts with CYP2E1: possi-ble role in protection against oxidative DNA damage. Carcinogenesis 23, 67–72.
Golubnitschaja, O., Moenkemann, H., Trog, D.B., Blom, H.J., De Vriese, A.S., 2006. Activationof genes inducing cell-cycle arrest and of increased DNA repair in the hearts of ratswith early streptozotocin-induced diabetes mellitus. Med. Sci. Monit. 12, 68–74.
Haddad, J.J., 2002. Antioxidant and prooxidantmechanisms in the regulation of redox (y)-sensitive transcription factors. Cell. Signal. 14, 879–897.
Halliwell, B., Gutteridge, J.M., Cross, C.E., 1992. Free radicals, antioxidants, and human dis-ease: where are we now? J. Lab. Clin. Med. 119, 598–620.
Huang da, W., Sherman, B.T., Lempicki, R.A., 2008. Systematic and integrative analysis oflarge gene lists using DAVID bioinformatics resources. Nat. Protoc. 4, 44–57.
Joenje, H., et al., 1979. Erythrocyte superoxide dismutase deficiency in Fanconi's anaemiaestablished by two independent methods of assay. Scand. J. Clin. Lab. Invest. 39,759–764.
Kennedy, R., D'Andrea, A., 2005. The Fanconi Anemia/BRCA pathway: new faces in thecrowd. Genes Dev. 19, 2925–2940.
Korgaonkar, S., Ghosh, K., Vundinti, B.R., 2010a. Clinical, genetic and cytogenetic study ofFanconi anemia in an Indian population. Hematology 15, 58–62.
Korgaonkar, S., Ghosh, K., Jijina, F., Vundinti, B.R., 2010b. Chromosomal breakage study inchildren suspected with Fanconi anemia in the Indian population. J. Pediatr. Hematol.Oncol. 32, 606–610.
Korkina, L.G., Samochatova, E.V., Maschan, A.A., Suslova, T.B., Cheremisina, Z.P., Afanas' ev,I.B., 1992. Release of active oxygen radicals by leukocytes of Fanconi anemia patients.J. Leukoc. Biol. 52, 357–362.
Korthof, E.T., et al., 2013. Immunological profile of Fanconi anemia: a multicentric retro-spective analysis of 61 patients. Am. J. Hematol. 88, 472–476.
Kumari, U., Ya Jun, W., Huat Bay, B., Lyakhovich, A., 2013. Evidence of mitochondrial dys-function and impaired ROS detoxifyingmachinery in Fanconi Anemia cells. Oncogene14 (10.1097).
Matsushita, N., et al., 2011. Direct inhibition of TNF-α promoter activity by Fanconi ane-mia protein FANCD2. PLoS One 6. http://dx.doi.org/10.1371/journal.pone.0023324.
Morten, K.J., Ackrell, B.A., Melov, S., 2006. Mitochondrial reactive oxygen species in micelacking superoxide dismutase 2: attenuation via antioxidant treatment. J. Biol.Chem. 281, 3354–3359.
Muthusamy, N., Barton, K., Leiden, J., 1995. Defective activation and survival of T cellslacking the Ets-1 transcription factor. Nature 377, 639–642.
Myers, K.C., et al., 2011. Impaired immune function in children with Fanconi anaemia. Br.J. Haematol. 154, 234–240.
Novellino, L., Napolitano, A., Prota, G., 1999. 5, 6-Dihydroxyindoles in the fenton reaction:a model study of the role of melanin precursors in oxidative stress andhyperpigmentary processes. Chem. Res. Toxicol. 12, 985–992.
Oikawa, T., Yamada, T., 2003. Molecular biology of the Ets family of transcription factors.Gene 303, 11–34.
Orkin, S.H., Nathan, D.G., Ginsburg, D., 2009. Inherited bone marrow failure syndromes.In: Orkin, S.H. (Ed.), Hematology of Infancy and Childhood. Saunders Elsevier, Phila-delphia, pp. 307–396.
Pácal, L., et al., 2011. Parameters of oxidative stress, DNA damage and DNA repair in type1 and type 2 diabetes mellitus. Arch. Physiol. Biochem. 117, 222–230.
Pagano, G., et al., 2005. Oxidative stress as a multiple effector in Fanconi anaemia clinicalphenotype. Eur. J. Haematol. 75, 93–100.
Pagano, G., Aiello Talamanca, A., Castello, G., Pallardó, F., Zatterale, A., Degan, P., 2011. Ox-idative stress in Fanconi anaemia: from cells and molecules toward prospects in clin-ical management. Biol. Chem. 393, 11–21.
Pagano, G., et al., 2013. From clinical description, to in vitro and animal studies, and back-ward to patients: oxidative stress and mitochondrial dysfunction in Fanconi anemia.Free Radic. Biol. Med. 58, 118–125.
Petridou, M., Barrett, A.J., 1990. Physical and laboratory characteristics of heterozygotecarriers of the Fanconi aplasia gene. Acta Paediatr. Scan. 79, 1069–1074.
Schultz, J.C., Shahidi, N.T., 1994. Detection of tumor necrosis factor-alpha in bonemarrowplasma and peripheral blood plasma from patients with aplastic anemia. Am.J. Hematol. 45, 32–38.
Taniguchi, T., D'Andrea, A.D., 2006. Molecular pathogenesis of Fanconi anemia: recentprogress. Blood 107, 4223–4233.
Wu, M.Y., Eldin, K.W., Beaudet, A.L., 2008. Identification of chromatin remodelinggenes Arid4a and Arid4b as leukemia suppressor genes. J. Natl. Cancer Inst.100, 1247–1259.
Yoshimitsu, K., Kobayashi, Y., Usui, T., 1984. Decreased superoxide dismutase activity oferythrocytes and leukocytes in Fanconi's anemia. Acta Haematol. 72, 208–210.