Introduction and Anemia 2007
-
Upload
gary-allegretta -
Category
Health & Medicine
-
view
1.755 -
download
16
description
Transcript of Introduction and Anemia 2007

UNE HEMATOLOGY SECTION
CLINICAL PEDIATRIC HEMATOLOGY
December, 2008

An Introduction
Pediatric Hematology-Oncology, 1984-98 Hospice & Palliative Care Medicine Medical Director, The Jason Program, 1998 -
2008
Gary Allegretta, MD

Pediatric Hematology Outline
Section 1: The Red Cell Section 2: Leukocytes & Marrow
Failure Section 3: Coagulation Section 4: Hematopoietic Malignancies Section 5: Hematologic Manifestations
of Systemic DiseaseTake-Home pointTake-Home point

Section I : The Red Cell
General Physiology Developmental Physiology Definition & Effects of Anemia Formulating a Differential Dx Specific Conditions
Newborns Children & Adolescents

Bilirubin Metabolism
Intravascular
Extravascular
Free Hgb+
Haptoglobin
Fe + Transferrin
Free Hgb
Red cells contain SGOT
& LDH
All Fe is recycled

Effects on Health & Disease
Developmental RBC Physiology

Newborn Blood Values
Age Hgb g/dl Hct% MCV Retic WBC Plts EPO
Term 14.5-22.5 48-69 95-121 0.4-6 9-30 84-478 35.6 mU/ml
3 days Same 44-72 Gradual Change
Gradual Change
150-400
2 weeks Gradual Change
Gradual Change
1-1.2 No Change
1 month 1-2.4 5-19
2 months 9-14 28-42 0.1-2.9 Gradual Change
11.5 mU/ml
6 months 70-86 0.1-1.3 18.8 mU/ml

Fetal Marrow Development
Primitive megaloblastic blood formationstarts at 18th day - recurs with
illness

Kleihauer-Betke Smear
Adult (Maternal) RBC
Fetal type RBC
Acid removes adult hemoglobin, but not fetal hemoglobin

Megaloblastic Condition
Primary cause: results from inhibition of DNA synthesis in red blood cell production B12 and/ or Folate deficiency Pernicious Anemia
Hematological findings Increased MCV Multi-segmented Neutrophils Howell-Jolly bodies

Megaloblastic Disease
Pre-Leukemia: Myelodysplastic Disease – Elevated MCV
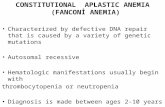
Fanconi Anemia People with FA may also have physical findings, which are highly
variable, and may include short stature, upper limb differences, kidney, cardiac, and gastrointestinal problems, brown-pigmented spots on the skin, hearing loss, and developmental delay.

Fetal Marrow Development
Normoblastic = 90% @ 10th week Liver is 1o site from 3rd-6th month Marrow is 1o site from 6th month Myeloid development starts ~4th
month Blood is rich in progenitors –
Cord blood transplants

Human Hemoglobins

Hgb Chain Production
Gestational Age 0 3 6 Birth 3
ß- Adultγ- Fetal (high O2 affinity)
є- Embryonic
ά- Adult

Fetal Hemoglobin
Oxygenated placental bloodOxygenated placental blood
Lower extremity bloodLower extremity blood
Fetal Brain PerfusionFetal Brain Perfusion

Fetal Circulation
Prenatal Fetal Circulation Video Postnatal

Severe anemia - Parvovirus

O2O2
Blood VesselBlood Vessel
Vascular WallVascular Wall
Cardiac Compensation to HypoxiaCardiac Compensation to Hypoxia
Hypoxia: Damaged RBC; Less RBC; Less Oxygen Delivery

High Output Heart Failure Cardiac Output = SV X HR Hypoxia requires increased
cardiac output HR increases first SV increases by Starling’s LawIntravascular
VolumeIntravascular
Volume
ContractilityContractility
Better Worse

Pleural EffusionPleural EffusionNormal LungNormal Lung
CardiomegalyCardiomegaly
Hydrops Fetalis RadiographHydrops Fetalis Radiograph

Infant with Hydrops FetalisInfant with Hydrops Fetalis

Malignancy until proven otherwise after first week of life
Leukoerythroblastic Blood Smear

“Unusual” Definition of Normal
Possible Sepsis Day of Birth: WBC 30K Next Day: WBC 34 K Peripheral Smear:
Leukoerythroblastic
Dx: Normal

Newborn Iron Acquisition
Physiology Review Fetus rapidly accumulates Hgb & Fe
Newborn will have normal Hgb & ferritin even if mother has mild-moderate iron deficiency - May cause of prematurity, LBW
Fe content at birth = ~ 75 mg/kg Varies with cord clamping technique Fe deficiency rare before 4 mos of age Neither human nor cow’s milk has iron Fe absorption better with human (lactoferrin)

Umbilical Cord Management
Placental vessels contain 75-125 ml of blood, ~ 25-30% fetal blood volume
Umbilical arteries constrict after birth Umbilical veins remain open gravity
flow Vaginal birth: ~ ½ placental volume
transfused 1 minute C-Section: keep infant below placenta
20 seconds prior to clamping the cord

Postnatal Erythropoiesis
RBC production 10X during 1st week Mechanism unknown -- EPO level = 0 Increases from wk 2 - 3 months Consequence = “physiologic anemia” Marked increase from 4 mos - 12 mos
due to body mass growth

Normal Infant Hgb Values
Lower Normal - TermLower Normal - Term
Lower Normal - PretermLower Normal - Preterm

RBC-Related Conditions of the Infant
Fetal Blood Loss (rare) Jaundice (very common) Newborn Immune Hemolysis (occasional) Congenital RBC Aplasia (rare)

Fetal-Maternal Blood Loss
Occurs through the placenta Causes: trauma, iatrogenic, idiopathic Cause of fetal death if >20% fetal
blood volume is lost Dx: Test maternal blood for fetal cells
Kleihauer-Betke Smear

Fetal-Fetal Blood Loss
Occurs in 70% of identical twins Significant if Hgb > 5 g/dl Chronic –
weight > 20% of larger twin Donor: SGA
Acute – weight < 20% of larger twin Donor: volume & rbc depleted

Fetal-Placental Loss
Placental Accidents Abruption Previa Multilobar placenta Rupture of a cord aneurysm Iatrogenic during C-section

Jaundice in the Newborn Fundamentals of physiology
Bilirubin produced by rbc breakdown Newborn liver conjugates poorly Lab: T/D Direct bili = conjugated Indirect bili = unconjugated
Common: indirect bilirubin (1/0.2) Physiologic; breast milk; rbc destruction;
Uncommon: direct bilirubin Cholestasis (abnormal ducts; sepsis;
mass)

Potential Consequences
Bilirubin toxicity Kernicterus –
deafness, retardation Caused by staining of basal ganglia
Risk level: > 20 if hemolysis

Jaundice Evaluation
Clinical – sick vs. well / normal color vs. orange

Jaundice Evaluation - Continued Examination for hepatomegaly Labs :
Bili T/D ?Hemolysis - SGOT, SGPT, LDH, Retic, CO-Hgb Maternal ABO Liver Function Studies



Management
Hydration Phototherapy
Isomerize unconjugated bilirubin
Degrades bilirubin to biliverdin
Exchange transfusion


Newborn Isoimmune Hemolysis - Rh
Anti-D (Rh) Setup -
mother Rh-, IgG Antibody + infant is Rh+
Mechanism – Maternal anti-D IgG crosses placenta, binds
fetal rbcs, fetal macrophages destroy rbcs Consequences –
jaundice, anemia, CHF
Rh-Rh-
Rh+Rh+
Maternal Anti-DMaternal Anti-D
MotherMother
BabyBaby

Prevention and Treatment
Prevention Administer Rhogam (IM anti-D antibody) at
28 weeks & at delivery Treatment (anti-D + mother)
Follow anti-D levels Amniocentesis (bilirubin) Fetal ultrasound – scalp edema
transfusion Infant – Exchange transfusions

Isoimmune Hemolysis - ABO
ABO Incompatibility Setup:
mother type O Mechanism:
Same Antibody is usually anti-A isohemaglutinnin
Infant: Jaundice before anemia Spherocytes – rbc membrane destruction
O +/-O +/-
A+ A+
Anti A & BAnti A & B
MotherMother
BabyBaby

Congenital Hypoplastic Anemia
Blackfan-Diamond Anemia Fault in one of the early steps of red
blood cell production 25% have a gene called RPS19
(short for 'small ribosomal protein 19') Symptoms
Fatigue, pallor, “open mouth” facies, protruding scapulae,web neck, cardiac abnormalities

Congenital Hypoplastic Anemia Dx:
Infantile normochromic, macrocytic anemia Reticulocytopenia Normocellular marrow with deficiency of rbc
precursors Nl or sl wbc Nl or sl platelets
Rx: Transfusions, steroids, marrow transplant

Common Anemias - Children & Adolescents
Iron Deficiency Lead poisoning Destructive Anemias

All Ages Anemia Definition Numerical -- Reduction in Hgb Level
> 2 S.D. Below the Population Mean
10
11
12
13
14
15
0.5-4yrs
5-7yrs
8-11yrs
12-14yrs
15-17yrs
18-50yrs
Hgb-Female
Hgb-Male

Clinical Definition
Generic Multisystem failure; Global CNS
depression Infants
Poor Feeding; Tachypnea; Apnea; Irritability
Children Poor Growth; Learning difficulties; Fatigue
Teens Headache; Fatigue; Poor school and
athletic performance
Tissue O2

Reasons for Investigating
General Health -- Sxs: Fatigue, headache, cardiac
failure Sign of Underlying Illness
Malnutrition; Lead poisoning; Marrow disease; Hypothyroid
Genetic Counseling

Evaluating an Anemia
Destruction Production Loss
Immune
Not Immune
GI
Marrow Disease
Marrow Invasion

Increased Destruction
Immune Not Immune
ABO
Rh
AIHA
EBV
SLE
Intrinsic Extrinsic
Enzyme
Membrane
HGB
DIC & Sepsis
Burns & Heat
Toxins
Heart Valve

Decreased Production
Marrow Disease Marrow Invasion
Nutritional Iron; Copper; FolateMetabolic Thyroid; B-12;Failure Aplastic Anemia Myelodysplasia InfectionCongenital Fanconi; BFD
Malignant Leukemia Neuroblastoma Lymphoma Solid TumorNon-Malignant Histiocytosis Storage Disease

Anemia Toolkit
First Step – History, family history, ROS Labs:
CBC – define anemia; rbc morphology; Retic – Helps with RBC destruction/production RBC Destruction – LDH, ALT(normal),AST( ),
CO, Haptoglobin ( in intravascular hemolysis) Urtinalysis – Hematuria Detailed tests then based on mechanism/sxs

Iron Deficiency
Physical Performance & Growth Restless Leg Syndrome Weakness, Dyspnea, Sexual dysfunctions Headaches
Intellectual Performance & Growth Attention Deficit Disorder, Cognitive or behavioral
dysfunction, fatigue, depression GI: pica, anorexia, headache, burning tongue, Endocrine: increased menstrual blood Immune: Increased severity of infections Skin: pruritis, paresthesias, pallor

Glossitis

Angular Chelitis

Koilonychia

Stages of Iron Deficiency
1. Decreased stores ( ferritin)2. Transferrin saturation3. Morphologic Changes
1. Anisocytosis2. Normochromic, normocytic anemia3. Hgb, MCV, MCHC; thrombocytosis
4. Bone marrow depletion

Causes
Blood loss GI: Cow’s milk in infants, Celiac disease Menses: 20% teenage girls are deficient Respiratory loss is rare
Dietary Nursing: 1 mg/kg/day required for term
infants starting at 4 months of age Children who drink a lot of milk Age 1-2 years; Female 14-30; Pregnancy; Males > 12 are OK (low requirement;
carnivorous)

Laboratory Dx
CBC terminology Peripheral Smear Iron Studies

Normal Blood Smear

Iron Deficiency Smear

Iron Studies
IronIron
IronVaries
TIBC NL
TIBC TIBC Varies
Normal Fe Deficient Chronic Disease
•Iron
•TIBC (transferrin)•Ferritin
Normal Fe Deficient ??? Chronic disease

Serum Ferritin
Generally correlates with iron stores Nl ferritin @ 6 mos-15 years lower than
other ages Taking Fe increases ferritin Normal Ferritin
Newborn: 25-200 ng/ml or SI units 1st month: 200-600 2-5 months: 50-200 > 5 months: 7-140 Adult Male: 20-250 Adult female: 10-120

Soluble Transferrin Receptor

Using TF Receptor
The concentration of cell surface transferrin receptor is regulated according to the internal iron content of the cell and its iron requirements.
Iron-deficient cells contain increased numbers of receptors, while receptor numbers are downregulated in iron-replete cells
Reference intervals: 3.5– 8.5 mg/L

Diagnoses with TR
Serum concentrations of transferrin receptor increase in iron-deficiency anemia
Transferrin receptor concentrations do not increase in anemia secondary to inflammatory disorders

Treatment
Iron replacement 3mg/kg elemental Fe daily X 3 months Poor compliance is main reason for failure Retics increase after 3 days; Hgb by 1
week GI absorptive defect very rare -
use intravenous Fe (not IM) Transfusion needed only if anemia is
hemodynamically very significant

Lead Poisoning
• Physiology – Absorbed like iron from air, paint, dirt, dust– Inhibits 1st and last steps in Hgb production– -ala and EPP basal ganglia damage– Disrupt CNS heme synthesis

Sources
Homes built before 1960 Ongoing home renovation Lead in water pipes Nearby industry Old furniture, toys, art supplies

Acute Neurological: hyperactivity or lethargy; increased
sleep; ataxia; coma, seizures, respiratory arrest Renal: Fanconi nephropathy
Chronic Neurological: behavioral changes, peripheral
neuropathy with pain & weakness of extensors, deteriorating cognitive function - even with mildly elevated Lead levels of ~ 20 mcg/dl
GI: abdominal pain, vomiting, malaise, constipation
Skeletal: Lead lines
Symptoms

Diagnosis
Increased serum lead level (veinipuncture)
CBC with microcytosis and basophilic stippling
X-ray: dense metaphyseal bands

Basophilic Stippling

Dense Metaphyseal Bands

Treatment
Asymptomatic: level 20-44 - consider chelation Level 45-69 - urgent chelation Level > 70 - emergency chelation
Symptomatic children require immediate supportive care and aggressive chelation
Identify the Source of Lead Quarantine the house Follow-up closely The state of Maine will help with all of this

Anemia of Increased Destruction
Intrinsic Hemoglobin disorders
Hgb SS Thalassemia
Membrane HS -- Stiff membrane
Metabolic PK
Extrinsic Autoimmune, mechanical, DIC

Laboratory Findings
Heme: retics; anemia; abnl smear Chem: LDH, AST (SGPT); haptoglobin Urine: Hgb (vs. myoglobin)

Sickle Cell Anemia
Pathophysiology Clinical
Autosplenectomy & OPSI Acute splenic sequestration Aplastic Crisis Vaso-occlusive crisis Stroke Endocrinopathies

Pain with Sickle Cell Disease
The most common symptom is pain Pain crises –people go to the emergency room
to get treated Pains seem to come from the bones, usually in the
arms, hands, legs, feet, or back acute chest syndrome Some have been accused of being addicted to pain
meds Prevention – avoid dehydration, excess exercise Rx – pain meds; hydration; steroids

-Thalassemia
1o problem is ineffective hematopoiesis -thal trait
Asymptomatic Low MCV, +/- mild anemia
-thal major Severe disease-some recommend BMT Severe anemia (hgb ~ 5) Progressive Fe overload causes morbidity &
mortality - cardiac, endocrine, liver Rx: Support; BMT

Hereditary Sphereocytosis
Defective membrane (stiff) Intrasplenic hemolysis Clinical
Varying degrees of severity Aplastic crises Anemia Increased MCHC Cholelithiasis WHY? Folate deficiency

Blood SmearSpherocytes

Osmotic Fragility
[NaCl] % Lysis % Lysis
1.0% NS (plasma) 0 0
.75% NS 10 20
.50% NS 30 60
.25% NS 70 90
.00% NS (water) 100100
•Normal •HS


Management
Follow infant Hgb & bilirubin closely Follow reticulocyte counts when well Follow growth & “wellness” Folic acid supplementation Rx aplastic crises with patience and
transfusion or steroids if necessary Splenectomy based on clinical course
Case Studies EndCase Studies End

Spherocytosis Case
7 year old boy, + OF and family history Taking folic acid daily 2 years of difficulty keeping up with
peers Retics ~ 15%, Hgb 9 mg/dl PE: Thin, short; spleen 8 cm below LCM


What needs to be done?
New labs show normal thyroid, celiac, growth hormone.
Options?……

Childhood Hemolytic Anemia
Autoimmune - antibody mediated Idiopathic Drug-Induced Disease-related
Infections - Viral (EBV, HIV), mycoplasma Autoimmune - SLE, RA, Thyroid, UC Immunodeficiency - all of them Cancer - Hodgkin’s, ALL, NHL, etc.

Clinical Course
Age usually < 4 yrs Acute onset - rapid Hgb fall 0-4 days Course can be acute (3-6 mos) or
chronic Mortality 9-19% Clinical: pallor, jaundice, dark urine,
fever, abdominal pain, hepatosplenomegaly, CHF

Diagnosis
Evidence of hemolysis Blood Smear: spherocytes; retics DAT - Direct antibody test
Macro (> 1000 IgG molecules/rbc) Micro (detects > 100 molecules/rbc)

Treatment
Observation Corticosteroids Intravenous Immunoglobulin (IVIG) Transfusion -- need a good lab Exchange transfusion - severe CHF Plasmapheresis Splenectomy Rituximab: anti-CD20 (new & cool)

Mechanical Destruction
DIC Sepsis, coagulopathy, tissue necrosis
Thermal burns, heatstroke
Infection Hardware
heart valve, thrombosed CVL Surgery - cardiac

Case Studies

Case 1 12 hr old black male term infant with jaundice Mother is 25 yrs. Old, G2P1001, O-, serology
-, uncomplicated pregnancy, received Rhogam @ 28 weeks
Infant is clinically well, has not voided or stooled
Labs: Bilirubin 16/0.5 CBC: WBC 21,000 60p/5b/27lymphs Hgb 16/ Hct 50; Platelets 165 K Peripheral Smear Type & Coombs: A+; DAT +; IAT + (anti-A)

Blood Smear

Case 2
5 yr old white male with a 4 mo. hx of irritability and inattention at school
Social hx: Lives with parents and 2 siblings in an old apartment that is under repair.
Family hx: “We all fed our babies whole milk, and nobody ever had a problem!”
Past hx: mild developmental delay. PE: hyperactivity; pale conjunctivae;
hyperreflexia;

Case 2 Labs
CBC-WBC 9,000, normal differentialHgb 9.0/Hct 27, MCV 72, Platelets 220 KSmear
Retics: 1%Lead: 21 mcg/dlFerritin: 5Fe low; TIBC elevated

High Power
Low Power

A Different Scenario
PE: grade II systolic murmur; no CHF Hgb: 4.9 MCV: 63 Retics: 0.5% WBC 6000, 10 polys, 90 lymphs Platelets: 1,300,000

Management Options
Dx: Fe Deficiency
Consider Hospitalization
Rx: Fe, 3-6 mg/kg/day
Folate, 1 mg/day
Retic in 3 Day Hgb in 1 Week
? Transfusion Continue Fe & Folate X 3 mos

Case 8
3 year old child presents for WCC. Parents note 2 months of increasing pallor & fatigue. No medical care since 4 months of age. Several recent colds.
Both parents are of Italian descent. Apartment is 80 years old & under repair.
PE: slightly pale. No dysmorphic features. Grade III SEM, no gallop. Liver down 2 cm.

Case 8 Labs CBC:
WBC 8,000 40 polys, 60 lymphs Hgb 3.8 Hct 11.9 MCV 80 Platelets 190 K Smear Retics: 0.5% Lead: 15 mcg/dl Ferritin: 50 Hgb Electrophoresis: A1= 97%; A2= 2%;
F=1% Bone marrow: decreased rbc precursors

Another Scenario
CBC- WBC 8,000 with a normal differential Hgb 3.8 Hct 11.9 MCV 100 Platelets 400,000 Smear: 2+ polychromasia, 1+ nrbcs Retics: 5% Bone marrow: increased RBC
precursors

Case 12 CC: 4 yr. old girl, 1 week of pallor & jaundice HX: Started with fever, malaise, congestion Progressive pallor, fatigue, abdominal
pain PE: Vitals: HR 130; RR 27; obvious pallor HEENT: Scleral icterus Cardiac: Grade II systolic murmur Abdomen: Spleen 5 cm below RCM

More History
Neonatal jaundice Transfused once in infancy Several similar episodes in past

Family History
Mother “always” anemic Mother and her sister with
cholecystectomy in early 20’s Mother’s Father had splenectomy “many
years ago”

Lab Tests
Hgb: 5.5 gm/dl MCHC: 32 Retic: 0.1% WBC & Platelets: Normal Coombs: Negative Smear

Break Time!
Grazing Horse, Freeport

Bilirubin MetabolismBilirubin Metabolism
Intravascular
Extravascular
Free Hgb+
Haptoglobin
Fe + Transferrin
Free Hgb
Red cells contain SGOT
& LDH
All Fe is recycled

The CBC - Definitions
WBC : Total leukocytes per mm3
ANC: Total # neutrophils per mm3
Hgb: Grams Hgb/dl Hct: % rbcs in a spun tube of blood MCV: mean rbc volume MCHC: mean Hgb concentration Platelets: # per MPV: mean platelet volume
Spun Capillary Tube

Blood Smear
Normal