Ekg
-
Upload
cristina-nechifor -
Category
Documents
-
view
25 -
download
1
description
Transcript of Ekg
Introduction to the 12 Lead EKG12 Leads are Universal in Their Placement:Lead I aVR V1 V4 Lead II aVL V2 V5 Lead III aVF V3 V6 Three Principles to Learn: When a wave of depolarization moves toward a + electrode of any lead, an upright wave is inscribed. When a wave of depolarization moves away from a + electrode of any lead, a negative wave is inscribed. When depolarization moves perpendicular to the + electrode of any lead, either a biphasic or line will be inscribed. Review: Conduction Systems of the Heart SA Node:Initiates a normal rhythmic electrical activity. Wave of depolarization moves through the atria. The SA node is very small and its electrical activity is not seen on the ECG. A P wave is seen when the atria depolarize. AV Node:Delays electrical activity before it proceeds into the ventricles. This normal delay allows time for the atria to depolarize when the ventricles are still in diastole. Junctional Bundle:Conducts impulse from atria into the ventricles. Electrical impulse travels into ventricular conduction system via the Junctional bundle and down the bundle branches. Purkinje fibersenter the myocardial cells and conduct the electrical impulses throughout the ventricles. QRS Complex (Normally <.12 seconds) First wave of complex is negative/below isoelectric line and called a q wave. Must be first wave of complex and must be negative and small. Amplitude (normal q wave) is less than one fourth height of its R-wave. R waveis always positive (above isoelectric line). No such thing as a "negative R-wave". S waveis a negative deflection following the R wave. T waverepresents ventricular repolarization. Normal T waves are in the same direction as their complex. Normal T wave is asymmetrical and it peaks toward the end, instead of the middle. Normal T: in frontal plan <= 5mm, in precordial plane <= 10mm tall. ST Segmentis measured from the end of complex to the beginning of T wave.ST is the beginning of ventricular repolarization. Normal STis on the isoelectric line or no more than 1mm above or below isoelectric line. Elevated STis more than 1mm above isoelectric line. Depressed STis more than 1 mm below isoelectric line. PRI (normal PRI 0.12 - .20 seconds)Normal PRI is measured from beginning of the P to the beginning of the complex. This measurement represents the time it takes for a wave of depolarization to spread through the atria, AV node, and AV junction.Paper and VoltageEach small box on the horizontal line represents 0.04 seconds. Each large box on the horizontal line represents 0.20 seconds. There are five small boxes in one large box. Each small box on the vertical line equals 0.1 millivolts. 10 small boxes = 10 mm tall. Leads, Lead Placement, Precordial LeadsThe activity of the heart produces electrical potentials, which can be measured on the surface of the body. Lead I, II, III:The three limb leads are placed across the heart. The heart,
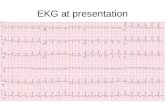
an electrical source, is the center for Einthoven's Triangle: forming a triaxial reference system. The frontal leads are augmented vector leads: leads that reflect the potentials of the right arm, left arm, and left leg are called VR, VL, aVR, AVL, and aVF. Precordial leads Surface view of leads Coronary Artery Distribution Right coronary artery: supplies right heart, in the ventricle it supplies inferior surface, 2/3 posterior and part of the left lateral wall. Left coronary arterybifurcates into two main branches: Left circumflex (LCX):supplies lateral wall of the left ventricle and part of the posterior wall. Left anterior descending coronary (LAD):supplies anterior wall of the left ventricle, the intraventricular septum, part of the lateral wall of the left ventricle - referred to as the "sudden death artery". Review of the Leads Inferior Leads RCA supplies the inferior wall of the ventricle. MI's involving inferior surface of the heart will be seen in leads II, III, and aVF. Lateral Leads Leads I, aVL, V5, V6. Lateral infarctions are usually associated with obstruction of the left circumflex artery. Septum and Anterior Leads Intraventricular septum - leads V1 and V2. Anterior Wall - V2, V3, V4. Anterior infarctions are usually associated with occlusion of the left anterior descending branch of the left coronary artery. Myocardial ischemia, injury, and acute infarction The three EKG changes are: elevated ST segments. inverted T waves. pathological Q abes. Elevated ST segments (myocardial injury) Normal ST segments are in the isoelectric line or no more than 1mm above or below it. An abnormal electrical charge is produced on membrane of myocardial cell resulting in abnormal current flow causing an elevation of ST segment. Myocardial injury causes elevation of ST segments over affected area of the ventricle. ST segments changes are the earliest indication on EKG. ST segment changes occur within a few hours or a few days and should return to the isoelectric line within 2 weeks. Inverted T waves (myocardial ischemia) Myocardial ischemia causes symmetrical inversion of the T wave. T wave abnormalities reflect a change in ventricular repolarization. As the ST segment begins to return to the isoelectric line, the symmetrical inversion of the T wave appears. The T wave will become progressively deeper as the ST segment returns to the isoelectric line. Pathological Q waves (myocardial infarction) Normal Q waves are small, less than 1 mm deep or wide and one fourth the height of their R wave.
Pathological Q waves usually develop when ST segments are elevated and appear several hours or days after the clinical manifestations of the MI. Abnormal Q must be one small square (0.04 sec) wide and greater than one-third of QRS height in Lead III. Myocardial infarction causes pathological Q waves over the affected area of the ventricle. The age of the infarction can be determined. Q waves only - old infarction Q waves with elevated ST segments (with or without T wave inversion) - acute infarction Q waves with inverted T waves - age undetermined. Acute Infarction on EKG Transmural MI- involves the full thickness of myocardium Nontransmural MI- does not involve the full thickness of myocardium. Also called subendocardial. Changes occur in ST-T wave. EKG changes in transmural MI occur both in depolarization -q wave and repolarization -ST-T. Four phases of acute MI on EKG: hyperacute phase- ST elevation and upright T waves. Occurs in first few hours and lasts 1-6 weeks. ST elevation beyond 6 weeks - suspect ventricular aneurysm. fully evolved phase- after hours or days. Deep T waves and appearance of diagnostic q waves. resolution phase- T waves return to normal within weeks to months. stabilized chronic phase- q waves remain permanent Bibliography Goldberger AL, Golderber E: Clinical Electrocardiography: simplified approach, ed 5, Chicago, 1994, Mosby. Norman, Ann E: 12 Lead Interpretation: a self teaching manual, St. Louis, 1992, McGraw-Hill, Inc. Return to Healthcare Providers Page Return to ACG Home Page ©1995, The Atlanta Cardiology Group, P.C. All rights reserved. 5665 Peachtree Dunwoody Rd Atlanta, Georgia 30342 404-851-5400