report Hepatic haemodynamics as through spleen, …Gut: first published as 10.1136/gut.30.2.265 on 1...
Transcript of report Hepatic haemodynamics as through spleen, …Gut: first published as 10.1136/gut.30.2.265 on 1...

Gut, 1989, 30, 265-278
Progress report
Hepatic haemodynamics as related toblood flow through gut, spleen, andpancreas
Current work fails to provide a true picture of hepatic haemodynamicsbecause the liver is studied as an isolated organ when in fact it is the onlyorgan in our body which depends for 80% of its blood supply from otherorgan systems, which include the gut, the spleen, and the pancreas. In spiteof this, studies on hepatic haemodynamics rarely include the behaviour ofthe splanchnic circulation.Westabyl summarised the status of the present approach to the study of
hepatic haemodynamics including its limits and disadvantages in man and inanimal models: 'In man, an estimate of total liver blood flow can be made bythe indocyanine green (ICG) infusion method although this is unreliable inthe presence of severe liver disease (and hence poor extraction. UltrasoundDoppler measurements represent a non-invasive method of measuringportal blood flow but the reproducibility of the measurements needs to beconfirmed. Animal models can overcome these difficulties and have beenthe basis ofsome of the most innovative work. The extent to which data fromsuch animal models can be extrapolated to man remains unclear.The search for drugs that alter hepatic haemodynamics continues,
although this is frequently no more than a procession of measurements ofthe portal pressure gradient (wedged hepatic venous pressure/free hepaticvenous pressure (WHVP-FHVP)) in reponse to vasoactive drugs withoutany clear understanding of the significance of the findings.' Moreover, themeasurement of hepatic blood flow is difficult - for example, Nxumalo et al2showed that the ICG method may overestimate the hepatic blood flow by 40to 60% compared with the electromagnetic flowmetry.
These critical comments emphasise the unsatisfactory position of hepatichaemodynamic studies at the present time. Westaby, however, failed toindicate the variables which are required for an ideal evaluation of hepatichaemodynamics.
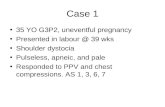
Table Variables to be monitored when studying liver haemodynamics
1 ECG, heart rate 10 Pancreatic branch of splenic artery2 Arterial pressure 11 Left gastric artery3 Portal pressure 12 Proper splenic artery4 Hepatic vein pressure 13 Superior mesenteric artery
14 Inferior mesenteric arteryFlow 15 Splenic vein5 Ascenting aorta 16 Portal vein6 Common hepatic artery 17a Inferior caval vein proximal to hepatic vein7 Gastro-duodenal artery b Inferior caval vein distal to hepatic vein8 Superior pancreatico-duodenal artery 17a-17b=hepatic vein flow9 Inferior pancreatico-duodenal artery
265
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Charbon andAnderson
In this survey we argue that a combined consideration of hepatic andsplanchnic circulations (Table) is required to depict hepatic haemodynamicsaccurately. In addition we discuss briefly some aspects of the changes insplanchnic vessels and metabolism that are important to hepatic function.The argument is supported by data from the literature and also from studieswhich are being conducted on anaesthetised and conscious dogs in ourlaboratories.
In the anaesthetised animals we measured blood flow using an electro-magnetic flowmeter (EMF) with an eight channel system at organ level onarteries with an external diameter equal to or greater than 0O5 mm. Arterialpressure was assessed with a catheter-tip manometer (Millar), peripheralvenous and portal venous pressure were measured with an open tip catheterconnected to an electromanometer. Heart rate was assessed from theR-R interval of the ECG limb leads. The method has been described indetail.34
In the conscious dogs, blood flow was measured using an eight gate,implanted, pulsed Doppler ultrasonic flowmeter (PDUF). The transducerassemblies were held in a circumferential cuff placed around the portal veinand the hepatic artery and connected by flexible cables to the signalprocessing and transmitter modules. The PDUF allows the measurement ofmultiple acute or chronic changes in blood flow in the hepatic artery andportal vein. Flow has been measured over long periods of up to two years.Such longterm measurements have confronted the investigators with a fargreater variability in portal flow than would be expected from the acutespanchnic measurements in anaesthetised dogs.5 The causes of this vari-ability are discussed below in the paragraph on main variables establishinghepatic perfusion. The system has been described in detail.S9
General haemodynamic and morphological considerations
Some general haemodynamic points as well as possible mechanisms of thevasoactivity of drugs will be discussed before the details of splanchnic andhepatic perfusion are considered.
MICROVASCULAR RESISTANCE AND CONDUCTANCEFlow through an organ depends on its vascular resistance and the pressuregradient across the organ. Resistance cannot be measured directly and mustbe calculated from flow and pressure measurements. In general outputvenous pressure and its changes are negligible compared with input arterialpressure (about 100 mmHg). But this is not so for the liver where the outputhepatic vein pressure is only a little lower than the input portal pressure(about 7 mmHg). Vascular resistance (R) is the quotient of mean arterialpressure (P) and mean macroscopical arterial flow (Q), even though theactual resistive vessels are the small arterioles (diameter appr 30 Fm)[R=P/Q]. According to Ohm's Law, the inverse of total peripheral vascularresistance is the sum of the reciprocals of individual vascular resistances. Forpractical reasons, simplifying the computation, conductance (g=Q/P) isoften used instead of resistance. Then, total vascular conductance is the sumof the local vascular conductances. The use of conductance has anotheradvantage, at a steady arterial pressure conductance and flow are directlyproportional.
266
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 267
1 n 1
RT i=1 RL,i
1
R
n
gT = LgL,ii=l
in whichRT = total peripheral resistance;n =number of vessels;RL = local peripheral resistance;gT =total peripheral conductance;gL =local peripheral conductance.
In these equations we have neglected the influence of vascular compliancewhich has a relatively small influence at organ level.
MECHANISMS OF VASOACTIVITYIn this section we address several questions. How do vasodilator drugs orendogenous compounds reduce microvascular resistance? Is arteriolar tonereduced by a direct action on smooth muscle or induces the agent primarilyto the target cells - for example, secretin on ductal cells in the pancreas - torelease a vasoactive metabolite which reaches the local arteriolar wall bydiffusion? If a vasodilator compound acts both directly on smooth muscleand on target cells, would the dose dependency for the two effects besimilar? The morphology of arterioles in different organs shows littlevariation. In contrast, the functional activity of organs varies a great deal. Ifa vasoactive compound acts directly on the microvascular wall, why wouldthe vasodilatation only occur in the target organ regardless of the similarityof the arteriolar morphology in various vascular beds. What does a similarmorphology tell us about the uniformity of receptor populations?
If, on the other hand, the vasoactivity is caused by the release of ametabolite from target cells, then the concentration of that metabolite maybe just sufficient to cause a local vasodilation through diffusion. Concentra-tion of the metabolite would be diluted in the venous outflow to exclude asystemic response. These fundamental questions have been discussed moreextensively elsewhere.'0
POWERThe arterial pressure is determined by the kinetic power output by the leftventricle (LV) and total peripheral resistance (TPR). These parameterscannot be measured directly. They must be calculated from the measuredleft ventricular volume output at the ascending aorta ('cardiac output',neglecting in practice coronary arterial flow) and ascending aortic pressure.Kinetic power output is calculated as the instantaneous product of ascendingaortic pressure [Table, no 2] and ascending aortic flow [Table, no 4]. Totalperipheral is the quotient of the mean ascending aortic pressure over meanascending aortic flow.
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Charbon andAnderson
The power output of the LV can be modified by noradrenaline (NA).Noradrenaline steeply enhances LV power output and constricts thearterioles in the small intestine. This rise of LV power output augmentssuperior mesenteric artery flow, particularly during systole, by increasingarterial pressure. This effect is displayed in a striking manner when theamount of kinetic energy dissipated in this vascular bed is plotted as ananalog signal.10The influence of LV power output on peripheral perfusion becomes
evident when the vascular effects of NA alone and after a 1I3-adrenergicblocking agent are compared. The NA-induced change ofLV activity can beprevented by a 13l-adrenergic blocking agent without impeding the vasocon-strictive potency of the catecholamine. When NA is given after the blockingagent, dips of systolic flow in the superior mesenteric artery appear inaddition to the steep reduction of its diastolic flow.'0
In a study of portal flow the influence of changing LV function [Table, no1, 2, 4] on mesenteric perfusion must be considered. Moreover, changes inmesenteric flow as a result of LV performance should be distinguishedfrom changes caused by altered local vascular conductance.
MORPHOLOGYIn the classic description of the vascular configuration of the liver, the'central vein' is the point of interest around which the other hepaticstructures are related forming the basic unit, the lobule. Blood flow iscentripetal in the lobule and blood runs from the periphery to the centralvein. No clear cut distinction is made between the contribution by thehepatic artery and by the portal vein."I 12
In 1966 this concept was changed by Rappaport et al,'3 who took thetriangle containing the terminal portal vein, the hepatic artery and the bileducts as the centre of a new unit, which they call acinus. In the acinus, bloodflow is centrifugal and the contributions from the hepatic artery and portalvein can be clearly distinguished. This concept enabled Rappaport todescribe the morphology and function of arterial flow blood in the liver ingreater detail""'6 and to separate the oxygen availability in the acinus intothree concentric zones of hepatocytes around the hepatic artery. Thesezones are related to local oxygen concentrations upon which the enzymesystems in the hepatocytes are dependent. This approach contrasts stronglywith the neglected role of the arterial blood supply until a decade ago. Forexample, in 1977, Motta'7 in a large and extensively illustrated review on thefine structure of the liver failed to present a single figure of the relationbetween the hepatic artery and its surrounding structures.
In the 1970's scanning electron microscopic studies emphasised the role ofthe arterial blood supply to the liver by visualising the peribiliary vascularplexus as well as the arterial branches draining directly into the hepaticsinusoids."23 Nevertheless, this plexus had been described 240 years ago byFerrein (1749), quoted by Andrews et al in 1949.24 Although McCuskey(1966)25 uses the lobule as the hepatic unit, his illustrations clearly show thestructural relationships between the hepatic artery sphincters, the portalvein branches and the sinusoid. He did, however, fail to describe theperibiliary plexus.The basic vascular unit of the liver is the 'acinus' and the use of the 'lobule'
is now obsolete.
268
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 269
Main variables establishing hepatic perfusion
PORTAL PRESSURE [Table, no 3]Because pressure in the portal vein is about 10 mmHg and in the hepatic veinnearly 3 mmHg, the pressure gradient for portal flow across the liver is onlyabout 7 mmHg, in contrast with the pressure gradient of about 100 mmHg inorgans supplied solely by arterial blood [Table, no 2].
If the portal inflow from the gut is steady, a rise of portal pressure of only2 mmHg implies a 29% rise of hepatic portal vascular resistance in the liverassuming pressure in the hepatic vein [Table, no 4] is stable. If the rise inportal pressure is accompanied by the development of collateral vessels - forexample, oesophageal varices, this implies - with a constant portal inflowfrom the gut - a reduction of portal vein flow notwithstanding the increasedportal pressure. Consequently the portal vascular resistance in the liverunder these circumstances is increased more than would be expected fromthe rise of portal pressure with constant portal inflow from the gut.
If, in contrast, portal inflow from the gut is reduced while the portalvascular resistance in the liver remains the same, portal pressure will tend todrop. The pressure gradient across the liver diminishes 14% for each mmHgbelow basal level thus reducing portal outflow through the liver. Thiscounteracts the fall of portal pressure secondary to the reduced inflow. But ifportal inflow from the gut is increased while the portal vascular resistance inthe liver remains the same, portal pressure will tend to rise. The pressuregradient across the liver is increased by 14% for each mmHg above basallevel, thus increasing portal outflow through the liver. This counteracts therise of portal pressure secondary to the increased inflow.
It is important to be aware of these relations particularly as Fioramontiand Bueno26 observed major changes in mesenteric perfusion parallel to themigrating myoelectric complexes activity. We have no information toindicate whether a change of portal pressure in itself alters hepatic arteryflow either directly through mechanical influence on arteriolar sphincters orindirectly through signals from autonomic sensors in the wall of the portalvein. On the other hand, we do know that a close anatomical and functionalrelationship exists between biochemical variables in the portal blood andhepatic arteriolar sphincter tone (see below; portal flow).Normal portal perfusion of the liver will follow changes of splanchnic
outflow rather smoothly but a change of resistance in the hepatic vasculaturemay greatly complicate this simple relationship.
PORTAL FLOW [Table, no 16]Portal blood flow comprises blood from the gut, the spleen and the pancreas.A number of complicating and conflicting results are encountered when weconsider the detailed vascular responses in these organs. For the purpose ofillustration, the vasoconstrictive effects of intravenous NA on the superiormesenteric artery will be used.'0 27 Even though portal flow is diminished by ahigh dose of NA, portal vein pressure may rise simultaneously, probablybecause ofcontraction of the portal capacitance vessels which is also inducedby NA.28 The reduction of flow in the superior mesenteric artery, however,contrasts strongly with the remarkable increase of splenic flow [Table, no12], implying splenic arteriolar vasodilation. Venous outflow from thespleen [Table, no 15] increases by a proportionally greater amount than
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Charbon andAnderson
arterial inflow. Apparently splenic arteriolar vasodilation and spleniccontraction occur simultaneously with small intestinal vasoconstriction.That the increased splenic contribution to portal flow is not an invariableconsequence of a reduced superior mesenteric artery outflow is confirmedby the effect of vasopressin which reduces both superior mesenteric outflow,and splenic flow with a similar dose dependency.29 30 Lebrec's suggestion3' toreplace vasopressin by a beta2-adrenergic blocking agent to reduce portalhypertension may therefore be attractive, at least on experimental grounds.On the one hand, vasopressin steeply reduces pancreatic blood flow while onthe other hand the pancreatic vessels do not respond to the beta2-agonist,insoprenaline32 and, therefore probably do not respond to a beta2-adrenergic antagonist. We should be aware, however, that the experimentalportal hypertension produced by portal vein stenosis and used by Braillon etal33 in Lebrec's group, is fundamentally different from the portal hyperten-sion in cirrhotics, particularly with regard to the degree of pressure in theportal inflow into the liver.The much smaller inferior mesenteric artery flow [Table, no 14] responds
in a similar way to NA. This increase of vascular resistance, however, isdifferent from that seen in the superior mesenteric artery, in that it is notprevented by the alphaadrenergic blocking agent, phenoxybenzamine.34A change in the superior mesenteric artery flow is not always proportional
to a change in portal vein flow. Such changes may at least be partiallycompensated for by the splenic outflow. Vasoconstriction induced by onedrug on two vascular beds may be based on stimulation (inhibition) of twodifferent receptor systems.Transcutaneous Doppler ultrasound can be used to detect blood velocity
in the abdominal vessels. Accurate estimates of blood flow using thistechnique are limited by several separate errors including those caused bythe difficulty of measuring precisely the angle of approach, the vessel crosssection area and the Doppler shift together with the question of theuniformity of scattering from the blood.35 The clinical use of the Dopplervelocity measurement encounters an additional pitfall. The primary interestis the - three-dimensional - volume of flow per unit of time, not only the -one-dimensional - flow velocity. This aspect was emphasised by Zoli et al,-who showed that portal flow velocity was a significant 35% lower incirrhotics than in controls, whereas the diameter of their portal vein was alsosignificantly 30% higher, resulting in a calculated blood flow that is incirrhotics on the average 6% greater than in controls (not significant). Theassumption that the portal vein has a circular cross section is not true. Noinformation was given on the resolution factor of the one-dimensionaldiameter measurement that is used to calculate the two-dimensional crosssection.
Extrapolation of the one-dimensional information from Doppler velocitymeasurements on portal flow to the three-dimensional volume of the flow iscrowded with pitfalls.
HEPATIC VASCULAR RESISTANCEWhen estimating change in hepatic vascular resistance total hepatic outflowshould be measured. Blood flow cannot be measured in the hepatic veinsdirectly because the veins are multiple and too short to allow the placementof a flow sensor. Total hepatic outflow therefore must be measured as the
270
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 271
difference between flow through the inferior vena cava proximal and distalto the hepatic veins [Table, nos 17a and 17b]. Hepatic venous outflowdepends on the portal and arterial inflow as well as the capacitance of thehepatic vessels. Note: (1) In a steady state hepatic outflow is the sum of theportal vein and arterial hepatic artery inflow; (2) The calculated hepaticvascular resistance is a combination of the arterial and the portal resistances;(3) arterial hepatic resistance is about 40 times greater than that of the portalsystem. (4) Contributions of biochemical variables in the hepatic outflowprovided by the proper hepatic arteries and by the portal vein cannot bemeasured separately.The difference in volume between portal inflow and hepatic outflow
caused by the contribution of the hepatic artery should be taken intoconsideration when the uptake or release of a biochemical compound fromthe liver is calculated. This also holds for calculations of biochemicalvariables in arterial hepatic flow. It is practically impossible to quantifyexactly the extraction (or addition) of a biochemical variable by eithercompartment (portal or arterial), as the outflow concentration in the hepaticveins is a mixture of the outflow concentrations of both compartments.
METABOLIC ASPECTThe contribution to the portal flow by a small branch of the coeliac arteryremains to be discussed. The left gastric artery [Table, no 11] supplies theparietal cells of the stomach and this vascular bed readily vasodilates afterpentagastrin which also increases blood flow in the common hepatic artery[Table, no 6] because of vasodilation in the gastroduodenal artery bed[Table, no 7]. This vasodilatation, however, appears to be restricted to thesuperior pancreaticoduodenal artery, supplying the duodenum and thepancreas. Pentagastrin also stimulates the enzyme secretion in thepancreas.'037 These data closely tie the haemodynamic response of penta-gastrin to the secretory response of acid produced by the stomach andenzymes by the pancreas.
This close relationship between blood perfusion and function leads to atopic of major importance. Up to now we have restricted the discussion toregulation of portal flow by the splanchnic bed without considering the effectof endogenous agents passing from the gut to the liver through the portalvein. These agents may be important to hepatic function. For example, thepancreas releases the hormones, insulin and glucagon, into the portal veindirectly to the liver which is the first organ to be passed by these twohormones which regulate the uptake and release of glucose by the liver.Small doses of lysine vasopressin, the hormone used clinically in the acutemanagement of portal hypertension, steeply reduce pancreatic perfusion[Table, nos 8, 9, 10] without altering arterial pressure. Vasopressin reducessecretin induced pancreatic secretion to a similar degree. Moreover thereare strong indications that vasopressin asphyxiates the pancreas,38 an effectwhich may imply modification of the release of insulin and/or glucagon bybasopressin. Finke and Seifert39 have extended these observations on thesplanchnic blood flow in anaesthetised dogs to vasoactive intestinal peptide(VIP), glucagon, secretin, and somatostatin. Gallavan et all have studied indetail the effect of digestion on hepatic blood flow in conscious dogs. Thespecific effects of single hormones have been studied by Beijer et al"4 forsecretin and by Blitz et al42 for VIP. Kvietys et al43 have discussed the
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Charbon andAnderson
discrepancies between vasoactive agents in relation to blood flow andoxygen uptake, comparing in vivo and in vitro data.A change in blood flow anywhere in the splanchnic system may indicate an
altered release of endogenous compounds including hormones; such analteration may produce selective changes in hepatic metabolism.
ARTERIAL HEPATIC FLOWTwenty per cent of hepatic blood flow is arterial and supplied by the properhepatic arteries which are multiple in the dog and individually too small toallow the direct measurement of their blood flow. Clearly, the arterial andportal systems are not linked by continuously open connections in the liverotherwise arterial blood would flood the portal system, raise portal pressureto arterial level and completely stem the venous outflow from the gut.
In their beautiful cinematographic studies Rappaport and Schneiderman'5visualised arteriolar sphincter like structures that permitted intermittentspurts of arterial blood to pass into the sinusoids of the liver. In this way, theproximal zone of hepatocytes in the acinus receives blood with a higheroxygen level than centrilobular hepatocytes in the distal zone. In addition,there is a fine arterial network around the bile canaliculi which emptiesdirectly into the terminal portal veins suggesting a special functionalrelationship between arterial blood and bile production.2"23
This functional relationship was noted by Kelly and Klopper'1 whoshowed that rabbits breathing room air had a P02 in bile of 83 mmHg, whichwas increased when hyperbaric oxygen was administered. Arterial P02 alsoincreased but not P02 in the portal vein. Andrews et all showed theimportance of studying hepatic artery extraction procedures studying theportal and arterial hepatic route separately and claimed a preferredextraction of BSP along the hepatic arterial route. This is at variance withBrauer's work' who failed to take into consideration the carryover effect ofusing both routes one after the other in the same animal. Andrews' datawere supported by Bradley47 who observed in man that a far greaterproportion of hepatic blood was cleared of BSP after a surgical formation ofa portocaval shunt. Data are, however, sparse, and insufficient informationis available to decide whether extraction by the liver of a particularcompound occurs along the portal, the arterial route, or both. Arterialhepatic blood flow can be obtained by subtracting gastroduodenal arterialflow from common hepatic arterial flow, neglecting the flow through the tinyright gastric artery [Table, nos 6, 7]. Evaluation of arterial hepatic flow fromthe common hepatic artery itself can be misleading as the following resultsshow.
Pentagastrin enhances flow in the common hepatic artery and in thegastroduodenal artery with a steal effect from the proper hepatic arteries.7Intravenous parathyroid hormone, on the other hand, causes an increase inthe common hepatic artery only and not in the gastroduodenal artery, sothat the increase in blood flow is purely from the arterial hepatic flow.48 Thedirect injection of parathyroid hormone into the portal vein also increasesarterial hepatic blood flow before recirculation takes place. This impliesa close relationship between portal flow and the arteriolar sphinctersdiscussed above, which prevents a continuous high pressure flow into theportal system.
Assessment of arterial hepatic flow requires simultaneous monitoring of
272
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 273
flow in the common hepatic and gastroduodenal arteries. The arterial bed inthe liver differs anatomically and functionally from the portal bed but thetwo are closely related. Arterial and portal perfusion should therefore beconsidered individually and preferably simultaneously.
RELATION BETWEEN PORTAL AND ARTERIAL HEPATIC FLOWThe physiological role of the hepatic artery has been thoroughly reviewed byGreenway and Stark49 and Rappaport and Schneiderman."5 The reciprocalrelationship of blood flow between the portal vein and the hepatic artery hasbeen a major source of controversy since it was first affirmed in the classicalstudies of Burton-Opitz.50The reciprocal relationship has been confirmed bymany investigators51-' and questioned by others.6263With careful experimental design, most investigators find that when
portal vein flow is decreased there is an increase in hepatic artery flow9Most strikingly, the reduction in portal vein flow after portocaval anastomo-sis is associated with a marked increase in hepatic artery blood flow."69Nevertheless, the increase in hepatic artery flow may not be quantitatively aslarge as the decrease in portal vein flow"9"57"7' possibly related to the higheroxygen content of the former.When, on the other hand, portal vein flow increases, the reciprocal
relationship of hepatic flow appears less impressive. After feeding there is amarked rise in portal vein flow in dogs.7' But Hopkinson and Schenk75found that one hour after a meal of meat though portal vein flow roseby 76% and total hepatic flow by 32%, hepatic artery flow remainedunchanged. In contrast Anderson and Mulroy78 observed after feeding anappreciable rise of portal vein and hepatic artery flow. The increase in portalvein flow after feeding can be traced to increased blood flow in the superiormesenteric artery.3777 Similarly, the administration of phenobarbital to ratsand rhesus monkeys produces a significant increase in portal vein flow due toa rise in splanchnic flow, whereas hepatic artery flow remains unchanged.78
In the preceding paragraphs it has been argued that portal flow essentiallyis the splanchnic outflow. If splanchnic flow diminishes, the liver cancompensate for it directly only through a rise of its arterial flow, or indirectlyby sending a neural or humoral signal to the splanchnic resistance vessels,and momentarily to the contractile tissue in the spleen. These control signalshave been extensively discussed by Richardson and Withrington.79 Thecapacitance function of the splanchnic venous bed was estimated at 27% oftotal blood volume by Greenway.8' So a change of splanchnic capacitancecan momentarily alter hepatic portal inflow to a great extent. As the arterialP02 level is higher than portal P02, a smaller volume of arterial supplementsuffices in this regard to compensate for a larger reduction of portal inflow.In contrast, the biochemical constituents of portal blood, like insulin andother hormones, which the liver may need, are often present at higher levelthan found in arterial blood.
Aspects of splanchnic and hepatic oxygen consumption as related to bloodperfusion have been discussed extensively.82"5 We know of only one author(Andreen') who distinguished elegantly between a major number ofvariables controlling splanchnic and hepatic perfusion and function. She hasstudied extensively the effects of inhalation and intravenous anaesthesia onhepatic and splanchnic circulations. But in most papers which discuss therelationship between portal and arterial hepatic perfusion, mechanical
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Charbon andAnderson
occlusion or operative deviation of one flow or the other is used. This isfundamentally different from the physiological and pathophysiologicalsituations seen in man except after a shunt operation. Normally changes arecaused by modifications of vascular resistance. This holds for the splanchnicflow and hypothetically for the arterial hepatic flow during digestion. Thenthe changes in blood flow are the result of the absorption of nutrients as wellas to protective metabolic transformations occurring within the liver. Inpathophysiology the most frequent increase of vascular resistance is seen inpatients with alcoholic cirrhosis of the liver.
Portal flow to the liver depends on the splanchnic flow. Splanchnic outflowcan change momentarily by alteration of the capacitance function of theportal vessels. A longer term change requires an alteration in splanchnicinflow, which varies with splanchnic vascular conductance and arterialpressure.The liver controls arterial hepatic flow directly through the hepatic
arterioles. Thus, the liver can compensate for a reduced arterial hepatic flowonly indirectly by modifying portal flow through humoral or nervous meansthat alter splanchnic outflow. Interactions between portal and arterialhepatic perfusion apparently do exist, but no completely clear picture hasyet emerged from the data in the literature and from our own work.
Conclusions
The liver receives 20% of its blood as arterial and 80% as portal flow. Itsvascular unit is the 'acinus'.
Assessment of arterial hepatic blood flow requires simultaneous monitor-ing of flow in the common hepatic and gastroduodenal arteries. The hepaticarterial bed differs anatomically and functionally from the hepatic portalbed. When attention is paid to arterial splanchnic flow in a study of portalflow, the influence of changing LV function on mesenteric perfusion shouldbe considered.The portal inflow to the liver depends on the splanchnic outflow. A
longterm change of portal flow requires an alteration in splanchnic inflow,which depends on splanchnic vascular conductance and on arterial pressure.In contrast, the liver can alter the arterial hepatic flow directly by adaptationof the hepatic arterioles.The healthy hepatic portal perfusion will follow changes of splanchnic
outflow rather smoothly, due to a low hepatic vascular resistance. A changeof resistance in the hepatic vasculature may greatly complicate this simplerelation.The difference in volume between portal inflow and hepatic outflow
should be taken into consideration when the uptake or release of abiochemical compound by the liver is calculated. The same holds for thecalculations on a biochemical variable in arterial hepatic flow. Thebiochemical variables in the outflow supplied by the proper hepatic arteriesand the outflow supplied by the portal vein cannot be assessed separately.A change in the superior mesenteric artery flow is not always representa-
tive of a change in the portal flow. It may, at least partly, be compensated forby the splenic outflow.The gastrointestinal tract supplies the liver not only with most of the
nutritional components absorbed from the gut, but it also offers hormones.
274
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 275
A change of blood flow anywhere in the splanchnic tract may indicate analtered release of endogenous compounds, which may alter hepatic meta-bolism selectively. Doppler velocity measurement on portal flow in man iscrowded with pitfalls.
Questions about liver perfusion require instantaneous and continuousinformation about blood perfusion through gut, spleen and pancreasassessed in situ and simultaneously. The only established method that is nowavailable for this purpose is multichannel electromagnetic flowmetry.87Confirmation of data obtained by the electromagnetic flowmetry onanaesthetised dogs can be sought in conscious animals using the implantedpulsed Doppler ultrasonic flowmetry.
G A CHARBON AND M F ANDERSONExperimental Laboratory for Peripheral Circulation,University Hospital, Utrecht, The Netherlands andDepartment ofRadiology, VA Medical Center,Fresno CA, USA.Address for correspondence: Dr M F Anderson, University of California, SanFrancisco/Fresno, Department of Radiology, Veterans Administration MedicalCenter, 2615 East Clinton Avenue, Fresno, California 93703, USA.
References
1 Westaby D. The pharmacological management of portal hypertension. Curr OpinionGastroenterology 1986; 2: 351-4.
2 Nxumalo L, Teranaka M, Schenk WG Jr. Hepatic blood flow measurement. Arch Surg1978; 113:169-72.
3 Charbon GA, Mark van der F. Use of electromagnetic flowmeter for the study of splanchnicblood flow. In: Granger DN, Bulkley GB, eds. Measurement of blood flow. Baltimore/London: Williams and Wilkins, 1981: 123-55.
4 Charbon GA, Brouwers HAA, Sala A. Histamine Hl- and H2-receptors in the gastro-intestinal circulation. Arch Pharm 1980; 312: 123-9.
5 Anderson MF, Drake-Bailey C. Measurement of hepatic blood flow in conscious dogs atrest, after feeding and during the development of portal hypertension. Proc 7th Internatconfer on biotelemetry 1982: 93-6.
6 Meindl JD, Ford AJ. Implantable telemetry 5. Meindl JD, Ford AJ. Implantable telemetryin biochemical research. IEEE Trans Biomed (Engl) 1984; 31: 814-23.
7 Meindl JD, Ford AJ, Taperell RE, et al. Implantable telemetry. In: Gray WI, Heavner JE,eds. Methods ofanimal experimentation. New York: Academic Press Inc, 1986; VII: part A,37-111.
8 Anderson MF. Pulsed Doppler ultrasonic flowmeter: application to the study of hepaticblood flow. In: Granger DN, Bulkley GB, eds. Measurement ofbloodflow. Applications tothe splanchnic circulation. Baltimore/London: Williams and Wilkins, 1981: 395-8.
9 Drake-Bailey C, Anderson MF, Knutti JW. Measurement of hepatic blood flow inconscious dogs at rest and after feeding. Gastroenterology 1982; 82: 1008.
10 Charbon GA. On vasodilators, magnesium and second messengers. J Mal Vasc 1986; 11:168-77.
11 Kiernan F. The anatomy and physiology of the liver. Philos Trans R Soc London (Biol)1833; 123:711-70.
12 Mall FP. A study of the structural unit of the liver. Am J Anat 1906; 5: 227-308.13 Rappaport AM, Knoblauch M. The hepatic artery, its structural, circulatory, and metabolic
functions. (3rd International Symposium of International Association on Study of Liver,Kyoto, 1966.) In: Vanderbroucke J, DeGroute J, Standaert LO, eds. Liver research,Antwerpen, Belgium. Antwerp: Tijdsch Gastroenterology, 1967: 118-28.
14 Rappaport AM. The microcirculatory hepatic unit. In: Gerok W, Sickinger K, eds. NewYork: Schattauer Verlag, Stuttgart, 1975: 425-34.
15 Rappaport AM, Schneiderman JJ. The function of the hepatic artery. Rev Physiol BiochemPharmacol 1976; 76: 129-75.
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

276 Charbon and Anderson
16 Rappaport AM. Hepatic blood flow: Morphologic aspects and physiologic regulation. IntRev Physiol 1980; 21: 1-63.
17 Motta PM. The three-dimensional fine structure of the liver as revealed by scanningelectron microscopy. Int Rev Cytol 1977; 6 [suppl]: 347-99.
18 Murakami T, Itoshima T, Shimada Y. Peribiliary portal system in the monkey liver asevidenced by the injection replica scanning electron microscope method. Arch Histol Jpn1974; 37: 245-60.
19 Ohtani 0, Murakami T. Peribiliary portal system in the rat liver as studied by the injectionreplica scanning electron microscope method. Scanning Electron Microscopy 1978; 11:241-4.
20 Nopanitaya W, Grisham JW, Aghajanian JG, Carson JL. Intrahepatic microcirculation:Scanning electron microscopy study of the terminal distribution of the hepatic artery.Scanning Electron Microsc 1978; 1: 837-42.
21 Ohtani 0. The peribiliary portal system in the rabbit liver. Arch HistolJpn 1979; 42: 153-67.22 Ohtani 0, Murakami T, Jones AL. Microcirculation of the liver, with special reference to
the peribiliary portal system. Basic Clin Hepatology 1982: 85-96.23 Ohtani 0, Kikuta A, Ohtsuka A, Taguchi T, Murakami T. Microvasculature as studied by
the microvascular corrosion casting/scanning electron microscope method. I. Endocrineand digestive system. Arch HistolJpn 1983; 46: 1-42.
24 Andrews WHH, Maegraith BG, Wenyon CE. Studies on the liver circulation. The micro-anatomy of the hepatic circulation. Ann Trop Med Parsitol 1949; 43: 229-37.
25 McCuskey RS. A dynamic and static study of hepatic arterioles and hepatic spincters. Am JAnat 1966; 119: 455-78.
26 Fioramonti J, Bueno L. Relation between intestinal motility and mesenteric blood flow inthe conscious dog. Am J Physiol 1984; 246: G108-13.
27 Anderson MF, Charbon GA. Response of gastro-intestinal circulation to norepinephrine,showing need for integrated studies of splanchnic and hepatic hemodynamics. Gastro-enterology 1984; 86: 1015.
28 Richardson PDI, Withrington PG. Alpha and beta adrenoceptors in the hepatic portalvenous vascular bed of the dog. Br J Pharmacol 1978; 62: 376-7.
29 Schuurkes JAJ, Brouwers HAA, Beijer HJM, Charbon GA, Schapiro H. Lysine-vasopressin: hemodynamic effects in various vascular areas in the anesthetized dog. Am JDig 1976; 21: 1012-9.
30 Kerr JC, Hobson RW, Seelig RF, Swan KG. Vasopressin: Route of administration andeffects on canine hepatic and superior mesenteric arterial blood flows. Ann Surg 1978; 187:137-42.
31 Lebrec D, Poynard T, Hillon P, Benhamou JP. Propranolol for prevention of recurrentgastrointestinal bleeding in patients with cirrhosis. N Engl J Med 1981; 305: 1371-81.
32 Immink WFGA, Beijer HJM, Charbon GA. Hemodynamic effects of norepinephrine andisoprenaline in various regions of the canine splanchnic area. Pfiuegers Arch 1976; 365: 107-18.
33 Braillon A, Cales, Girod C, Lebrec D. Alteration in response of the portal tributaryvascular bed to the B-agonist dobutamine in rats with extrahepatic portal hypertension.J Hepatol 1986; 2: 267-74.
34 Immink WFGA, Beijer HJM, Charbon GA. a- and n-receptor blockade of isoproterenol-and norepinephrine-induced effects on regional blood flow and blood flow acceleration. EurJ Pharmacol 1978; 50: 159-73.
35 Gill RW. Measurement of blood flow by ultrasound: accuracy and sources of error.Ultrasound Med Biol 1985; 11: 623-41.
36 Zoli M, Marchesini G, Cordiani MR, et al. Echo-Doppler measurement of splanchnic bloodflow in control and cirrhotic subjects. J Clin Ultrasound 1986; 14: 429-35.
37 Hulstaert PF, Geurts WJC, Brouwer FAS, Beijer HJM, Charbon GA. Hemodynamicactions of pentagastrin. Scand J Gastroenterol 1980; 15: 7-15.
38 Beijer HJM, Maas AHJ, Charbon GA. A vasopressin-induced decrease in pancreatic bloodflow and in pancreatic exocrine secretion in the anesthetized dog. Pfluegers Arch 1984; 400:324-8.
39 Finke U, Seifert J. Differential effects of gastrointestinal hormones on the blood flow of thealimentary tract of the dog. Exp Med 1986; 186: 151-65.
40 Gallavan RH Jr, Chou CC, Kvietys PR, Sit SP. Regional blood flow during digestion in theconscious dog. Am J Physiol 1980; 238: H220-5.
41 Beijer HJM, Maas AHJ, Charbon GA. Pancreatic 02 consumption and CO2 output duringsecretin-induced, exocrine secretion from the pancreas in the anesthetized dog. PfluegersArch 1984; 400: 318-23.
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

Hepatic haemodynamics related to bloodflow through gut, spleen, andpancreas 277
42 Blitz W, Charbon GA. Regional vascular influences of vasoactive intestinal polypeptide.Scand J Gastroenterol 1983; 18: 755-63.
43 Kvietys PR, Granger DN. Vasoactive and splanchnic oxygen uptake. Am J Physiol 1982;243: G1-9.
44 Kelly KA, Klopper PJ. Influence of isobaric and hyperbaric oxygen on biliary P02 and themechanics of bile flow. Am J Physiol 1967; 212: 1017-9.
45 Andrews WHH, Maegraith BG, Richards TG. The effect upon bromsulphalein extractionof the rate and distribution of blood flow in the perfused canine liver. J Physiol 1956; 131:669-77.
46 Brauer RW, Shill OS, Krebs JS. Studies concerning functional differences betweenliver regions supplied by the hepatic artery and by the portal vein. J Clin Invest 1959; 38:2202-14.
47 Bradley SE, Macpherson Al, Gammeltoft A, Blakemore AH. Effect of portacavalanastomosis on hepatic oxygen extraction and estimated hepatic blood flow in patients withcirrhosis. J Clin Invest 1951; 30: 630.
48 Charbon GA, Hulstaert PF. Augmentation of arterial hepatic and renal flow by extractedand synthetic parathyroid hormone. Endocrinology 1974; 96: 621-6.
49 Greenway CV, Stark RD. Hepatic vascular bed. Physiol Rev 1971; 51: 23-65.50 Burton-Opitz R. The vascularity of the liver. II. The influence of the portal blood flow upon
the flow in the hepatic artery. Q J Exp Physiol 1911; 4: 93.51 Hanson KM. Dilator responses of the canine hepatic vasculature. Angiologia 1973; 10:
15.52 Cohn R, Kountz S. Factors influencing control of arterial circulation to the liver of the dog.Am J Physiol 1963; 205: 1269.
53 Gingsburg M, Grayson J. Factors controlling liver blood flow in the rat. J Physiol (Lond)1954; 123: 574.
54 Grayson J, Mendel D. Observations on the intrahepatic flow interactions of the hepaticartery and portal vein. J Physiol (Lond) 1957; 139: 167.
55 Hanson KM. Experiments on autoregulation of hepatic blood flow in the dog. Circ Res1964; 15 [suppl I]: 222.
56 Torrance HB. The control of the hepatic arterial circulation. J Physiol (Lond) 1961; 158: 39.57 Hanson KM, Johnson PC. Local control of hepatic arterial and portal venous flow in the
dog. Am J Physiol 1966; 211: 712.58 Katz ML, Bergman EN. Simultaneous measurements of hepatic and portal venous blood
flow in the sheep and dog. Am J Physiol 1969; 216: 946.59 Matsuno H. Study on the hepatic circulation (part II): the relation of hepatic artery and
portal vein under hypoxia and pulmonary embolism. Jpn Circ J 1969; 33: 391.60 Sancetta SM. Dynamic and neurogenic factors determining the hepatic arterial flow after
portal occlusion. Circ Res 1953; 1: 414.61 Neutze JF, Wyler F, Rudolph AM. Changes in distribution of cardiac output after
hemorrhage in rabbits. Am J Physiol 1969; 215: 857.62 Condon RE, Nyphus ELM, Chapman ND, Harkins HW. Portal vein and hepatic artery
interaction. Studies in the isolated perfused liver. Gastroenterology 1962; 43: 547.63 Takeuchi J, Kubo T, Tone T, Takada A, Kitagawa T, Yoshida H. Autoregulation and
interaction between two vascular systems in the dog liver. J Appl Physiol 1969; 27: 77.64 Schenk WG, McDonald JC, McDonald K, Drapanas T. Direct measurement of hepatic
blood flow in surgical patients: with related observations on hepatic blood flow dynamics inexperimental animals. Ann Surg 1962; 156: 463.
65 Price JB, Britton RC, Peterson LM, Reilly PJW, Voorhees AB. The validity of chronichepatic blood flow measurements obtained by the electromagnetic flowmeter. J Surg Res1965; 5:313.
66 Ackroyd FW, Mito M, McDermott WV. Autonomic vasomotor controls in hepatic bloodflow. Am JSurg 1966; 112: 356.
67 BeBettencourt JM, Cruz JM. La circulation hepatique normale et pathologique. Paris:Expansion scientifique francaise, 1970.
68 Slater G, Vladeck BC, Bassin R, Shoemaker WC. Sequential changes in hepatic blood flowsduring hemorrhagic shock. Am J Physiol 1972; 223: 1428.
69 Gelman S, Ernst EA. The role of pH, CO2 and 02 content of portal blood in hepaticcirculatory autoregulation. Am J Physiol 1977; 233: E255-62.
70 Fischer A. Dynamics of the circulation in the liver. In: Rouiller C, ed. The liver,morphology, biochemistry and physiology. New York: New York Academic, 1963; vol 1:329.
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from

278 Charbon andAnderson
71 Rabinovici N, Vardi J. The intrahepatic portal vein-hepatic artery relationship. SurgGynecol Obstet 1965; 120: 38.
72 Herrick JF, Mann FC, Essex HE, Baldes EJ. The effect of the digestion of food on theblood flow from the liver of the dog. Am J Physiol 1934; 109: 52P.
73 Elwyn DH, Parikh HC, Shoemaker WC. Amino acid movements between gut, liver andperiphery in unanesthetised dogs. Am J Physiol 1969; 215: 1260.
74 Orrego H, Mena I, Baraona E, Palma R. Modifications in hepatic blood flow and portalpressure produced by different diets. Am J Dig Dis 1965; 10: 239.
75 Hopkinson BR, Schenk WG Jr. The electromagnetic measurements of liver blood flow andcardiac output in conscious dogs during feeding and exercise. Surgery 1968; 63: 970.
76 Anderson MF, Mulroy P. Changes in blood flow in the portal vein and hepatic artery afterfeeding. Gastroenterology 1986; 90: 1326.
77 Fronek K, Stahlgren LH. Systemic and regional hemodynamic changes during food intakeand digestion in nonanesthetised dogs. Circ Res 1968; 23: 687.
78 Nies AS, Wilkinson GR, Rush BD, Strother JT, McDevitt, DG. Effects of alteration ofhepatic blood microsomal enzyme activity on liver blood flow in the rat. BiochemPharmacol 1976; 25: 1991.
79 Richardson PDI, Withrington PG. Liver blood flow. I. Intrinsic and nervous control of liverblood flow. Gastroenterology 1981; 81: 159-73.
80 Richardson PDI, Withrington PG. Liver blood flow. II. Effects of drugs and hormones onliver blood flow. Gastroenterology 1981; 81: 356-75.
81 Greenway CV. Role of splanchnic venous system in overall cardiovascular homeostasis.Fed Proc 1983; 42: 1678-84.
82 Scholtholt J. Das Verhalten der Durchblutung der Leber bei Steigerung desSauerstoffverbrauches der Leber. Pfluegers Arch 1970; 318: 202-16.
83 Lautt WW. Effects of acute, passive hepatic congestion on blood flow and oxygen uptake inthe intact liver of the cat. Circ Res 1977; 41: 787-90.
84 Gottlieb ME, Sarfeh IJ, Stratton H. et al. Hepatic perfusion and splanchnic oxygenconsumption in patients postinjury. J Trauma 1983; 23: 83643.
85 Hayashi N, Kasahara A, Kurosawa K, et al. Oxygen supply to the liver in patients withalcoholic liver disease assessed by organ-reflectance spectrophotometry. Gastroenterology1985; 88: 881-6.
86 Andreen M. Inhalation versus intravenous anaesthesia. Effects on the hepatic andsplanchnic circulation. Acta Anaesthesiol Scand 1982; 75: 25-31.
87 Larsen KR, Moody FG. Selection of appropriate methodology for the measurement ofblood flow in the gut. In: Granger DN, Bulkley GB, eds. Measurement of blood flow.Applications to the splanchnic circulation. Baltimore/London: Williams and Wilkins, 1981:511-28.
on June 7, 2020 by guest. Protected by copyright.
http://gut.bmj.com
/G
ut: first published as 10.1136/gut.30.2.265 on 1 February 1989. D
ownloaded from