PANCREATIC PSEUDOCYST 2.pptx
-
Upload
azharulhassanqureshi -
Category
Documents
-
view
78 -
download
6
Transcript of PANCREATIC PSEUDOCYST 2.pptx
PowerPoint Presentation
PANCREATIC PSEUDOCYSTByMaj. Amir Iqbal
Resident General Surgery
SupervisorLt Col Syed Mukarram HussainConsultant Laparoscopic Surgeon
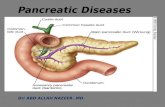
Pancreatic pseudocyst is best defined as a localized fluid collection that is rich in amylase and other pancreatic enzymeshas a non-epithelialized wall consisting of fibrous and granulation tissueusually appears several weeks(4 weeks or more) later after the onset of either acute or chronic pancreatitis.
Brun A, Agarwal N, Pitchumoni CS. Fluid collections in and around the pancreas in acute pancreatitis. J Clin Gastroenterol . Aug 2011;45(7):614-25.INTRODUCTIONThese characteristics contrast with those of acute fluid collections, which are more evanescent and are serosanguinous inflammatory reactions to acute pancreatitis. These collections are noted in moderate-to-severe pancreatitis. Acute fluid collections usually have an irregular shape and lack a well-defined wall. In general, they resolve in about 65% of cases.Two other types of fluid collection should be considered. First, organized necrosis is actually devitalized pancreatic tissue that appears cystlike on CT scan, but it appears to be solid on other imaging modalities. Second, an abscess is an infected area of necrosis or fluid.2Most common cystic lesions of the pancreas, accounting for 75-80% of such massesMay be single or multiple50% have a communication with main pancreatic ductIn children, pseudocysts and trauma are frequently associatedLocationLesser peritoneal sac in proximity to the pancreasLarge pseudocysts can extend into the paracolic gutters, pelvis, mediastinum, neck or scrotum
PATHOPHYSIOLOGYPancreatic ductal disruption secondary toAcute pancreatitis Pancreatic necrosis causes ductular disruption, resulting in leakage of pancreatic juice from inflamed area of gland, accumulates in space adjacent to pancreas Inflammatory response induces formation of distinct cyst wall composed of granulation tissue, organizes with connective tissue and fibrosis
4PATHOPHYSIOLOGY (Cont.)Chronic pancreatitis Pancreatic duct chronically obstructed ongoing proximal pancreatic secretion leads to secular dilation of duct true retention cystFormed micro cysts can eventually coalesce and lose epithelial lining as enlargeTraumaDuctal obstruction and pancreatic neoplasms
COMPOSITIONThick fibrous capsule not a true epithelial lining Pseudocyst fluid Similar electrolyte concentrations to plasma High concentration of amylase, lipase, and enterokinases such as trypsinPRESENTATIONSymptoms Abdominal pain > 3 weeks (80 90%) Nausea / vomiting Early satiety Bloating, indigestion
Cohen et al: Pancreatic pseudocyst . In: Cameron JL, ed. Current Surgical Therapy. 7th ed.; 2001: 543-7Signs Tenderness Abdominal fullness/mass Icterus / pleural effusion Peritoneal signs indicate ruptured or infected cyst
DIAGNOSISClinically suspect a pseudocyst ifEpisode of pancreatitis fails to resolve Amylase levels persistently high Persistant abdominal pain Epigastric mass palpated after pancreatitisDIFFERENTIAL DIAGNOSISOrganized pancreatic necrosisAcute pancreatic fluid collectionsSerous cystadenoma of the pancreasMucinous cystadenoma of the pancreas Mucinous cystadenocarcinoma Pancreatic retention cysts
OthersPancreatic CancerPancreatic Necrosis and Pancreatic AbscessPancreatic PseudoaneurysmPancreatitis, AcutePancreatitis, Chronicvon Hippel-Lindau Disease
INVESTIGATIONSSerum tests have limited use. Amylase and lipase levels may be elevated.Bilirubin and liver function test (LFT) findings may be elevated if the biliary tree is involved.Analysis of the cyst fluid may help differentiate pseudocysts from tumors. 11CHARACTERISTICPSEUDOCYSTTUMORCarcinoembryonic antigen (CEA) LowHighCarcinoembryonic antigen-125 (CEA-125) LowHighFluid ViscosityLowHighAmylase levels HighLowCytologyInflammatory cellsTumor cells*A CEA level of greater than 400 ng/mL within the cyst fluid strongly suggests malignancyINVESTIGATIONS (contd.)Plain X-rayNot very usefulUltrasoundAbdominal or endoscopic75 -90% sensitiveMay be used to visualize cystic fluid collections in and around the pancreasCTImaging criterion standard for pancreatic pseudocysts90-100% sensitivity ERCP is not necessary in diagnosing pseudocysts however, it is useful in planning drainage strategy. MRCP to establish the relationship of the pseudocyst to the pancreatic ducts
The usual finding on CT scan is a large cyst cavity in and around the pancreas.Multiple cysts may be present.The pancreas may appear irregular or have calcifications.Pseudoaneurysms of the splenic artery, bleeding into a pseudocyst, biliary and enteric obstruction, and other complications may be noted on CT scan.The CT scan provides a very good appreciation of the wall thickness of the pseudocyst, which is useful in planning therapy.
13Sonographic evaluation
EUS showing pseudocyst
Pseudocyst compressing the stomach wall posteriorly
HISTOLOGYHistologic findings vary with age because older cysts have thicker walls with more collagen. The etiology of the cyst does not change the histology. Note the following zone features:Zone 1 - Hemosiderin pigment and loose connective tissueZone 2 - Inflammatory cells and capillary-rich fibrous tissueZone 3 - Hyalinized acellular connective tissueZone 4 - Capillary-rich fibrous stroma
CLASSIFICATION BASED ON DUCT ANATOMYType I: normal duct/no communication with cyst. Type II: normal duct with duct-cyst communication. Type III: otherwise normal duct with stricture and no duct-cyst communication. Type IV: otherwise normal duct with stricture and duct-cyst communication. Type V: otherwise normal duct with complete cut-off. Type VI: chronic pancreatitis, no duct-cyst communication. Type VII: chronic pancreatitis with duct-cyst communication
System to categorize ductal disruptions or ductal abnormalities seen in patients with pancreatic pseudocysts. The main pancreatic duct is represented in all types. Type 1 is a normal pancreatic duct with a noncommunicating pseudocyst represented by the dotted elliptical mass. Type 2 represents a normal duct with communication with the cyst. Type 5 represents the so-called isolated pancreatic segment. Types 6 and 7 represent chronic pancreatitis.18NATURAL HISTORY OF PSEUDOCYST50% resolve spontaneouslySizeNearly all < 4cm resolve spontaneously>6cm 60-80% persist, necessitate interventionCauseTraumatic, chronic pancreatitis 6-8 weeksTREATMENTNo medications are specific to the treatment of pancreatic pseudocystsInitial NPO TPN Octreotide - be useful as an adjunct to catheter drainage. Used to reduce pancreatic exocrine secretion. Antibiotics - are an adjunct to drainage of infected pseudocysts.INTERVENTIONIndications for drainagePresence of symptoms (> 6 wks)Enlargement of pseudocyst ( > 6 cm)ComplicationsSuspicion of malignancyINTERVENTIONS (cont.) External Drainage Percutaneous drainage Open Drainage Internal Drainage Endoscopic Transpapillary Drainage Transmural drainage ( Transgastric or Transduodenal ) Laparoscopic Drainage Cysto-gastrostomy Cysto-jejunostomy Open Surgical drainage Cysto-gastrostomy Cysto-jejunostom (Roux-en-Y) Pancreatic Resection Excision of the pseudocyst PancreaticoduodenectomyPERCUTANEOUS DRAINAGEContinuous drainage until output < 50 ml/day + amylase activity Failure rate 16% Recurrence rates 7% ComplicationsConversion into an infected pseudocyst (10%)Catheter-site cellulitis Damage to adjacent organsPancreatico-cutaneous fistulaGI hemorrhageGumaste et al: Pancreatic pseudocyst. Gastroenterologist 1996 Mar; 4(1): 33-43
EXTERNAL DRAINAGE
ENDOSCOPIC MANAGEMENTIndicationsMature cyst wall < 1 cm thickAdherent to the duodenum or posterior gastric wallPrevious abd surgery or significant comorbiditiesContraindicationsBleeding dyscrasiasGastric varicesAcute inflammatory changes that may prevent cyst from adhering to the enteric wallCT findingsThick debris Multiloculated pseudocystsENDOSCOPIC DRAINAGETransenteric drainageCystogastrostomyCystoduodenostomyTranspapillary drainageERCP with sphincterotomy, balloon dilatation of pancreatic duct strictures, and stent placement beyond strictures
LAPAROSCOPIC MANAGEMENTThe interface b/w the cyst and the enteric lumen must be 5 cm for adequate drainageApproachesPancreatitis secondary to biliary etiology extraluminal approach with concurrent laparoscopic cholecystectomyNon-biliary origin intraluminal (combined laparoscopic/endoscopic) approach. Mortality rate is 3%, and the complication rate is approximately 24%. The success rate is 85-90%.Aljarabah M, Ammori BJ. Laparoscopic and endoscopic approaches for drainage of pancreatic pseudocysts: a systematic review of published series.Surg Endosc. Nov 2007;21(11):1936-44.OPEN SURGICAL OPTIONSInternal drainage Cystogastrostomy Cystojejunostomy Permanent resolution confirmed in b/w 91%97% of patientsCystoduodenostomy Can be complicated by duodenal fistula and bleeding at anastomotic siteCysto-gastrostomy
Cysto-jejunostomy
PANCREATIC RESECTIONEnucleation of Pseudocyst Pseudocyst of Head of pancreas with strictures of pancreatic or bile ducts need pancreaticoduodenectomyEnucleation of Pseudocyst
PREFERRED INTERVENTIONSurgical drainage is the traditional approach gold standard.Percutaneous catheter drainage high chance of persistant pancreatic fistula.Endoscopic drainage - less invasive, becoming more popular, technically demandingSurgery necessary in complicated pseudocyts, failed nonsurgical, and multiple pseudocysts.FOLLOW-UPDietary Advice: Patients may eat a low-fat diet as tolerated. Patients who have endoscopically placed stents must be monitored via serial CT scans to observe resolution of the cyst. Stents may then be endoscopically removed after resolution. Closely monitor patients with percutaneous drains for pain , infection , or catheter migration . Remove the drain when drainage ceasesCOMPLICATIONSInfectionAbscessSystemic sepsisRuptureInto the gutGI bleedInternal fistulaInto peritoneumPeritonitis
EnlargementPressure effectsObstructive jaundiceBowel ObstructionPainErosion into a vesselHaemorrhage into the cystHaemoperitoneum
PROGNOSISMost pseudocysts resolve without interference, and patients do well without intervention. Outcome is much worse for patients who develop complications. The presence of pancreatic necrosis is a poor prognostic sign. The failure rate for drainage procedures is about 10%, the recurrence rate is about 15%, and the complication rate is 15-20%.THANK YOU