Biochemistry 3070 – Nucleic Acids 1 Nucleic Acids Biochemistry 3070.
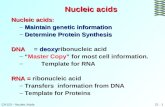
Nucleic Acids
Transcript of Nucleic Acids

NUCLEIC ACIDS: RNA AND DNA
NUCLEIC ACIDS
A nucleic acid is a complex, high-molecular-weight biochemical macromolecule composed of nucleotide chains that convey genetic information.
The most common nucleic acids are deoxyribonucleic acid (DNA) and ribonucleic acid (RNA). Nucleic acids are found in all living cells and viruses. Artificial nucleic acids include peptide nucleic acid (PNA), Morpholino and locked nucleic acid (LNA), as well as glycol nucleic acid (GNA) and threose nucleic acid (TNA). Each of these is distinguished from naturally occurring DNA or RNA by changes to the backbone of the molecule.
Medical Functions:
The use of DNA and RNA probe technology in the clinical laboratory has grown over the past decade from a research-oriented activity to become an established facet of diagnostic testing.
The technology has been particularly well received for infectious disease testing applications, but applications in cancer and genetic disease diagnosis are of increasing interest to clinicians.
One indication of the emergence of molecular biology as an established clinical discipline is the establishment of molecular diagnostics sections in clinical laboratories in most major medical centers
Those departments generally focus their activities in the areas of testing for genetic disorders, oncology testing, human leukocyte antigen typing, and infectious disease testing.
The structure and base sequence of RNA are determinants of protein synthesis and the transmission of genetic information
DNA carries the cell's genetic information and hereditary characteristics via its nucleotides and their sequence and is capable of self-replication and RNA synthesis.
Physical and Chemical Properties of Nucleic Acids:

Chemical Stability of Nucleic Acids
-DNA is generally quite stable. It will resist attack in acid and alkali solutions. However, in mild acid solutions - at pH 4 - the beta-glycosidic bonds to the purine bases are hydrolyzed. Protonation of purine bases (N7 of guanine, N3 of adenine) occurs at this pH. Protonated purines are good leaving groups hence the hydrolysis. Once this happens, the depurinated sugar can easily isomerize into the open-chain form and in this form the depurinated (or apurinic) DNA is susceptible to cleavage by hydroxyl ions.
Physical Stability of DNA
-The two polynucleotide chains of double-helical DNA can be separated under certain conditions, most usually by raising the temperature. The transition from double-stranded DNA (dsDNA) to single-stranded random coil DNA (ssDNA) is called a helix-coil transition. Terms that describe the change from dsDNA to ssDNA are: melting, denaturation, strand separation. Terms that describe the change from ssDNA to dsDNA are annealing, renaturation, and, in certain contexts, hybridization.
Base composition
- More energy is required to disrupt the three hydrogen bonds of a GC base pair than is required to disrupt the two hydrogen bonds of an AT base pair. More energy is required to disrupt the stacking interactions involving GC base pair than is required to disrupt stacking interactions involving AT base pairs.
- This effect can be seen most readily by examining the thermal denaturation profiles of DNA samples which contain different GC content.
- The denaturation of double stranded DNA is easily followed spectroscopically. The purine and pyrimidine bases in DNA absorb UV light maximally at a wavelength of approximately 260 nm. In double-stranded DNA, however, the absorption is decreased due to base-stacking interactions. When DNA is denatured, these interactions are disrupted and an increase in absorbance is seen. This change is called the hyperchromic effect. The extent of the effect can be monitored as a function of temperature.

Salt concentration
- The negatively charged phosphate groups in the DNA double helix are close together and will tend to repel one another unless they are neutralized. Since the concentration of salt (cations) in solution will affect the degree of neutralization, the stability of DNA double helices also depends on the salt concentration.
- In the cell, neutralization is achieved through salt ions, polyamines and special DNA-binding proteins. There are circumstances in the cell when DNA must be (at least partially) denatured. Under normal circumstances, partially denatured regions of DNA will not be stable. Therefore, special proteins exist which bind to ssDNA to maintain it in a single-stranded conformation when necessary.
pH
- While not chemically susceptible to strong alkali, DNA is nevertheless affected by strong alkali solutions because these will also cause denaturation of the double helix.
- The use of alkaline conditions to denature DNA is commonly used to prepare single-stranded templates for DNA sequencing reactions.
SOURCES
DNA- Fish, nuts, seafood, fish, beans, mushrooms, beef, broth and vegetable soups, Sardines
RNA- blood or soft tissue samples, extracted from semen, saliva, hair roots and even from several skin cells left on the surface of a pint glass after it was touched
DISEASES
Examples of disease in DNA1. Cockayne Syndrome
2. Lesch-Nyhan syndrome Examples of disease in RNA
1. Pyruvate carboxylase deficiency2. 21-hydroxylase deficiency3. Canine Phosphofructokinase

Supplementary Questions
1. Where are the nucleoproteins found in the body?o Most Nucleoproteins are found in the DNA and RNA.
2. Discuss in detail the hydrolytic reaction of nucleic acid.o Hydrolysis of nucleic acids gives nucleotides which can be considered the
units that makeup the polymer.
Does it happen in vitro? No.
3. Could the diphenylamine reaction be used to distinguish RNA from DNA? Support your answer. Yes, RNA can be distinguish for DNA by using Diphenylamine indication. It will confirm the presence of DNA. This procedure involves chemical hydrolysis of DNA when reacted in acid. The reaction requires Deoxyribose sugar in DNA, there is no reaction with the Ribose of sugars of the DNA.
EXPERIMENT 14

BLOOD
Blood
- is a highly specialized circulating tissue consisting of several types of cells suspended in a fluid medium known as plasma.
- The cellular constituents are: red blood cells, which carry respiratory gases and give it its red color because they contain hemoglobin (an iron-containing protein that binds oxygen in the lungs and transports it to tissues in the body), white blood cells (leukocytes), which fight disease, and platelets, cell fragments which play an important part in the clotting of the blood.
- Medical terms related to blood often begin with hemo- or hemato- Anatomically, blood is considered a connective tissue from both its origin in the bones and its function.
CHARACTERISTICS OF BLOOD
Blood has distinctive physical characteristics:
Amount
a person has 4-6 liters of blood, depending on the body size. Of the total blood volume in the human body, 38% to 48% is composed of the various blood cells also called “formed elements”. The remaining 52% to 62% of the blood volume is the plasma or the liquid portion of the blood.
Color
Red. Arterial blood is bright red because it contains high levels of oxygen. Venous blood has given up much of its oxygen in tissues and has a darker,

dull red color. This may be important in the assessment of the source of bleeding.
pH
the normal pH range of blood is 7.35-7.45, which is slightly alkaline.
Viscosity
this means the thickness or the resistance to flow. Blood is about 3 to 5 times thicker than water. Viscosity is increased by the presence of blood cells and the plasma proteins, and this thickness contributes to normal blood pressure.
COMPOSITION OF BLOOD
When a sample of blood is spun in a centrifuge, the cells and cell fragments are separated from the liquid. Because the formed elements are heavier than the liquid matrix, they are packed in the bottom of the tube by the centrifugal force. The straw colored liquid on the top is the plasma.
A GIVEN VOLUME OF BLOOD IS 55 PERCENT PLASMA AND 45 PERCENT FORMED CELLS.
Plasma is the liquid portion of blood, and it is about 90% water. The remaining portion consists of more than 100 different organic and inorganic solutes that are dissolved in water. Because plasma is a transport medium, it's solutes are continuously changing as substances are added or removed by the cells.

Plasma proteins are the most abundant solutes in the plasma. These proteins remain in the blood and interstitial fluid and are not used for energy. The three major classes of plasma proteins are: albumins, globulins, and fibrinogen. Many of the plasma proteins are synthesized in the liver, and each one has a different function.
Albumins
- is the most abundant plasma proteins. It is synthesized by the liver. Because they are so abundant, they contribute to the osmotic pressure of the blood and play an important role in maintaining fluid balance between blood and interstitial fluid. If the osmotic pressure of the blood decreases, fluid moves from the blood into the interstitial spaces, which results in edema. This also decreases blood volume and, in severe cases, may reduce blood pressure. When blood osmotic pressure increases, fluid moves from the interstitial spaces
The general functions of blood include
Transportation, Regulation Protection.
The following activities are under the transportation function:
Carries O2 and nutrients to the cells
Transports CO2 and wastes from the tissues to the lungs and the kidneys where wastes can be removed from the body
Carries hormones to the endocrine glands to the target tissues
The following activities are under the regulation function :

Helps to regulate body temperature by removing heat from active areas, such as skeletal muscles and transporting it to other areas of the skin so the heat can be dissipated
Plays a significant role in fluid and electrolyte balance because salt and plasma proteins contribute to the osmotic pressure by providing weight and bulk to our blood
Functions in pH regulation through the action of buffers in the blood
Functions of the blood that in the protection category:
Clotting mechanisms prevent fluid loss through hemorrhage when blood vessels become damaged
Certain cells in the blood, phagocytic white blood cells help to protect the body against diseases by engulfing and destroying the agent
Antibodies in the plasma help protect against disease by their reactions with offending agents
Certain types of white blood cells produce antibodies, special proteins that recognize foreign materials and help the body destroy or neutralize them.
When a person has an infection, his or her white cell count (the number of cells in a given amount of blood) often is higher than when he or she is well because more white blood cells are being produced or are entering the bloodstream to battle the infection.
After the body has been challenged by some infections, lymphocytes "remember" how to make the specific antibodies that will quickly attack the same germ if it enters the body again.
Blood is essential for good health because the body depends on a steady supply of fuel and oxygen to reach its billions of cells.

Even the heart couldn't survive without blood flowing through the vessels that bring nourishment to its muscular walls!
Blood also carries carbon dioxide and other waste materials to the lungs, kidneys, and digestive system, from where they are removed from the body.
PROPERTIES OF BLOOD
Our bodies consist of metabolically active cells that need a continuous supply of nutrients and oxygen. Metabolic waste products need to be removed from the cells to maintain a stable cellular environment. Blood is the primary transport medium that is responsible for meeting these cellular demands.
Materials transported by the blood include nutrients, waste products, gases, and hormones. The blood helps to regulate the fluid and electrolyte balance, acid base balance, and the body temperature. Protection against pathogens is provided by white blood cells, and the clotting mechanism prevents excessive loss of blood after injuries.
Diseases of the Red Blood Cells
Anemia resulting from inadequate red blood cell productionThere are several conditions that can cause a reduced production of red blood cells, including:
o Iron deficiency anemia. Iron deficiency anemia is the most common type of anemia and affects kids and teens of any age who have a diet low in iron or who've lost a lot of red blood cells (and the iron they contain) through bleeding..
o Lead poisoning. When lead enters the body, most of it goes into red blood cells where it can interfere with the production of hemoglobin. This can result in anemia. Lead poisoning can also affect - and sometimes permanently damage - other body tissues including the brain and nervous system.

o Anemia due to chronic disease. Children with chronic diseases (such as cancer or human immunodeficiency virus infection) often develop anemia as a complication of their illness.
o Anemia due to kidney disease. The kidneys produce erythropoietin, a hormone that stimulates production of red cells in the bone marrow. Kidney disease can interfere with the production of this hormone.
Anemia resulting from unusually rapid red blood cell destructionWhen red blood cells are destroyed more quickly than normal by disease (this process is called hemolysis, pronounced: hih-mah-luh-sus), the bone marrow will make up for it by increasing production of new red cells to take their place. But if red blood cells are destroyed faster than they can be replaced, a person will develop anemia. There are several causes of increased red blood cell destruction that can affect teens:
o G6PD deficiency. G6PD is an enzyme that helps to protect red blood cells from the destructive effects of certain chemicals found in foods and medications. When the enzyme is deficient, these chemicals can cause red cells to hemolyze, or burst. G6PD deficiency is a common hereditary disease among people of African, Mediterranean, and Southeast Asian descent.
o Hereditary spherocytosis (pronounced: sfeer-o-sye-toe-sus) is an inherited condition in which red blood cells are misshapen (like tiny spheres, instead of disks) and especially fragile because of a genetic problem with a protein in the structure of the red blood cell. This fragility causes the cells to be easily destroyed.
Diseases of the White Blood Cells
Neutropenia (pronounced: noo-truh-pee-nee-uh) occurs when there aren't enough of a certain type of white blood cell to protect the body against bacterial infections. People who take certain chemotherapy drugs to treat cancer may develop neutropenia.
Human immunodeficiency virus (HIV) is a virus that attacks certain types of white blood cells (lymphocytes) that work to fight infection. Infection with the virus can result in AIDS (acquired immunodeficiency syndrome), leaving the body prone to infections and certain other diseases.

Leukemias (pronounced: loo-kee-mee-uhz) are cancers of the cells that produce white blood cells. These cancers include acute myeloid leukemia (AML), chronic myeloid leukemia (CML), acute lymphocytic leukemia (ALL), and chronic lymphocytic leukemia (CLL). The most common types of leukemia affecting kids are ALL and AML..
Diseases of Platelets
Thrombocytopenia (pronounced: throm-buh-syte-uh-pee-nee-uh), or a lower than normal number of platelets, is usually diagnosed because a person has abnormal bruising or bleeding. Thrombocytopenia can happen when a person takes certain drugs or develops infections or leukemia or when the body uses up too many platelets.
EXPERIMENT 14
BLOOD
PROCEDURE
1. Separation of serum from whole blood
Blood can be obtained through venipuncture, but this should only be done by an expert with required aseptic preparation and process. Extracted blood is kept in small test tube. Centrifugation of the whole blood separates the serum (clear yellow fluid). Pipet out the serum slowly and place in a test tube. Divide the serum into four portions. (If the fluid collected appears to be reddish, discard the fluid collected).
2. Separation for the presence of Carbohydrates1. To the first portion of serum, add 5 drops of Benedict’s reagent2. Boil in a water bath until a positive result is obtained.
What is the positive result?
Brick red precipitate.
What does it indicate?

Sugar in blood serums present.
Explain the basis of the test.
There is a small amount of hexose. Glucose is a hexose sugar found in the blood plasma of a normal individual stored in the form of glycogen. Plasma protein include albumin, globulin and fibrinogen.
3. Test for the presence of Protein1. Test for serum albumin and globulin
To the second portion of the serum, add an equal volume of saturated ammonium sulfate solution. Describe the result.
Solution with precipitate
1. Add 1% of sodium chloride solution drop by drop. Shake. Describe what happens.
Precipitate is dissolved; white solution.
2. Add ammonium sulfate crystals to the solution until saturated. What happens?
+ Ammonium Sulfate crystals: Precipitate did not dissolve.
What is the role of ammonium sulfate? Precipitating Agent
Of NaCl? Dissolving Agent
4. Chloride determination1. To the third portion of the serum, acidify with 2 drops of 10% HNO3.2. Add 5 drops of 5% silver nitrate. What did you observe?
Write the chemical equation involved in the reaction.

(HNO3)
Cl- + AgNO3 AgCl + NO3
5. Phosphate determination1. To the fourth portion of the serum, acidify with 2 drops of 10% nitric acid.2. Add 2 mL of 5% ammonium molybdate solution.3. Heat in a water bath and note the formation of yellow precipitate.
What is the chemical composition of the yellow precipitate?
PO4-3 + NH4 MoO4 (NH4)3 + PO4
6. Test for fibrin in the clotted blood
Describe the color and texture of the fibrin. Pink cream thread like structure.
1. To the first portion, add 2 mL Millon’s reagent in a test tube. Place it in a water bath for about 10 minutes.
What is the result?
Brick red precipitate.
What does it indicate? Tyrosine is present.
2. Mix 3 mL of Hpokin’s Cole reagent and drop by drop of 3 mL concentrated sulfuric acid. Add the second portion of the fibrin.
Is there a positive reaction?
Violet ring formed in the solution.

What does the result indicate? Tryptophan is present.
7. Test for the presence of Cholesterol
Chloroform extract: Clear light green solution.
Standard cholesterol: Dark green solution.
8. Iron determination1. Put 2 mL of blood in an evaporating dish and heat until ash is formed.
(PERFORM UNDER THE FUME HOOD)
2. Cool and dissolve the ash in dilute HCl. Filter.
Test the filtrate for the presence of iron by adding ammonium thiocyanate drop by drop. Describe the resulting solution.
(+) Result: Salmon pink color of solution.
What is the purpose of adding ammonium thiocyante?
To detect iron in the blood.
9. Blood gases1. Dilute 1 mL of blood with about 3 mL of water in atest tube. Shake and
note the bright red color of oxyhemoglobin. Observation.
The result is: Brick red solution.

2. Put half of this in aother test tube to serve as control.3. Put the remaining half in another test tube, add 1 Ml of Stoke’s reagent
and add enough ammonium hydroxide to dissolve the precipitate. This gives a strong reducing solution.
4. Add a few drops of this reagent to the oxyhemoglobin solution. Shake the test tube vigorously. Describe the resulting solution.
Dark red solution with bubbles.
Explain the reaction that took place.
Blood + H20 Bright red color due to oxyhemoglobin
Blood + H20 + Stoke agent Dark red solution
ppt and bubbles (reduced hemoglobin)
SUPPLEMENTARY QUESTIONS
1. What is the difference between blood plasma and interstitial fluid in terms of composition?
Blood Plasma composed of water, blood proteins, and inorganic electrolytes.
Interstitial fluid consists of a water solvent containing amino acids, sugars, fatty acids, coenzymes, hormones, neurotransmitters, salts, as well as waste products from the cells.
2. What is the chief function in the blood of each of the following:
1. Hemoglobin

The pigment which gives the red blood cells their color;
Act as a carrier of oxygen from the lungs to the tissue.
2. Chloride ions
Inorganic constituent of the blood.
Major Extracellular Anion.
Component of Gastric acid
3. Phosphate ions
Inorganic constituents of the blood.
Primary intracellular Anion.
Acid based balance of the body.
Protection of ATP.
4. Sodium ions
Major Extracellular Cation.
Maintain osmotic pressure of Extracellular fluid.
Control water retention of the tissue spaces.
Help maintain blood pressure.
Maintain acid-base balance.
5. Potassium ions
Major intracellular cation.

Maintain osmotic pressure of the cell.
Maintain electrical potential of cell.
Maintain size of the cells.
Maintain proper contraction of the heart.
3. What is the principal anion present in blood and interstitial fluid?
Principal anion is chloride ion and phosphate ion. This is the fluid found in the tissues spaces. It is derived partly from blood plasma and partly from the cells. Nutrients pass into the cells.
EXPERIMENT 15
URINE
Chemical analysis
Urine contains a range of substances that vary with what is introduced into the body. Aside from water, urine contains an assortment of inorganic

salts and organic compounds, including proteins, hormones, and a wide range of metabolites.
Unusual color
Colorless urine indicates over-hydration, which is usually considered much healthier than dehydration. In the context of a drug test, it could indicate a potential attempt to avoid detection of illicit drugs in the bloodstream through over-hydration.
Dark yellow urine is often indicative of dehydration. Yellowing/light orange may be caused by removal of excess B vitamins from the
bloodstream. Certain medications such as rifampin and pyridium can cause orange urine. Bloody urine is termed hematuria, potentially a sign of a bladder infection. Dark orange to brown urine can be a symptom of jaundice, rhabdomyolysis,
or Gilbert's syndrome. Black or dark-colored urine is referred to as melanuria and may be caused by
a melanoma. Fluorescent yellow / greenish urine may be caused by dietary supplemental
vitamins, especially the B vitamins. Consumption of beets can cause urine to have a pinkish tint,
and asparagus consumption can turn urine greenish. Reddish or brown urine may be caused by porphyria. Although again, the
consumption of beets can cause the urine to have a harmless, temporary pink or reddish tint.
B. Transparency (cloudiness or turbidity)
A fresh sample of normal urine should be transparent, but may become cloudy after standing awhile. Cloudy urine may be evidence of phosphates, urates, pus, mucus, bacteria, epithelial cells, fat, and chyle. Phosphates disappear with the addition of dilute acetic acid and urates dissipate with heat. Other causes of turbidity can be analyzed by microscopic examination.
After shaking your sample, determine the degree of cloudiness and record it on the Urinalysis worksheet.
C. Hydrogen Ion Concentration (pH).

Although freshly voided urine is usually acidic (around pH 6), the normal range is between 4.8 and 7.5. The pH will vary with the time of day and diet. Twenty-four-hour specimens are less acidic than fresh specimens and may become alkaline after standing due to bacterial decomposition of urea to ammonia. High acidity is present in acidosis, fevers, and high protein diets. Excess alkalinity may be due to urine retention in the bladder, chronic cystitis, anemia, obstructing gastric ulcers, and alkaline therapy. The simplest way to determine pH is to use pH indicator paper strips.
D. Protein
Although the large size of protein molecules normally prevents their presence in urine, certain conditions can allow them to filter through. Excessive muscular exertion, prolonged cold baths and excessive ingestion of protein may result in physiological albuminuria. Pathologic albuminuria, on the other hand, exists when albumin of the urine is due to kidney congestion, toxemia of pregnancy, febrile disease and anemias.
E. Glucose.
As stated above, only a small amount of glucose is normally present in urine (0.01 to 0.03 g/100 ml of urine). When urine contains glucose in amounts greater than this, glucosuria exists. This is usually an indication of diabetes mellitus. Lack of insulin production by the pancreas or insensitivity to insulin is the cause of the disease. Insulin is necessary to stimulate the conversion of excess glucose to glycogen in the liver and muscles. It is also essential to stimulate the oxidation of glucose by cells. A deficiency of insulin function, thus, will result in high blood concentrations of glucose. The renal threshold of glucose is around 160 mg/100 ml. Glucosuria indicates that blood concentrations of glucose exceed this amount and the kidneys are unable to accomplish 100% reabsorption of this carbohydrate.
F. Ketones.

Normal catabolism of fats produces carbon dioxide and water as final end products. When there is not an adequate amount of carbohydrate in the diet, or when there is a defect in carbohydrate metabolism, the body begins to utilize an increasing amount of fatty acids. When this increased fat metabolism reaches a certain point, fatty acid utilization becomes incomplete, and intermediary products of fat metabolism occur in the blood and urine. These intermediary substances are the three ketone bodies: acetoacetic acid (diacetic acid), acetone, and beta hydroxybutyric acid. The presence of these substances in urine is called ketonuria.
Diabetes mellitus is the most common disorder in which ketonuria occurs. Progressive diabetic ketosis is the cause of diabetic acidosis, due to the increased concentration of ketoacids which can eventually lead to coma or death. It is for this reason that the detection of ketonuria in diabetics is of great significance.
G. Hemoglobin
When red blood cells disintegrate (hemolysis) in the body, hemoglobin is released into the surrounding fluid. If the hemolysis occurs in the blood vessels, the hemoglobin becomes a constituent of plasma. Some of it will be excreted by the kidneys into urine. If the red blood cells enter the urinary tract due to disease or trauma, the cells will hemolyze in the urine. The presence of hemoglobin in urine is called hemoglobinuria.
Hemoglobinuria may be evidence of a variety of pathologies such as hemolytic anemia, transfusion reactions, yellow fever, smallpox, malaria, hepatitis, mushroom poisoning, renal infections, burns, etc.
H. Specific Gravity
Urine specific gravity is a measure of urine concentration. It is the weight of a substance, presented as a ratio, compared to an equal volume of water. The specific gravity of a 24-hour specimen of normal urine will be between 1.015 and 1.025. Single urine specimens may range from 1.002 to 1.030. The more solids in solution, the higher will

be the specific gravity. The greater the volume of urine in a 24-hour specimen, the lower will be the specific gravity. A low specific gravity will be present in chronic nephritis and diabetes insipidis. A high specific gravity may indicate diabetes mellitus, fever, and acute nephritis.
To measure specific gravity use one of the refractometers. Open the plastic cover on the front of the instrument and place a drop of sample on the glass surface, lower the cover carefully or the sample will splash. While pointing the refractometer toward a light source, look through the eyepiece and adjust the focus ring until the field is clear. You will see a circular field with several numeric scales, bisected by a horizontal line where the upper darker colored portion of the field and the lower lighter colored portion of the field meet. The specific gravity of your sample is the number where this line intersects the UG (urine gravity) scale. Normal urine gravity is between 1.001 and 1.060.
Composition of urine
Urea
Nitrogen
Phosphorous
potassium
Salts
Sodium chloride
Water
Uric acid
Ammonia
Creatinine
Classifications of color of urine
o Darkened urineo Clear urine

o Pink urineo Cloudy urineo Blood urineo Red urineo Orange urine
EXPERIMENT 15
URINE
PROCEDURE
1. Physical Characteristics
Describe the urine specimen as to color, odor, transparency and pH.
Color: Yellow Orange Odor: Strongly Ammonical odor
Transparency: Clear pH: 6
1. Determination of Specific Gravity
Actual specific gravity 1.015
Room temperature 25 0 C
Urinometer temperature 22-25 0 C
Corrected specific gravity 1.015916~1.016
2. Test for Organic Constituents
1. Test for Creatine.

To 5.0 mL urine in a test tube, add 1 mL of saturated picric acid and 1.0 mL of 10% NaOH. Note the color formed. From yellow orange to dark orange.
Describe the resulting solution. Dark orange: Upper layer and a precipitate.
How does creatine form? It is the excretion of the urine wherein when it is added by acid or base it turns to creatine.
2. Test for Urea.
Make 2.0 mL of the urine sample alkaline by adding NaOH; then heat it. Note the odor produced. Test the fumes with moist red litmus paper and a small piece of filter paper wet with a drop of Nessler’s solution. (NOTE: An appearance of reddish orange color in the filter paper indicates the presence of ammonia.)
What did you observe? Odor: Burnt Odor Color of filter paper: reddish orange
Account for such observation. There is presence of Ammonia
3. Test for Inorganic Constituents
1. Test for Chlorides
1. Evaporate 1.0 mL of urine in an evaporating dish in the hood until NaCl crystallizes out. Dissolve in 2.0 mL of distilled water and transfer into small test tubes.
2. Add 2.0 drops of 1.0 M HNO3 and 5.0 drops of 1% AgNO3.
What did you observe? The color became brownish yellow with white ppt.
Write the chemical reaction involved: crystallization of NaCl
2. Test for Carbonates.

To 5.0 mL of urine sample in a test tube, add 10 drops of concentrated HCl. A slight effervescence of carbon dioxide indicates the presence of carbonates.
Observation: A slight effervescence of carbon dioxide formed .
Does the sample contain carbonates? Yes.
How does it appear in urine? It appears by the appearance of slight moistur inside the test tube.
3. Test for Sulfates.
To 5 mL of urine sample, add 1 mL of 10% HCl. Add a few drops of 5% BaCl2. What did you observe? It becomes cloudy yellow solution with white precipitate.
Account for such observation. 5ml urine and 10% HCl = no change but upon addition of 5% BaCl2, it formed a cloudy yellow solution with white precipitate due to the presence of mucus, leukocytes and epithelial cells that settle at the buttom of the container.
4. Test for Pathological Constituents
1. Test for Glucose (Benedict’s Test)
1. To 1.0 mL of urine sample in a test tube, add 5 mL of Benedict;s reagent. Boil in a water bath for 2 minutes. Observation: Turned to cloudy but did not change its color and there is a cloudy settlement at the bottom.
2. Repeat procedures a and b by using 1 mL of pathological urine sample or 1 mL of normal urine with a drop of 5% glucose.
Observation: Slight cloudiness but it did not changed its color, form pale yellow, its color still remain.
Difference: 1 st test tube with Benedict’s reagent: cloudy sediments with a green color settled at the bottom while in 2 nd test tube of 5% glucose with a few white cloudy sediments.

Benedict's reagent is used as a test for the presence of reducing sugars
2. Test for Ketone Bodies (Rothera’s Test)
1. Place 5 mL of urine into a test tube. Add 2 to 3 drops of 5% (NH4)2SO4 and to 2 to 3 drops of 5% sodium nitroprusside. Carefully add 1 mL of concentrated NH4OH and set aside for 2 to 3 minutes before observing.
Observation: Upper- light red
Middle: cloudy light red
Lower: pale yellow
2. Repeat procedure a using 5 mL of pathological urine sample or 5 mL normal urine with 5 drops of acetone. (A red purple ring at the zone of contact is a positive result.)
Observation: No Reaction.
Noted difference from 2-a: Color is still pale yellow.
What is the basis of this test? Rothera's test A test for the presence of ketone bodies, diacetic acid and acetone in urine
3. Test for Protein (Osgood Ruskin Test)
Pour 5 mL of urine sample into a large test tube. Add 1 mL of 5.0% acetic acid and 3 mL of saturated NaCl solution. Using a test tube holder, heat the upper portion of the test tube over the flame. What happened after a few minutes?
Urine + Acetic acid + 3ml sat. NaCl= The color was turn to light yellow instead of dark yellow with tiny bubble.
Repeat using 5 mL of pathological urine sample or 5 mL of normal urine with 5 mL of 5% albumin.
Observation: Forms a cloudy with white precipitate.

Noted difference from that of normal urine: Normal urine was bladder and golden yellow in color white with albumin it turns to pale yellow with white ppt.
4. Test for Bile Acids
Cool the urine sample in an ice bath for about 30 minutes. Sprinkle upon the surface a small amount of finely powdered sulfur. If the bile acids are present, the sulfir sinks at once. If there are no bile acids, the sulfur remains afloat even after gentle shaking. Observation: Before: pale yellow.
Give the function of bile acids: Upon shaking in an ice bath for 30 minutes it becomes lighten addition of sulfur the sulfur doesn’t sink. There are no bile acids. There are some small particles below and some big particles above.
Bile acids serve many functions. They aid in fat absorption (enabling formation of micelles in the
gastrointestinal system) and modulate cholesterol levels by bile acid synthesis.
Bile acids are produced from cholesterol in the liver. Cholesterol is converted to the carboxylic acids cholic and
chenodeoxych-olic acid, which are the primary bile acids in most species.
The liver conjugates the acids to either glycine or taurine and subsequently secre-tes them into the bile.
The gall bladder serves to store bile acids until contraction associated with feeding.In the intestine, ninety-five percent of the bile acids are actively resorbed in the ileum. The remaining five percent is excreted in the feces.
The reabsorbed bile acids are carried to the liver where they are reconjugated and excreted as part of the enterohepatic circulation of bile acids.
The concentration of bile acids in serum from fasting patients tends to be abnormally high when one or more of the following occurs:

Cholestasis causes "regurgitation" of bile acids back into blood (along with conjugated bilirubin).
Reduced functional hepatic mass impairs extraction of bile acids from portal blood.
Congenital and acquired vascular shunts allow an increased proportion of portal blood to bypass the liver.
SUPPLEMENTARY QUESTIONS
1. Discuss urine formation.
The formation of urine had three processes: filtration, reabsorption, and tubular excretion. During filtration, or glomerular excretion, blood pressure forces all the small molecules in the blood into the lumen of the nephron through the pores both in the walls of the glomerular capillaries and in the wall of the Bowman's capsule. The filtrate has the same concentration of dissolved substances as the blood minus the formed elements and the plasma proteins which are too large to fit through the pores of the capillaries and the Bowman's capsule. As the filtrate passes through the tubules of the nephron, water and many dissolved materials are reabsorbed by the blood. In fact, during the filtrate's passage through the tubules up to 99 percent of the water is reabsorbed. In addition, the tubules also remove substances from the blood. This process, called tubular excretion, supplements the initial glomerular filtration.

2. What are the threshold substances?
The threshold substances are the urea, a creatinine, uric acid, sulfates, phenol and other toxic materials.
3. Give the different pathological conditions that can be identified in the urine.
Deviations from normal color that have pathological implications are as follows:
1. Milky: pus, bacteria, fat or chyle

2. Reddish amber: urobilinogen or porphyrin. Urobilinogen is produced in the intestine by the action of bacteria on bile pigment. Porphyrin may be evidence of liver cirrhosis, jaundice, Addison's disease and other conditions.
3. Brownish yellow or green: bile pigments. Yellow foam is definite evidence of bile pigments.
4. Red to smoky brown: blood and blood pigments.
Carrots, beets, rhubarb and certain drugs may color the urine, yet have no pathological significance. Carrots may cause increased yellow color due to carotene; beets cause reddening; rhubarb causes urine to become brown.
Properties of the Cardiac Skeletal Muscle
CENA MJ, DIMABAYAO BT, GARCERA AAC, GUILLERMO MLB, and OMAR AT
Institute of Biology, College of Science, University of the Philippines, Diliman, Quezon City, Philippines 1101
Abstract
Basic properties of cardiac skeletal muscles were observed using frog heart. Hehehe.
INTRODUCTION
The heart is a muscular organ that pumps blood through the body. It consists of chambers connected in series and guarded by valves allowing only unidirectional blood flow (Randall et al. 2001). It is enclosed in a fibrous sac – the pericardium – located in the thorax. A watery fluid fills the space between the pericardium and the heart; functioning as a lubricant as the heart moves within the sac (Vander et al. 2001).
As opposed to the four-chambered mammalian heart, the frog heart only has three chambers: two atria and a single ventricle. The right atrium receives deoxygenated blood from the systemic veins; while the left atrium receives oxygenated blood veins draining the lungs and the skin. Atrial blood from both chambers then flow into a common ventricle. Oxygenated blood is sent relatively pure to carotid arteries which supply the brain. Deoxygenated blood is then sent via pulmocutaneous arteries to the respiratory organs (lungs and skin) where oxygen could be picked

up. Blood passing through the aortic arches, on the other hand, are mixed and are sent to the rest of the body (Kimball 2003).
Much like other tissues of the cardiovascular system, an endothelium lines the inner surface of the heart that is in direct contact with the blood within the chambers. The outer wall or the myocardium, on the other hand, is composed of cardiac muscle arranged in layers and tightly bound together (Vander et al.).
Cardiac muscle combines properties of both skeletal and smooth muscle. As with skeletal muscle, cardiac muscle cells are striated as a result of the arrangement of the thick myosin and thin actin filaments. Unlike skeletal muscle, on the other hand, cardiac muscle fibers are small elongated cells, tapered at both ends and containing only a single nucleus. They are also joined end to end via intercalated disks in which desmosomes function in anchoring while gap junctions function in electrical coupling (Randall et al. 2001; Vander et al. 2001).
Moreover, cardiac muscle contraction is myogenic rather than neurogenic. This means that contraction is initiated in the muscle fibers themselves as electrical signals arise endogenously in pacemaker fibers and spread as action potentials through the heart via the gap junctions (Randall et al. 2001). In the frog heart, the pacemaker is the sinus venosus – a bulbous region found between the vena cava and the right atrium (Richard 2003).
In this experiment, some properties of the cardiac muscle are demonstrated. The effect of temperature on the firing of the sinus venosus pacemaker is evaluated. The contractile responses to different electrical stimuli are also observed as the refractory period and the all-or-none response is exhibited. Moreover, the effects of adrenaline, acetylcholine, and other chemical solutions on heart contraction and beating are investigated.
The frog heart is used in this experiment as it functions well at room temperature and will continue to beat even when excised from the body (Richard 2003).
METHODOLOGY
Preparation. The marine toad (Bufo marinus) was used in this study to observe the effects of various stimuli on the cardiac muscles. All toads used were double-pithed prior to dissection. In most of the experiments, the heart was completely exposed from the pericardium. In order to detect heart contractions, the apex of the heart was attached in a vertical upward position to a transducer, which converts mechanical signals to analogue signals. This was in turn attached to a Powerlab hardware that converts analogue signals to digital signals. These digital signals are then transmitted on to a computer screen, via the Chart for Windows version 4.2.4 software.
The effect of temperature, chemical control, inorganic ions, and electric shock on the different phases of heart contraction was observed (Table 1). Changes in the heart rate, amplitude, and duration of contraction was recorded for each condition.
Table 1: The various conditions used to observe the effect of different stimuli on the behavior of cardiac muscles.

Stimuli Conditions
Temperature 1. Warm Ringer’s solution on the sinus venosus
2. Warm Ringer’s solution on the atrium
3. Warm Ringer’s solution on the ventricle
4. Cold Ringer’s solution
Chemical 1. 1% Acetylcholine2. Adrenalin followed by 1%
Acetylcholine3. 0.5% Atropine
Electric Shock
1. Early systole2. Middle systole3. Late systole4. Early diastole5. Middle diastole6. Late diastole
Inorganic Ions
1. Ringer’s Solution2. 0.7% NaCl3. Ringer’s Solution4. 0.9% KCl5. Ringer’s Solution6. 1% CaCl2
7. Distilled Water
Temperature. After normal heart contractions were observed, the effect of different temperatures on heart contraction was examined (Table 1). Following this, the heart was rinsed with Ringer’s solution at room temperature until the normal beat was restored.
Chemical control of the heart. For the chemical control of the heart, 2-3 drops of 1% acetylcholine and adrenalin, and 5 drops of atropine were applied to the heart. Ringer’s solution was in between treatments to be able to wash off the remnants of the solution/s previously added. The duration of the effect of each chemical was recorded (until normal heart rates were again observed).

Refractory period of the heart. The ventricle of the heart was stimulated at six different phases of its cycle, using single-shock stimulus, at a rate of 1 stimulation per cycle. The occurrence of premature and compensatory contractions were recorded.
Effect of Inorganic Ions. For this experiment, the heart was completely excised from the toad’s body, and placed in Ringer’s solution. The solutions for the inorganic ions used (Table 1) were placed in four small beakers. The heart was immersed into each solution (in chronological order, from a-e), where the number of beats per minute was counted.
All or None Law. In this experiment, the ventricle was isolated from the rest of the heart, with its apex connected to the transducer, and the base pinned on to a dissecting pan. Electric shock was used to stimulate its contraction. After the threshold was determined, the strength of the current used was increased. The response of the ventricle was then recorded.
RESULTS
Normal cardiac activity was recorded (Figure 1), and the normal heart rate at the beginning of the experiment was determined to be 0.97 beats per second. The ventricular and the atrial contractions were observed in each contraction.
Temperature. A general increase in the heart rate of the frog was observed with the application of warm Ringer’s solution to the different heart chamber, while slower rate was seen observed when cold Ringer’s solution was applied. Application of warm Ringer’s solution to the sinus venosus of the heart elicited an increase in the heart rate to 1.2 beats per second (Figure 2B). When applied to the atrium, heart rate was found to be 1.0 beat per second (Figure 2C). The same rate, at 1 beat per second was obtained when it was applied to the ventricle of the heart (Figure 2D). Upon the application of cold Ringer’s solution, the heart rate slowed down to 0.57 beats per second (Figure 2E).
Chemical Control of the Heart. Prior to testing for the effects chemicals on the activity of the heart, the distance between each peak during normal heart activity was measured and was determined to be at 1.2 cm (Figure 3A). The application of acetylcholine elicited an immediate decrease in heart rate, showing a distance of 3.2 cm between peeks (Figure 3B). Normal heart rate was restored only after 6.63 minutes.
Application of adrenalin, followed by a subsequent application of acetylcholine showed a preliminary increase in heart rate (due to adrenalin), followed by a marked decrease in heart rate (due to acetylocholine) (Figure 3C). Application of atropine on the heart showed no apparent effect on the rate of heart contraction.
Refractory Period of the Heart. The refractory period of the heart was observed during the middle (Figure 4A) and late diastole (Figure 4B). No observations were made during the early, middle, and late systole, as well as during the early diastole.


F
Figure 1: (A) The normal cardiac activity, showing the ventricular and atrial contractions in each cycle. (B) A section of the normal cardiac activity showing one cycle.
igure 1: The normal cardiac activity, showing the ventricular and atrial contractions in each cycle. (B) A section of the normal
Figure 2: The effect of temperature on the activity of the activity: (A) normal cardiac activity, (B) application of warm Ringer’s solution to the sinus venosus, (C) application of warm Ringer’s solution to the atrium, (D) application of warm Ringer’s solution to the ventricle, (E) application of cold Ringer’s solution.

Figure 3: Chemical control on the heart. (A) shows the normal contraction of the heart, without the addition of any chemicals, (B) shows the decrease in heart rate after the addition of 1% acetylcholine, (C) shows the increased heart rate due to the application of adrenalin, followed by a decrease in heart rate from the application of acetylcholine, while (D) shows no apparent difference in the heart rate upon the addition of atropine.
Figure 4: The refractory period of the heart, as shown by electric stimulation during the (A) middle diastole of ventricular contraction, and the (B) late diastole of ventricular contraction. The premature contraction after each stimulation followed by the compensatory period is also shown.

Figure 5: The all or none law, showing stimulation at (A) threshold (2V), and increasing voltages at (B) 3V, (C) 5V, (D) 6V, (E) 7V, and (F) 10V.
Table 2 : The effect of inorganic ions on the activity of the heart; heart contractions are measured in beats per minute (BPM).
Solution BPM
Ringer's solution 59
0.7% NaCl 45
Ringer's solution 55
0.9% KCl 27

Ringer's solution 8
1% CaCl2 30
Ringer's solution 32
Dist. H20 26

Premature contractions were seen after stimulations conducted during middle and late diastole, followed by compensatory contractions. No premature contractions were observed during early, middle and late systole, as well as during the early diastole.
Effect of Inorganic Ions. The effect of inorganic ions on the excised heart can be seen in Table 2. Heart rate increased when placed in the NaCl solution, and decreased considerably when immersed in KCl, in many cases, the heart even ceases to beat after its immersion in KCl, and again in increases when immersed in CaCl2. Cardiac activity was observed to return to normal when placed in Ringer’s solution.
All or None Law. After the threshold level of the cardiac muscle was determined at 2V, increase in electric shock was performed up to 10 V (Figure 5). The cardiac was observed to respond at these very high voltages, illustrating the all or none law.
DISCUSSION
Blah blah blah
LITERATURE CITED
Ito ang lit cited ng intro. Yung lit cited sa discussion plus sa questions incorporate mo nlng.
Kimball JW. 2003. “Animal Circulatory Systems.” Available from: users.rcn.com/jkimball.ma.ultranet/BiologyPages/A/AnimalHearts.html. Accessed 05 March 2008.
Randall D, Burggren W, and French K. 2001. Eckert Animal Physiology: Mechanisms and Adaptations. 5th ed. W.H. Freeman and Co.
Richard DS. 2003. “Cardiac Muscle Physiology.” Available from: http://www.susqu.edu/FacStaff/r/richard/Frog%20heart.html. Accessed 05 March 2008.
Vander AJ, Sherman J, and Luciano D. 2001. Human Physiology: The Mechanism of Body Function. 8th ed. McGraw-Hill Co.
GENERAL ANESTHESIA
Surgery 2General Anesthesia

I. Principles of General Anesthesia
II. Pharmacology in General Anesthesia
III. Conduct of General Anesthesia
IV. Complications of General Anesthesia
I. PRINCIPLES OF GENERAL ANESTHESIA
General Anesthesia
“General Anesthesia is a drug-induced loss of consciousness during which patients are not arousable, even by painful stimulation. The ability to independently maintain ventilatory function is often impaired. Patients often require assistance in maintaining a patent airway, and positive pressure ventilation may be required because of depressed spontaneous ventilation or drug-induced depression of neuromuscular function. Cardiovascular function may be impaired.”
CONTINUUM OF DEPTH OF SEDATION: DEFINITION OF GENERAL ANESTHESIA AND LEVELS OF SEDATION/ANALGESIA*
Minimal Sedation
Analgesia
Moderate Sedation (Conscious Sedation)
Deep Sedation
(Anxiolysis)
General Anesthesia / Analgesia
Responsiveness Normal response to verbal stimulation
Purposeful response to verbal or tactile stimulation
Purposeful response following repeated or painful stimulation
Unarousable even with painful stimulus
Airway Unaffected No intervention required
Intervention may be required
Intervention often required
Respiratory Function
Unaffected Adequate May be inadequate
Frequently inadequate
Cardiovascular Function
Unaffected Usually maintained
Usually maintained
May be impaired

Stages of General Anesthesia
Stage 1 (amnesia)o From induction of anesthesia to loss of consciousness (loss of eyelid reflex)o Pain perception threshold is not lowered.
Stage 2 (delirium/excitement)o Characterized with uninhibited excitation, agitation, delirium, irregular respiration and breath holdingo Pupils are dilated and eyes are divergento Responses to noxious stimuli can occur: vomiting, laryngospasm, hypertension, tachycardia, and
uncontrolled movements
Stage 3 (surgical anesthesia)o characterized by central gaze, constricted pupils, and regular respirationso Painful stimulation does not elicit somatic reflexes or deleterious autonomic responses.o Target depth of anesthesia is sufficient when painful stimulation does not elicit somatic reflexes or
deleterious autonomic responses. Stage 4 (impending death/overdose)
o characterized by onset of apnea, dilated and nonreactive pupils, and hypotensiono may progress to circulatory failure
Minimum Alveolar Concentration (MAC)
the minimum concentration necessary to prevent movement in 50% of patients in response to a surgical skin incision The lower the MAC, the more potent the agent MAC values for different volatile agents are additive
MAC awake concentrations required to prevent eye opening on verbal command

(50% MAC)
MAC Endotracheal Intubation Concentrations required to prevent movement and coughing in response to endotracheal intubation (130% MAC)
MAC BAR Concentrations required to prevent adrenergic response to skin incision (Blockade of autonomic response) (150% MAC)
MAC Amnesia concentration that blocks anterograde memory in 50% of awake patients (25% MAC)
**remember: there is no such thing as twilight anesthesia!
Meyer-Overton Hypothesis
The MAC of a volatile substance is inversely proportional to its lipid solubility (oil:gas coefficient) High MAC equals low lipid solubility
Backtrack:
MAC is inversely related to potency (high MAC equals low potency)
Correlation between lipid solubility with potencyo onset of anesthesia occurs when sufficient molecules of the agent have dissolved in the cell's lipid
membraneso High lipid solubility equals high potency (and low MAC)

Potency
Factors Affecting the Meyer - Overton Hypothesis
Convulsant propertieso Complete halogenation, or complete end-methyl halogenation of alkanes and ethers results in decreased
anesthetic potency and appearance of convulsant activity
Specific Receptorso e.g. opioid receptorso there is reduction of MAC by opioids
suggests two sites of action: the opioid receptor and some hydrophobic site. For a given MAC reduction, plasma levels of morphine, alfentanyl, sufentanyl and fentanyl
vary around 5000 fold. Levels of these four agents in brain lipid vary 10 fold Dexmedetomidine ( D-medetomidine)
o an alpha-2- agonist, results in marked reduction in MAC, whereas its optical isomer, with identical lipid solubility, has no effect.
Hydrophilic site of actiono correlation between ability to form clathrates and anesthetic potencyo Clathrates (of water) are postulized to alter membrane ion transporto anaesthetic molecules act as seeds for crystals of water, which subsequently alter membrane ion transport
Blood/gas (B/G) solubility coefficient
a measure of the uptake of an agent by blood less soluble agents (lower B/G solubility coefficients), such as nitrous oxide and desflurane, are associated with more
rapid induction and emergence.

II. OVERVIEW OF PHARMACOLOGIC AGENTS USED IN GENERAL ANESTHESIA
Inhaled Anesthetics Intravenous induction Agents Neuromuscular Blocking Agents Opioids Benzodiazepines Anticholinergic agents Anticholinesterases
INHALATIONAL AGENTS
Used in the induction and maintenance of anesthesia Halogenated alkane or ether-derived compounds Nitrous oxide (N2O; laughing gas) is the only inorganic anesthetic gas in clinical use Produce dose-dependent systemic effects Associated with Malignant Hyperthermia Examples:
o Ethero Halothaneo Methoxyfluraneo Enfluraneo Isofluraneo Sevofluraneo Desfluraneo Nitrous Oxideo Xenon
Summary of physical properties of volatile anesthetics
Halothane Isoflurane Enflurane Desflurane Sevoflurane
Molecular weight 197 184 184 168 200
Boiling point (°C) 50.2 48.5 56.5 22.8 58.5
Saturated vapor pressure at 20°C
243 238 175 669 157
MAC in 100% O2 0.75 1.15 1.8 6 2.05
% Biotransformation
20 0.2 2 <0.1 3 - 5
Blood / gas 2.2 1.36 1.91 0.45 0.6

Oil / gas 224 98 98.5 28 47
AGENT ADVANTAGE DISADVANTAGE
Nitrous Oxide (aka cyclopropane, laughing gas)
Analgesia
Minimal cardiac
Respiratory depression
Alters methionine synthetase production teratogenic effects
Polyneuropathy
Sympathetic stimulation
Expansion of closed air space
Chloroform Hepatic toxicity
Fatal cardiac arrhythmia
Halothane Effective in low concentrations
Minimal airway irritability
Inexpensive
Pleasant odor
Most potent volatile anesthetic in modern practice
Associated in hepatitis, malignant hyperthermia; cardiac depression and arrhythmia; hepatic necrosis;
Slow elimination
Methoxyflurane Fluoride nephrotoxicity
Enflurane Muscle relaxation
No effect on cardiac rate or rhythm
Induce epileptiform EEG changes
Strong smell
Seizures
Isoflurane Muscle relaxation
No effect on cardiac rate or rhythm
Coronary steal (the term given to blood being stolen from one region of the coronary tree by another)
Strong smell

INHALATIONAL AGENT
BLOOD PRESSURE HEART RATE
CARDIAC OUTPUT
VENTILATORY DEPRESSION BRONCHODILATION
Nitrous oxide Little effect Little effect Little effect Minimal No
Halothane Marked dose-dependent decrease
Moderate decrease
Marked dose-dependent decrease
Moderate dose-dependent effect
Moderate
Enflurane Marked dose-dependent decrease
Moderate decrease
Moderate dose-dependent decrease
Marked dose-dependent effect
Minimal
Isoflurane Moderate dose-dependent decrease
Variable increase
Minimal decrease
Marked dose-dependent effect
Moderate
Sevoflurane Moderate dose-dependent decrease
Little effect Moderate dose-dependent decrease
Moderate dose-dependent effect
Moderate
Desflurane Minimal decrease
Variable; marked increase with rapid increase in concentration
Minimal decrease
Marked dose-dependent effect
Moderate
Ethero characterized by notoriously slow induction and equally delayed emergence but could produce
unconsciousness, amnesia, analgesia, and lack of movement without the addition of other agents
ANESTHETIC POTENCY
SPEED OF INDUCTION AND EMERGENCE
SUITABILITY FOR INHALATIONAL INDUCTION
SENSITIZATION TO CATECHOLAMINES
METABOLIZED (%)
Nitrous oxide Weak Fast Insufficient alone None Minimal
Diethyl ether Potent Very slow Suitable None 10
Halothane Potent Medium Suitable High 20+
Enflurane Potent Medium Not suitable Medium <10
Isoflurane Potent Medium Not suitable Minimal <2
Sevoflurane Potent Rapid Suitable Minimal <5
Desflurane Potent Rapid Not suitable Minimal 0.02

INTRAVENOUS INDUCTION AGENTS
Used as premedications, sedatives, intravenous induction agents and in the maintenance of anesthesia. Total intravenous anesthesia (TIVA) Examples:
o Barbiturates (Thiopental, thiamylal, and methohexital)o Benzodiazepines (Midazolam)o Ketamineo Etomidateo Propofol
Thiopentalo mechanism of action is at the gamma-aminobutyric acid (GABA) receptor, where they inhibit excitatory
synaptic transmissiono Redistribution of the agent from the brain to peripheral tissues, particularly fat associated with rapid
emergenceo Hepatic elimination about 10% per houro Can cause hypotension, vasodilation and cardiac depressiono Can precipitate bronchospasm in patients with reactive airway diseaseo Decreases CMRO2 in neuroanesthesia
Ketamineo Produces dissociative state of anesthesiao Only IV induction agent that increases blood pressure and heart rateo Decreases bronchomotor toneo May be used as sole anesthetic for short procedureso Produces profound amnesia and analgesiao Increases intracranial pressureo Produces emergence delirium and bad dreamso least amount of ventilatory depression and loss of airway reflexeso administered with a drying agent such as glycopyrrolate due to induction of copious oropharyngeal
secretions
Propofol (2,6-diisopropylphenol)o Short-acting induction agento Available as oil-in-water emulsion containing soybean oil, glycerol, and egg lecithino Ideal for ambulatory surgeryo Can decrease blood pressure in susceptible patientso Produces bronchodilatationo Associated injection pain
Etomidateo Imidazole compoundo Produces minimal hemodynamic changes (ideal for patients with cardiovascular disease)

o Produces pain on injection, abnormal muscular movements and adrenal suppression
Midazolamo A benzodiazepine (Other BZD: Diazepam, Lorazepam)o Because of minimal cardiovascular effects, used for anesthesia inductiono Produces anxiolysis and profound amnesiao Also used as a premedicant
OPIOIDS
Used as part of general anesthesia, and in patients receiving regional anesthesia Produces profound analgesia and minimal cardiac depression Cause ventilatory depression Classification of opioids
Traditional Origin Function
Strong
Morphine
Pethidine
Fentanyl
Alfentanil
Remifentanil
Sufentanil
Intermediate
Buprenorphine
Pentazocine
Butorphanol
Nalbuphine
Weak
Codeine
Naturally occurring
Morphine
Codeine
Papavarine
Thebaine
Semisynthetic
Diamorphine
Dihydrocodeine
Buprenorphine
Synthetic
Phenylpyperidines:
pethidine, fentanyl, alfentanil,
sufentanil
Diphenylpropylamines:
methadone, dextropropoxyphene
Morphinans:
Pure agonists
Morphine
Fentanyl
Alfentanil
Remifentanil
Sufentanil
Partial agonist
Buprenorphine
Agonists-antagonists
Pentazocine
Nalbuphine
Nalorphine
Pure Antagonists
Naloxone
Naltrexone

butorphanol, levorphanol
Benzomorphans:
pentazocine
Opioid Receptors
DOP (delta opioid peptide receptor) [δ1, δ2]
analgesia
antidepressant effects
physical dependence
KOP (kappa opioid peptide receptor) [κ1, κ2, κ3]
Spinal analgesia
sedation
miosis
inhibition of ADH release
MOP (mu opioid peptide receptor)
[μ1, μ2, μ3]
μ1:
Supraspinal analgesia
physical dependence
μ2:
respiratory depression
miosis
euphoria
reduced GI motility
physical dependence
μ3:
?

NOP (nociceptin orphanin FQ peptide receptor)
[ORL1]
anxiety
depression
appetite
development of tolerance to μ agonists
Most commonly used:
o Agonists: Morphine, Fentanyl, Meperidineo Antagonists: Naloxone, Naltrexoneo Agonist-Antagonist: Nalbuphine, Butorphanol
Uses in General Anesthesiao Reduces MAC of potent inhalational agentso Blunt the sympathetic response (increase in BP and HR) to direct laryngoscopy, intubation and surgical
incisiono Provide analgesia extending into postoperative periodo May be used as complete anesthetics (may provide analgesia, hypnosis and analgesia)o May be added in local anesthetic solutions in regional anesthesia to improve quality of analgesia

NEUROMUSCULAR BLOCKING AGENTS
o Uses in anesthesia Facilitates endotracheal intubation Provides muscle relaxation necessary for the conduct of surgery
Types: (Review Pharmacology)o DEPOLARIZING (non-competitive) AGENTS
exert agonistic effects at the cholinergic receptors of the neuromuscular junction, initially causing contractions evident as fasciculations, followed by an interval of profound relaxation
Succinylcholine: mimics the action of acetylcholine by depolarizing the postsynaptic membrane at the neuromuscular junction (non-competitive antagonism)
Advantages of Succinylcholine Rapid onset, short duration of action Used in rapid-sequence induction
Adverse effects of Succinylcholine Bradycardia (esp. in pediatrics) Life-threatening hyperkalemia in burn patients May trigger malignant hyperthermia Myalgia (from fasciculations) and myoglobinuria Increased ICP, CBF, IOP Increased intragastric pressure Prolonged blockade in susceptible individuals (in decreased plasma
cholinesterase activity, myopathies)
o NON-DEPOLARIZING AGENTS
Produces reversible competitive antagonism of Ach Compete for receptor sites with acetylcholine, with the magnitude of block dependent
on the availability of acetylcholine and the affinity of the agent for the receptor. May be aminosteroid or benzylisoquinoline compounds Used when succinylcholine is contraindicated Choice of agent
Based on mode of excretion Hoffman degradation (atracurium, cis-atracurium) Renal Hepatic
Based on duration of action
Short acting: Mivacurium Intermediate: Atracurium, Rocuronium Long-acting: Pancuronium
Concerns in anesthesia (neuromuscular blocking agents) Paralysis can mask signs of inadequate anesthesia Higher doses required for intubation than for surgical relaxation Other drugs can potentiate effects of non-depolarizing agents Variable individual responses Residual blockade may result to postoperative problems

TOF monitoring Clinical assessment
ANTICHOLINERGICS
competitively inhibits the action of acetylcholine at muscarinic receptors with little or no effect at nicotinic receptors. Examples:
o Atropine*, Scopolamine§, Glycopyrrolate¤
Uses in anesthesia:o Amnesia and Sedation§
o Antisialogogue effect §*¤
o Tachycardia*o Bronchodilation*
ANTICHOLINESTERASES
Inactivate acetylcholinesterase by reversibly binding to the enzyme increasing the amount of acetylcholine available to compete with the nondepolarizing agent
Increases acetylcholine at both nicotinic and muscarinic receptors Muscarinic side effects can be blocked by administration of atropine or glycopyrrolate Examples:
o edrophonium, neostigmine, pyridostigmine, physostigmine Use in anesthesia: reversal of neuromuscular blockade
III. CONDUCT OF GENERAL ANESTHESIA
Induction Techniques Intubation Maintenance Emergence and Extubation
Patient Monitoring in Anesthesia
Routine

Pulse oximetry Automated BP ECG Capnography Oxygen analyzer Ventilator pressure monitor Thermometry
Specialized
Foley catheter Arterial catheter Ventral venous catheter Pulmonary artery catheter Precordial doppler Transesophageal Echocardiography Esophageal Doppler Esophageal and Precordial Stethoscope
Airway Examination

Mallampati Scoreo The patient is asked to maximally open his mouth and protrude his tongue while in the sitting position
Class 1 Faucial pillars, uvula, soft palate seen
Class 2 Uvula masked by tongue base
Class 3 Only soft and hard palate visualized
Class 4 Only hard palate
Interdental Distance (3)o Measures the distance between the 2 incisors, with the mouth fully opened
Thyromental Distance (3)o Measures the distance between the chin (mentum) and the thyroid cartilage
Thyrohyoid Distance (2)
o Measures the distance between the hyoid and the thyroid cartilage

Bellhouse-Doreo maximal flexion and extension of the neck will identify limitations that might prevent optimal alignment of
the OPL axes.
* Normal atlanto-occipital joint: 35 degrees of extension

Strategies in General Anesthesia
Questions to ask prior to conduct of anesthesia:o Is the patient’s condition or scheduled surgery require additional monitoring techniques?o Does the patient have conditions that contraindicate certain drugso Is endotracheal intubation required?o Are there anticipated difficulties in oral translaryngeal intubation?o Are NMBs required during surgery?o Are there special surgical requirements that mandate use of or avoidance of specific interventions? (e.g.
NMBs)o Is substantial blood loss or fluid shifts anticipated?
Induction of Anesthesia
Sequence of interventions during induction vary depending on the patient and type of surgery Concerns
o Loss of consciousnesso Inability to maintain a natural airwayo Reduction or cessation of spontaneous ventilationo Use of drugs that may depress the myocardium and change vascular tone
Awake Intubation
May be supplemented with sedatives, opioids, and topical or local anesthesia Accomplished via “blind” nasal, fiberoptic bronchoscopy, and direct visualization Indications:
inadequate mouth opening facial trauma cervical spine injury chronic cervical spine disease lesions in the upper airway
Nasal Intubationo Endotracheal tube (ET) is inserted through the nose and guided into the tracheal by listening to the
transmitted breath soundo Fiberoptic intubation
o Passing an ET through the nose or mouth into the pharynx, then passing a bronchoscope through the tube. The larynx and the trachea are visualized and the ET is thread over the bronchoscope
Intravenous Induction
Disadvantageso Spontaneous ventilation is abolished without certainty that patient can be manually ventilatedo Endotracheal intubation is performed while the patient is lightly anesthetized, precipitating hypertension,
tachycardia, or bronchospasm

o What to do if the patient can’t breathe, and you can’t intubate? Pray!
Inhalational Induction
May be used in children and cooperative adults Disadvantages
o Depending on the induction agent, patients progress from the awake state to surgical level of anesthesia.o Stage 2 anesthesia prodispose the patient to laryngospasm, vomiting and aspiration
Agents used for Inhalational induction:o Sevofluraneo Halothane

Rapid Sequence Induction
Indicated for patients at high risk for acid aspiration Examples
o Obese patientso Pregnant patientso History of gastroesophageal reflux diseaseo Patients with bowel obstruction
Sellick’s Maneuver:o pressure on the cricoid cartilage to occlude the esophagus, thus preventing passive regurgitation from the
stomach to the pharynx

Combined Intravenous and Inhalational Anesthesia
Agents are combined to gain advantage of smooth and rapid hypnosis but still permit establishment of deep level of inhalational anesthesia prior to airway instrumentation
Techniques in Managing Airway Obstruction (please refer to the Anesthesia rotation handout for further description)

Chin tilt Extension of neck Anterior displacement of mandible Use of airway adjuncts (oral and nasal airway) Use of supraglottic airway (e.g. LMA)
Orotracheal Intubation Technique
Position the Patiento Sniffing Positiono Pads and Pillows
Open the mouth Insert the laryngoscope blade Sweep the tongue from right to left Identify landmarks Advance the laryngoscope blade
o Macintosh blade: valleculao Miller blade: epiglottis
Identify and elevate the epiglottis Visualize the vocal cords and glottic opening
Insert the endotracheal tube from the corner of the mouth Advance the tube into the glottic opening Withdraw laryngoscope blade Ventilate Confirm tube placement Inflate ET balloon cuff Secure the endotracheal tube Periodically check tube
Confirmation of Successful Endotracheal Intubation
Direct visualization of the ET tube passing though the vocal cords. Carbon dioxide in exhaled gases (documentation of end-tidal CO2 in at least three consecutive breaths). Maintenance of arterial oxygenation. Bilateral breath sounds. Absence of air movement during epigastric auscultation. Condensation (fogging) of water vapor in the tube during exhalation. Refilling of reservoir bag during exhalation. Chest x-ray: the tip of ET tube should be between the carina and thoracic inlet or approximately at the level of the
aortic notch or at the level of T5.

Maintenance of Anesthesia
Goalso Facilitate surgical exposureo Ensure adequate amnesiao Ensure adequate analgesia
Parameters used in assuring adequacy of anesthesia:
o Autonomic signs (BP, HR, RR)o Monitoring of Neuromuscular Blockadeo BIS Monitoring (for awareness)
TITRATABLE COMBINATION OF:
IV opioids (e.g. fentanyl) IV sedative-hypnotics (e.g. midazolam) O2+volatile agent Nitrous oxide
NITROUS-NARCOTIC TECHNIQUE:
IV opioids IV sedative-hypnotics O2+ Nitrous oxide
TOTAL INTRAVENOUS ANESTHESIA: (TIVA)
IV sedative-hypnotics (e.g. propofol) via infusion or TCI IV short-acting opioids + NMBs (in patients requiring intubation/muscle relaxation)
Emergence and Extubation

requires the knowledge and experience with the pharmacokinetic and pharmacodynamic principles that underlie the elimination of inhalational and intravenous agents and that govern the reversal of neuromuscular blockade
Parameters for Extubation:o Patient follows commandso Active spontaneous respirationo Ability to protect the airway (reflexes)
Deep extubation
o Used in patients at risk for bronchospasm with stimulation of the trachea during emergence from anesthesia
Criteria for Extubation
awake and responsive patient stable vital signs reversal of paralysis good hand grip sustained head lift for five seconds Negative inspiratory force > -20 mmHg vital capacity >15 ml/kg Other Concerns:
o Aspiration risk

o Airway patency Subjective Clinical Criteria:
o Follows commandso Clear oropharynx/hypopharynx (e.g., no active bleeding, secretions cleared)o Intact gag reflexo Sustained head lift for 5 seconds, sustained hand graspo Adequate pain controlo Minimal end-expiratory concentration of inhaled anesthetics
Objective Criteria:o Vital capacity: ≥10 mL/kgo Peak voluntary negative inspiratory pressure: >20 cm H2Oo Tidal volume >6 cc/kgo Sustained tetanic contraction (5 sec)o T1/T4 ratio >0.7o Alveolar-Arterial Pao2 gradient (on FIO2 of 1.0): <350 mm Hgao Dead space to tidal volume ratio: ≤0.6a
IV. COMPLICATIONS OF GENERAL ANESTHESIA
INDUCTION
Individual variable response to drugs Depression of the CNS / respiratory / cardiovascular systems Hypersensitivity reactions Aspiration Problems in ventilation
Hypoxemia Hypercarbia Obstruction Difficult ventilation

INTUBATION
Physiologic Responses
Hypertension, Tachycardia Laryngospasm Bronchospasm
Airway Trauma
Injury to teeth and airway tissues Tracheal and laryngeal trauma Post-intubation hoarseness and sore throat Difficult intubation
Tracheal Tube Positioning
Endobronchial Intubation Esophageal Intubation Inadequate insertion depth
MAINTENANCE
Individual Variable response Hypersensitivity reactions Depression of the CNS / respiratory / cardiovascular systems Inadequate depth of anesthesia Awareness
EXTUBATION
Aspiration Laryngospasm Airway trauma Residual Neuromuscular Blockade Delayed Emergence
OTHERS

Peripheral Nerve Palsies Corneal Abrasions