Non immuine hydrops fetalis
-
Upload
varsha-deshmukh -
Category
Healthcare
-
view
173 -
download
0
Transcript of Non immuine hydrops fetalis
HISTORY
• 25 Yrs. Old• 7 Months Amenorrhoea• Swelling of Feet 1 month• Headache 3 days
OBST. HISTORY
• G5 P4 L1 A0• First 3 Preterm deliveries all died.• 4th FTND 3 year old female live KAY
GENERAL EXAMINATION• GC Moderate, afebrile, pulse 96 /min., BP – 150/110 mm.Hg.• Pallor +, Edema +• CVS, RS wnl • Per abdomen • Ut over distended, tense, fetal parts not felt, FHS CNL• Per Vaginum Cx 1 Fl, 60 % Effaced, Membranes + breech at – 2 St.• Pelvis adequate • Provisional Diagnosis G5 P4 L1 A0, Sev. PIH, ? Twins ? Hydramnios• Ultrasonography KAY
LABOUR NOTES
• Preterm Vaginal Delivery on 11/7/2003 (within 7 hrs.of active labour)
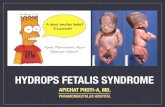
• Female child 2200 gm., MSB, e/o Hydrops Fetalis +
• Hyperplacentosis +, WT 1500 gm
KAY
INVESTIGATIONS
• Bld gr Orh+ve • Hemogram Normal • LFTs, KFTs Wnl • BSL Normal• Urine Exam. Normal• Findings of neonatal autopsy :• Macerated baby, distension of abd, edema all over body, peeling of skin.• Pericardial effusion, fluid in peritoneal cavity 200 cc.• Congested liver, lungs, spleen, kidneys• diagnosis – non immunize hydrops fetalis
KAY
INTRODUCTION
Potter in 1943 described clinical entity, thataffected non-Rh sensitised pregnancies,
NIH –1) Fetal ansarca.2) Placental oedema3) Fetal serous effusions
NIH does not represent a specific disease. “Late manifestation of many severe diseases”. KAY
ETIOLOGY
• Cardiovascular anomalies - tachyarrhythmia, Anatomic defects
• Chromosomal - Down syndrome, Turner Syndrome.
• Malformation syndrome• Twin pregnancy- Twin transfusion
syndrome• Hematologic - Arteriovenous shunt• Genitourinary - Congenital nephrosis
KAY
ETIOLOGY
• Respiratory - Pulmonary hypoplasia• Gastrointestinal• Liver• Maternal - Severe diabetes mellitus,
severe anemia, Hypoproteinemia• Placenta-umbilical cord - Chorionic vein
thrombosis• Medications - Antepartum indomethacin• Infectious - Parvovirus B 19, TORCH• Miscellaneous KAY
DIAGNOSIS
• Ultrasound evaluation.
• Skin thickness more than 5 mm.
• Placental thickness more than 4 cm
• Ascitis, pericardial effusion, pleural effusion.
• Polyhydramnios. KAY
MANAGEMENTAll NIH should be referred to a unit where
facilities exist for detailed anomaly scans including - echocardiography, fetal blood sampling and tertiary neonatal care.
Principles of Management• If detected at <20 wks option for
termination of pregnancy given.• Establish underlying cause• Determine appropriate therapy & optimal
timing of therapy.Prognosis :Overall mortality ranges 50% - 90% .
CONCLUSION
• USG has a pivotal role in diagnosis.• Generalised lymphoedema has a poor
prognosis • Cardiovascular anomalies is the most
identifiable cause. Arrhythmias are amenable to therapy.
• Knowledge of etiology and fetal karyotype will determine whether aggressive management is warranted.
• Parent’s of affected child, need counselling regarding accurate diagnosis and prognosis.