Neonatal resuscitation 2012 AG
-
Upload
akshay-golwalkar -
Category
Healthcare
-
view
2.556 -
download
1
Transcript of Neonatal resuscitation 2012 AG

Neonatal Resuscitation
Presented By Dr. Akshay Golwalkar
Moderated By Dr. Sunil Gavhane

FACTS• 90% Don’t require any intervention
• 10% require intervention
• 1 % need major resuscitation
• Preterms are at high risk

How often do we use our resuscitation skills?

Primary causes of death*
18 %Other causes09 %Malformation29 %Perinatal hypoxia17 %Infection27 %Prematurity
DeathsCause
*Text book of Neonatal Resuscitation 6th edition

Alveoli are fluid filled
Blood vessels are constricted

After birthFluid in the alveoli is absorbed
Alveoli • Expand• Get filled with Air
1.

2.
Pulmonary vessels dilate, causing increased blood flow to lungs

Requirements• Personnel
– At least one trained person for all deliveries
– Two persons, if high risk; or for advanced resuscitation


Bag, Mask, & Oxygen
Suction Equipment
Laryngoscope and ETT Tube
Warmer & Blankets

Resuscitation
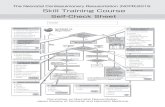
•Is the newborn term?
•Is the newborn breathing or crying?
•Does the newborn have good muscle tone?
•Dry & remove wet cloth•Clear airway if necessary•Wrap in prewarmed dry cloth•Breast feeds •Ongoing Evalution
YES
Baby is Delivered ( Ask)
Routine Care


Dry & Remove wet linen

Routine Care• Vigorous term infants with no risk factors• Babies who required but responded to initial steps, They
now can stay with Mother • Skin to skin contact recommended • Clear airway, dry newborn, provide ongoing evaluation:
– Breathing – Activity – Color
• Transfer to New Born Nursery


Positioning

Clear Airway, if necessary

Clear airways(if necessary)

Oral Suctioning
Deep suction should be performed

Stimulate

• Breathing : Regular / Gasping / Irregular / Absent
• Heart Rate : >100/m OR< 100/m OR Absent
• SpO2
EVALUATE


Pulse Oximetry: Resuscitation monitor
• Advantageso Not affected
by acrocyanosis
o Be patient and get a reading


Supplemental oxygen
Free-flow oxygen cannot be given reliably by a mask attached to a self-inflating bag

PPV/Bag & mask ventilation

•HR below 100•Apnoea/gasping
YES
•Start PPV•Consider SpO2 monitering

Indications for Bag & Mask ventilation
• Apnea or gasping respirationOR
• Heart rate < 100 bpmOR
• Saturation below target values despite free flow supplemental oxygen

Key point
The most important and effective action in neonatal resuscitation is
EFFECTIVE Ventilation

Selecting equipment
• Size of bag (200-750 ml) : To deliver a tidal volume of 6-8
ml/kg
• Oxygen capability : Oxygen source, reservoir

Oxygen Reservoirs

Safety features
Pop-up valve

Testing the self-inflating bag
• Squeeze against your palm
– Pressure felt– Pressure release valve– Pressure manometer– Re-inflation

Without Reservoir

With Reservoir

Self inflating bag
• Advantages
• Easier to use• Pressure release valve• Don’t not need a gas source to
inflate

Self inflating bag
• Disadvantages
• Requires a reservoir to deliver 100% oxygen
• Can not be used to deliver 100% free flow oxygen

Masks• Cushioned/Non-cushioned• Round/Anatomical shaped• Size 0 or 1

The surface on which the baby is placed should always be warm as well as flat, firm and clean
POSITION

Correct position of mask

Positioning
• Positioning the infant & resuscitator


Forming & checking the seal

Ventilation rate and pressure

Evaluation-Decision-Evaluation-Decision-Action cycleAction cycle
Evaluation
Action Decision
30 sec30 sec

Signs of Effective Ventilation
Sign of response to ventilation:Sign of response to ventilation:• Improved heart rate
Signs of improvement in newborn:Signs of improvement in newborn:
• Improved heart rate, color, breathing, tone, and saturation

Contraindications
• Diaphragmatic hernia
• Non -vigorous baby born through meconium stained liquor

No improvement
• Is chest rise adequate?
• Is adequate oxygen being administered?

MR. SOPA MR. SOPA •M- Adjust Mask on the face
•R- Reposition the head to open airway oRe-attempt to ventilate…if not effective then
•S- Suction mouth then nose
•O- Open mouth and lift jaw forward oRe-attempt to ventilate…if not effective then
•P- Gradually increase Pressure every few breaths until visible chest rise is noted
oMax Pip 40cmH2O If still not effective then…
•A- Alternative Airway (ETT or LMA)

When to stop ?
• Heart rate above 100/min• Spontaneous breathing
• Baby in Post Resuscitation care

Chest Compressions
Its a 2 personnel job


Indication
If after 30 seconds of EFFECTIVE bag and mask ventilation with 100% oxygen, Heart Rate is below 60 per minute
Indications

• Pump out blood from the heart during compression and fill up blood in the heart during release
• Must always be accompanied by ventilation with 100% oxygen
Principle

CompressRelease
Heart Heart
sternum
Mechanism of Chest Compressions
sternum

• Position– Neck slightly extended with firm support for the
back– Lower 1/3rd of sternum between nipple line &
sternum• Pressure required – depth
– 1/3rd of the AP diameter of chest• Rate
– 90/min
Components


Two-finger method
Techniques of Chest Compressions
Thumb method

Thumb Technique

• Easier with right hand for right handed
• Index and middle or ring fingers
• Other hand used to support the back
• Pressure applied vertically
2 Finger Technique

2 Finger Technique

Don’t lift your fingers/thumbs

• Advantages• Better control of depth• Less tiring• Superior generation of peak systolic & coronary
perfusion pressure• Nails do not hinder performance
• Disadvantages• Difficult when baby is big• Umbilicus difficult to canulate
Preferred method - Thumb

Rate • 3 Chest Compressions then 1 ventilation• 90 Chest Compressions to 30 ventilations in
one minute
Adequacy • Palpate femoral/carotid pulse
Rate and Adequacy

• Consists of 3 compression & one ventilation• 120 events in 60 seconds• 1 cycles in 2 seconds
• ONE- AND – TWO – AND – THREE – AND - ONE- AND – TWO – AND – THREE – AND - BREATHBREATH
Cycle of events

• No pressure to be applied on ribs, Xipisternum, abdomen
• Do not lift thumbs/fingers
Precautions

Dangers • Broken ribs • Lacerated liver • Pneumothorax
Chest Compressions

• HR 60 per minute or more Stop CC, continue BMV at 40-60/min
• If no improvement, check :– Effectiveness of BMV– Oxygen is 100%– Technique of CC is correct
Evaluation after 30 sec of CC & BMV

When to stop chest compressions
• When heart rate is 60 per minute or more

Key points
• 2 personnel job• Ensure 100 % oxygen• Ensure adequate chest movement
during ventilation• Co-ordinate B & M with CC at 3 : 1• Check HR every 30 seconds• Use thumb or 2 finger technique

Intubation

Indications for intubation
• Meconium suctioning in non vigorous baby
• Diaphragmatic hernia• Prolonged or ineffective ventilation• Elective
– VLBW– with CC

Intubation equipment

Preparing laryngoscope
• No. 1 for full term• No. 0 for preterm / LBW• No. 00 for extremely preterm
(optional)

3.5
3.0
2.5
Stylet
>2000 gm
1000-2000 gm
<1000 gm

Selecting endotracheal tube
Tube Size(ID mm)
Weight(gm)
Gest. Age(Wks)
2.5 < 1000 < 28
3.0 1000-2000 28-34
3.5 2000-3000 35-38
4.0 >3000 > 38
ID=Internal Diameter

Preparing endotracheal tube
• Shorten the tube to 13 cm• Replace ET tube connector• Insert stylet (optional)

Additional itemsTape : For securing the tubeSuction equipmentOxygen• For free flow oxygen during intubation• For Use with the resuscitation bagResuscitation Bag and Mask• To ventilate the infant in between
intubation• To check tube placement

Positioning the infant
• On a flat surface• Head in midline• Neck slightly extended• Optimal viewing of glottis


Intubation view

Vocal cord guide

Lip reference mark: (6 + weight in kilos) cm
9-10 cm at the lip for this term infant

Tube in Rt. Main bronchus
• Breath sounds only on right chest• No air heard entering stomach• No gastric distention
ActionWithdraw the tube, recheck

Tube in esophagus• No breath sounds heard• Air heard entering stomach• Gastric distention may be seen• No mist in tube
Action Remove the tube, oxygenate the infant with a bag and mask, reintroduce ET tube

Complications of intubation
• Hypoxia• Bradycardia• Apnea• Pneumothorax• Soft tissue injury• Infection

Minimizing hypoxia during intubation
• Providing free-flow oxygen (Assistant’s responsibility)
• Limiting each intubation attempt to 20 seconds

CPR Medications


2:1000 newborns
MEDICATIONS

No drugs for me!No drugs for me!

MEDICATIONS
• Epinephrine
• Volume expansion

Neonatal Resuscitation
No role of • Atropine • Calcium • Dexamethasone• Dextrose• Intra cardiac adrenaline• Naloxone

Epinephrine
• Formulation 1:1000• Dilution 1:10000 (Ten times)
0.2 ml in 1.8 ml • Load 1 ml (in 1ml
syringe) • Dose 0.1-0.3 ml/kg• Route IV (preferable)• Rate Rapid bolus

Epinephrine Follow up: if HR < 60 or 0• Repeat epinephrine q 3-5 minutes• Ensure: effective ventilation effective chest compressions endotracheal intubation (if not done already) • Consider using volume expander

What is expected response
•After 30 seconds of administration and continued PPV and CC– HR should increase to > 60 bpm
•If no response repeat the dose every 3-5 minutes
•Repeat doses should preferably be give IV

“If the baby appears to be in shock and is not responding to resuscitation, administration of a volume expander may be indicated”
! Shock - Hypovolemia

Signs of Hypovolemia
• Pallor persisting beyond oxygenation• Weak pulses• Low blood pressure• Lack of response to resuscitation
Hypovolemia is a common but often unrecognized cause of need for resuscitation

Volume Expansion
• Indicated when there is no response to resuscitation and there is evidence of blood loss or hypovolemia
• Repeated doses may be necessary if there is minimal response after the first dose
• Umbilical vein remains preferred route but intraosseous acceptable

Medication Administration via Umbilical Vein
• Preferred route for intravenous access
• 3.5F or 5F end-hole catheter
• Sterile technique
Placing catheter in Placing catheter in umbilical veinumbilical vein


Volume Expanders
• Normal saline
• Ringer’s lactate
• Whole blood (O Neg cross matched with mother’s blood)

Normal saline
Indications
• Evidence or suspicion of acute blood loss with signs of hypovolemia and/or baby responding poorly to resuscitation

• Dose – 10ml/kg
• Route – Umbilical vein
• Preparation – large syringe
• Rate of administration – 5-10 minutesIn premature babies: Rapid boluses may induce ICH
Normal saline

Volume expanders
• Effect : Volume expansion, correction of metabolic acidosis
• Expectation : Better BP & pulses, less pallor
• Follow up : If signs of hypoperfusion persist, repeat volume expander, consider sodium bicarbonate or dopamine


!! THANK YOU !!