Pediatric & Neonatal Resuscitation
description
Transcript of Pediatric & Neonatal Resuscitation

Pediatric & Neonatal Resuscitation
Dr. Edward Les

OutlineCase-based
• Illustration of basic PALS/NALS principles– Emphasis on differences from adults
• What’s new in pediatric resuscitation– ILCOR 2000 guidelines and beyond
• Pre-hospital care controversies
Pediatric trauma not covered – Sept 11

Why do kids freak docs out?
• Infrequently treat critically ill children
• Emotional aspect of death/illness in child vs adult
• Age/size related issues – how to remember what’s normal, what equipment/drugs to use, etc…… especially when the s#$@ is hitting the fan

Simplify, simplify
Most of us can’t drive, eat a sandwich, read the newspaper, and balance the chequebook at the same time…

Luten, R. et al. Acad Emerg Med 2002; 9:840-847
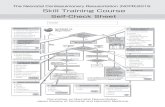
Reduce your cognitive load:
• Make non-automatic behaviours automatic ones as much as possible
• Know the essentials of what’s different about pediatric anatomy/physiology
• Learn a few basic rules of thumb
• Use resuscitation aids!!

Black et al. Emerg Med 2002; 14:160-165
• Prospective comparison of six weight-estimation methods in 495 kids in ED
• Broselow tape and DWEM most accurate
• APLS method was the worst!

Case
3 year old in father’s arms
• lethargy, decreased appetite today
• Dad noticed rash several hours ago on neck, now entire body covered
• P 150 R 32 BP 76/30 T 39.1 Sats 94%
• Toxic appearance, sleepy
• Airway patent, good BS
• CRT 5 seconds• Petechial rash

Heart rate norms

Heart Rates in ChildrenHeart Rates in Children
85 220 300 Normal
SVT
Normal
60 180 200
SVT
Child
Infant
Sinus Tachycardia
Sinus Tachycardia
Cute l’il Moritz

Normal resting RR
Newborn 30-60Infant (1–6 months) 30-50Infant (6-12 months) 24-461-4 yrs 20-304-6 yrs 20-256-12 yrs 16-20>12 yrs 12-16
* >60 abnormal in all age groups

Estimate of Minimum Systolic Blood Pressure
Estimate of Minimum Systolic Blood Pressure
Age Minimum systolic blood pressure (5th
percentile)
0 to 1 month 60 mm Hg
>1 month to 1 year 70 mm Hg
1 to 10 years of age 70 mm Hg + (2 age in
years)
>10 years of age 90 mm Hg

Hypotension: LATE! SUDDEN!
Compensated vs
decompensated shock

Back to case... IV access?• Attempt IO immediately
• Previously attempt PIV 90 seconds
• Useful adjunct in ALL age groups
• Previously < 6 years
• All drugs, fluids OK; can draw bloodwork
• Complications: #, compartment, infection


McCarthy et al. Resuscitation 2003; 56:183-186
“Successful intraosseous infusion in the critically ill patient does not require a medullary cavity”
Adult cadaveric specimens
Successful infusion of methyl green in 5 of 8 case using the calcaneus and radial styloid

ABC’S (S=Sugar)
• Routine rapid assessment of blood sugar: delay in dx of hypoglycemia irreversible CNS damage
• 18/49 (18%) of nontrauma-related pediatric resusc cases: Low BG
Losek, JD. Annals of Emergency Medicine 2000 35(1)

sweets – how much? D10W 5-10 mL/kgD25W 2-4 mL/kg
*Use D10W 2-4 ml/kg in newborns

Case: 11 p.m. at ACH
• 15 month boy carried in by Dad• Acute onset barky cough, noisy
breathing• Airway patent, audible stridor at
rest with nasal flaring and accessory muscle use; no drooling
• P 175, BP 95/50, RR 42, sat 96% RA

Case (cont)
• Gets racemic epi, 02, dex• Initial good response
• 1 hour later: rebound resp distress with significant stridor
• P 175, R28, sat 86% on 2 LPM by NC, becomes somnolent despite repeated racemic and BVM

RSI for kids
• Preoxygenation: may need PPV with Sellick maneuver
(sedate first)• Basal oxygen use per kg 2x adults: shorter “safe
apnea” interval before desaturation
• Premed: Atropine 20 mcg/kg (minimum 100
mcg) • < 1 y.o.• 1-5 y.o. receiving sux• Adolescents receiving 2nd dose sux

RSI for kids
• Premed: defasciculation recommended with sux when > 5 y.o.
• Paralytic:Tendency to avoid sux; certainly
avoid 2nd dose: infants/children exquisitely sensitive intractable brady/arrest
• Rocuronium good alternative

In this 15-month-old with croup…
ETT size?
cuffed?
depth of insertion?
• Broselow – best!!• (16 + age in years) 4
• Uncuffed < 8 years old (exceptions)
• Depth of insertion (cm): tube ID (mm) x 3or age (yrs)/2 + 12

Hofer et al. Br J Anaesth 2002; 88:283-285
(16 + age in years) 4
Broselow
• overestimated tube size in > 50%
• Correct size in 41%
• correct size in 55%• tendency to
underestimate tube size

Anatomical airway issues in kids
• big tongue, soft tissue obstruction
• narrowest at subglottis, soft trachea no cuff • anterior/cephalad larynx difficult visualization
• short trachea R mainstem intubation
• nose breathers < 4 mos
• big occiput neck flexion
• big floppy epiglottis straight blade




failed intubation
• BMV with Sellick
• LMA an option
• No cricothyroidotomy under 8 years
• in a pinch: Needle cric

Case
22 year old female brought to ED by ambulance c/o severe abdo pain/bleeding @ 34 wks GA
• As moved from ambulance – membranes rupture, infant delivers through bloody, mec-stained amniotic fluid
• Infant is cyanotic and flaccid, no spont resps; appearance consistent with 34 wks GA
What now?

Save the baby
• Call for help - NICU• Warm, dry, position, suction (+/- mec),
stimulate, free-flow O2• BVM – when? What about the meconium?• Chest compressions – when, how often?• Intubate – tube size?• Meds – which? Dosages?• Fluids – how much, what, where?

O2 – 21% or 100%?
• Saugstad et al. Resuscitation of newborn infants with 21% or 100% oxygen: follow-up at 18-24 months. Pediatrics 2003; 112:296-300
• Saugstad et al. Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 1998; 102:1
• Vento et al. Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics 2001; 107: 642-647
• Ramji et al. Resuscitation of asphyxic newborn infants with room air or 100% oxygen. Pediatr Res 1993; 34:809-812
• Lundstrom et al. Oxygen at birth and prolonged cerebral vasoconstriction in preterm infants. Arch Dis Child 1995; 73:F81-F86
• Vento et al. Six years of experience with the use of room air for the resuscitation of asphyxiated newly born term infants. Biol Neonate 2001; 79:261-267

O2 – 21% vs 100%
• No differences in outcomes
• ? Some evidence of oxygen toxicity• Studies plagued with problems
Bottom line – jury’s still out- no change to protocols yet

Most newborns save themselves


neonatal/preemie CPR
• Ventilation 40-60 minute
• Compression rate 100/minute
• Together: – 120 events per
minute in 3:1 rhythm = 90 compressions/30
breaths/minute

PreemiesWeight (g)
Gest age (wk)
ETT size
Depth of insertion(cm)
<1000 <28 2.5 6 +Weight (kg)
i.e. 6+1.5kg= 7.5 cm
1000-2000
28-34 3.0
2000-3000
34-38 3.5
>3000 >38 3.5

Meconium
10-20% of all deliveries Suction nose and mouth when head delivered
• If vigorous : routine care
• If depressed (poor resp effort, flaccid, HR < 100) direct visualization of glottis on warmer and suction below cords**
**before drying/stimulation

• > 100 mm HG suction; repeat passes if necessary and if have time
• OG to empty stomach of green muck

Newborn – resus meds
Epinephrine: 0.1 to 0.3 mL/kg 1:10,000 IV or intratracheal
*never use 1:1000 epi*
Naloxone: 0.1 mg/kg IM/IV/SC/ETT if narcotics during delivery
* do not use if mom drug user
Sugar: D10W 2 ml/kg IV

Newborn – volume expansion
• Use umbilical vein• 3.5 or 5 Fr• Depth 1 to 4 cm
(good blood return)
• 10 ml/kg/bolus NS

Case
• Frantic mom runs up to triage with her 8 month old son; her 3 year old gave him a piece of popcorn in the car about 5 minutes ago. He has been choking and coughing ever since. Mom tried to retrieve it with her fingers but couldn’t grab it. Now he’s visibly cyanotic, has obvious stridor, flailing his arms….
• What to do first?

Foreign body airway obstruction
No abdominal thrusts under 1 year of age (risk of organ damage)
• Alternate 5 back blows with 5 chest thrusts until relief of obstruction or unresponsive

Case
You’re knocking a soccer ball around with some little neighbourhood kids at the park, when a little six year old boy suddenly keels over while chasing the ball.
You run over and find him unresponsive, not breathing, no pulse.

Case (cont)
Do you:
a) provide CPR , then call 911 or
b) call 911, then provide CPR

“Phone FIRST” vs “Phone FAST”
< 8 years• CPR first,
then phone fast
Exception: apparent sudden
cardiac collapse
> 8 years• Phone first, then provide CPR
Exception: unresponsiveness with respiratory compromise (submersion, trauma, drug overdose)
Chain of Survival

Pediatric CPA
• Much less likely primary cardiac• Generally…
• Progression from hypoxia and hypercarbia (respiratory failure) OR shock respiratory arrest and bradycardia asystolic cardiac arrest
• Therefore ventilation (CPR) priority over defib (vs adults)
• Recognize early respiratory failure and shock: “Keep the pulse”

Generally, of survivors…
Airway intervention saves 90%
IV access saves 9%
Drugs save 1%

Etiologies
Out-of-hospital• SIDS• Trauma (most
common > 6 months)
• Submersion• Sepsis• Cardiac diagnosis• Pulmonary disease
In-hospital• Sepsis• Respiratory
failure• Drug toxicity• Metabolic
disorders• Arrhythmias

Pediatric CPA
Collective review of 41 published studies by Young and Seidel (3,094 patients)
Ann Emerg Med 1999. 33(195-205)» small sample sizes» poor standardization» vague definitions
50% < 1 yearOut of hospital arrest witnessed in 31%
• Bystander CPR in 30% of these
Initial rhythm: bradysystole 73%VF/VT 10%

Engdahl et al. Resuscitation 2003; 58:131-138
20 years: 98 cases of pediatric CPA 42 % less than 1 year of ageWitnessed arrest 34 %
Initial rhythm:asystole 65%v.fib 8%PEA 19%

What % of pediatric cardiopulmonary arrest
victims survive to discharge?

Roberts et al. Am J Emerg Med 2000. 18 (465-68)
Survival est. in pediatric CPA…
401 people surveyed:•Lay rescuers
•Physicians•Nurses
63%
45%
41%

the reality…
Young and Seidel’s review:13% (0 – 17%)
Engdahl et al:5%
Severe neurologic impairment frequent

Respiratory arrest alone: 75% survival to discharge for apneic
patients with a pulse
Respiratory arrest alone: 75% survival to discharge for apneic
patients with a pulse100%
50%
0%Respiratory
arrestCardiopulmonary
arrest
Survivalrate

Factors associated with survival
Better prognosis
• Age > 1 year• Near-drowning• VF/VT as
presenting rhythm
• Bystander CPR
Poorer prognosis
• Age < 1 year• SIDS presentation• Bradysystole as
presenting rhythm

…there’s an Automated External Defibrillator
available at the soccer field
Do you use it?

Effect of Time to Defibrillation on Survival From Witnessed VF Cardiac
Arrest
Effect of Time to Defibrillation on Survival From Witnessed VF Cardiac
Arrest
0
1020
30
4050
60
70
8090
100
1 MIN 2 MIN 3 MIN 4 MIN 5 MIN 6 MIN 7 MIN 8 MIN 9 MIN 10 MIN
Per
cent
sur
viva
l
Cummins 1989

AED’s in kids: initial concerns
• ? can’t distinguish between tachycardic non-arrest and VF/VT in infants
• Most AED’s designed to deliver 150 – 200 joules
2000 guideline< 8 yrs indeterminate> 8 yrs indicated (Class IIb recommendation)

Atkinson et al. Ann Emerg Med 2003; 42:185-196
• LIFEPAK 500 AED• 203 pediatric patients (median age
11 months, range birth to 7 years)• 1,561 rhythm samples
• Sensitivity 99% for v.fib. (72of 73)• Specificity 99.5% (1,465 of 1,472)

Cecchin et al. Circulation 2001; 1103:2483-2488
Forerunner AED
696 rhythms in 191 kids < 12 years old
• Sensitivity 96% for v.fib.• Specificity 100%

New ILCOR recommendation
• AED’s may be used for kids 1-8 years of age • Ideally, the device should use a pediatric
dose• Insufficient evidence to support a
recommendation for or against the use of AEDs in children <1 year of age
• Still one minute of CPR first unless suspect sudden cardiac collapse
Resuscitation 2003; 57:237-43

Case cont.
The six-year old soccer player is intubated and defibrillated successfully at field; transport to ACH ER
In room 1 he loses his pulse to another run of VF
CPR, defibrillation (how much juice?), and epi …. Still no pulse

Pediatric ALS algorithm modifications (2000)
• Amiodarone: 5 mg/kg IV push for refractory VF/pulseless VT
: 5 mg/kg IV over 20 to 60 minutes for refactory tachycardia with poor perfusion
• Vagal maneuvers for SVT » Ice to face» Blocked straw
• Magnesium for torsades

Amiodarone - FDA warning
• Amiodarone leaches plasticizer from IV tubing during slow infusions
• Benzyl alcohol preservative has been linked to neonatal “gasping syndrome”
Still acceptable for use – be aware of toxicities and monitor side effects
Consult pediatric cardiologist for long-term therapy

Case
• EMS patches in: they are en route with a 4-year-old girl just pulled from a swimming pool. She is apneic , but has a perfusing rhythm of 120
• She is receiving BVM ventilation and ETA is 15 minutes.

Does pre-hospital intubation make any
difference?

Prehospital care in pediatric CPA
1997 study of 141 CPA victims Kumar et al. Ann Emerg Med 1997. 29(743-
747)
• 55% of children intubated vs 93% adults• Intubation attempt in those not intubated:
62% vs 86%
• vascular access: 38% vs 83% • attempted in those who arrived without vascular
access: 3% vs 94% • No epi even if IV access: 40%vs 7%

Gausche et al. JAMA. 2000; 283:783-90.
• 3 year prospective controlled trial in L.A.:kids < 12 years old requiring prehospital airway intervention
830 patients
410 420BVM Tube

Gausche et al.:Survival
OverallBVM ETI
123/404 (30%) 110/416 (26%)
OR 0.82 (95% CI 0.61 - 1.11)
No difference!

Gausche et al.:Survival
Full CPABVM ETI
24/290 (8%) 24/301 (8%)
Also no difference between groups for neurologic outcome

Gausche et al.:Survival
Respiratory arrest only
BVM ETI
46/54 (85% ) 33/54 (61%)OR: 0.27 (95% CI 0.11-0.69)
Did better with bag-mask ventilation only!

Gausche et al:
Complications of intubation
• Successful tracheal intubation rate: 57%
• Intubation attempts increased time at the scene by 2 to 3 minutes
• Unrecognized tube displacement or misplacement: 8% —Esophageal intubation: 2%—Unrecognized extubation: 6%
—14 of these 15 patients died

Gausche et al.
But:• Short transport times: < 25 minutes
(mean 6 minutes)
• Paramedics didn’t use sedatives/NM blockers
• Only 7% of 2584 paramedics actually intubated a patient in the 3 years!

The San Diego experienceVilke et al. J Emerg Med 2002;
22:71-74Retrospective 4-year review of pediatric
endotracheal intubations by paramedics
• 324 intubations attempted• 264 successful (82%)
• 3 (1%) unrecognized esoph intubations; all 3 died (2 SIDS, 1 drowning) – esoph intub not felt to have contributed to death

Pittsburgh
Pitetti et al. Prehosp Emerg Care 2002; 6:283-290
Retrospective review of 189 pediatric CPA cases
• Compared outcomes (survival to discharge):
BLS (including BVM vent but no meds) vs
ALS (intubation plus meds)

Pittsburgh
*f/u available for 3/5: all severely neurologically impaired/vegetative
BLSn=39
ALSn=150
P
Survival in ED
4 24 0.46
Survival in ICU
0 5 0.59
Survival to discharge
0 5* 0.59

Case
2 week old infant previously well• Found in crib having difficulty breathing• P 180, BP 50/P R arm, RR 80• Lethargic, pale, mottled especially below
the waist; perioral cyanosis• Airway patent, cries intermittently• Weak radial pulses, no femoral pulses, CRT
4 seconds• Sunken fontanel• Liver 3 cm BRCM

Differential?

Ductal-dependent heart lesions
Have a HIGH index of suspicion!!
• Age: first day to a couple weeks or more
• HLH, coarctation, AS: systemic circ dependent on R L shunt
• Pulmonary/tricuspid atresia, critical PS: pulmonary circ dependent on L R shunt
• Duct closure : CHF : shock

Prostaglandin E1
• Bolus 0.1 mcg/kg, follow with infusion 0.05-0.10 mcg/kg/minute
Side effects:Apnea, hypotension, bradycardia, seizures, hypothermia

Case progression…
Rapidly develops asystole and total cardiopulmonary collapse
• Chest compressions
• How and how often?
• Epinephrine• Dose?

Coronary Perfusion Pressure Improves With Sequential Compressions
Coronary Perfusion Pressure Improves With Sequential Compressions
CPP at 5:1 ratio
CPP at 15:2 ratio

Dorph et al. Effectiveness of ventilation-compression ratios 1:5 and 2:15 in simulated single-rescuer paediatric resuscitation. Resuscitation 2002;
54:259-264
• No difference in ventilation – because of time lost changing positions
• Almost one-and-a-half times as many compressions with 2:15 ratio
?? 2:15 training for all age groups for layperson CPR

After 25 minutes the baby is still pulseless and apneic despite your
excellent interventions…
Do you call it?

When to quit?
• Prospective study of 300 kids in CPA• No survivor received epinephrine
Sirbaugh et al. Annals of Emerg Med 1999. 33(174)
• 101 kids with CPA or resp arrest• No survivors needed resuscitative efforts for more
than 20 minutes or > 2 doses of epinephrineSchindler et al. New Eng J Med 1996. 335(1473-79)
• Multiple other studies– Small sample sizes, heterogeneous
populations, retrospective designs, etc: Difficult to draw firm conclusions

Current guidelines
• If a child fails to respond to two doses of epinephrine with a ROSC the child is unlikely to survive
• Resuscitative efforts may be ceased in pediatric CPA victims after 30 minutes unless exceptional circumstances exist
i.e.• primary hypothermic insult• toxic drug exposure• recurrent or refractory VF/VT

Caveats…
• Most pediatric ALS recommendations are “class indeterminate”
= promising but low-level evidence or high-level but inconsistent evidence
• None are “class I”= at least one RCT with excellent critical
assessment and positive, homogeneous results

Summary…Pre-hospital:• Single rescuer EMS activation: “Call fast” except
“Call first” for sudden collapse• Prehospital use of AEDs recommended for
victims > 1 year old• Role of pre-hospital intubation still controversial
CPR:• Compression-ventilation ratio: 15:2 if > 8 yo,
5:1 < 8 y.o., 3:1 neonates• 2-rescuer CPR: 2 thumb-encircling hands
compression technique for small infants• No Heimlich in children less than 1 year

Summary…
Advanced life support:• Know your “rules of thumb”• IO access in any age group, immediately if
indicated• Atropine with RSI; careful with sux• Keep newborn resusc kit stocked in your ED• Don’t forget to think about congenital heart
disease in “septic” infant
• Above all: use the Broselow!!

always have a flight plan…

Major reference