NATIONAL OPEN UNIVERSITY OF NIGERIA · 2020. 2. 10. · mons pubis in front to end at perineum....
Transcript of NATIONAL OPEN UNIVERSITY OF NIGERIA · 2020. 2. 10. · mons pubis in front to end at perineum....

ii
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
NSC501 PUBLIC-COMMUNITY HEALTH NURSING III
NATIONAL OPEN UNIVERSITY OF NIGERIA

iii
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
COURSE CODE: NSC501
COURSE TITLE: PUBLIC-COMMUNITY HEALTH NURSING III COURSE GUIDE
NSC501 PUBLIC-COMMUNITY HEALTH NURSING III

iv
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Course Team DR NDIE ELKENAH (Course Writer/Developer and
programme leader)
NATIONAL OPEN UNIVERSITY OF NIGERIA
NATIONA OPEN UNIVERSITY OF NIGERIA, HEADQUATERS, UNIVERSITY VILLAGE CADASTRAL ZONE NNAMDI AZIKIWE EXPRESS WAY,JABI, ABUJA
1.0 Introduction NSC501 is a Five (5) credit unit course. It is a 500 level core course
available for Bachelor of Nursing Science (B.NSc) students. The goal is
to assist the individual, family and community in attaining their highest
level of holistic health in Maternal and child care
The main objective of Public-Community Health Nursing III is

v
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
to provide optimum care to individual, and community through
maternal and child care. Services includes proper antenatal care, post-
natal, family planning nutritional assessment and education..
The course consist of two module and 10 units plus a course guide
which tells you briefly what the course is about, what course materials
you will use and how you can go through these materials with
maximum benefit. In addition the course Guide gives you guidance in
respect to your Tutor- marked Assignments (TMA) which will be made
available to you in assignment files in the study center. It is for your
best interest to attend the facilitation sessions.
Course Aim The course broad objective is to build in your ability to understand and
apply the principles, concepts and process of community health nursing
in providing maternal and child care contemporary society.
Course Objectives
In order to achieve the broad objectives, each unit has specific
objectives which are usually stated at the beginning of the unit. You are
expected to read these unit objectives before your study of the unit and
as you progress in your study of the unit you are also advised to check
these objectives. At the completion of each unit make sure you review
those objectives for self- assessment. At the end of this course, you are
expected to meet the comprehensive objectives as stated below. On
successful completion of the course you should be able to:
• Describe the structures, functions of reproductive organs.
• Define fertilizations and the foetal development.
• Describe maternal physiological adaptation to pregnancy.
• Discuss maternal psycho-social adaptation to pregnancy.
• Describe Sings and symptoms of pregnancy.
• Describe the care of minor disorders of pregnancy.
• Outline the antenatal care of pregnant mother.
• Discuss the stages of labour.
• Outline the role of a nurse in
management of labour
• Outline the care of new born
• Describe the characterist ics and special care of
childhood and adolescent.
D e s c r i b e f a m i l y p l a n n i n g
m e t h o d s
Discuss family health records
Working through the Course

vi
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
To complete the course, you are expected to study through the units, the
recommended textbooks and other relevant materials. Each unit has a
model questions which you are required to answer
Course Material
The following are the components of this course:
- The Course Guide
- Study Units
- Textbooks

vii
NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Study Units Module 1
Unit 1 Review of reproductive system
Unit 2 Pregnancy
Unit 3 Antenatal care
Unit 4 Labour management
Module 2
Unit 1 NEW BORN CARE
Unit2 CHILDHOOD
Unit 3 ADOLESCENCE
Unit 4 ANTHROPOMETRY
Unit 5 FANILY PLANNING
Unit 6 FAMILY RECORD
Tutor-Marked Assignments (TMAS) There will be 30 objective question from all the units of the course
materials. The questions will be divided into three tutor marked
assignments that will be uploaded to the NOUN website for you to
download and answer and the upload. It is computer marked. The value
is 30% of the total mark.
Final Examination and Grading The final examination for course NSC501 will be pen-on-paper and has
a value of 70% of the total course grade. The examination Pass mark is
50%.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Facilitation
There are hours of f a c i l i t a t i o n t o support this course material. You
will be notified of the dates, times and locations of these facilitation as well as
the names and phone numbers of your facilitator.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
CONTENT MODULE 1 MATERNUTY NURSING
UNIT 1 REVIEW OF PRODUCTIVE SYSTEM
Unit 2 EMBROYOLOGY
UNIT 3 ANTENATAL CARE
UNIT 4 LABOUR
MODULE 2 NEW BORN, CHILDHOOD, ADOLESCENCE AND ANTHROPOMETRY
UNIT 1 NEW BORN
UNIT 2 CHILDHOOD
UNIT 3 ADOLESCENTCE
UNIT 4 ANTHROPOMETRY

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
MODULE 1 MATERNUTY NURSING
UNIT 1 REVIEW OF PRODUCTIVE SYSTEM
CONTENTS
1.0 Introduction
2.0 Objectives
3.0 Main Content
3.1 Anatomy and Physiology of Female and Male Reproductive System
3.1.1 External Organs
3.1.2 Internal Organs
3.1.3 Related Pelvic Organs
3.1.4 The Breasts
3.1.5 The Physiology of Female Reproductive System
3.2 Anatomy and Physiology of Male Reproductive System
3.2.1 Organs of Male Reproductive System
3.2.2 Physiology of Male Reproductive System
3.3 Obstetrical Anatomy
3.3.1 Pelvis
3.3.2 Foetal Skull
4.0 Conclusion
5.0 Summary

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
6.0 Tutor-Marked Assignment
7.0 References/Further Reading
1.0 INTRODUCTION
In the preceding units, you have learnt Family Health Care which included concepts and
principles of family health care, assessment of family needs, identification of risk
families, nursing intervention and family health records. In this module, we deal with
one of the important aspects of family health care i.e. Maternal and Child Health. In this
unit, you will review the anatomy and physiology of female and male reproductive
systems. You will also gain deeper understanding of female reproductive organs and the
importance of the related pelvic organs. We will also discuss, to some extent, the female
pelvis and foetal skull and their importance and relationship in obstetrics.
2.0 OBJECTIVES
In this unit you are going to learn about the anatomical structure of female and male
reproductive organs and their physiological functions.
After going through this unit you should be able to:
Identify the female reproductive organs
list the organs of female reproductive system
list the related pelvic organs of female reproductive system.
describe the physiology of female reproductive organs
list the male reproductive organs
describe the physiology of male reproductive system.
3.0 MAIN CONTENT
3.1 Anatomy and Physiology of Female Reproductive System
You know that the female reproductive system is divided into two groups - external and
the internal reproductive organs (genitalia). Let us discuss these external and inters
organs, and breasts and other accessory organs in the following sub-sections.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.1.1 External Organs
The external reproductive female organs i.e. vulva (Pudendum) (the term which is
derived from the Latin word meaning covering) includes everything that is visible
externally from the lower margin of the pubis to the perineum. These structures are
shown in Fig. 1.1.
Mons Pubis (Mons Venaris): It is a firm cushion like formation. It covers the symphysis
pubis and is covered with hair. It constitutes the upper aspect of the vulva. is composed
of adipose tissue. It lies anterior to the vaginal and urethral openings.
Fig. 1.1: The External genitalia
Labia Majora (Singular-Labia Majus)
These are bilateral prominent cutaneous folds extended downwards on each side from
mons pubis in front to end at perineum. Each fold is 7-9 cm long, 2-4 cm wide. The labia
majora contains fatty areolar tissue, veno plexus and nonstriated muscle fibers with a
covering of stratified squamous epithelium of skin. The covering skin is hairy on outer
Mons veneris
Labium majus
Clitoris
Vestibule
Urethral meatus Labium minus
Vaginal orifice
Hymen
Fourchette
Central part of
perineum
Anus

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
aspects of labia. Both inner and outer surfaces contain sebaceous and sweat glands.
Child birth trauma can cause vulval haematoma. Labia majora is homologous with
scrotum in male.
Labia Minora (Singular-Labia Minus)
The labia minora are two thin folds of cutaneous tissues lying between and parallel to
the labia majora. They are reddish in colour. Each fold is about 5 cm long, 0.5 - 1 cm
thick. The inner surfaces generally remain in contact with each other. Upper divisions of
each labia minus unite to form a hood like structure for the clitoris. This skin fold
hanging over the clitoris is termed as prepuce. The lower divisions unite to form frenum
of clitoris. Posteriorly they unite in the middle to form a thin ridge of skin called
fourchette. Labia minors contain two of nonkeratinized skin containing elastic tissue,
veins, a few smooth muscles, abundant; nerve endings, and sebaceous glands but no
hair follicles or sweat glands. They become erectile on sexual activity. They are
homologous to pineal urethra in male.
Clitoris
Ibis is a midline 2.5cm cylindrical erectile structure attached to the undersurface of
symphysis pubis by suspensory ligament. Clitoris lies 2.5 cm above external urinary
meatus and its body lies in front of symphysis pubis. Childbirth can cause tear around
clitoris and excessive hemorrhage. Clitoris is an analogue to penis in male.
Vaginal Vestibule
It is a triangular area between the labia minora laterally, from clitoris at the apex to
fourchette anteroposteriorly. There are four openings into the Vestibule:
i) External urethral opening
This is a midline anteroposterior slit with two lateral lips lying behind clitoris and just
in front of vaginal orifice. Paraurethral ductsspim (Skene's duct) opens on either side of
external urethral meatus or on its posterior wall inside the orifice.
ii) Vaginal orifice (introitus)
It is a median slit behind urethral opening. It is completely .guarded by a septum of
mucous membrane called hymen. In a virgin, hymen has a small eccentric opening not
usually admitting the finger tip. On coitus it gets ruptured. Following childbirth per

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
vagina hymenal tags carunculae myrtiformes. are visible. Hymen is composed of double
layer of stratified squamous epithelium with intervening vascular connective tissue.
Vaginal introitus gets dilated on coitus and child birth.
iii) Two openings of Bartholin gland ducts
Bartholin glands are pea sized mucus secreting oval glands. Each gland is situated
posterior to Vestibule. The duct is about 2 cm long and opens in the groove between
hymen and labia minus. The gland and duct are lined by single layer of columnar
epithelia, except for the duct opening which is lined with stratified squamous
epithelium. On sexual excitement, bartholin glands secrete alkaline mucus that
lubricates the vaginal introitus to facilitate coitus. The gland can become infected and
infection is termed as Bartholin abscess or Bartholinitis.
The vulva receives its blood supply from the pudendal arteries and nerve supply from
pudendal nerves.
Now we come to the important organs of reproduction i.e. pelvic floor and perinial
region.
The Pelvic Floor and Perinial Region: The pelvic floor is also known as pelvic diaphragm.
It is composed of two pairs of muscles, levator ani muscles and the coccygeus muscles.
The diagram of pelvic floor is given below in Fig. 3.2.
Fig. 1.2: The Pelvic Floor
Lachio-cavernosus Lachio-cavernosus
Clitoria
Lachio-cavernosus
Bulbo-cavernosus
Transverse perinei
Gluteus maximus
Urethral orifice
Vaginal orifice
Levator ani
& coccygeus muscles
Anal sphincter

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The deeper layer is composed of three pairs of coccygeus muscles:
1. The Pubo Coccygeus Muscle 2. The Ilio Coccygeus Muscle 3. The Ischio Coccygeus Muscle The superficial layer is composed of fine muscles:
1. The external anal sphincter 2. The transverse perennial muscle 3. The bulbo cavernous muscle 4. The ischie cavernous muscle 5. The membraneous sphincter of the urethra. The functions of this region includes the following:
1. Supports the weight of the abdominal and pelvic organs 2. Its muscles are responsible for the voluntary control of micturition, defecation
and play an important part in sexual intercourse. 3. During childbirth it enhances passive movements of the foetus through the birth
canal. Perinial Body and Perineum
The perinial body is a wedge shaped mass of fibrous muscular tissue that extends
upwards from the perineum and occupies the area between the vagina and the rectum.
The base is called perineum. The perinial body is 4 cm in width and depth. Deep and
superficial muscles fuse in the centre of this body. The perinial body is stretched and
flattened when the vagina is distended as the foetus passes through birth canal during
delivery.
3.1.2 Internal Organs
The internal reproductive organs are contained in the true pelvic cavity and comprise
the uterus, vagina, ovaries and fallopian tubes.
Uterus
Uterus is a hollow muscular, pear shaped organ contained in the cavity of the true
pelvis. It is situated behind the urinary bladder and in front of rectum. It has a body
which has a rounded upper part called fundus and a lower part called neck or cervix. It
measures approximately 7.5 cm in length, 5 cm in width at its widest part and 2.5 cm in
thickness (in anterioposterior diameter). It weights approximately 60 gm. In it, the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
fertilised ovum embeds, is nourished and protected for 40 weeks, until during labour,
the fetus is expelled by the powerful constructions of the uterine muscle.
The angle where the Fallopian tube is inserted is known as the Cornu or horn. The body
of the uterus gradually tapers downwards and the constricted area immediately above
the cervix is known as Isthmus which distends during pregnancy to form the lower
uterine segment.
The perimetrium is a layer of peritoneum; which covers the uterus except at the sides, beyond which it extends to form the broad ligaments. The perimetrium is firmly attached to the uterine wall except at the lower anterior part where, at the level of the isthmus, the peritoneum is reflected on to the bladder.
The myometrium, or muscle coat has very great expansile properties. It forms seven-eights of the thickness of the uterine wall and consists of three layers, an inner circular layer of fibres, a thick intermediate layer, the fibres of which form an encircling figure of eight arrangement surrounding the blood vessels, and by constricting them act as living ligatures to control, bleeding during the third stage of labour. The fibres of the outer muscle layer are arranged longitudinally and because they are four times more plentiful in the fundus the decreasing gradient plays a part in the expulsion of the fetus.
The endometrium lines the body of the uterus and consists of columnar epithelium glands, which produce an alkaline secretion, and stroma or connective tissue cells capable of the rapid regeneration necessary following menstruation. It is also a rich source of prostaglandins. The endometrium is richly supplied with blood and is about 1.5 mm thick. When embedding of the fertilised ovum occurs the endometrium is known as the decidua, because after labour it will be shed.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Fig. 1.3: The uterus and the left uterine tube and ovary
There are 4 pairs of ligaments which give additional support and maintain the uterus in
its forward inclination. These are:
1. The two broad ligaments-continuous structure that is formed by a fold of the peritoneum.
2. The two round ligaments, one on each side, are fibromuscular chords composed of muscles prolonged from the uterus and a small amount of connective tissue.
3. The two utero-sacral ligaments, again one on each side extend backward from the cervix, pass on each side of the rectum, and insert at the posterior wall of the pelvis.
4. The transverse cervical ligaments gives support to the uterus from below. The blood supply to the uterus is through the uterine artery which is a branch of
the internal iliac artery. The autonomous nerves (sympathetic and
parasympathetic) supply the uterus.
Vagina
Vagina is a muscular membraneous canal. It connects the internal and external
reproductive organs.
The vagina consists of:
a muscular layer
a loose connective tissue layer
the mucous layer which is arranged in folds called rugae.
Fundus
Uterine tube
Ligament of ovary
Ovary
Fimbria
5.0cm

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
During child bearing years of life the vaginal secretion is normally acidic, with a pH
ranging from 4.0 to 5.0 due to lactic acid resulting from breakdown of glycogen by
Doderlin bacilli.
The space between the cervix and vagina is termed as fornix (an archlike structure).
There are four fornices of vagina: the anterior, the posterior and two lateral fornices.
The posterior fomix is considerably deeper than the anterior because posterior wall of
vagina is larger. Anterior wall of vagina is 6.7 cm long whereas posterior vaginal wall is
8-y cm long. Fomices are important in pelvic examination.
Fallopian Tubes or Uterine Tubes or Oviducts
Fallopian tubes, are two slender muscular tubes, that extend laterally from the cornua
of the uterine cavity, one from each side. It consists of three layers:
Serous layer- the outer layer, made up of peritoneum covering
Muscular layer- the middle layer
Epithelial layer - the inner surface is lined by ciliated and nonciliated, secretory cells.
The length varies from 7 to 14 cm. and thickness also varies. The proximal end is very
small, but there is a slight gradual increase in width distally.
Each tube has four parts:
The interstitial portion - passes through the muscle wall
The Isthmus is immediately adjacent to the cornua of uterus
The Ampulla is the expanded lateral portion
The fimbriated end or infundibulum, is the wide distal funnel shaped opening Ovaries
The ovaries are the female sex glands (gonads). They are two small, flatten almond
shaped organs located one on each side of the uterus. Each ovary is attached the
posterior surface of the broad ligament by the mesovarian ligament. The ovaries the
fallopian tubes are supplied by the ovarian arteries.
An ovary is usually described as having the size and shape of an almond; each is about 4-
5 cm long, 2 cm wide, and 1 cm thick and weighs about 3 gm.
The ovary consists of two parts: central portion or medulla, and an outer layer or co The
medulla is composed of connective tissue, blood and lymph vessels and nerves. In the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
cortex numerous minute follicles are embedded, each of which contains an ocyte, germ
cell of the female. These are produced during the first five to six months of foe life.
It is estimated that 200,000 ocyte are present in each ovary at birth. At the beginning
adolescence 500,000 ocyte are present, called primary ocyte. At mature stage during
reproductive period these are termed as graafian follicle. The ovaries perform two vital
functions:
i) they produce, mature and extrude ova
ii) they secrete hormones
Fig. 1.4: Life cycle of the Graafian follicle
The function of ovaries will be described in detail in subsection 1.2.5.
3.1.3 Related Pelvic Organs
We have already learnt about the external and internal reproductive organs of the
female. Now you will learn about the related organs such as bladder and rectum which
are situated in the pelvic cavity, and lie in close proximity to the reproductive organs.
We will learn in brief the structure, function and exact location of these organs. If
bladder or rectum is full, it interferes with satisfactory pelvic examination of woman.
Full bladder and rectum also cause delay in the progress of labour. Injuries to bladder
Fully developed corpus luteum
Ovarian ligament
Corpus albicans
Developing follicles
Ovulation

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
and rectum do occur sometimes at the time of childbirth. Let us discuss bladder and
urethra first and then talk of rectum.
Bladder and Urethra
The urinary bladder is a muscular membraneous sac. It is situated behind the symphysis
pubis and in front of the uterus and vagina. Urine is collected into the bladder by the
ureters. The ureters pass across the brim of the bony pelvis, to the posterior part of the
bladder, which they enter-somewhat obliquely at about the level of the cervix.
The bladder empties through urethra - a short passage/tube 3-8 cm long that terminates
in the urinary meatus. The meatus is a small opening situated in the middle of its
vestibule between the clitoris and vaginal orifice.
Rectum
The lowest segment of the intestinal tract is situated behind and to the left of the uterus
and vagina. The terminal inch of the rectum is called the anal canal. The anus is a deeply
pigmented, puckered opening situated 4-5 cm below the vaginal orifice. It consists of
bands of circular muscles, the internal and external sphincter ani muscle. Veins of the
lower rectum and anal canal sometimes become engorged and inflamed during
pregnancy, as a result of pressure exerted by greatly enlarged uterus. The distended
veins or enlargement of veins of lower rectum and anal canal are called hemorrhoids or
piles.
3.1.4 The Breasts
The breasts of the female may be regarded as accessory glands of the reproductive
system. These are two in number. Breasts are situated one on each side of the chest
between second and sixth ribs. The nipple and areola is covered by small elevations
known as the Tubercles of the Montgomery.
The breasts are compound secretory glands composed mainly of glandular tissue which-
is arranged in lobes, approximately 20 in number (see Fig. 1.5). Each lobe is divided into
lobules and consists of alveoli with secretory cells which produce milk. Small lactiferrous
ducts carrying milk from the alveoli of each lobe, unite to form 20 large ducts. These
ducts, before opening on the surface of the nipple widen to form ampulla which act as
temporary reservoirs for milk.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The nipple, composed of erectile tissue is covered with epittelium and contain plan
muscle fibres which has a sphincter like action in controlling the flow of milk.
Surrounding the nipple is an area of loose skin known as the areola.
In early puberty the breasts undergo extensive changes. Mammary growth is controlled
by hormones. The combined influence of the ovarian hormones (estrogen and
progesterone), the anterior pituitary hormones, somatotropin (growth hormone) and
prolactin bring about normal growth of the breast. At the end of puberty the breasts
reach a size that is characteristic for the individual woman. During pregnancy major
changes take place in the development of secretory tissue
Fig. 1.5: The Breast

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
As early as six weeks of pregnancy, the breasts become enlarged, tense and sometimes
tender. The growth of breasts continue throughout pregnancy. The nipple becomes
darker in colour and more erectile.
The primary areola
At 12 weeks there is darkening of the area around the nipple. this time a clear fluid can
be expressed from the breasts, but true clostrum does not appear until the 16th week.
Montgomery's tubercles
From the 8th week onwards, 12 to 13 small nodules appear on the primary areola. They
are the pouting mouths of sebaceous glands, and the sebum they secrete keep the
nipple soft and pliable.
The secondary areola: It is seen after the 16th week. It is a mottled zone of
pigmentation, extending beyond the primary areola and sometimes covering half of the
breasts. The breast pigmentation may persist for 12 months after childbirth.
3.1.5 The Physiology of Female Reproductive System
During childhood the reproductive system undergoes gradual growth, along with other
parts of the body, and becomes mature during adolescence. About the age of 9 to 11
years the reproductive organs begin to undergo rapid development. Given below is a
note on the physical changes of puberty; i.e. the usual sequence of sexual development
in girls and the average age at which these changes are first seen:
1. Before 8 years precocious sexual development 2. Appearance of secondary sex characteristics before the age of eight years in girls.
(Certain pathological conditions may stimulate the ovaries to premature activity) 3. 12-13 years - average age of sexual development 4. After 12-13 years-Delayed sexual development, physical changes, growth of bony
pelvis and widening of hips, 5. Certain changes in breasts also appear 6. Growth of public hair, auxiliary hair, growth of external genitalia 7. Acceleration of growth 8. The first menstrual period is termed as menarche. Menarche appears between 9
to 17 years. 9. Ovulation usually begins one or two years following menarche. Functions of the mature reproductive cycle

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
After the ability to reproduce has been attained, the reproductive organs of the female
go through a series of cyclic changes each month throughout child bearing period (like
menstruation) except during pregnancy, lactation and cessation of menstruation
(menopause). These changes involve two cycles:
i) Ovarian cycle
ii) Endometrial cycle or menstruation
Let us discuss ovarian cycle first.
3.1.5.1 The Ovarian Cycle
The ovarian cycle consist,-. of the series of changes in an ovary that are repeated at „
monthly intervals. Main phrase of the cycle includes of development of the-graafian
follicles, ovulation and formation. of corpus luteum.
Let's discuss briefly these three developments below:
Graafian Follicles
It is estimated that at birth each ovary contains two lacs of immature follicles.
Approximately fifty thousand are present in each ovary when puberty is reached. From
the time ovulation begins during puberty until the menopause, some of the primary
follicles, under the influence of follicle stimulating hormones (FSH) from the anterior
pituitary develop to full maturation. The structure of a fully mature graafian follicle (see
Fig. 1.6) shows the following structures.
Theca internal - inner layer
Theca external - external layer
Mendera ganulosa - cells lining the graafian follicle
Discus proligerous - mass of cells
Liquor follicle - fluid accumulates in the centre of the graafian follicle
Ocyte - enclose in discus proligerous.
Follicle beginning of
Antrum formation
Developing
Primary Follicle Germinal
Epithelium
Mature Follicle
Follicular Fluid
Ovum
Released Ovum
Raptured Follicle
Corpus albicans

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Fig. 1.6: Ovulation
3.1.5.2 Ovulation
When a graafian follicle, with its enclosed maturing ocyte, reaches the surface of the
ovary, its wall becomes thinner and it finally ruptures. The process of extrusion of a
matured ocyte from the ovary through rupture of graafian follicle is called ovulation.
The ovum is discharged near the fimbriated end of the fallopian tube. Ovulation is the
dividing period between the two phases of the ovarian and amenstrual cycle. The pre-
ovulatory period is termed follicular phase and post-ovulatory period termed luteal
phase.
The time of ovulation is approximately 10 days before the end of a cycle.
Several signs and symptoms may give evidence that ovulation will or has taken place.
These are:
1. Mid-cycle abdominal pain.
2. Mid-cycle vaginal bleeding amounting to no more than spotting.
3. A shift in basal body temperature. Body temperature is relatively higher during
post-ovulatory period. The basal body temperature shift is a useful clinical
method of determining the approximate time of ovulation. The woman is
instructed to take her oral temperature daily for six months immediately after

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
awaking in the morning and before getting out of bed to determine the time of
ovulation.
Corpus Luteum
After ovulation the cavity of the ruptured graafian follicle is replaced by a compact mass
of tissue termed as corpus Lueum (Yellow body), so named because it is of yellow
colour. The corpus luteum functions as an endocrine organ. It produces progesterone
and -sécretes the follicular hormone estrogen. Corpus luteum degenerates and forms
the corpus albicans. If pregnancy occurs, it is termed corpus luteum of pregnancy, and
continues approximately three months.
3.1.5.3 Ovarian Hormones
The ovaries produce two steroid hormones: estrogen and progesterone.
i) Estrogen: is a female sex hormone. It is responsible for the growth of female
reproductive organs and the mammary glands. Estrogen is also involved in a
number of systemic processes such as fluid, electrolyte balance and body
temperature. The functions of estrogen are as under:
a) Changes cervical mucus to favour migration of sperms.
b) It stimulates mobility of fallopian tubes to propel matured ova through
them.
c) It prepares endometrium for implantation of fertilized ovum.
d) It helps in the growth of uterus and breasts during pregnancy.
ii) Progesterone: The corpus luteum secrets progesterone in large amount and also
some estrogen. Progesterone is a progestational hormone. Its functions include
the following:
a) It prepares uterus for implantation of a fertilized ovum and maintenance
of pregnancy.
b) Progesterone along with estrogen causes cyclic changes in the
reproductive tract.
c) It is necessary for the complete development of the mammary glands.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
d) It has some effect on metabolic process.
Ovarian hormones bring cyclic changes in the cervix and vagina.
Cervical Mucus
Varies considerably in its characteristics during the course of each cycle. Cervical mucus
can be examined and evaluated for its qualities to determine approximate time of
ovulation and to assess ovarian functions.
Vaginal Mucosa
Mucosal cells and the secretions of the vagina undergo regular changes during each
ovarian cycle. Vaginal smears may be used to estimate estrogen activity.
Now we will come to the discussion on endometrial cycle.
3.1.5.4 Endometrial cycle (menstrual)
As the ovary under goés cyclic changes, so the endometrial lining of the uterus also
undergoes a series of changes. The endometrial cycle can be described in three main
phases:
i) The Follicular Phase: This phase commences about two days after the cessation
of menstruation and lasts until ovulation takes place (14 days previous to next
menstruation period). Estrogens are responsible for the growth of the
endometrium which takes place at this time.
ii) The Luteal Phase: The premenstrual phase commences after ovulation, when
progesterône causes the endometrium, which has already been growing under
the influence of estrogens to hypertrophy still further. The endometrium glands
increase in size, the capillaries are distended with blood, and small haematoma
form under the epithelium producing red congested surface. This thick soft
vascular membrane is admirably prepared for the reception of the fertilised
ovum. Should fertilization not take place, the ovum dies, the corpus luteum
disintegrates, the secretion of estrogens and progesterone falls and
endometrium shows degenerative changes which are followed by desquamation
and bleeding.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
iii) The Menstrual Phase: The menstrual phase, characterised by vaginal bleeding,
lasts for three or four days, and occurs every 28-30 days from puberty to the
menopause in the normal woman. This is the terminal phase of the menstrual
cycle. The superficial layer of the endometrium is shed, along with blood from
the capillaries. The unfertilised ovum is also discarded. As soon as menstruation
ceases the regeneration of the endometrium begins. The remaining glands and
stroma cells multiply and the effused blood is absorbed as in the healing of a
wound. The endometrium is reformed.
Certain signs and symptoms appear a few days before the onset of menstruation.
Collectively these signs and symptoms are called premenstrual syndrome.
Let us discuss the premenstrual syndrome.
3.1.5.5 Premenstrual Syndrome
A few days before bleeding begins, certain promontory signs are frequently noticed.
Common signs are abdominal distention, headache, backache, breastfullness, bladder
irritability, constipation and pre-menstrual tension characterised by depression or
anxiety These signs and symptoms should be considered as normal. It is believed that if
menstruation is accepted/regarded as a normal physiological process it often reduces
discomforts of menstruation such as dysmenorrhoea.
The Climacteric or Menopause
The cyclic changes of the reproductive organs of female continue during the child
bearing period. Beyond this period the function of the ovary gradually decreases and
ultimately stops. This period is called climacteric or menopause.
The climacteric, frequently termed as the menopause and sometimes called "the change
of life", is the period of life at which ovarian function gradually decreases and eventually
stops. Menopause means permanent cessation of menstruation. The climate occurs
between the age of 40 and 50, but there is considerable variation of time. As
menopause approaches menstruation often occurs irregularly. The flow sometimes
increases slightly, but usually begins to decrease in amount.
Vaso-motor changes - hot flushes - of the face and neck sweats and flashes of heat that
may involve the entire body are the most characteristic symptoms of climacteric.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.2 Anatomy and Physiology of Male Reproductive System
In the foregoing section and subsections you have learnt about anatomy and physiology
of female reproductive organs. In this section we shall focus the anatomy and
physiology of male reproductive organs. The description of these organs is given below
in subsection 1.3.1.
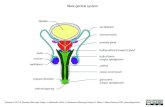
3.2.1 Organs of Male Reproductive System
The male reproductive organs are:
1. Testes 2. Epididymis 3. Vas deferentia (Singuler -vas deferens) 4. Seminal Vesicles 5. Ejaculatory ducts 6. Prostate Gland 7. Bulbo Urethral Glands (Cowper's Glands) 8. Penis 9. Scrotum and Spermatic
Vas deference
Ductus
epididymis
Urethra
Bladde
Seminal vesicle
Ejaculatory duct
Prostate gland
Efferent ductule
Seminiferous
Tunica
Testes
Septu
Lobule
Penis

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Fig. 1.7: Male reproductive organs
Let us discuss each of these organs.
3.2.1 Testes
The testes, the sex organs or gonads, of the male are two slightly flattened, ovoid,
glandular bodies. The testes are formed in the peritoneal cavity during foetal
development and then normally migrate through the inguinal canal into, the scrotum
during the eight or ninth month of pregnancy, or occasionally soon after birth. Descent
into the scrotum by the age of puberty is essential for normal spermatogenesis; which is
adversely affected by the relatively higher temperature within the body. Each testes has
a mass of narrow, coiled tubules, called semiferous tubules. These tubules are from 1 to
3 feet long. The combined length of many tubules in one testis equals almost one mile.
Epididymis
The epididymies are bilateral narrow bodies situated along the upper posterior part of
each testis. Each contain a narrow, tortuous tubule approximately 20 ft.in length. This
tubule serves as the area to which the spermatozoa that have been released into the
semiferous tubules are conveyed, and where they may remain for about three weeks.
Here they are retained until physiological maturation is complete and until they become
motile. As the tubule of the epididymis leaves the body, it becomes known as vas
deferens.
Vas deferentia
The vas deferentia are bilateral ducts, approximately 18 inches long, which continue
from each epididymis and then terminate in the bilateral ejaculatory ducts, which open
into the urethra. A vas deferens ascends from each testes through a spermatic cord,
passes through the inguinal canal, crosses the pelvic cavity, and after coursing upward
and medially, passes downward to the base of the bladder where it widens into an
ampulla. This terminal end joins with a duct from seminal vesicle, and they become the
ejaculatory duct. The vas deferens serves as a storage site for sperm.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Seminal Vesicles: The seminal vesicles are two membraneous pouches, situated
between the lower part of the bladder and the rectum. Through a short duct each
vesicle joins the terminal end of a vas deferens and with it becomes an ejaculatory duct.
Ejaculatory Ducts
The ejaculatory ducts are paired, narrow, short tubes formed by the joining of the
terminal ends of the vas deferentia and the ducts from the seminal vesicles. These two
ducts descend between the lobes of the prostate gland and open into the urethra into
which they discharge sperm and secretions from the seminal vesicles and epididymis.
3.2.2 Prostate Gland
The prostate gland is located just below the bladder and surrounds the upper portion of
the urethra. It secretes a thin, complex fluid that is discharged into the urethra through
many small tubules that open into it.
Bulbo Urethral Glands (Cowper's Glands)
The bulbo urethral glands are two small pea sized bodies located below the prostate
gland within the pelvic floor. They secrete an alkaline, viscous fluid that is emptied into
the urethra, through a small duct from each gland.
3.2.3 Penis
The penis is the male organ of copulation. Semen is ejaculated through it into the vagina
of the female during intercourse, and the active spermatozoa in the semen can enter
the cervix and travel through the fallopian tubes where fertilization of an ovum may
take place. The penis is a cylindrical organ composed of three elongated masses of
erectile tissue. A slight enlargement at the end of the penis, called the glans penis,
contains urethral opening and many very sensitive nerve endings. The skin of the penis
extends over its end, covers the glans, and become folded upon itself. This is called the
prepuce or the foreskin and is the portion that is surgically removed when a
circumcision is performed.
Urethra
The male urethra, which extends from the neck of the bladder to the orifice in the glans
of the penis, serves two purposes. It conveys urine from the urinary bladder at urination
and transmits semen containing spermatozoa at copulation.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Scrotum and Spermatic Cord: The spermatic cords originate just above the inguinal
canal, pass through the canal, and down to the scrotum. Scrotum a pouch like double
chambered structure is made up of skin, fascia and muscle. The testes, epididymis, and
parts of the spermatic cords are enclosed.
3.2.4 Physiology of Male Reproductive System
Physical changes occur in puberty in boys. The earliest physical changes in boys are ,
testicular growth, and thinning and pigmentation of scrotal skin. The growth of genital
organs then continues.
Pubic hair begin to appear. Prostaatc growth and secretary activity begins. Breast also
enlarge slightly. Axillary hair grow. Fine hair appear on upper lip. Deepening of voice
occur at this time. Physical growth is accelerated and height production increases
rapidly.Boys continue to grow even beyond the age of 18 years. Fertility develops soon
after mid puberty in boys.
The mature reproductive organs of the male performs three major functions i.e. of
hormones, spermatogenesis and secretions from glands. The hypothalamus and
pituitary gland are closely inter-linked with function of the reproductive organs.
.Hormonal function is carried out by specialised cells of the testes called interstitial cells.
These cells secrete` the male hormone testosterone. Testosterone is necessary for
normal development and activity of male organs. Spermatogenesis also takes place in
the lining of seminiferous tubules. The secretions from the male accessory glands are as
follows:
1. The semen - produced and released from testes 2. The seminal fluid - the seminal vesicle secrete a yellow fluid 3. The secretion from the prostate gland the combined secretion from the seminal
glands provides a fluid that serves as a medium for sperm transport and as a favourable substance to sperm fertility.
The pH of semen varies 7.35 to 7.50. Semen is ejected from the male genital tract in an
average volume of 3 ml. Each milliliter of semen normally contains 50 to 150 million
spermatozoa.
So far we have discussed the anatomy and physiology of female and male reproductive
systems in general. Now we shall talk of obstetrical anatomy which is important from
the point of view of MCH care during pregnancy, child birth and postnatal care.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.3 Obstetrical Anatomy
The internal organs of the female are contained in the pelvic cavity. The size and shape
of the pelvis is important because the foetus has to pass through it during labour.
There are three factors which are concerned during labour.
1. The passage - The pelvis (hard and soft parts) 2. The passenger - The foetal skull (the whole) 3. The powers - The uterine contractions (the general health of mother). The passage and passenger will be described here. The powers i.e. the uterine
constructions will be discussed in Section 2.4. Let us begin with passage i.e. pelvis fast.
3.3.1 Pelvis
Pelvis has been classified into four types according to the shape of the brim (Fig. 1.8).
Fig. 1.8: Characteristic inlet of the flour types of pelivs
1. The gynaecoid pelvis - or true pelvis, has a round brim 2. The android pelvis - has a heart shape brim 3. The anthropoid pelvis - has an oval brim, diameter 4. The platypelloid pelvis - or simple flat pelvis, has a kidney shaped brim, in the
anteroposterior diameter
Anthropoid
Android Gynaecoid
Platypelloid (flat)

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
We will discuss only gynaecoid pelvis here as it is of obstetric importance.
Gynaecoid pelvis
The gynaecoid pelvis is composed of:
i) Two innominate bones or hip bones composed of three parts:
Ilium
Ischium
OS pubis i) Sacrum ii) Coccyx There are three pelvic joints:
One symphysis pubic joint
Two sacroiliac joints
One sacrococcygealjoint There are five pelvic ligaments:
Interpubic ligament
Sacroiliac ligament
Sacrococcygeal ligament
Sacrotuberous ligament
Sacrospinous ligament The pelvis is divided into two parts:
False pelvis - The upper expanded part
True pelvis - The bony canal The true pelvis is divided into:
Pelvic brim or inlet
Cavity
Outlet The pelvic measurements are as follows:
Diameters of the pelvic brim or inlet
i) Anteroposterior diameters also called the obstetrical conjugate is 11 cm
i) Oblique diameters is 12 cm

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
iii) Transverse diameter is 13 cm
Diameters of the Cavity
Cavity is circular in shape. All the diameters are 12 cm.
Diameters of the outlet
The anteroposterior is 13 cm
The oblique diameter is 12 cm
The transverse diameter is 11cm
Fig. 1.9: The pelvic measurements
3.3.2 Foetal Skull
The foetal skull contains the delicate brain which may be subjected to great pressure,
during labour. It is large in comparison with the true pelvis. Head is the most difficult
part to deliver. Some adaptation between skull and pelvis must take place during
labour. Therefore the foetal skull is extremely important in obstetrics. See Figs. 1.10.
and 1.11.
Antero – posterior Obligue Transverse
Brim
Cavity
11 12 13
12 12 12
13 12 11
ANTERIOR FONTANELLE
OR BREGMA

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Fig. 1.10: Foetal skull, showing regions and landmarks of obstetrical
The foetal head may be divided into vault, face and base
Bones of the vault of the foetal skull are:
occipital bone
two parietal bones
two frontal bones
Fig. 1.11: Diagrammatic representation of the vertex area of foetal skull showing sutures
and fontanelles
The Sutures
Are cranial joints. The important sutures in the foetal skull are:
The lambdoidal suture
The sagittal suture
The coronal suture
Lambdoidal Suture
Sagittal Suture
Coronal Suture
Frontal Suture
Posterior
Fontanelle
Anterior
Frontanelle
Occipital
L. Parietal R. Parietal
½ Frontal ½ Frontal

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The frontal suture The Fontanelles
Where two or more sutures meet, a fontanelle is formed. Therg two important
fontanelle of foetal skull:
Posterior fontanelle, closes 6 weeks after birth
Anterior fontanelle, closes 18 months after birth Regions of the foetal skull
The occiput
The vertex
The sinciput or brow
The face The diameters of the foetal skull are given below:
Bitemporal 8.2 cms
Biparietal diameter 9.5 cms
Suboccipito bregmatic 9.5 cms
Suboccieito frontal 10.5 cm
Occieito frontal 11.5 cm
Mento vertical 13.5 cm
Submento vertical 11.5 cm
Submento bregmatic 9.5 cm Moulding is the change in shape of the foetal skull that takes place during the p through
the birth canal, due to overriding of bones because of sutures and fontanelle.
Diagnosis of presentation and position of foetus are ascertained by means of pal vaginal
examination, x-ray or ultrasound.
4.0 CONCLUSION
You have seen that female as well as male reproductive organs are important for
reproduction. Female reproductive external organs are collectively termed as vulva.
The internal organs are vagina, uterus, fallopian tubes and ovaries. The ovaries produce
female hormones and ovum. Under the influence of hormones- uterus becomes

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
prepared for pregnancy each month. When pregnancy does not take place, the
endometrium of the uterus sheds off in menstrual flow. These cyclic changes continue
throughout child bearing except in pregnancy and lactation. Related organs such as
bladder and urethra are also important because of their close proximity.
The breasts are accessory organs of reproduction. Their main function is to secrete milk
after child birth.
In male, reproductive organs and urinary organs, e.g. urethra, are together. Main
functions of mature reproductive organs of male are:
Hormonal
Spermatogenesis
Secretions from various glands

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Unit 2– PREGNANCY
CONTENT
1.0 INTRODUCTION
2.0 Objective:- At the end of this unit the students should
1. Discuss conception
2. Describe the maternal-foetal environment.
3. Describe maternal physiological adaptation to pregnancy.
4. Outline maternal psychological adaptation to pregnancy.
3.0 Maine Content
3.1. Conception
Fertilization
Definition of terms
Gametogenesis is a process in which germ cells are produced. The
female germ cells are produced. The female gamete (Ovum) is produced in
the grootion follide during oogenesis the male gamete is produced in the
seminiferous tubules of the testes during spermatogenesis.
MEIOSIS:- This is a special process of cell division in gometermy that
reduces the number of chromosomes in each gamete to half of the normal 46
to 23. Therefore, each fertilized ovum will have half of its genetic material
from the mother, and half from the father of the 23 chromosomes, one is a
sex chromosome. The sex chromosome from the mother will always be on X
chromosome. The sex chromosome from the father can be either on X or a Y
chromosome. Ovulation occurs 14 days before the beginning of the next
menstrual cycle – day 14 of a 28-day cycle and day 20 of a 34-day cycle.
Conception occurs when the ovum and sperm unit in the outer one third of
the fallopian tube. The fertilized ovum contains a total of 46 chromosomes
(22 pairs of matched chromosome and 2 sex chromosomes). The fertilized
ovum is called a zygote. A female zygot is created if a sperm carrying on x
chromosome fertilizes the ovum, which results in the zygote having the
female sex chromosomes of XX: a male zygot occurs when the ovum is
fertilized by a sperm carrying a Y chromosome, which result in the zygote
having the male sex chromosome of XY.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
After the fertilization the zygote is transported through the fallopian tube by
a fluid current. The zygote changes through a process called cleavage. The
early cellular changes result in cells called the morale, to blastomere and
then the blastocyst. The developing fetus is called a pre-embryo for the first
2 weeks of gestation, and embryo from week 3 through week 8 and a foetus
until the time of birth.
3.1.2 Embryonic membranes and amniotic fluid: The embryonic membranes,
called the amnion and chorionic, are formed at the time of implantation. The
membranes surrounding the growing embryo and foetus contain amniotic
fluid which is slightly alkaline in nature. The volume of amniotic fluid
ranges from 500-1000ml after 20 weeks of gestation. The fluid is constantly
replaced. The foetus swallows approximately 400-500ml/day. The foetus
also “breaths” amniotic fluid in and out of the lungs. Substances contained in
the amniotic fluid include albumin, bilirubin, creatinine, fat, enzymes,
epithelial cells, lecithin and sphingomyelin.
Functions of amniotic fluid
The functions are
1. Provide a fluid cushion to prevent trauma
2. Allow the foetus to move with ease
3. Maintain the foetus at a uniform temperature
4. Promote development of foetal lung tissues
5. Provide fluid for the foetus to swallow
6. Protect the foetal head during labour.
3.1.3 PLACENTA
The placenta is an organ that provides metabolic and nutrients exchange
between the water and foetal systems. The placenta development and
circulation begin about 3 weeks after conception. The placenta fully formed
and functioning at 3 months of gestation.
At 40 weeks‟ gestation, the placenta contain 15-20 subdivision called
cotyledon and about 6-8 inches in diameter 1-1.2 inches thick and weighs
about one sixth the weight of the foetus. The maternal surface is red, and
flesh like while the foetal surface is shining and smooth.
The placenta produce four hormones
1. Progesterone which is essential for the pregnancy
- It stimulates development of decidedness
- It decreases contractility of uterus
2. Oestrogen or oestrus
- It stimulates proliferation of breast tissue and enlargement of uterus
- It stimulates uterine contractility

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
- Depends on essential precursors from foetal advenal glands and its
production.
3. Human placental lactogenic (HPL) that is also called human chorionic
semotomonimotropin.
- It enhances maternal metabolism
4. Human chorionic gonadotropin (HCG)
- It stimulates corpus lutein to secrete oestrogen and progesterone
- It exerts on effect on interstitional cells of lestes to produce testosterone in
the make foetus.
3.1.4 UMBILICAL CORD
The umbilical cord attaches the foetus to the placenta. It contains two
arteries and one vein. The umbilical vessels are surrounded by Wharton‟s
jelly, which protects the cord from pressure and kinking. The cord is
approximately 50-55cm in length. It is attached to the center of the foetal
side of the placenta. Occasionally it is attached to the edge of the placenta
and this is called Battledore insertion.
3.1.5 FOETAL CIRCULATION
The foetal circulation contain five unique structures
1. Umbilical vein: It carries oxygen and nutrients to the foetus.
2. Two umbilical atria: Which carry deoxygenated blood and waste product
from the foetus.
3. Ductus Venous: This shunts the umbilical vein to the inferior vena cava, by
passing the liver and organs of digestion.
4. Foramen Ovale: This shunts blood from right atria to left atria, by passing
the ventrides and lungs
5. Dustus arferiosus: This shunt blood from pulmory artery to aota, bypass the
lungs.
See fig 1
3.2 MATERNAL PHYSIOLOGICAL ADOPTATIONS TO PREGNANCY.
3.2.1: Cardiovascular System:
The maternal blood volume increases progressively during pregnancy until it is
about 45% above prepregnant levels. A 30%-50% increase in blood volume is due
to increases in both plasma and red blood cells. The pulse may increase to about 10
beats/minutes. The maternal blood pressure is lowered in the second trimester and

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
gradually increased in the third trimester but should not exceed prepregnancy level.
The total RBC increased by 20% while cardiac output increases by 20%-30%. The
haemoglobin may decrease to 10.5g/dL because of the haemodilution. This is
called physiologic anaemia. Iron supplementation is not needed unless the
haemoglobin falls below 10.5g/dL.
White blood cell (WBC) production increases as blood volume increase.
The fibrin level of blood increases by about 40%.
3.2.2 Respiratory System
Pregnancy induces small increase hyperventilation in the mother which causes a
mild respiratory alkalosis. Oxygen consumption increases by about 15%-20%
between 16th and 40
th week of gestation. Vital capacity increases slightly. The
respiratory rate remains unchanged.
3.2.3 Gastrointestinal System
The gastrointestinal symptoms of nowzia and vomiting are common in first
trimester due to secretion of HCG. There is alteration in taste and small are
common. The gum tissue may become soft, swollen and bleeds easily. Gastric
emptying time and intestinal mobility is delayed which leads to bloating and
constipation. Haemorrhoid may occur at late pregnancy due to increase venous
pressure.
3.2.4 Urinary Tract
Urinary frequency occur in the first trimester due to pressure of enlarging uterus on
the bladder near the end of the pregnancy, the weight of the uterus once again
comes pressure on the bladder, resulting in urinary frequency. Dilution of the
kidney, renal pelvis and ureters may occur especially on the right side because of
the elevated progesterone levels and pressure of the enlarged uterus. The
glomerular filtration rate and renal plasma flow increase early in pregnancy.
Glycosuria may occur because of increased glomerular filtration. Clearance of
creatinine and urea increases due to increased renal function.
3.2.5 Endocrine System:-
The thyroid gland has increased vascularity and hyperplasia which is associated
with increased circulating oestrogens. The based metabolic rate rises to +50% in
late pregnancy. The increase is associated with the demands of foetus and uterus
and with oxygen consumption increase. The size of parathyroid increases. The
increase parallels foetal calcium need. The pituitary glands enlarge slightly.
Circulating cortisol levels are increased because of increased oestrogen levels. The
cortisol levels regulates carbohydrate and protein metabolism.
3.2.6 Reproductive System

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.2.6.1 Uterus
The uterus enlarges primarily as a result of an increase in size of myometrial cells.
The size and number of blood vessels and hypnotics increase during pregnancy.
Irregular contractions called Braxton Hicks sign occur throughout pregnancy, but
may not be noticed by the pregnant woman until the third trimester. These
contractions must be differentiated from regular contractions which result in
cervical dilution.
3.2.6.2 Cervix
The endocervical glands secrete a thick, tenacious mucus plug. The plug is
expelled from the endocervical canal when cervical dilation begins. Increased
vascularization causes softening of the cervix, which is called Goodell‟s sign. This
softening also causes easy flexion of the uterus against the cervix called
McDonald‟s sign. The cervix takes on a blue-purple coloration and also caused by
increase vascularization which is called Chadwick‟s sign.
3.2.6.3 Ovaries
The ovaries cease to produce ovum. The corpusluteum persists until the 10th-12
th
week of pregnancy.
3.2.6.4 Vagina and Labia:-
Hypertrophy of vaginal epithelium occurs. There is also increased vascularization
and hyperplasia. The vaginal cells contain higher levels of glycogen, which
redispose pregnant woman to vaginal yeast infection. The vaginal secretions which
are thick, white and acidic are increased.
3.2.7 BREAST
The breast size increases. The superficial veins become prominent. The nipples
become more erectile. Hypertrophy of Montgomery‟s tubercles occurs and
colostrum may leak from the breasts in the last trimester.
3.2.8 SKIN
There is increased level of melanocyte-stimulating hormone that lead to increased
pigmentation. The pigmentation of skin may increase in areola, the nipples, the
vulva, the perenial area, and limen Alba. The increase in pigmentation of the line
from the umbilical to the pubis is called lineanigra 70% of women develop
pigmentation over the forehead, cheeks, and nose. This is called chloasma Striace
(reddish purple stretch marks) may occur on the abdomen, breasts, thighs and
upper arms.
3.3. MATERNAL PSYCHOLOGICAL ADOPTATION TO PREGNANCY

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.3.1 Psychological response to pregnancy:- Pregnancy is viewed as a
developmental stage. The woman‟s response varies according to her own
emotional makeup, her sociocultural background, her support system and her
acceptance or rejection of the pregnancy. The psychological responses include.
- Ambivalence:- This feeling occurs early in pregnancy and is common even
when the pregnancy is planned.
- Acceptance:- This is when the woman accepts the pregnancy. She tends to
display happiness and pleasure and experience fewer physical discomforts.
- Introversion:- A turning inward is common to pregnant women as they
attend to planning for and adjusting to the new baby.
- Mood swings:- The extent of mood swings ranges from ecstasy to great
despair. Mood swings are more prevalent in early pregnancy as hormone
levels increase.
- Body image changes:- Pregnancy is associated with marked changes in a
woman‟s body. These physical changes affect how a woman views herself
as well as how she perceives others to view her.
3.3.2 Maternal tasks of pregnancy; There are four maternal tasks of pregnancy
as the pregnant woman forms a relationship with her foetus and rearranges
family relationship.
a) Seeking safe passage:- This is the most important task for the woman. It is
the process of ensuring the safety of herself and her foetus through
pregnancy and birth by obtaining prenatal care and following the traditional
practices of her culture as they relate to pregnancy, birth and the postpartum
period.
b) Securing Acceptance:- The woman try to secure acceptance of the
pregnancy and body from other family members including reworking family
relationship so that the woman‟s new role as a mother and the new body is
welcomed as a family members.
c) Learning to give of self:- This is a task that must be learned by a pregnant
woman. This process starts when the woman learn she is pregnant and
allows the foetus to grow and develop within her body. Pregnant women
learn to give by both giving and receiving.
d) Committing herself to the unborn child:- This maternal task of pregnancy is
also known as developing attachment to the foetus. This is the only maternal
task that starts in the first trimester and does not end until the end of the new
born period. This task is called “binding in” to pregnancy. The events that
make it more real include feeling foetal movement or heavy the foetal heart
beat. The woman feels protective of her foetus and has increased feeling of
vulnerability. She starts to take please in thinking about her new role as a
mother.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
UNIT 3 ANTENATAL CARE
CONTENT
1.0 INTRODUCTION
2.0 Objectives
At the end of this unit the student will be able to (i) Calculate the expected date of delivery
(ii) Discuss the history taking in antenatal clinic
(iii) Conduct abdominal palpation on pregnant mother
(iv) Identify at risk pregnancy
(v) Describe nutritional needs in pregnancy
3.0 MAIN CONTENT
3.1 Estimating the Probable Date of Delivery (EPD) or Expected Date of Delivery (EDD)
Now after knowing the signs and symptoms, you need to estimate the probable date of
delivery. The exact duration of pregnancy can be ascertained. The duration of pregnancy
is generally 280 days or 40 weeks or ten lunar months. The approximate date of delivery
may be estimated by adding seven days to the first day of the list menstrual period and
counting forward nine calendar months.
Other methods are:
i) By measuring the height of uterus with tape measure in centimeters
ii) By palpating the uterus

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
iii) Estimating the duration of pregnancy by counting forward 22-24 weeks from the
day on which the expectant mother fast feels foetal movement
iv) Dates when pregnancy tests are positive in relation to last menstrual period
v) When foetal heart is first heard by an ordinary foetoscope.
3.2 Maternal Care During Pregnancy
The antepartum (antenatal) period extends from conception until the onset of labour.
Pregnancy is a normal biological event. But it is an unusual one in the life of a woman
and as such requires special attention for promotion of her health and that of her
foetus: For the promotion of maternal and foetal health, the pregnant woman has
several needs. To initiate these needs maternal care during pregnancy is given below.
3.2.1 Initiating Antepartum Care
As soon as a woman suspects herself to be pregnant, she should make an appointment
with the clinic/health workers. The health worker should also identify pregnant woman
during routine home visiting.
The first antepartum contact should be primarily one of the assessment for both the
woman and health professionals. The main purpose of the antepartum contact is to
determine the physiological and psychological responses of the woman to pregnancy by
means of thorough assessment. Three methods of data collection for assessment are
explained below: i) the health history, ii) the physical examination and iii) laboratory
screening procedures. Further assessment of high risk factors and mother-foetal
physiological status are also discussed in this subsection.
i) The Health History
Taking the health history is the most important method of data collection. The history
has to be recorded under the following headings:
a)Menstrual history Age of menarche Regularity, interval, and duration of flow Dysmenorrhoea or other complications Date of first day of, last menstrual period
b) Obstetrical history

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Past pregnancy
Date
Courses of pregnancy labour and postpartum period
Sex, name, birth weight and gestational age of infant
Present health of the child c) Present pregnancy
Planned vs Unplanned
Subjective signs and symptoms d) Medical History
Family
Personal d) Social history
Education of woman and her husband
Occupation of the couple
Marital and sexual history
General health habits, regarding rest and sleep, nutrition, elimination and recreation
ii) The Physical Examination
a) General Examination -Weight, height; blood pressure, temperature, pulse, respiration etc.
b) Obstetrical examination - Examination of breasts, abdominal palpation vaginal examination (if necessary)
iii) Laboratory Screening Procedure
The following laboratory screening tests are done during pregnancy, depending on
individual needs of the woman:
Haematocit haemoglobin
White blood cell count and differential white cell count
Blood grouping
Antibody screening
Urine analysis
Serological examination
Cervical smear
Papanicolaou smear
Blood sugar examination 3.2.2 Assessment of Perinatal Risk or High Risk Factors

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
After completing the history, physical examination and laboratory examination, are
analysed to determine risk factors.
Factors of "high risk" pregnancy
Age-under 15 or above 30
Multigravida
Short statured primi (140 cm and below)
Mal-presentation, multiple pregnancies
Anaemia (Hb 50 per cent and below)
Pre-eclampsia and eclampsia,
Antepartum haemorrhage
Previous still births, Intra-uterine deaths, Instrumental delivery, Caesarian section
Prolonged pregnancy (14 days + after expected date of delivery)
Twins, hydraminios
Pregnancy associated with general disease, viz. cardiovascular disease, diabetes, kidney disease, etc.
3.2.3 Assessment of mother-foetal physiological status
Monitoring of the physicalphysiological changes of pregnancy and the growth and
development of the foetus is achieved by a series of visits by the mother to the clinic at
intervals, throughout gestation. A typical schedule for these visits is as follows:
Once a month for the first 30 weeks
Every two weeks until the 36th week
Every week until the onset of labour
Organising an Antepartum Visit
Determine the purpose of visit
Renew the present plan of care
Collect subjective data
Collect objective data i.e., to check weight, blood pressure, urine testing and haemoglobin testing
Obtain necessary assessment
Modify plan of care based on obtained informations
Give appropriate teaching/counselling i.e. on diet, rest, exercises, etc.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.3 Management of General Health during Pregnancy
Pregnancy is a time of rapid and dramatic physical changes which makes the woman
feel, as well as look, more feminine and attractive.
An increased interest in health awareness is to be created. Advice on the following
aspects should be given to all pregnant women in general and particularly to
primigravida.
Grooming and personal hygiene A daily bath or shower is ideal
Clothing Pregnant mother should be advised to wear loose and attractive cloths.
Footwear Shoes with 4-5 cm heel having a broad base should be worn. Narrow high heels cause
fatigue in maintaining good posture.
Care of breasts and nipples An uplifting brassier should be worn. The brassier should not be tight to depress the
nipples.
Exercise and recreation Outdoor exercise is ideal and pregnant women need to be encouraged to continue with
such outdoor recreation as they have been accustomed to, so long as it does not cause
jolting. Games should not be strenuous. As good brisk walk is excellent. House-work
brings many, but not all muscles into play, so exercises have been devised to keep the
muscles to be used during labour in good trim and the pelvic joint flexible. The pregnant
women should not lift heavy weights, as this may predispose to abortion in susceptible
cases. The woman should not climb to reach high shelves, because of the likelihood of
over balancing and her tendency to faint.
Sexuality In woman who have a history of abortion, coitus should be prohibited during the early
months of pregnancy.
Teeth Soft bristle tooth brush should be used to clean teeth as there may be greater tendency
for gums to bleed.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Use of drugs during pregnancy It is generally believed that most drugs cross the placenta. Drugs taken during
pregnancy exert their effect in many ways. Women should be advised not to take any
medication without the prescription of a doctor.
Smoking Smoking during pregnancy is associated with a significant increase in low birth weight
baby. It is a good health teaching practice to encourage women to stop or at least cut
down smoking.
Fresh air and sunshine The pregnant woman should spend two hours a day in the fresh air, if possible away
from busy streets and preferably walking or sitting in the garden or park.
Safe work environment Woman should not work around ionizing radiation or chemical hazards.
Travel During the first three months the jarring and the excitement may induce abortion in
susceptible women. Industries should consider reassignment of work for the pregnant
woman.
Preparation for infant A room, or area with-in a room is designated as the "baby care unit" and a crib or
bassinet is installed. If there are other children in the family these preparations can be
one way of helping them realise that an infant is coming and allows them to participate
in the fun of anticipation. Some parents, because of their cultural background, may
consider it bad to purchase baby clothe prior to birth of the baby. In these cases the
relatives or neighbour usually have old baby cloths ready. About three weeks before her
due date, the woman should organise her belonging that she plans to take to hospital.
Arrangement should be made for the care of older children.
3.4 Common Discomforts during Pregnancy
Many minor discomforts may be present during pregnancy. They are not serious and
require home remedial measure. When any symptom is severe or persists longer,
medical intervention is indicated. These discomforts are listed below:

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
i) Gastro-intestinal symptoms are nausea, vomiting, heart-burn, flatulence and
constipation
ii) Pressure symptoms are edema, varicosities, hemorrhoids, muscle cramps and
dysponea
iii) Back-ache, pulling pain in lower abdomen
iv) Fatigue
v) Insomnia
vi) Vaginal Discharge
vii) Itching
3.5.1 PALPATION
Palpation is examination by touch using the fingers. It is done to determine
the normalcy of foetal growth in relations gestational age, position and
presentation of the foetus.
Purpose
1. To measure the abdominal girth
2. To determine fundal height
3. To determine abdominal muscle tone
4. To determine the foetal lie, presentation, position engagement of the
head
5. To determine the position location of the foetal height tone
6. To observe signs of pregnancy
7. To detect deviation from normal
Requirements
1. Couch

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
2. Screen
3. Fetoscope
4. Measuring tape
5. Pelvimeter
6. Patients wrapper
Procedure
1. Explain procedure to client
2. Instruct patient to empty her bladder
3. Provide privacy
4. Assist client to lie on the couch or examination table, relax her
abdominal muscle by bending her knee slightly
5. Wash hands thoroughly with soap and dry
6. Rub hands together to generate warmth before beginning to palpate
7. Rest your hands on the mother’s abdomen lightly while giving
explanation about procedure
8. Use flat of the palm and not fingers tips
9. Keep fingers of hands together and apply deep pressure as firm is
necessary to obtain accurate findings.
10. Perform fundal height estimation to determine gestational age
11. Perform the first manoeuve (fundal palpation) to determine
presentation
12. Face the woman’s head, place your hand on the side of the fundus
and curve the finger around the lap of the uterus
13. Palpate for size, shape, consistency and mobility of the foetal part in
the fundus

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
14. Do the second manoeuvre (lateral Palpation continue to face the
woman’s head, place your hands on both sides of the uterus about
midway between the symphysis pubis and the fundus.
15. Apply pressure with one had against the side of the uterus pushing
the foetus to the other side or stabilizing it there.
16. Palpate the other side of the abdomen with the examining finger from
the midline to the lateral and from the fundus using smooth pressure
or rotatory movement.
17. Third manoeuvre (Pawlik’s grip) continue to face the woman’s head,
ensure the woman’s knees are bent.
18. Grip the portion of the lower abdomen immediately above the
symphysis between the thumbs and middline finger of one of your
hand.
19. Fourth Manoeuvre (pelvic palpation) Turn and face the woman’s feet
(ensure the woman’s knees are bent).
20. Place your hands on the side of uterus, with the part of your hand just
below the level of the umbilicus on your finger directing the
symphysis pubis.
21. Press deeply with your fingertips into the lower abdomen and move
them towards the pelvic inlet, the hand covering around the
presenting part when the head is not engaged.
22. The hands will diverge away from the presenting part and there will
be no mobility if the presenting part engaged.
NOTE:
1. Fundal palpation is done to know the gestational age, presentation at
the fundus e.g Breech or cephalic.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
2. Pelvic palpitation is to know whether presenting part is engaged and
determined presentation
3. Lateral palpitation is to identify position of back and foetal limbs
4. Estimate weeks by using birth calculator or tape measure
5. Take fundal height it cm by tape measurement
6. Determine the fundal height using ulnar side of the palm at:
a. 12weeks - Level of the symphysis pubis
b. 16weeks - Midway between symphysis pubis and umbilicus
c. 22weeks - One- two finger breaths below the umbilicus
d. 24weeks - level of umbilicus
e. 28weeks - Five- six finger breaths above the umbilicus
f. 32weeks - Halfway between umbilicus and xiphoid process
g. 36weeks - Level of xiphoid process
h. 40week - Two- three finger breaths below the xiphoid process if lighting has occurred.
3.5.2 Measuring fundal Height using tape method:
1. By using measuring tape, place zero line of the tape measure on the
superior border of the symphysis pubis
2. Stretch the tape across the contour of the abdomen to the top of the
fundus along the midline
3. The number of centimeter measure should be approximately equal to
the weeks of gestation at 22 to 24 weeks
4. Measure the abdominal girth by encircling the woman’s abdomen
with a tape measure at the level of the umbilicus
5. Document findings

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.6 AUSCULTATION
To listen to foetal heart and record the rate.
Procedure
1. Place stethoscope over the convex portion of the foetus, closest to the
anterior uterine wall. Foetal heart sounds are heard over foetal back in
vertex scapular in breech presentations and over the chest in face
presentation
2. Inform the mother of your findings
3. Make her comfortable
4. Replace equipment
5. Document findings
3.7 SUBSEQUENT VISITS
Mother craft talks should be given accordingly on every clinic visit taking
one topic at a time.
Note: clients should have at least 4 antenatal visits before delivery and feel
free to visit the clinic at any time they are or have complaints.
3.7.1 Clinic Routine
1. Mother craft talks
2. Collect card
3. Urine and Haemoglobin estimation
4. (Haemoglobin should be done monthly)
5. Blood pressure estimation
6. Weight
7. Examination, appointments date for next visit given

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
8. Refer clients/patients to doctor if necessary
9. Collect drugs
Tetanus Toxoid (IT) injections to be given when due
3.8.1 Nutritional Care during Pregnancy and Lactation
The human embryo and foetus can obtain nutrient only from mother through the
placenta. If mother is undernourished, adequate growth nutrients may not be available
and intrauterine growth retardation may occur. Both science and folklore have
recognised the important relationship between food and pregnancy. It is necessary to
obtain dietary history along with health history of antepartum mother.
Factors affecting food intake are:
Daily activity
Cultural, religious and family food, customs
Socio-economic status
Psychological factors
Pregnancy symptoms Optimum maternal nutrition and adequate daily food intake are essential during
pregnancy.
The nutritional requirement of non pregnant, pregnant and lactating mother are given
in 2.1.
Calories
Minerals
Protein
Vitamins
Fat
Water
Carbohydrate These are necessary for utilization of energy and synthesis of metabolite-enzymes,
hormones etc.
Table 2.1: Dally Nutritional Requirements of Mothers

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Nutrients Non Pregnant Late Pregnant Lactating
Calories 2200 2200 + 300 (2500) 2200 + 700(2900)
Protein 50 gm 50 gm + 10 = 60 gm 50 gm + 20 = 70 gm
(1 gm per kg body wt.) 10 = 60 gm 20-70 gm
Fat 50 gm 50 gm 60 gm
(1 gm per kg body wt.)
Carbohydrate 395 gm 395 + 65 = 460 gm 395 + 155 = 550 gm
Iron 20 mg 40 mg 30 mg
Calcium 500 mg 1 gm 1 grn
Vitamin A 3000 kg 3000 mg 4600 mg.
Vitamin B 1.1 kg 1.3 mg 1.5 mg
Folic acid 100 kg 150-300 kg 150 mg
Vitamin B12 0.1 kg 1.5 kg 1.5 mg
Vitamin C 50 kg 50 kg 80 mg
Vitamin D 200 kg 200 kg 200 mg
During late pregnancy, energy requirement will increase due to demands of foetus,
placenta, uterus and breasts. Additional daily energy requirement of about 20%
becomes necessary during second half of pregnancy amounting to 300 calories. Energy
requirement of moderately active non pregnant adult woman is about 40 cal/kg body
weight. Energy requirement increases throughout pregnancy. During lactation, for the
production of milk additional 700 calories are required.
Intake of protein is essentially necessary to build tissue protein and is not utilised for
energy purpose. One half of protein must be given as protein of high biological value.
The daily protein requirement of a non-pregnant woman is 1 mg per kg. body weight.
For a woman whose weight is 50 kg., the protein requirement is 50 gms. Protein
requirement of a pregnant woman is 50 gms. plus 10 gms i.e. 60 gms. During lactation,
protein requirement increases to 20 gm.in addition to normal requirement. i.e 70 gm.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Minerals, and sodium chloride requirements during pregnancy is 5-10 gm. It is taken as
common salt and also is present in water, milk and all ordinary articles of diet. During
pregnancy, overloading of salt over 10 gm causes oedema and raises blood pressure.
Daily water requirement is 2.5 litres, since 1 ml is needed for every caloric food intake,
6-8 glasses of water is needed daily.
3.8.2 Mineral requirement during pregnancy and lactation
Iron and calcium requirement increase during pregnancy and lactation. Iron
requirement in pregnancy is 40 mg compared to 20 mg in non pregnant woman and 30
mg in lactation. Similarly, calcium requirement increases to 1 gm in pregnancy and
lactation as compared to 500 mg in non pregnant yeoman. All animal foods e.g. meat,
liver, egg; vegetables e.g. peas, lentils, green leaves and fruits are rich sources of iron.
Milk, egg, cheese and green vegetables are the chief sources of calcium.
Other trace elements necessary for metabolic processes are zinc, copper, magnesium.
3.8.3 Vitamin requirement during pregnancy and lactation
Daily intake of most of the vitamins need to be enhanced during pregnancy. Water
soluble B vitamins, particularly foliate and vitamin B12 are important. Foliate is necessary
for DNA synthesis in growing tissue and red cell formation. Vit B12 is necessary for
haemopoiesis, storage and secretion of milk. Adequate amounts of milk, fruits and
vegetables can supply all necessary vitamins and folic acid. Rich source are fresh green
leafy vegetables, liver and kidney. Lesser amounts are-present in fish, cereals and
muscle meat.
Vitamin B12 is rich in animal food, liver, and muscle meat. It is in lesser amount in fish,
egg, cheese and milk. Fruits particularly lemon and amla are rich (Vitamin C) sources.
Other sources include tomato, sprouted gram and leafy vegetables.
Vitamin A
Animal Source - Codliver oil, milk butter, egg, fish, vegetables such as carrots, spinach,
green leaves and yellow fruits like mango, papaya, banana.
Vitamin D

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Codliver oil, butter, milk, egg.
Other B complex Vitamin
Cereal, pulses, green vegetables, egg yolk.
UNIT 4 LABOUR
CONTENT
1.0 Introduction
A pregnant woman in labour is admitted to the labour room for observation,
treatment, care and safe delivery, which can be in the community or
hospital. This marks the beginning of intra-natal care.
2.0 Objectives; At the end of this unit the student should be able to
1. Prepare the woman for safe delivery
2. Monitor feto-maternal conditions
3. Ensure immediate care of the new-born
4. Prevent infection to mother and child
3.0 Main content
3.1 Principles of labour management
1. Foetal heart rate should be listened to and counted in between
contractions

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
2. Apply sanitary pad when patients is draining liquor
3. No vaginal examination should be done when patient is bleeding
4. Partograph chart should be used for eligible patients
5. Confine patient with liquor drainage to bed to avoid cord prolapsed.
3.2.1 Requirement (Trolley)
Top shelf
1. Delivery kit/pack
2. Sterile gloves
Bottom Shelf
1. Patients charts/Partograph
2. Fetoscope
3. A tray for TPR/B/P
4. Enema tray
5. Kidney dish
6. Razor blade (optional)
3.2.2 Procedure
1. Welcome client and relations
2. Admit her into the first stage room
3. Reassure relations and allow them to wait
4. Take history of labour
5. Obtain clients antennal card to sort out antenatal records if booked or
registered
6. Encourage client to change into labour gown
7. If not booked take full history e.g social, medical/ surgical, past and
present obstetric history

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
8. Obtain urine specimen and test
9. Measure height and record
10. Take and record vital signs/foetal heart rate
11. Carry out general examination and palpation
12. Shave vulva (optional)
13. Perform vaginal examination noting the state of the vulva,
vaginal, cervix, cervical dilation, membranes and position of
presenting part
14. Open partograph chart
15. Document findings in patients admission folder
16. Give enema (optional)
17. Continue observation in the first stage room
18. Inform relatives to stay around until labour is completed
19. Inform doctor immediately or refer if any complication is
suspected.
3.3 MANAGEMENT IN THE FIRST STAGE OF LABOUR
3.3.1 Observation
Temperature - 4hourly, if no pyrexia
Pulse - 2 hourly, hourly as labour Progresses
Respiration - 2 hourly, hourly as labour Progresses
Blood Pressure - 4 hourly if normal, hourly if Abnormal
Contractions - Hourly, ½ hourly, every 10 Minutes as labour
progresses.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
(Note the strength, frequency, duration and record)
Foetal heart rate - ½ hourly throughout labour
(Note rhythm, volume and rate)
1. Bladder – encourage to empty as often as possible, measure amount
and test for protein or acetone
2. General Condition- Note if client rests well between contractions or is
distressed
3. Give copious glucose drinks for hydration and rehydration
4. Note progress in descent of presenting part especially if not engaged
on admission
5. Diet- in early labour, give light diet e.g pap or tea
6. Encourage client to move around if desired as long as she is
comfortable and embrances are intact
7. Give arm bath if permissible
8. Change perineal pad when necessary
9. Vagina Examination – Every 4 hours, note progress in cervical
dilation, position of presenting part, degree of effacement, condition
of cervix (thin or thick), intact or ruptured membranes. In rupture of
membranes, note colour, odour and amount of liquor amnii. Normally,
liquor is clear with a characteristics odour. Abnormally, it may be
meconium or blood stained, offensive odour .
Note: degree of moulding and descent of presenting part
3.3.2 Full Cervical Dilatation:
Transfer to delivery bed

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Set sterile delivery trolley
Position client and encourage her to bear down
Pain in labour can be relieved through the following measures:
1. Breathing exercise (Encourage patients to breath in and out during
contractions)
2. Viewing of television
3. Reading interesting magazines
4. Give psychotherapy
5. Administration of recommended analgesic depending on the stage of
dilation.
THE PARTOGRAPH
Introduction
The partograph is a useful tool for effective monitoring and management of all
the events of labour or progress of labour. It is labour records form designed to
record the patients profile and time of admission and plot salient features such
as the maternal and foetal conditions and progress of labour in a graphic form
after each vaginal examination. It provides the opportunity for early
identification of deviation from normal or prolonged labour and appropriate
action. WHO modified partograph, making it simpler to use as plotting now
begins from the active stage when the cervical dilatation is 4cm.
Contra-Indication to the Use of Partopgraph
Women who are not eligible for Partograph include:
Cervical dilation of 1-3 or 9-10cm
Elective Caesarean Section
Emergency Caesarean Section on admission
Gestational age less than 30 weeks
Ante-Partum Haemorrhage
Severe Pregnancy induced Hypertension (PIH) e.g. Severe Pre-Elcampsia
Mal-presentation and abnormal lie e.g. breech, face, brow, and transverse
lie
Confirmed Cephalo-Pelvic Disproportion (CPD)
USE OF PARTOGRAMPH (recording and charting)

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Record patient’s information: full name, gravida, parity, hospital number,
date and time of admission at the top of the graph/form. The actual time of
the day if recorded as „zero-time‟ below the hour line.
Locate the right hour line/column and record maternal vital signs:
- Temperature and respiration in the spaces provided
- BP as a plus sign (+)
- Pulse as a dot sign (.) in the block between the time lines and
- Connect the dot using a ruler or straight edge
Record urinary data as: Volume in mls, Protein 0 to 4+; Ketones 0 to 4+
Record drugs and rehydration fluids including oral and intravenous in the
space provided (if given).
Record Oxytocin given in a separate column above the column for fluids and
drugs.
Plot FHR with a dot(.) in each square and on the time line and conntect the
dots using a ruler or straight edge
Record findings on amniotic fluid as:
I: Membranes intact OR A: Liquor is absent
R: Membranes ruptured
C: Membranes ruptured; clear fluid/liquor
M: Meconium stained fluid/liquor
B: Blood stained fluid/liquor
Record and plot findings on moulding in the corresponding time hour as:
- “O: no moulding
- +: mild ++@moderate +++: severe
Plot finding on cervical dilatation in the corresponding time hour as a cross
(x) beginning from 4cm
Plot findings on uterine contractions (frequency and duration) in the
corresponding time hour as a cross (X) beginning from 4cm.
Plot findings on uterine contractions (frequency and duration) in the
corresponding time hour as:
(Dots) Mild Uterine contractions of less than 20 seconds duration per
10 minutes
(Diagonal lines) Moderate contractions of 20 to 40 seconds duration
(Solid colour) Strong contractions of longer than 40 second duration.
Note:
All observations on the maternal and foetal conditions are to be
recorded on the time line at which the observations are made at the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
bottom of the partograph every 4 hours during the latent phase and 2
hourly during the active phase.
Encourage the mother to empty her bladder every 2 hours

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.5 VAGINAL EXAMINATION
It is the examination done vaginally to ascertain the state of the
vagina and cervix, diagnose and assess the progress of labour,
Purpose
1. To ascertain onset labour
2 Monitor cervical dilatation
3. Identify fetal presentation
4. Ascertain if membranes hove ruptured
5. Identify risk for cord prolapse
6. Assess progress in labour
7. Confirm full dilatation
8 Assess status of head and degree of moulding
Requirements
A sterile vaginal examination tray containing.
1. 2 Gaillipots
2. 1 Kidney dish
3. 3 dressing towels
4. 2 perineal pads
5. Kocker’ (Artery forceps)
6. 1 Cusco’s or Sims vaginal speculum (optional)
7. Sterile gloves
8. Face mask
9. 2 urethral catheters
10. Hibitane cream (lubricant)
1 1 . Lotion for swabbing e.g. savlon 1:200

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
1 2. Screen
Procedures
1. Explain procedure to client
2. Encourage client to empty the bladder
3. Emphasize the need for cooperation during the procedure
4. Read the patient’s chart for Previous findings
5. Set requirement on the trolley
6. Screen the bed to provide privacy
7. Position the woman in a lithotomy position
8 Drape the patient
9 Do surgical hand washing
10 Wear sterile gloves
11. Observe the external genitalia
1 2. Clean the vulva and perineal area with cotton swab.
13. Lubricate the index and middle fingers with hibitane cream
1 4. lnsert examining fingers into the vagina, explore and note the
following:
15. If the vaginal walls are moist or dry; warm or hot, feel for scar from
previous perineal wound, cystocele or rectocel
16. Examine the cervix and locate the OS
17. Asses the cervix for: effacement, dilatation, consistency (thick or thin)
18. Assess the level of presenting part in relationship to maternal ischial
spines
l9. Identify the presentation by feeling the hard bones of the vault of the
skull, fontanels and sutures
20. Assess moulding by feeling amount of over lapping of the skull

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
bones
21 . Remove your fingers from the vagina and observe the colour of
secretion and amniotic fluid
22. Make client comfortable
23. Explain your findings to client
24 Document all your findings on the partograph
Point to note on Vaginal Examination
1. Vulva- Any signs of infection, discharge, Oedema, varicose veins and
circumcision scar
2. Perienum – Any scar
3. Condition of membrane- intact or ruptured. If ruptured note colour,
odour and amount of amniotic fluid
4. Vagina – warm and moist, hot or dry
5. Cervix- Effacement and application to presenting part, consistency
(soft, thin or thick and unyielding)
6. Cervical OS- Degree of delatation
7. Presentation- station of presenting part, position as determined by
sutures and fontanelles, presence of caput or excessive moulding
8. Adequacy of pelvis – Inability to reach the sacral promontory, none
prominence of the ischial spines.
a. Accommodation of 4 knuckles of a clenched fist
between the buttocks and the two Ischial
tuberosities
b. Admission of two stretched fingers under the pubic
arch.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.6.1 MANAGEMENT OF THE SECOND STAGE OF LABOUR
This is the period from full dilatation of the cervical OS to the delivery of the
baby. More frequent observations should be made of both mother and
baby.
Observations
1. Mother
a. Contractions:
i. Frequency
ii. Strength
iii. Duration
iv, Character – Bearing down or expulsive
b. Pulse: Check every 1 5 minutes and record.
c. Blood Pressure: Check and record as directed b Midwife in charge.
d. Bladder: Check and see that bladder is empty if not catheterise to empty
it.
e. Note Signs of Second stage:
i. Advancement of presenting part
ii. Bearing Down urge
iii. Gapping of the anus, etc.
iv. Confirm 2 stage by vaginal examination transfer to delivery bed
f. Note general condition of mother: whether between contractions or
exhausted.
g. Give oral glucose drinks
2 Foetus
a. Foetal heart rate
i Check after each contraction

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
ii Record every 5 minutes
b Observe and report abnormalities e.g.
i. Meconium stained liquor (except in breech)
ii Rapid slow foetal heart rate
3.6.2 Mechanism of LOA and ROA
Definition: Mechanism of labour is the series of pas’vt movements of the
fetus during its passage through t) maternal pelvis during labour.
Principles of Mechanism of Labour:
1. Descent takes place through-out labour
2. Whichever part leads and first meets the resistance of the pelvic floor
will rotate forward until it comes under the symphysis pubis.
3 Whatever emerges from the pelvis will pivot around the pubic bone.
LEFT OCCIPITO ANTERIOR (LOA)
Lie : Longitudinal
Presentation : Vertex
Position : LOA
Attitude: Flexion
Denominator: Occiput
Presenting part: Posterior port of the right parietal bone.
Engaging diameter:sub-occipito bragmatic (9.5cm)
• Descent
Descent takes place due to forceful uterine contraction c retraction, rupture
of membranes, complete dilatation.
Flexion
When the head meets the resistance flexion is increased.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The increased flexion will decrease the presenting diameter of sub
occipito-frontal (10cm) to a smaller diameter suboccipito-bregmatic
(9.5cm).
The occiput becomes the leading part.
Internal rotation of the head
The occiput leads and reached the pelvic floor first and rotates
anteriorly 1/8th of the circle to come under the symphysis pubis.
The anteroposterior diameter of the head now lies in the
anteroposterior diameter of the pelvic outlet.
Crowning
The occiput slips beneath the subpubic arch and crowning occurs
when the head no longer recedes back between the contractions and
the widest transverse diameter (biparietal) is born.
Extension of the head
The fetal head pivots around the pubic bone while the sinciput, face
and chin sweep the perineum and head is born by the movement of
extension.
Restitution
The twist in the neck of the fetus that resulted from internal rotation is
now corrected by a slight untwisting movement.
The occiput moves 1/8th of the circle towards the side from which it
started.
23. Explain your findings to client
24 Document all your findings on the partograph
Point to note on Vaginal Examination

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
9. Vulva- Any signs of infection, discharge, Oedema, varicose veins and
circumcision scar
10. Perienum – Any scar
11. Condition of membrane- intact or ruptured. If ruptured note
colour, odour and amount of amniotic fluid
12. Vagina – warm and moist, hot or dry
13. Cervix- Effacement and application to presenting part,
consistency (soft, thin or thick and unyielding)
14. Cervical OS- Degree of delatation
15. Presentation- station of presenting part, position as determined
by sutures and fontanelles, presence of caput or excessive moulding
16. Adequacy of pelvis – Inability to reach the sacral promontory,
none prominence of the ischial spines.
c. Accommodation of 4 knuckles of a clenched fist
between the buttocks and the two Ischial
tuberosities
d. Admission of two stretched fingers under the pubic
arch.
3.7.1 ACTIVE MANAGEMENT OF THIRD STAGE OF LABOUR
(According to WHO)
1. Give Oxytocin 10 units IM within one minute of the birth of the baby
after checking for a second baby
2. Controlled cord traction to deliver placenta. Wait for strong uterine
contractions (2 -3 minutes). Assist delivery of the placenta by
controlled cord traction while holding the uterus up
3. Massage uterus: massage the uterus immediately after delivery of the
placenta for 1 5 seconds

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Note:
Oxytocin is given within one minute of the baby’s birth (after checking
for a second baby)
do not wait for separation instead:
feel the top of the uterus for a contraction
wait for the uterus to contract
apply controlled cord traction while holding the uterus up
Placenta delivers by controlled cord traction while holding the uterus
up. Mother does not push
Massage the uterus immediately after the placenta delivers
3.7.2 Controlled Cord Traction
1. On completion of delivery, take pulse, note colour and keep client
comfortable.
2 Place end of cord with clamp into a sterile kidney dish and place
between the client’s thighs.
3. With hand above pubic bone, apply pressure in an upward direction
(towards the woman’s head) to apply counter traction and stabilize
the uterus
4. At the same time with the other hand, pull with steady tension on the
cord in a do5 Receive placenta with cupped hands and gently
ease the membranes out.
6 Place placenta in the kidney dish and leave at the bottom of the
trolley.
7 Check for firmness of the uterus
8. Clean the vulva, separate labia and inspect vaginal wall for
laceration.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
9 Check perineum for laceration or extension episiotomy (laceration or
episiotomy is to be repaired within an hour of delivery).
10. Check uterus again and expel blood clots.
11. Collect clots and add to previous loss.
12. Clean client up, apply vulva pad and make client comfortable.
1 3. Take and record vital signs.
14. Offer something to drink or eat
1 5. Wheel out delivery trolley to the sluice room:
a. Examine placenta and membranes completeness and weigh
b. Measure blood loss.
c. Discard all other things on the trolley.
16. Record findings and complete labour charts.
17 Weigh baby and record.
1 8. Leave mother and baby to rest but they must 4 observed closely.
19. After one hour, detailed examination of the baby is carried out. The
cord is shortened and temperature recorded.
20. If baby’s condition is satisfactory, clean baby and warm.
21 Bathe mother, allow her to pass urine, check uterus, check blood
loss, take and record vital signs.
22. Inform postnatal word staff, and
23. Transfer mother and baby to the postnatal ward.
3.7.3 EXAMINATION OF THE PLACENTA
There should be a thorough inspection and examination of the placenta
and membranes, soon after expulsion for its completeness. The
management of the third stage of labour is not considered ended until the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
placenta and its membranes have been examined and found to be
complete.
Purpose
1. Ensure that the entire placenta and membrane hove been
expelled and no part has retained.
2. Make sure that placenta is of normal size, shape, consistency and
weight
3. Ascertain the health of the cord, number of blood vessels and site
of the insertion of the cord
4. Check weight of placenta and measure length of cord.
5. Assess abnormality such as infarctions or additional lobes or
additional lobes
Requirements
1. Placenta in a bowl
2. A washable surface to lay the placenta for examination
3. Weighing scale
4. Kidney dish
5. Pair of clean gloves
procedure
1. Examine the placenta under running tap
2. Using gloved hands to hold the placenta by the allow the
membrane to hang (twisting the cord twice around the fingers will
provide a firm grip)
3. Identify the opening through which the baby was delivered.
4. Hold the cord with the placenta and membranes hanging down to
check for

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
completeness membranes.
5. Insert hand through the opening and spread fingers to view the
membranes and blood
vessels.
6. Remove the hand from inside the membranes and lay the placenta
on a flat surface with
the foetal surface up. Identify the site of cord insertion.
7. Examine the two membranes, (amnion and chorion for
completeness and presence of
abnormality indicating succenturiate lobe
8. Invert the placenta, expose the maternal surface and remove clots
present.
9. Examine the maternal surface by spreading it in palms of your two
hands and placing the cotyledon in close approximation.
Note: any missing lobe or fragments.
10. Assess for presence of abnormalities such as infarctions,
calcifications or succenturiate
lobes.
11 . lnspect the cut end of the umbilical cord for presence of three
umbilical vessels.
12. The placenta is weighed, and important facts regarding if are
recorded in the chart.
13. The blood loss, including clots, is poured into a measuring jug and a
good estimate of the spiIIed blood is made and recorded (Blood loss above
500mls within 24 hours of delivery is considered primary PPH).
NOTE: The examination of the placenta is a very important duty of the
midwife because of the danger of a cotyledon or fragment of membranes

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
being retained. If the placenta is normal and the doctor has not requested
that if should kept for inspection, it is disposed of by burying if possible.
It is important to report to the doctor immediately if it is thought that a piece
of placenta tissue or membrane has been retained.
The midwife must not leave her patient, for she may have a severe
haemorrhage at any time while it remains in the uterus
3.7.4 Vulva swabbing (Perineal care)
Introduction
Perineal care involves cleaning of the genitalia with antiseptic lotion.
principle
Clean from the cleanest to the less clean area
Introduction
- Patients who are unable to carry out self care
- Patients with indwelling catheters
- Patients with surgical interventions
Requirements (trolley procedure):
Top shelf:
- Bowl with cotton balls
- Long artery forceps in a receiver
- Receiver for used swabs
- Sterile gloves
- Clean linen

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
- Perineal Pads
Bottom shelf:
• Mackintosh
• Bedpan
• Lotion for swabbing e.g savlon 1:200
Extra requirement
• Screen
Procedure
- Greet client and introduce self
- Explain the procedure lo the client and obtain consent
- Provide privacy
- Encourage client to empty bladder
Position and drape client
- Wash hands and put on gloves
- Hold swabs with forceps and clean from top to bottom
- Use one swab once and discard
- Clean the perineal region and anus thoroughly
- Remove the equipment
- Make client comfortable
- Wash hands
- Document findings

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Non-Pneumatic Anti Shock Garment (NSAG)
The non-pneumatic anti shock garment (NSAG) also known as “Life Wrap” is a
first-aid device that reverses hypovolemic shock and decreases obstetric
haemorrhage. It was recommended by WHO in 2012 as a life saving device for the
treatment of life threatening post-partum haemorrhage and hypovolemic shock in
low referral facilities and treatment delays pending clients transfer for definitive
management. It is easy to apply after a brief training. It is no replacement for
standard definitive care, protocol should be followed. It is made up of washable,
reusable light weight neoprene close tightly with Velcro. It is about 1.5kg in
weight, cuts into segments labelled 1,2,3,4,5, and 6 which contain a foam ball for
extra pressure and adaptable to a wide range of women. Each segment of the
device is wrapped in sequence around the legs, pelvis and to the navel region and
looks like a lower half of wet suit or “a trouser”. It is applied as soon as a signs of
shock are identified with three segments on each leg, one segment over the pelvis
and another, over the abdomen. T is contraindicated in patient with heart diseases.
It is designed to give easy access to other interventions such as vaginal procedures,
perineum and episiotomy repair, as well as surgical procedures by removing
segments 5 & 6. It comes in different colours including blue, green, black and
brown. It must be applied by a single person except in an unconscious mother.
MECHANISM OF ACTION
The NASG act by ensuring circumferential compression of the abdomen and legs
reduces total vascular volume (container size) while expending the central
circulation.
Purpose
- To control postpartum haemorrhage
- To treat shock
- To resuscitate, stabilize and prevent further bleeding
NASG APPLICATION PROCEDURE
Position patient in a lying position on a flat surface
Wear a pair of glove
Open the NASG and place under the woman ensuring that the part labelled 5
matches the patient‟s navel, if the patient is unconscious, two people can roll
her onto her side placing the garment underneath her, similar to making an
occupied bed.
Stretch and fasten the garment tightly, starting with the ankle labelled
segment 1

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Continue with segment 2 below the knees and segment 3 on the thighs (for
shorter women, fold segment 1 into segment 2 before starting to ensure that
segments 1 & 2 are below the knees).
Secure the pelvic segment 4 tightly at the level of the symhpysis pubis
Apply segment 5 over the umbilicus (navel) and close by securing the two
flaps of segment 6 over segment 5 (do this one at a time on each side).
If the woman experiences difficulty in breathing, slightly loosen-but do not
remove the abdominal segment..
Monitor the patients pulse rate and BP every 15 minutes until stable
Monitor the urinary output hourly.
Resuscitate the patient with IV fluids and/or blood as required (give 3mls of
fluid for every 1ml of blood loss).
If NASG application does not result in prompt increase systolic blood
pressure (SBP) and decreased pulse, check for adequate tightness and give
additional IV fluids.
Determine the cause of haemorrhage
Refer patient to the nearest higher facility while still on NASG (between 12-
36hours) if there is no improvement in the condition of the patient.
NASG REMOVAL
The NASG must be removed only under skilled supervision in a setting
where vital signs can be monitored and there are adequate IV fluids.
The NASG should not be removed until the woman has been
haemodynamically stable for at least 2 hours with blood loss 50ml/hour,
pulse 100BPM and SBP 100mm Hg.
To safely remove NASG, with the ankle segments and proceed upwards.
Allow 15 minutes between opening each segment for the redistribution of
blood, then check vital signs.
If SBP falls by 20mm Hg or the pulse increase by 20BPM, rapidly replace
all segments and consider the need for more saline or blood transfusions.
If there is recurrent bleeding, replace the NASG and determine the source of
bleeding.
Clean the garment in .01% chlorine solution and store in a cool dry place
after removal.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
MODULE 2 CHILD CARE
UNIT 1 CARE OF NEW BORN
UNIT 2 CHILDHOOH
UNIT 3 ADOLESCENT
UNIT 4 ANTHROPOMERY
UNIT 5 FAMITY PLANNING
UNIT 6 FAMILY RECORD
UNIT 1 CARE OF NEW BORN
CONTENT
1.0Introduction
2.0 Objectives
3.0 Main Content
3.1 Delivering the baby
1.0 CARE OF THE NEWBORN AT BIRTH
1.1 Delivering the baby
THE HEAD
1. As head is delivered, the midwife quickly picks a gauze swab and
wipes mouth, nose and face using a swab at a time.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
2. Give a gentle handling.
THE BODY
1. The body is delivered over the mother’s abdomen
2. Clamp and cut cord
3. Record time of birth and Apgar score at birth, 5 minutes and 10
minutes
4. Clean eyes and apply 0.4% terramycin eye ointment or erythromycin
eye ointment (when medically indicated)
5. Dry body, wrap and keep warm
6. Note sex of baby, show sex to mother
7. Apply name tag on baby’s wrist
8. Quickly examine baby from head to toe
9. Put baby to breasts
3.2 SIMPLE RESUSCITATION
This is carried out when the Apgar Score at birth is between 7 to 10
Requirements
1. Mucus extractor/ catheter (or improvise)
2. Clean gauze
3. Clean dry cloth to keep baby warm
4. Oxygen giving set (cylinder nasal catheter or face
mask or Ambubag
Procedure
This is for healthy baby with Apgar 7:
1. Keep baby warm with a dry cloth
2. Clean nose and mouth
3. Look to see if the baby is breathing
4. Place your hand on the chest over the heart

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
5 Feel how regular, strong and fast the heart is beating
6. Look at baby’s Colour
7. Dry baby quickly and keep baby warm
8. Handle baby gently
9. Place baby on mother’s chest if no problem
10. Cover both mother and baby with cloth.
3.3 Physical Examination of New born
A good examination of the baby is normally Carried about one hour after
birth and before the bath ( hour) when the temperature is stable. A general
physical examination of the new-born is done systematically to detect any
abnormality
Requirement
A tray Containing the following
1. A gallipot with swabs
2. Another gallipot with sterile water
3. Kidney dish for soiled swabs
4. Rectal thermometer in its container or kidney dish with a lubricant
5. Measuring tape
6. Weighing scale
Procedure 1. Do a general examination from head to toe
2. Check Patency of anus using rectal thermometer
3. Measure length, head circumference and baby
4 Treat the cord with 7.1 percent chlorhexidine
5 Re-clamp the cord and cut
6 Keep baby warm with cloths

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
7 Put baby in warm cot
7 Transfer baby with mother to Postnatal warm
Procedure
1. Prepare a flat Surface preferably a table(cover surface with a clean
sheet)
2. Take tray to the prepared table
3. Wash hands thoroughly
4. Bring the baby out from the cot, Unwrap and qui weigh the baby if the
was not done at
birth
5. Take the following measurement
a. Length: grasp the baby’s feet and gently turn baby upside down.
Measure from the heels to the vertex.
b. Head circumference. Measure from the sinciput through the Occipital
protuberance round the head
The Head
The head is examined for the following:
1. Excessive moulding
2. The width of the sutures and size of the fontanelles.
3. Large caput formation
4. The size of the head whether too large or too small
5. Any abnormal growth
6. Bruises on the head
The Eyes
Examine the eyes for:
1. Presence of the eye balls
2. Discharges

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3. Sub-conjunctival haemorrhage
4. The setting of the eyes: too closely set or wide apart
5. Yellowish discolouration
Nose:
1. Take note of the presence of the nostrils
2. Any discharge
Mouth:
The mouth is examined with a good light taking note of:
1. Any tongue tie
2. Presence of teeth
3. Harelip and cleft palate
The Ears
1. Examine the ears for the lobes
2. The setting
3. The openings
4. Discharges
The Neck
The length —whether it is too long or short, presence of any congenital
growth.
The Chest
1. Shape and size of the chest
2. Type and rate of respiration, note any abnormality
The Abdomen

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Take note of the size of the abdomen to identify any abnormality such as:
1. Hydropsfefalis and exomphalus
2. Check the cord for any bleeding
3. Check for femoral or inguinal Hermia or hydrocele
External Genitalia
1. The sex of the baby should be identified
2. In the male, the scrotum and testes should be for any abnormality
3. In the female, check size of the labia majora and minora.
4. Check to make sure that the two openings are (Vaginal and urethral
openings)
5. Check for position of urethra in the penis
6. Any abnormality should be noted,
1. Pick Anal thermometer, shake down and wipe it with a wet swab.
2. Lubricate and insert into the anus to determine whether it is
perforated or
3. Take the temperature at once and record.
The Back
1. Inspect the back for presence of spinal bifida and any discontinuity in
the vertebrae.
2. The Hip: The hip is examined for any abnormalities
e.g. congenital dislocation of the hip.
3. For this, Barlow’s or Ortolani’s test is done. The thighs flexed and
abducted through 90 degree. A clicking sound, denotes an
abnormality.
The Extremities

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The upper and lower extremities are examined accordingly
1. Equality
2. Mobility
3 Fracture
4 Extra and webbed digits
5 Talipes of the legs
At the end of the examination, any abnormality detected should be
recorded and reported for Prompt action to be taken. The baby is then
given the first bath and dressed up.
3.4 SUBSEQUENT CARE OF THE NEWBORN
Daily Bathing of Baby
The baby needs daily baths.
A trolley with the following:
Requirements
A trolley with the following:
Top Shelf
A tray Containing.
A. Bathing Soap in a Soap dish
B. Talcum Powder
C. Chlorhexidine gel
D. Olive oil
E. Vaseline
F Baby lotion (optional)
G. Sterile Swabs in gallipot
H. Comb and brush
I. Kidney dish Containing Sterile Scissors

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
J. Sterile water in gallipot
K. Extra ligature
L. 2 jugs-one Containing cold water and the other Water
Bottom Shelf
a) Baby Clothing
b) Face flannel
c) Large towel
d) Kidney dish for used swabs
e) A bath, thermometer
f) A large basin or plastic bowl on a stand
9) A bucket for used water
Procure
1. Assemble requirement
2. Close nearby doors, windows and turn off fans to
avoid draught
3. Put on water-proof apron and wash hands
4. Prepare the bath water to a temperature of 37.20c (the
temperature of the water can be determined with the
bath thermometer or by using the elbow)
5. The baby is wrapped with a large towel to avoid chills.
6. Clean the face and head with warm water, using each swab once
only.
7. Swab eyes from inside out with cotton wool
8. Clean face and dry with face flannel
9. The head is washed by supporting the baby’s neck in the left hand

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
10. The body may be tucked under the Midwife’s arm or supported on the
lap. The head is dried with a towel
using the flat of a hand.
11. Change water
12. The towel is unwrapped.
13. Remove venix-caseosa if present with swab dipped in warm olive oil,
and soap the baby paying particular attention to the skin folds.
14. The baby is immersed in the bath, the head and shoulders supported
on the Midwife’s left arm while
she washes off the soap with her right hand.
15. The baby is lifted out and placed face downwards on the towel.
16. The back is dried and baby turned over to dry the front
17. Wash your hands and treat cord with chlorhexidine gel.
18. Should the cord bleed or is longer than normal should be re-ligatured
and shortened with scissors.
19. Vaseline is applied to the buttocks and the diaper (e.g pampers) put
on.
20. The baby is dressed; hair combed, and wrapped in a shawl and lay
on its side in the cot.
3.5 SUBSEQUENT CARE OF THE CORD
The umbilical cord is treated twice daily.
Requirements
A tray containing:
1. Chlorhexidine gel
2. Sterile cotton wool swabs in a sterile bowl or dressing pack can be
used.
3. Gauze bandage and dressing if needed

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
4. A receiver for used swabs.
Procedure
Care of the cord is usually carried out along with bathing the child or when
the napkin is completely soiled.
1. Assemble the requirements and wash your hands clean
2. In some hospital a cord dressing pack is used
3. Expose the cord and clean with 7.1 percent chlorhexidine gel.
4 One stroke at a time from the cord end, for the first dressing.
Subsequently, start from the stump to the end of the cord.
5. After cleaning, expose to air (open method)
6. Apply napkin below the umbilicus and make baby comfortable
7. Cleaning is done at least twice daily or more often when the napkin is
soiled
8. Note and record abnormalities such as redness, offensive odour or
bleeding.
9. Report to doctor when any of such abnormalities arise.
1 0. When the cord falls off and there is no inflammation, clean stump with
chlorhexidine as
often as - possible.
NOTE: Cord usually falls off between the 4 -10th day.
3.6 KANGAROO MOTHER CARE
Requirement
Baby in socks, nappy and a cap
Front-open top

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Baby shawl
2 bowl with clean and Soapy water
Hands towel
Procedure
Explain the procedure to the mother
Gather necessary equipment
Wash hand with soap and water and dry
Ensure warm and clean environment
Observe baby’s general condition, including the vital signs to ensure
fitness
Dress the baby in socks, napkin and a cap
Place the baby between the mother’s breast
Secure the baby on the mother’s chest with a cloth
Put a blanket or shawl on top for additional warmth
Instruct the mother to put on a front opened top to maintain an
effective skin to skin contact
Instruct mother to keep baby up right when walking or sitting
Counsel the mother on the importance of having the baby in a
continuous skin to skin contact twenty four hours daily
Advice the mother to sleep in half sitting position in order to maintain
the baby in vertical position.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
UNIT 2: CHILDHOOD
CONTENTS
1.0 Introduction
2.0 Objectives
3.0 Main Content
3.1 The Neonate
3.1.1 Pre-natal Development
3.1.2 Physiological Status of Neonate
3.1.3 Assessment of the Neonate and Nursing Management
3.1.4 Common Health Problems of Neonate
3.2 The Infant
3.2.1 Growth and Development
3.2.2 Health Promotion
3.2.3 Common Health Problems
3.3 The Toddler
3.3.1 Growth and Development
3.3.2 Promoting Optimum Development
3.4 The Pre-Schoolage
3.4.1 Growth and Development
3.4.2 Psychosocial Development and Play
3.5 The Schoolage Child

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.5.1 Growth and Development
3.5.2 Mental and Psychosocial Development
3.5.3 Health Promotion
4.0 CONCLUSION
5.0 Summary
6.0 Tutor-Marked Assignment
7.0 References/Further Reading
1.0 INTRODUCTION
The child has to pass through various stages of growth and development. Safe childhood
and adolescence are the essence of child survival and family welfare in primary health
care. In this Unit you will learn about prenatal development of the foetus, care of the
neonate and study the growth and development of infant and toddler. Growth and
development of preschool and school age will be explained. You will be made familiar
with the health problems of the child at various stages of development, and their
prevention. Finally you will study the physical and intellectual development of the
adolescent both male and female.
2.0 OBJECTIVES
In this unit you will learn various developmental stages of a child in order to give the
child a safe childhood and adolescence.
After going through this Unit you should be able to:
Describe physiological status of new-born
Advise on care of new-born
Describe the growth and development of infant
Explain the procedure of infant weaning
Explain the growth and development of pre-school and school-age child
List the common health problems of various stages of development
Advise on their prevention.
3.0 MAIN CONTENT

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.1 The Neonate
The neonatal period is from birth to 28 days. The neonate after birth has to make
physiological adjustment to extra uterine environment. Health status of newborn
depend; on pre-natal development. The pre-natal development, physiological status,
assessment and common problems of neonate are briefly described in the following
subsections.
3.1.1 Pre-natal Development
Development from zygote to fully mature infant is due to two process:
1. Growth that result when cells divide and synthesize.
2. Differentiation by which these cells are systematically organised to form all the
tissues necessary to assure an organised, coordinated individual.
The development process is as follows:
Embryogenis
Soon after fertilization, the zygote changes into morula stage, and followed by
blastocyst stage. The outside layer of blastocyst is called trophoblast. The collection of
cells inside the blastocyst is called inner cell mass. Implanation occurs on the 9th day.
Villous structure at the point of attachment forms the placenta and chorion. Embryonic
cells form the amnion.
Foetal Growth
Foetal growth is accomplished by two processes - Hyperplasia and Hypertrophy. Most
rapid linear growth takes place: during mid-foetal life. The most rapid gain in weight
occurs in late foetal life.
Environmental Factors
Before birth unfavourable maternally imposed environment may produce long range
health problems in the infant or child. These factors are maternal age, chemicals,
infections, radiations and mechanical factors.
3.1.2 Physiological Status of Neonate

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
New-born period or neonatal period is the first 28 days after birth. The first 24 hours of
birth are the most critical period during which respiration is initiated. Heat loss can also
occur through conduction and convection and neonate has to adjust to extra uterine
life.
The physiological status of new-born is given below:
Respiratory system: Respiration in new-born is abdominal. The rate is generally 30-50
breaths per minute.
Haemopoietic system
The average red blood cells count of the new-born is 5 million/ mm 3. The average
hemoglobin value at birth is 16-18 g/100 ml of blood. The levels of serum bilirubin from
the breakdown of red blood cells rises due to immaturity of liver of new-born.
Fluid and electrolyte balance
The infant has higher ratio of extracelluler fluid than the adult and higher level of total
body sodium chloride and a lower level of potassium.
Thermoregulation
The major sources of body heat are heart, liver and brain. There is an additional source
unique to neonate, that is brown fat. It has a greater capacity for heat production.
Gastro-intestinal system
The stomach has a capacity of 90 ml. The intestines are longer in relation to body size.
Regurgitation is common due to immature cardiac sphincter. Enzymes are adequate to
handle digestion. The liver is most immature.
Renal system
All the structural components are present in the renal system. But their functional
deficiency exists in the kidneys.
Integumentary system
All the structures within the skin are present but many of the functions are immature.
The protective function of the skin is fairly efficient.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Musculoskeletal system: Contains larger amounts of cartilage than ossified bones. The
process of ossification is rapid during the first year.
Defences against infection
The infant is born with several defences against infection and is protected against major
neonate diseases.
Endocrine system
Is adequately developed. Maternal sex hormone causes engorgement of infant breast
which secretes milk during the first few days of life. Female new-born may have pseudo
menstruation due to sudden drop of the level of oestrogen and progesterone.
Neurological system
At birth, the nervous system is incompletely integrated. Most of the neurological
functions are primitive reflexes.
Sensory functions
1. Taste
The lips and tongue are very sensitive. The sense of taste is not very well developed, but
babies seem to prefer sweeter food.
2. Hearing
Loud noises cause the baby to cry, but the ability to discriminate between sounds is not
developed for two or three months.
3. Sight
True vision is not present at birth, but at one month the baby looks towards bright light.
The eyes do not focus properly for some weeks.
3.1.3 Assessment of the Neonate and Nursing Management
The assessment includes physical and neurological assessment as given below. We shall
briefly discuss this here. The physical assessment
1. Head circumference: 33 to 35.5 cm

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
2. Chest circumference: 30.5 to 33 cm 3. Crown to rump length: 31 to 35 cm 4. Head to feet length is 48 to 53 cm 5. Weight 2700 to 4000 g. Vital signs
1. Temperature: 35.5°C to 37.5°C 2. Pulse: 100 to 140 beats per minute 3. Respiration: 30-50 breaths per minute. General appearance
Posture
Is one of flexion, a result of inutero position.
Colour
The infant becomes red when crying.
Skin
The skin is smooth and puffy. The skin is covered with vernix caseosa, lanugo is present
on the skin.
Milia as tiny white papules appear on the cheeks. Several colour changes may be noted
on the skin.
Head
The nurse palpates the skull for all patent sutures and fontanelle noting the size, shape,
moulding and for any presence of Caput succedaneum and cephalohaematoma.
Eyes, ears and nose
Are examined to detect abnormalities.
Mouth
The nurse inspects the mouth and looks for cleft lip and palate.
Neck, chest, abdomen, genitalia, lower extremities and back are examined to locate.
congenital abnormalities especially for imperforated anus.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Neurological Assessment
Several reflexes such as sucking, gaging, resting, corneal and papillary reflexes are
usually observed during physical examination. Several other reflexes are seen such as
moros reflex, tonic neck and startle reflex.
Nursrng Care of the Neonate
We have discussed the physical and neurological assessment of the new-born. Now we
shall talk briefly of nursing management of neonate.
The objectives/principles of care of the new-born include:
1. Establishment and maintenance of air way 2. Maintenance of stable body temperature 3. Protection from infection 4. Provision of adequate nutrition 5. Promotion of infant parent attachment (child-parent bond) Nursing care of neonate can be divided into two periods: immediate care and delayed
care.
Immediate care includes the following:
Vital signs
Temperature, heartbeat and respiration should be observed after every 15 minutes
immediately after birth, for the first hour; then 2 hourly for the next S hours and every 4
hourly until 24 hours of age. Rectal temperature is preferable to axillary temperature.
Observe colour, muscle tone and reflexes
Apgar Scoring chart may be used to evaluate the condition of the new-born for the first
minute and 5 minutes after birth.
Bathing
Should be done after 24 hours after the vital signs are stabilized. Bathing time is an
excellent time for observations of infant behaviour such as irritability, state of arousal,
alertness and muscular activity.
Umbilical cord: The umbilical cord separates through the process of drying and usually
falls off between 7-10 days. The umbilical stump is an excellent medium for bacterial

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
growth. Therefore, it should be kept clean and dry. Instruct parents regarding proper
umbilical care.
Infant nutrition
Although heredity determines the infant's growth but nutrition influences the
attainment of the growth. Hence optimum nutrition during foetal life and infancy should
be the goal for each child. In general, two methods of infant feeding are used: that is,
breast feeding and artificial feeding. Breast milk is the best and most perfect food for
infant nutrition.
Identification and registration of the neonate.
3.1.4 Common Health Problems of Neonate
The neonate can have following problems after birth.
Hyperbilirubinaemia
Hyperbilirubinaemia may occur due to physiological jaundice and Rh or ABO
incompatibility.
Neonatal hypoglycaemia
This condition of low blood glucose (less than 30 mg/100 ml.) Commonly occurring
during the first 48 hours of life, is a hazardous state that must be recognised and dealt
with at once. Early feeding of babies has reduced the incidence of hypoglycaemia.
Hypothermia
The normal baby's temperature may fall to 35.5°C or less within one hour of birth,
unless precautions are taken to avoid chilling, the new born may go into hypothermia
with the temperature falling below 35.5°C.
Sepsis
Within few hours of birth, staphylococci generate colonies on the baby's skin and in the
nasal passages: the umbilicus becomes infected, more readily then nostrils and skinfolds
such as axilla and groin. Any person suffering from respiratory infection or diarrhea, or
one who has any septic focus should not be allowed to come in contact with babies.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Eye infections
The baby's eyes may be infected during his passage through the birth canal, or later by
the mother's hands. A number of cases of neonatal conjunctivitis are due to the B-
Proteus and staphylococci which produces a yellow discharge. Pneumococci and
streptococci are sometimes found but gonococcal infection is the most dreaded
infection.
Oral thrush
Oral thrush is characterised by white patches in the mouth. The causal organism is the
Candid albicans which is present in the vagina of some women.
3.2 The Infant
We have discussed the care of the new-born. Now we shall learn about the physical
growth of the infant, its health promotion and health problems. Here we shall discuss
the preventive and promotive aspect in the care of an infant, the growth and
development aspect will be discussed in detail in course NSS 511 (Paediatric
Nursing).
3.2.1 Growth and Development
The first year of life is characterized by rapid changes in body size, proportion and
function. The infant increases in length dramatically during the first year. By the end of
the first year the infant's increase in length is 50 per cent greater than at birth. The birth
weight trebles. Physiological changes occur in all the systems of the body. Intellectual
growth takes place gradually. The child starts interacting with his environment. Few
teeth appear the child crawls, sits and tries to stand.
3.2.2 Health Promotion
Health promotion during first year includes the following aspects: i) nutrition guidance,
ii) immunisation, iii) safety and security.
i) Nutrition guidance: Infant nutrition and feeding habits or ways are highly
individualised. Breast milk or cow's milk are excellent sources of nutrition for the
infant for the first three months of life. While giving supplementary milk, teach
methods to develop the habit of using cup and spoon and not to use feeding

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
bottle. Supplementation of mineral or vitamins is dependent upon the type of
formula given. After three months, milk does not meet the nutritional
requirement of the infant, so solid foods should be introduced as discussed
below.
a) Introduction of solids: The main purpose of initiating the feeding of solid
foods to the infant is to provide adequate iron; cereal is an excellent
source of iron. The type of iron added to the commercial formula is better
absorbed. Solid foods facilitate adequate chewing and digestion of foods
in later life. Cereal is introduced first because of its high iron content.
Preparing food at home is simple and inexpensive. Spoon should be used
to feed the child. New foods should be introduced to small amounts and
singly at intervals of 4-7 days. The introduction of the infant to solid foods
is called weaning.
b) Weaning: is the process of giving up one method of feeding for another. It
is psychologically significant because the infant is required, to give up a
major source of pleasure and gratification. There is no fixed time or
weaning, but most children show signs of readiness at the age about five
to six months. Over-feeding should be avoided. Obesity in infancy may
predispose to obesity in later life.
ii) Immunisation: Primary schedule of immunization begins during infancy and is
completed during early childhood with the exception of booster doses. The
discussion on childhood immunizations for diphtheria, tetanus, pertussis, polio,
measles, mumps and rubella will be presented in Unit 11.
iii) Safety and Security: Accidents are a major cause of death during infancy.
Common accident hazards are suffocation, falls, burns, poisoning, aspiration of
foreign object, road accidents and drowning etc. You must be aware of possible
causes of injury and plan anticipatory preventive teaching for the parents.
Teething, thumb sucking, sleep etc. are some of the concerns of parents requiring
extension of guidance to them.
3.2.3 Common Health Problems:The infant's immature physiological system
predisposes him/her to several potential health problems during the first year. Some of
the important problems are listed as under.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
i) Nutritional Deficiencies
a) Iron deficiency anaemia
b) Protein calorie deficiencies - Kwashiorkor - Marasmus
c) Vitamin deficiencies like night blindness, scurvy, rickets
ii) Allergy
Is an adverse reaction to a foreign substance or an antigen. During infancy eczema,
nutritional allergies and seborrheic dermatitis can occur.
iii) Colic
Colic is described as paroxysmal abdominal pain or cramping that is manifested by loud
crying. It is more common in the infant under the age of three months. Causative factors
may be too rapid feeding, over-eating and swallowing excessive air. Colic is considered a
mild ailment but can have an intense emotional impact on a colicky infant.
iv) Failure to thrive
Is also referred to as maternal deprivation syndrome. There is lack of physical growth
due to lack of emotional and sensory stimulation from the mother.
v) Sudden infant death
Syndrome is also referred to as crib death between the ages of 2 weeks to 1 year. The
airway gets blocked at the level of vocal cords from laryngospasm. There are many
theories regarding the etiology of sudden infant death. Parents should be explained that
it cannot be predicted or prevented.
vi) Diarrhea
Infant diarrhea is common due to unhygiene feeding habits and drinking unsafe water.
viii) Acute respiratory infection
This is common where the child is unprotected from the natural elements of
environment such as, cold, heat, rain, wind etc. It becomes serious if immediate care is
not given.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.3 The Toddler
The "terrible twos" has been.used to describe the toddler's years from 12 months to 24
months of age. It is a time of intense exploration of the environment. You must
understand the dynamics of behaviour in order to help parents to deal effectively with
the tasks of this age. The growth and development pattems.of toddler are given below.
3.3.1 Growth and Development
The growth and development of the toddler has been explained as under:
i) Development Tasks
The toddler is faced with the mastering of several important tasks. Toddler period builds
on previously acquired needs and acquired completion of tasks. The toddler has the
need for self esteem - the desire to feel important, in control, competent in his/her own
way. The toddler's ability to control his/her environment is greatly enhanced by his/her
increased motor skills and energy. The birth of a new sibling has special significance for
the toddler in his/her quest for autonomy. There is development of ego which may be
thought of as reason or common sense. It is evident that the child is able to tolerate
delayed gratification. There is also rudimentary beginning of super ego. Within the
psychosexual framework the anal zone becomes the center of child's physical,
emotional and psychological activities. Pleasure comes from moving his bowels.
Cleanliness of toileting should not be over-emphasised as this may make the toddler
tense.
ii. Biological development
Biological development and maturation of body systems is less dramatic during early
childhood. Physical growth slows considerably in toddlers as compared to the infant.
iii) Neurological development
By the end of the first year all the brain cells are present but they continue to increase in
size. Visual ability is fairly developed by the end of the first year and undergoes
refinement until the age of 6 years. The senses of hearing, smell, taste and touch
become increasingly well developed.
iv) Musculoskeletal system

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Bone growth continues to be rapid. More than 25 ossification centres appear during the
second year. Growth in height is mainly due to elongation of legs, the feet develops
normal arches.
Dentition
By one year of age most children have between six and eight temporary teeth -- the
upper and lower central and lateral incisors: 'Dental hygiene can be started when the
fast tooth erupts.
The defense mechanism is much more efficient in the toddler than in infant.
v) Adaptive behaviour
Gross and fine motor behaviour: The major gross motor skill during the toddler period is
the acquisition of locomotion. Fine motor development is demonstrated in increasingly
skillful manual dexterity.
vi) Language behaviour
Increasing levels of comprehension develop. By the end of two years the child acquires
300 words. The child uses multi-word sentences.
vii) Intellectual development:
By the beginning of the second year the toddler 'thinks' and 'reasons', things out. There
is deliberate trial and error experiment to produce certain results. The mental abstracts
of time, space and causality begin to have meaning.
3.3.2 Promoting Optimum Development
As a health care provider, you have to teach parents how to ensure the optimum
development of their child according to the following guidelines.
i) Developing a sense of autonomy
Give children opportunity to assert themselves. Appropriate limit setting and discipline
are essential. Discipline is a positive, necessary component of child rearing. A child's
wants and needs may be restricted. Unrestricted freedom is a threat to their security
and safety.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
ii) Temper Tantrum
Children may assert their independence by violently objecting to discipline. It is best to
investigate temper tantrums and other forms of indiscipline which can occur during
such as meal times, bedtime and toilet training. Sibling rivalry is a crisis for even the best
prepared toddler.
iii) Health Promotion during the Toddler Years
Nutritional requirement: Calorie requirement for toddler is 100 Kcl/kg; Protein 2.0
gm/kg; Fluid 125 ml/kg. Vitamins requirement remains the same as in the case of the
infant. The need for minerals, iron, calcium and phosphorous is still high. Health
Hazards. You should also teach the parents about the prevention of common accidents
to the toddler. These can be:
1. Road accidents 2. Drowning 3. Bums 4. Poisoning 5. Aspiration and asphyxia 6. Cuts and abrasions
3.4 The Pre-Schoolage
Pre-schoolers are emerging as creative persons. This is also a time for changes in the
parent-child relationship. Growth and development, psychosocial development and play
is described in the following subsections.
3.4.1 Growth and Development
1. Biological growth
Children in the pre-school years grow relatively slowly, they become taller and thinner.
Weight and height
The pre-schooler gains approximately 1.8 kg per year. Growth and height occur at a
fairly steady pace. Sex related differences in weight and height are insignificant in the
pre-school period.
Body proportions: A pre-schooler looks like an adult because of skeletal maturation.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Dentition
Changes in dentition are few during the pre-school years. Dental carries are most
common during the pre-school period.
Integumentary system
Dry skin continues to be a problem because of the minimal amount of serum
production. The hair continues to become courser, darker and straighter.
Blood value
During pre-school years, fat replaces the red bone marrow of the long bones.
Respiratory system
When respiratory tract infections occur, they are localised in the upper tract. Tonsils and
adenoids remain large and should not be removed.
Immune system
Adult level-immunoglobin A (1gA) are reached during the preschool years.
Nervous system
Cerebral dominance is achieved. Co-ordination and the ability to voluntarily control
movements is increased significantly.
Sensory development
The development of auditory structures is complete by the end of pre-school years. The
other senses of taste, smell and touch continue to develop. In addition, children
experience pleasurable feelings associated with touching their bodies.
ii) Cognitive Development
Mental powers develop rapidly between 3-6 years. At the beginning of pre-school, they
remain in the pre-conceptual phase. They devote a great deal of time to imitation and
symbolic play. During this period children are very rigid in their demands. They have
great difficulty in disentangling an object from its background, a problem that has been
termed field dependency. From the age of 4 years children are in the stage of mental
development which is described as intuitive phase. Children use numerous concepts.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Children's attention span, . level of interest and ability to communicate and interact
with the environment to facilitate rapid acquisition of concepts and knowledge,
increases. Pre-school children become involved in the formation of new concepts. They
tend to define objects according to their use, e.g., a bed to sleep. Perception of time and
space is fairly good in the pre-school child. Reasoning and generalisation in their own
thinking is also developed.
Memory is influenced by the levels of perceiving and conceptualizing, modes of
attending and capacity for extracting meaning from the situation. The memory of pre-
school children can be improved through the intervention of parents, teachers or
nurses. Language development proceeds at a fast pace during the pre-school years. At
the age of two years the child has a vocabulary of about 300 words. At the age of six this
has grown to 8000-14000 words. There is also a steady increase in the number of words
used in a sentence.
3.4.2 Psychosocial Development and Play
Interdependency in all spheres of development is again demonstrated in the pre-school
child. Intelligence and reason play a large part in the development and maturing of the
capacities of the ego. With the increase of mental and physical powers, the ego is
assisted in its function of testing reality through interaction with and exploration of the
environment. A child's ego becomes strengthened through relationships with children
and adults.
The areas of psychosocial development are described below.
i) Identification with parents
Identification refers to the process whereby a pre-school child begins to behave like the
parent of the same sex. Identification is facilitated by dependency on parents and by
conscious awareness of parental expectations related to cultural standards of behaviour
and sex role identity. Identification is also furthered by acquisition of attributes or skills
currently defined masculine and feminine behaviour; children's perceptions that others
regard them as possessing a particular sex role; experiencing the parents as powerful
and significant nurturants who are in command of the desired goal such as power and
love.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
ii) Conscience development: Through identification, the child may come to
resemble not only what the parent is, but also what the parent wishes the child to
become. Parents' standards and ideals become internalized in the child's character, so
that the child is no longer as dependent on the parents for behaviour regulation. With
the development of conscience or superego, older children are able to resist
temptations in the absence of parents. They begin to feel guilt for their misdeeds.
iii) The internalization of moral standards involves three different components.
Behavioural
Emotional
Judgmental The child's conscience becomes modified in later stages of development, though
meeting and adapting to the standards and conversions of his or her group, peers,
teachers and eventually the wider community. Development of Moral Judgment: As
children begin to interact with others and acquire increasing cognitive capacity to define
situations, their reasoning for moral action becomes more mature. During the pre-
school and early school years, children view rules passed down by their parents as fixed
and absolute. As children's experiences increase, their moral judgements progress
toward more internal and subjective values.
iv) Socialization and Social relationships
During the pre-school period, children identify with their own particular culture and
adopt its value, belief and norms. Family structure, educational institutions and child
rearing practices vary among societies. The culture in which children grow up
determines both the content and the methods of socialization of its members.
During pre-school period parents continue to act as the major agents of socialization of
children. In school, children can learn to become more independent and to express
feelings with greater freedom because relationships to other adults are less emotionally
charged than the relationship with parents. In a group, children's potentials for
socialisation can unfold, and the teacher can help them to turn to playmates for release
of affectionate feelings. When children succeed in making friends with other children in
the group, disappointment over family relationships becomes more tolerable. For many
children, a pre-school experience provides the first opportunity to interact with children
from different socioeconomic, cultural, ethnic and religious backgrounds. Optimum
health is also vital to children beginning a new experience. Health problems have a

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
direct bearing on the child's capacity for adjustment and ability to handle this new
experience constructively.
Adjustment to pre-school experience is usually gradual. Children have different method
of coping with the unfamiliar situation. Some children plunge into new situation
aggressively and others are passive at first and need to survey the situation from a
distance before entering into group activity.
v) Development of sex role
As the child begins to behave like the parent of the same sex, he or she begins to
experience some of the emotions as the parent. For example, while cuddling a doll the
girl may feel warmth, happiness, and pride the emotions her mother felt while caring for
her. The boy may experience pride when he learns to throw a ball like his father and
receives praise for his accomplishment.
Gender role of sex typing is important to most parents in the socialization of their
children. From the time of birth they may have given differential treatment to their child
according to sex, so that the child learns, throughout early childhood that particular
behaviours and mannerisms are expected of sex role identity in a particular culture.
Older sibling and peers also influence the child's sex role training, and can act as models.
For instance, boys with older sisters are more likely to exhibit greater feminine
characteristics whereas the reverse is true for girls with brothers.
vi) Development of body image:
When children begin to distinguish themselves as separate persons, they begin to, form
a mental image of themselves and their bodies. They also begin to recognise and
respond to parental pride or disappointment in their appearance and abilities. Vision
plays a part in the developing body image. When first viewing themselves in a mirror,
babies may shriek with distress. Later, however, they are able to recognise the image as
the self and to incorporate the external image into the concept of the body. If parents
register, disapproval of exploration of body parts during care taking activities, a child
may develop long lasting disgust. Natural curiosity about the body may be transformed
into guilt and anxiety.
At this age, children develop an image of their bodies as attractive or unattractive, and
normal or 'different' as a reflection of the opinions of others particularly those of

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
parents. We discussed about psychosocial development now we become to the next
part i.e. play as given below.
Play is the principal business of early childhood. Play provides an outlet for their needs
for self-expression. In dramatic play, children practice before one another the roles they
may play as parents.
Purposes of play
Play develops creativity in children.
Children develop cognitive map of the environment with patterns of time and space.
Play relieves tension, stress and painful experiences.
Through play children learn social interaction. Enhancing play activities
In the home, neighbourhood and in pre-school, adults should be sensitive to children's
needs for play. Play area should be checked for hazards. The play equipment should be
checked frequently to prevent accidents. Children should be dressed appropriately for
play. Parents interference should be kept to a minimum. They should not be left
unattended. Play articles should be selected according to the physical and mental
development of each child. They should be colourful and harmless.
3.5 The School age Child
The period of life from age 6-12 years (school age) has been given a series of labels. This
age is also called the "gang age" as the child gives more importance to peers during this
period. This is also the stage of industry and complexes. Between 6-12 years the child
achieves intellectual development and mastery of concrete operations. Let us discuss
the physical and mental development of the school age child.
3.5.1 Growth and Development
During the school years the child shows progressively slower growth in height and a
rapid growth in weight. General growth is slow until the growth spurt just before
puberty. Muscular co-ordination improves steadily. Posture is good. The lymphatic
tissues reach its maximum growth. During this period there is eruption of permanent
teeth. The temperature, pulse and respiration approach the adult norms.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3.5.2 Mental and Psychosocial Development
In school the child has an opportunity to widen his social contacts as he develops his
mental abilities. Let us first talk of mental development and then we shall discuss
psychosocial aspects of development.
Mental Development
During school age the child gives up, to a large extent, his earlier pre-operational
egocentricity. He is able to function at a higher level in terms of his mental abilities.
Therefore he is able to learn in school. The school age child is able to arrange things or
concrete objects according to their size and relationship to other things. The child is able
to classify objects in a more complex manner. He can solve problems because he can
manipulate symbols. As regards the concept of time, the child not only thinks about the
present but of the past and future. The child's ability to speak and play becomes
socialized and cooperative during school age.
Psychosocial Development
Sense of industry
Between the ages of six and twelve years the child develops a sense of industry and a
desire to engage in tasks in the real world. The child enjoys doing socially useful tasks
for others which will yield a sense of worth. He learns how to cooperate with others.
The kind of school a child attends is important to his developing a sense of industry.
Relation with family, siblings and friends
More time is spent with other children but the family still provides security and a place
to relax. Children of large families find adjusting to peers and sharing with the group
easier than an only child. The school child's jealousy of younger and older siblings
increases as he/she attempts to keep ahead of a younger child and in pace with an older
one. Scholastic ability is a principal cause of sibling jealous among school children,
particularly in a child who is mentally inferior. School children often prefer to be with
their friends rather than their siblings.
Body image
The body image of school children is constantly changing because they are changing
physically, emotionally and socially. Modesty appears at about 9 years of age and at 10

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
years investigation of their own sexual organs begins. The pubescent years bring rapid
changes in body image.
Gang or groups
They form close friendships and ultimately form a group with other children. It may be a
secret society or an antisocial gang. Girls also form their own groups and discuss their
problems. Towards the end of the school period children learn to compete, compromise
and cooperate. Parents should understand and accept the activities of their children.
Children still need the continued love, interest and support of both parents.
Psycho-sexual development
Between 8 and 11 years, children begin to perceive sex roles in a near adult fashion.
Boys and girls (as they approach puberty) should be informed about the reproductive
cycle and their respective role. Both male and female sexual changes should be
discussed by parents.
Spiritual development
During these years children are learning the specifics of their religion that will later
develop into religious philosophy.
Play and work
Today school age children are increasingly interested in the type of play and work
usually associated with those of the opposite sex i.e. the girls may be interested in
participating in team sports traditionally reserved for boys. Boys may be interested in
learning to bake and. cook. Play serves as a learning tool for children and their play
changes with development needs. Children participate in more organised sports.
3.5.3 Health Promotion
The health of the school child is influenced by the health supervision received from the
family physician, nurse practitioner, the dentist, health instructions given by parents,
teachers, school and school nurse, the home and school environment. As a health care
provider you have to play the role of school health nurse as given below.
The Role of School Health Nurse Practitioner

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The role of school health nurse practitioner or school health nurse is changing from
being child centred to being family centred. Health fairs present the concepts (if health
and well-being to school children. Hospital tours. can also be arranged by the school
health nurse to familiarise the children with a hospital and prepare them for possible
hospitalisation. The school health nurse should give health education in the' following
areas.
Areas of Health Education
Nutrition
School children usually eat well and have fewer food fads than pre-school children.
Eating problems relate more to the time of eating. Milk and fruits are preferable to
candy and cookies. As a school health nurse you have to ensure that the diet of the child
should contain all the nutrients in proper adequate proportion and advise the child and
parents on a balanced diet to prevent nutritional deficiency.
Eating habits
Meal time should be pleasant. There should be resting period in the day, but some
parents do not keep it so because of over emphasis on manners. The child’s eating
habits improve as he grows older. A friendly atmosphere and enjoyment of the meal are
the best aids to appetite. Your responsibility as a school health nurse is to ensure and
advise the child and parents regarding healthy eating habits such as washing hands
before and after eating and eating in clean surroundings.
Dental problems
Dental health is of particular importance during this stage of development. Ideally,
children should receive regular preventive dental care and supervision in daily hygiene
from the time the teeth begin to erupt. Inadequate dental care results in dental caries,
malocclusion and trauma. These conditions have harmful long range effects on
children's health. The most effective means of preventing dental problems is to provide
information to the child and parents regarding brushing of teeth and washing of mouth
in both early morning and after taking food.
Sleep and rest: The amount of sleep and rest required during childhood is a highly
individual matter and unique to every child. During school age children usually sleep 11-
12 hours.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Exercise and activity
Exercise is essential for developmental progress in a number of areas such as the
following muscle development and tone, refinement of balance and co-ordination,
gaining strength and endurance, and stimulating body functions and metabolic
processes. Children need ample space to run, jump, skip and climb and safe equipment
to use inside and outside the home or school. Most children need little encouragement
to engage in physical activity. They have so much energy that they seldom know when
to stop.
Sex education
Evidence, indicates that many children experience some form of sex play during or prior
to preadolescence as a response to normal curiosity; not from love or sexual urge.
Children are experimentalists by nature, and this play is incidental and transitory. You,
as a school health nurse, can provide information on human sexuality to both parents
and children.
Prevention of accidents
As in all other age groups, the most common cause of serious accident, injury and death
in school age children is motor vehicle accidents - either as pedestrians or passengers.
Physically active, school age children are highly susceptible to cuts and abrasions,
fractures, strains and sprains. The most effective means of prevention is education of
the child and family regarding hazards of risk taking and improper use of equipment.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
UNIT 3 THE ADOLESCENT
CONTENT
3..1 Physical Growth
3..2 Psychosocial and Emotional Development
3..3 Health Promotions and Anticipatory Guidance
INTRODUCTION
Achieving. independence from the family is an important goal of adolescence. The time
period extends from 10-12 years to 18 years. This period is also called the teenager. The
adolescent period has three stages i.e. Prepubescent or pre-puberty period is refers to
the period of rapid physical growth when secondary sex characteristics appear.
Objectives
After going through this Unit you should be able to:
Describe physiological status of adolescent
Describe the growth and development of adolescent
Explain the growth and development of adolescent
List the common health problems of various stages of development
Advise on their problem prevention
4.0 CONCLUSION
5.0 Summary
6.0 Tutor-Marked Assignment
7.0 References/Further Reading
3.1 Puberty

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
This is the age at which girls begin to menstruate and the boys to produce spermatozoa.
Adolescence begins when the secondary sex characteristics appear and when somatic
growth is completed. The individual now is psychologically mature, capable of becoming
a contributory member of society.Let us discuss the growth and development of
puberty first and then talk of adolescence.
3.1.1 Physical Growth
Puberty is a period of rapid physical change and personality growth. Girls begin their
pre-adolescent growth spurt at about 10 years of age and boys at 12 years of age.
The physical characteristics of puberty are given below.
Weight and height Rate of growth in height tends to decrease each year from birth but with the onset of
puberty there is a rapid increase, or spurt, and the child becomes tall. Gain in weight is
proportionately greater than gain in height during early adolescence.
Body proportion The skeletal system grows faster than its supporting muscles. This tends to cause
clumsiness, poor posture, and lack of co-ordination. The extremities, hands, and feet
grow out of proportion to the rest of the body and cause more co-ordination problems.
Dentition The number of permanent teeth increase.
Physiological development It is believed that due to changes in hypothalamus with resultant neuro-hormonal and
pituitary gland, stimulation development of secondary sex characteristics occurs.
Physical changes in boys include in order of appearance Increase in size of genitalia; swelling of the breast, growth of pubic, axillary, facial and
chest hair; voice changes; and production of spermatozoa. Boys grow rapidly in shoulder
breadth from about the age of 13 years. Boys can become disturbed by nocturnal
emissions and the loss of seminal fluid during sleep. If they have not been told that this
is normal they may regard it as a disease or as a punishment because of masturbation or
thinking too much about sex. They may also believe it is devitalizing. Nocturnal emission
is due to the activities of glands, and occasional release of spermatic fluid during sleep
should cause no concern.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Physical changes in girls in order of appearance Include increase in the transverse diameter of the pelvis; development of the breasts;
change in the vaginal secretions; and growth of pubic and axillary-hair. Menstruation
begins. Average age of menarche (time of first menstruation) is 12.5 to 12.8 years. A
girl's hips begin to broaden from about the age of 12 years. Because of lack of adequate
information, girls may have misconceptions about menstruation. Children should be
well oriented to the anatomic and functional differences between the sexes. Girls
should have clear understanding about ovulation, fertilization, pregnancy and birth.
Menstruation is a normal physiological phenomenon, so women need not curb their
normal activities during it.
Integumentary system The sebaceous glands of the face, back and chest become more active. If the pores are
too small, sebaceous material cannot escape. It collects beneath the skin and produces
pimples or acne; perspiration is increased. Vasomotor activity produces blushing.
Cardiovascular and respiratory system
Heart and lungs grow more slowly than the rest of the body. The supply of oxygen may
be inadequate, causing the pubescent to feel constantly tired. So far we have discussed
the physical characteristics of puberty. Now we shall talk of adolescence.
3.1.2 Physical characteristics of Adolescence
After the pubescent years growth slows and the changes in the body proportion occurs
more gradually. The stages of puberty and adolescence are on a continuum. Stress and
anxiety may occur with these physical, emotional, social and intellectual changes in the
young maturing person. Usually by 15 to 16 years secondary sex characteristics have
developed fully, and adolescents are capable of reproduction. At the end of
adolescence, young persons appear physically like adults. The head is approximately one
eighth of body length.
3.2 Psychosocial and Emotional Development
Children become increasingly more adaptable, approaching their peer group and
problem situations at home and at school, with greater confidence. Parents become
aware that during pubescence the hostility that previously existed between boys and
girls gradually disappears.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The sense of identity and the sense of intimacy:
Adolescence is a period of stress for young people and their parents. Adolescents must
know who they are and must modify their conscious thought of their adult role in life.
Adolescents today are faced with many pressures; rapid rate of social change, the threat
of nuclear war, the increase in speed of travel and technological progress and access to
mind-altering drugs, pose problems. Although sense of identity is difficult to achieve,
young persons must gain it, in order to be saved from emotional turmoil. After
developing a sense of identity during early adolescence, they should be able to develop
a sense of intimacy between themselves with persons of both sexes.
If individuals have weak egos, and are uncertain of self, they will not be able to form
close ties of friendship or love with other people. Close relations between boys and girls
begin during pubescence; these are not intimate relations and serve only as settings for
discussion, on what they think and feel. During late adolescence these relations serve
another purpose. While a healthy adolescent is establishing a sense of intimacy, a
struggle with sexual feelings, may be experienced. As a result peers become very
important.
Achievement of independence from parents
Adolescent-parent separation is part of the natural course of the life cycle. The
adolescent may also adopt the alternative styles of dress, philosophic view points, and
goals of the peer group. The rules of the house set by parents are no longer acceptable
to the adolescence. They begin to internalize the qualities of their parents, if they are
perceived as valuable. These values may be constructive or destructive.
Emotional-Social needs
Adolescence is characterized by mood swings and extremes in behaviour. Friendships
are important to adolescents. Groups of friends are important during early adolescence,
but with maturity older adolescents pick and choose their friends. Peers influence
greatly the adolescent's sense of identity.
Due to rapid body growth, there are changes in body image. To integrate these changing
body image into their self-concepts, adolescents spend a great deal of time in body
hygiene, grooming, and select clothing. Some individuals achieve emotional maturity
during the later stages of adolescence whereas others may achieve it during adulthood.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Psycho-sexual Development: Masturbation: Masturbation is a central concern in early
adolescence, especially in boys. Girls may indulge in it to a lesser degree. Adolescents
should be informed that masturbation is a normal response to increased sexual
development.
Factors influencing decisions about sexual behaviour:
Value and ethics
Value and ethics come from family, religion and peers and society.
Intellectual or Cognitive Development
Formal operational stage (11-15 years): Children progress from concrete to formal
operations during early adolescence. Adolescents can make use of assumptions while
thinking, formulating hypotheses,, and constructing theories. They can use hypothetical
deductive reasoning. They may reject the authority if they are not satisfied with the
rationale and logic.
School
School subjects become more complex. Adolescents experience a period of rapid
increase in vocabulary and language development. Mental growth is not correlated with
increase in size. Adolescents may face some difficulties in adjustment to school. They
may spend more time in extra curricular activities. Adolescents' academic abilities and
interest vary greatly. Besides academic preparation for adult life, high school offers
adolescents an opportunity for extra-curricular activities to satisfy their needs for
security, recognition and success. Parents should continue to take interest in the school
life of the adolescent.
3.3 Health Promotions and Anticipatory Guidance
The adolescent girls and boys should be advised on the following general points.
1. Physical examination
- Personal hygiene
- Nutrition
- Exercise and sports

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
- Dental health
- Accident prevention
- Prevention of addictive behaviour
- Sex education
2. Health concerns of girls
- Menstruation
- Pre-menstrual syndrome
- Dysmenorrhoea
- Amenorrhoea
- Breast size and shape
3. Health concern of boys
- Size of genitalia
- Gynecomastia
- Muscle development
- Acne
- Growth of secondary sex characters.
4.0 CONCLUSION
5.0 SUMMARY
Adolescent years are important for the family and the community. We have seen that
growth and development start right from the time of conception. The health of foetus
depends on maternal environment. The neonate period is most critical. The newborn
has to make physical adjustments to service. During the first year of life growth is very
rapid. In addition to this other developmental changes begin. Toddlers are more difficult
to manage. They need to be prevented from accidents. During pre-school and school
age, the child is exposed to different kind of environment. Infections are common

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
among these children. Physical examination of these children is to be carried out by the
school health nurse. Adolescents are unique. Teachers and parents should understand
their needs and problems.
6.0 TUTOR-MARKED ASSIGNMENT

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
UNIT 4 ANTHROPOMETRIC MEASUREMENT
CONTENT
3.1 Introduction
3.2 Objectives
3,1 Growth monitoring
3.1.2 Height measurement
3.2.1 Nutritional assessment
3.2.2 Mid-upper-arm circumference
3.3 Body Mass Index
3.4 Infant and young children feeding
3.5 Malnutrition management
1.0 Introduction
Growth Monitoring is a simple prevent way to identify the child is growing. It is
used at the time growth is fastest which is first 36 months of life. Growth
monitoring refers to regular assessment of the growth of children through weighing
in the presence of the mother/caregiver from birth to five years to detect deviation
from normal growth and the application of appropriate interventions.
2.0 Objectives
After the completion of this unit you should be able to
i) Describe growth development and monitoring
ii) Discuss nutritional assessment
iii) Determine Body Mass Index
iv) Discuss management of malnutrition
3.0 Main Content
3.1 GROWTH MONITORING
Growth monitoring begins immediately after birth by taking the birth weight. The
birth weights form the base line for growth monitoring. It shows underweight,
overweight and or normal weight gain. This is done on a regular basis using road-
to health chart. It is used until the child is five years (i.e. pre-school age). As a
child grows, he gains weight so long as he remains healthy. Malnutrition and
diseases disrupt this process of growth and can abnormally increase or decrease the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
weight. The kind of scale used depends on the age of the child. For example, for
infants and young children 0-24 months, hanging scales is used in the rural areas
where there is no Salter bowl type scale. For older children, bathroom type scale
can be used.
IMPLIMENTATION OF GROWTH MONITORING
Before a child is weighed, correct and accurate age to the nearest months of birth
(birth month) should be determined from birth records. The growth charts were
designed for mothers and families as means of communication between them and
the health workers. It is a home-based records that need to be brought along with
her to the health facilities whenever she has an appointment.
- Weights of children are taken on regular (monthly) intervals and plotted
against the age (in moths) by joining the monthly Dot(.) made on the growth
chart.
- The month is written in full (i.e. November, October)
- He chart is for use during the first five years of the child‟s life
- The graph has two weights-for-age curves or lines.
- The Upper one represents the 50th centile (for boys) and lower, the 3
rd centile
(for girls).
- The space between the two is called the “ROAD TO HEALTH” which most
healthy children are expected to follow.
- In addition to the two standard curves described, some graphs may have a
third curve, the 97th
centile.
- The shape of the curve of the normal healthy child‟s growth line is similar to
that of the reference lines on the growth chart. The slope of the growth line
is then compared with the normal average growth curve already printed on
the card.
There are three shapes or three reference curve directions for growth
monitoring which must be recognised and their implications understood.
(a) Upward direction : Good. The child is gaining weight and growing well
(normal development). The mother should be commended.
(b) Horizontal or flat line : Warning sign. Child is not gaining weight (static).
Growth has flattered. Something is wrong and requires investigation.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
(c) Downward line: Very dangerous. Weight does not rise above the lower line.
Child is losing weight. Very abnormal and urgent action must be taken. As
and check for infection (treat if present). Breastfeeding and complimentary
foods, personal and environmental hygiene are advised as appropriate.
As a guide, weight between 80-100% of the standard reference is good.
Weights between 60-80% are referred to as underweight and such a child is
said to be at risk of malnutrition. If a child‟s weight is < 60% of normal
standard weight, he is said to be malnourished. He is either suffering from
marasmus or kwashiorkor.
To be able to get the above percentage (%) is used
Actual age of the child x100
Standard Weight
3.1.2 HEIGHT MEASUREMENT
It is used to estimate the rate of growth of the individual and correlate the relation
of height with general health.
The implementation include the following
Inform the mother about the procedure and gain consent
Lay the child on a flat even surface like table
Hold the head and heel firmly
Place two books or any flat non injurious objects one each at the head and
heel level.
Instruct the mother to remove the infant
Place a measuring tape between the two blocks and measure height
Record the height and inform the mother
To measure school children and adults
Inform the client about the procedure and gain consent
Instruct the client to stand against a wall on a flat surface or against the
height rod with his feet together, arms and hands down, head erect and eyes
straight, without footwear, feet parallel and heels, buttocks, shoulders and
back of head touching the wall.
Place the ruler on top of the head level and mark the area with pencil where
the ruler touches the head.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Instruct the client to move away from the area marked.
Measure from ground level to the marked area with a measuring tape or if a
height is used, read the measurement that appears at the point where the
ruler touches the head.
3.2.1 NUTRITIONAL ASSESSMENT
Nutrition is the provision of energy and essential nutrients to maintain optimal
growth and development. An adequate diet contains all kinds of food in the right
proportion. To remain healthy, an individual (child, adolescent and adult) must
have the right amount and kind of food. Inadequate diet may result in under
nutrition, overweight or obesity (mal nutrition) there are four elements of
nutritional assessment. These include the following:
Biochemical data such as Hb, PVC and urinalysis
Clinical data such as information about individual‟s medical history which
include acute and chronic illness, diagnostic procedures or treatment which
can increase or decrease nutrients.
Dietary data taken during a nutritional interview about the meal taking
during previous day previous twenty four hours. Estimating portion or size
of food is difficult.
Anthropometric measurement such as weight, height, write circumference,
skinfold thickness, mid upper arm circumference, chest and head
circumference are carried out for assessing the level of malnutrition in
children while the body mass index (weight and height2) in adolescents and
adults.
3.2.2MEASURING THE MID-UPPER ARM CIRCUMFERENCE (MUAC)
Mid-Upper Arm Circumference is age independent measurement to assess the
nutritional status or to screen malnutrition in children between ages one and five
years. Measuring the mid-upper arm circumference is one of the direct
anthropometric techniques of assessing the nutritional status of children between 1-
5 years of age. It is one of the cheapest, easiest and quickest techniques. The
MUAC changes with about 1cm or less from 1-5 years regardless of the sex of the
child. At birth, it is between 7 and 9 centimetres and increases minimally in

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
diameter between the first and fifth birthdays in healthy normal children. Any child
whose MUAC is below 14.6centimeters within 1-5 years of age is undernourished.
The device for the measurement of MUAC is called SHAKIR strip (named at the
developer) or MUAC tape. MUAC strip can be made from old X-ray films
(previously washed). At its simplest form, the strip has a zero mark and three areas
marked by colours green, yellow and red. “Green” signifies healthy baby, colour
“yellow” indicates caution/warning and that the child is not getting enough and not
growing well. The colour “red” is generally noted for danger.
The three colours of the strip can be effectively used as nutrition educational tool
for mothers. The colour “green” can be used to give information to the mothers on
locally available food stuffs and encourage the mothers to give green leafy
vegetables, yellow colour signifies the need to give food and fruits such as
pawpaw, mangoes, pineapple, banana, yellow yam, oranges, and other yellowish
fruits. Reds colour indicates the need for reddish foods such as palm oil, tomatoes,
as good sources of carotene.
IMPLEMENTATION
Nurses implementation include:
Collect appropriate requirements needed including Shorka‟s strip
Greet and explain to the mother the reasons for using the MUAC strip/tape
Ensure mother is well seated with the child on her laps
Give the MUAC tape/strip to the child to examine or hold before applying it
Push up clothing from the left arm
Allow arm to hang freely
Locate the middle point by measuring the length between the tip of the
should (acromion) and the elbow (olecranon) of the left arm using non-
stretchable fibre tape as the arm hangs freely.
Place the MUAC tape/strip round the middle of the upper arm at the marked
spot (i.e.mid-way).
Put the end of the tape through the small slot in the wide of the tape
Pull the tape/strip firm but not too tight that it pinches or pull the skin
Read and record the colour where the tape/strip intercepts the original
marked line on the strip (in-between the arrows)

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Counsel the mother accordingly to the result of the MUAC Tape (Nutrition
Education).
Green-Normal (commend good efforts)
Yellow-Warning sign (child requires attention)
Red – Danger sign (child needs immediate attention with follow-up instructions
on nutrition, personal and environmental hygiene and immunization.
3.3 BODY MASS INDEX
Body Mass Index (BMI) can be described as a reliable indicator that measures
generalized body fatness for adult adolescents and children. It is calculated by
dividing the weight (kg) by height (m) squared. The average normal BMI for
men and women is 24.99kg/m2. Anything above 25kg/m
2 but less than 30.0 is
regarded as overweight and when it is above 30 but less than 40, regarded as
morbid obesity. The BMI for children and young adults‟ age 2 t0 20 years is
expressed in percentiles. Regardless of gender when the BMI falls below the
5th
, it is referred to as underweight, when it is between the 5th percentile and less
than 85th percentile, it is within healthy weight. When it is within 85
th but less
than the 95th percentile the classification is overweight and when the BMI for
boys and girls 2 to 20 years can be numerically classified.
BOYS 2 T0 20 years Girls 2 to 20 years
<14.8- Underweight <14.4 – Underweight
14.8 – Healthy weight 14.4 – 18.0 Healthy weight
18.4 – 19.2 Overweight 18.0 – 19.0 Overweight
>19.4 – Obese >19.0 – Obese
BMI Formula = Weight in kilogrammes
Height in metres2
The interpretation is as follows:
Less than 20 - Inadequate nutrition
20 – 24 - Normal
25 – 29 - Overweight. Possibly obese

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
30 – 39 - Moderately obese
40 and above - Grossly obese
3.4 INFANT AND YOUNG CHILD FEEDING
Infant and young child feeding (IYCF) encompasses the set of feeding practices
needed to prevent malnutrition. These practices are essential for the nutrition,
growth, development and survival of infants and young children. Breast feeding
should be initiated within 30 minutes of delivery and infants should be exclusively
breastfed for the first six months of life and thereafter breastfeeding should
continue up to two years and beyond while safe complementary foods are
introduced at six months after delivery.
Inappropriate breastfeeding practices are a major factor contributing to infant and
child mortality in Nigeria. Children from 0-6 months who are not breastfed have
five and seven times higher risk of dying from pneumonia and diarrhoea
respectively. In addition, these children are at higher risk of developing non
communicable diseases in adulthood promotion of Exclusive Breast Feeding (EBF)
for six months and continued breastfeeding with adequate complementary foods
until 24 months and beyond constitutes the most effective preventive interventions
reducing child morbidity and mortality.
Skilled behaviour change counselling and support for infant and you child nutrition
should be integrated into all points of contact between mothers and health service
providers during pregnancy and the first two years of life of a child. Community
based support networks are needed to help support appropriate infant and young
child feeding (IYCF) at all levels.
Table 1: Interventions Focusing on Infant and Young Child Feeding. (Pls. correct
the font/or use this
Intervention Description Target
Population
Potential Dietary
Platform Breast feeding promotion
and support, taking into
account policies and
recommendations of HIV
and infant feeding.
Early initiation of
breast feeding within
30 minutes of delivery
EBF for 6 months and
continued
breastfeeding until 2
years of age and 12
months for HIV
exposed infants.
Pregnant mothers
and parents of
infants under 6
months of age
Health Facilities
Community
structures
Campaigns/Outreac
hes. Home Visits
Complementary feeding Behaviour change Pregnant mothers Health Facilities

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
promotion promotion to follow
international best
practices Provision of
CIYCF counselling
provision of nutrient
dense complementary
foods for children
under two.
and parents of
infants and young
children under
two years of age.
Community
structures
Campaigns/Outreac
hes Home Visits
Strengthening of optimal
feeding of a sick child
during and after illness
and exceptional
circumstances
Encouragement of
breastfeeding increase
frequency of eating
during and after illness.
Pregnant mothers
and parents of
infants and young
children under 5
years of age.
Health Facilities
Community
Structures
Campaigns/Outreac
hes. Home Visits
Advocacy for monitoring
and strengthening
enforcement of the
international code of
marketing of breast milk
substitutes
Advocate for increased
monitoring and
enforcement that
supports breast feeding
promotion
Legislators Health Facilities
Community
structures
campaigns/outreach
es. Home Visits
Sources: Nutritional policy- National strategic plan of action for nutrition in
Nigeria (2014-2019)
3.5 MANAGEMENT OF SEVERE ACUTE MALNUTRITION IN
CHILDRENT UNDER FIVE YEARS
Health workers who have contact with infant and young children should be
oriented on the early signs and dangers of under nutrition. They should know how
to identify the underlying causes of under nutrition, be able to recognize poor child
caring practices and advices caregivers on corrective action and be equipped with
screening tools for acute under nutrition and appropriate information for referral
and follow up. Children with acute malnutrition are at higher risk of dying
particularly those with (SAM) Severe Acute Malnutrition and require feeding with
appropriate treatment.
TABLE 2
Intervention Description Target
Population
Potential Dietary Plat
Form
Prevention and
management of
moderate under
nutrition in
children 0-23
months of age
Population with
high prevalence
of children 0-23
months of age
with weight for
age
Health Facilities
Community structures
Campaigns/Outreaches.
Home Visits

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Treatment of
Severe
malnutrition
Identification of
SAM and
subsequent
treatment
Children 6-59
months of age
with weight to
height (with or
without oedema)
or with
MUAC<110cm
Health Facilities
Community structures
Campaigns/Outreaches.
Source: Nutritional policy – National strategic plan of action for nutrition in
Nigeria (2014-2019)
Micro Nutrient Deficiency Control
Vitamin A and mineral deficiencies contribute to morbidity and mortality among
children by impairing immunity, impeding cognitive development and growth
thereby reducing physical capacity and work performance in adulthood.
Micro nutrient deficiencies of public health importance in Nigeria include Vitamin
A, Zinc, Iron, Folic acid and iodine. Multiple strategies are needed to control these
deficiencies.
Table 3: Intervention Focusing on Micronutrient Deficiency Control (PI. Use this
format)
Intervention Description Target Population Potential Delivery
Platform
Vitamin A
Supplementation
Bi-annual doses for
children. Used in
the management of
measles infection
Children 6-59
months
Health Facilities
Community Structures
Campaigns/Outreaches
Zinc
Supplementation
As part of
diarrhoea
management
Children 6-23
months of age
Health Facilities
Community structures
Campaigns/Outreaches
Multiple Micro
nutrient powders
Micronutrient
powders for in-
home fortification
of complementary
foods
Children 6-23
months of age
Health Facilities
Community Structures
Campaigns/Outreaches
Deworming Two rounds of
treatment per year
Children 12
months-59 months
of age
Health Facilities
Community structures
Campaigns/Outreaches.
Nutrition Education
on Bio-fortified
foods
Promote
consumption of
fortified foods.
Parents and
caregivers
Health Facilities
Community structures
Campaigns/Outreaches.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Sources: Nutritional policy-National strategic plan of action for nutrition in
Nigeria (2014-2019).
Diet Related Non Communicable Diseases (DRNCD)
diet related non communicable diseases (DRNCD) such as obesity, diabetes
mellitus and cardiovascular diseases are increasing in public health importance in
Nigeria. Researchers have empirically identified the link between non-
communicable diseases and globalization, urbanization, demographics, lifestyle
transition socio-cultural factors, poverty, poor maternal, foetal and infant nutrition.
Table 4: Intervention focusing on DRNCD (PI. Use this format)
Intervention Description Target Population Potential Delivery
Platform
Awareness of
DRNCD
Identify risk factors
providing
education and
increasing service
for DRNCD
General population Health Facilities
Community structures
Campaigns/Outreaches.
Sources: Nutritional policy – National strategic plan of action for nutrition in
Nigeria (2014-2019)
4.0 Conclusion 5.0 Reference

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Unit 5 FAMILY PLANNING 1.0 Introduction The current population of Nigeria is 200,000,000 with annual increase of population of 3.5%. This is about the highest rate of increase in the world. This unit enables you to understand the needs of family planning, the methods and the roles of the public-community health nursing in the implementation of family planning. 2.0 Objectives
This unit will enable you (1) Outline the importance of family planning (2) State different types of planning methods (3) Discuss the mode of action of the method (4) Discuss the roles of public-community health nurses in family planning implementation.
3.0 MAIN CONTENT 3.1 Family Planning refers to practices that help individuals or couples to attain the following objectives including to: i). Avoid unwanted birth ii). Bring about wanted birth iii). Regulate intervals of pregnancy Iv). Control the time of birth in relation to age of the parents v). Determine the number of children in the family Family planning is basic human right. The scope involved sterility, sex education, screening for pathological conditions related to reproductive system and marriage counseling. The eligibility couples are defined as currently married wherein the wife is in reproductive age of 15-45years who need family planning servicecs. 3.2 CONTRACEPTIONS These are methods designed to prevent conception. There is no ideal contraception suitable for all couples. Each has advantages and disadvantages that must be put into consideration when making recommendation. It is the duty of the Public-community health nurse to provide the information to the couples to make informed choice on utilization of family planning. The conventional contraception include the following
1. Spacing method

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Barrier method- This include physical, chemical and combined methods
Intra-uterine devices
Hormonal contraceptions
Post-conraceptional method 2. Terminal Method
Vasectomy (male sterilization)
Tubectomy (female sterilization) PHYSICAL METHOD:
1) Condom: This is the most common and widely used by men all over the world. It also protects individuals from sexually transmitted diseases. It is for a single use and is worn on the erected penis before coitus. When it is correctly used is effective. Currently there is female condom that is also effective.
2) DIAPHRAGM: It is made of synthetic rubber and is used by wemen. It is cup-like with a rim that is strengthened by a spring. It is inserted into the vaginal canal before coitus and it is left in place six hours after intercourse.
3) CHEMICAL METHODS: The chemical methods include foam tablets, foam aerosol, creams and Jellies and pastes. These products contain spermicides.
4) NTRAUTERINE DEVICE (IUD) It is the introduction of a specially designed device into the uterine cavity of a fertile woman who desires to prevent conception/ pregnancy for specific period of time. This is classified into
First generation IUCD: They are made up of inert materials from polyethylene. Lippes loop is S-shaped with a thread attached at the end that help to identify it and aids the removal.
The second generation is made of metallic copper. It is a T-shape.
The third generation IUCD are with progestogen which is released slowly into the uterus

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
The mode of action of IUCD is to cause biochemical changes in the uterus that alter the mucus secretion and impair the survival of the sperm in the vagina.
Purpose: 1. To ovoid unwonted pregnancy 2. To space pregnancy
Requirements: Trolley Procedure
Top Shelf
A Sterile Pock Containing the following:
1. 2 gallipots for iodine and swabs
2. 1 Artery forceps curved 81/2 long
3 Uterine forcepts
4. 1 single or multiple toothed vulselum (Tenaculurn)
5. 1 pair dressing forceps
6 1 Pair of sponge forceps
7 1 I.U.D removal forceps (Alligator fang type 8’-I
8 1 Curette for biopsy
9. Sterile Scissors size 8’
1 0. Uterine sound
11 . Vaginal speculum (CUSCOs) medium and large
12 .Sterile water.
Bottom Shelf
1. A jar with cheatle forceps
2. Disinfectant
3. Mask
4. Receiver for soiled swabs

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
5. Angle poise lamp
Procedure
1. Explain procedure to the client to allay anxiety
2. Assemble requirements on the trolley
3. Put the client in lithotomy position in the insertion room and
screen the client
4. Put-on mask
5. Swab vulva
6. Perform bimanual examination (vaginal examination)
7. Apply vaginal speculum, leave it in situ and inspect the cervix
excluding any
abnormality
8. Stabilize the cervix with tenaculum clamping at 10cm or 2pm
direction to prevent
haemorrhage
9. Use uterine sound gently to determine the depth of the uterus.
1 0. The bloody discharges leaves a mark of the depth on the uterine
sound, but if done after
the menstrual flow, apply a small quantity of contraceptive cream
or jelly on its tip
before inserting. (Correct sounding, should not be painful).
11 . After sounding, withdraw gently and note the depth of the uterus.
a. For uterine depth less than 4.5cm or type of IUD. 4.5-6.5cm (copper
T, or small’ T-coil
6.5- 9.9cm) most IUD are acceptable type).
b. For uterine depth 10cm or more, use large with a backup.
12, Load the device appropriately into its tube following the makers

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
guideline
13. Place the loaded tube alongside the uterine s and adjust the tube to
the appropriate
depth of the uterus using the adjuster for Copper T.
14. Lippies loop, may not need an adjuster because its firmly
attached to the body of the barrel (Not in use in Nigeria).
I5. Select the correct size of the lippes loop or saf T.coil that
corresponds with the parity and
depth of the uterus and load (Do not load and keep for a long
otherwise the device will
lose its memory). Copper T need no selection.
16. HoIdIng the tenaculum, apply a gentle outward pressure to
strengthen the cervix
17. lnsert, using proper technique of pushing in for lippies loop or
withdrawal for copper T.
That is, for lippies loop push in to release the device.
18. For Copper T, hold the piston stationary, and retract the barrel (vice
versa)
1 9. After inserting the device, withdraw the tube and piston
20. Unclamp the cervix
21 . Trim the string and swab the cervix
22. Remove the vaginal speculum and push the string i the anterior or
posterior fornix of the
vagina.
23. Move the client backward and disengage the legs from the stirrups
24. Clean her buttocks and make her comfortable
25. Remove all equipment for washing and sterilization

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
26. Record the findings and the device into the client chart
27. instruct the client accordingly on how to check for the string
28. For checking the string, she is advised to wash her hands clean, in
squatting position r
lying down position, she should carry out a self vaginal examination
usually before and
after menses
29. No intercourse for 2days after the insertion.
30. Analgesic can be given for pain and the need for personal hygiene
stressed
31. For follow-up next appointment is 6 weeks. 2 appointment in 3
months, 3rd
appointment in 6 months.
32. Client should report early if she has pelvic pain, persistent painful
intercourse, vaginal
discharge, unusual vaginal bleeding or fever.
33. Appointment card with necessary information should be given to the
client.
NOTE: Methods for disinfecting instruments and IUDs:
1. Instruments are boiled for 5 minutes, if not soaked in disinfectant.
2. Do not use salvon (cetrimide) for sterilization as it is a weak
disinfectant.
3.3 INSERTION AND REMOVAL OF JADELLE
(LEVONORGESTREL IMPLANT)
It is a long-acting reversible contraceptive implant design to prevent
pregnancy. It is a two-rod implant developed in the 1 980s by the

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Population Council for five years of continuous use (population council
2010) Jadelle acts by preventing the release of the ovum and also
thickening the cervical mucus thereby blocking the sperm.
Purpose
1. To avoid unplanned pregnancy
2. To enhance child spacing (pregnancy)
Requirement
1. Examination table or couch
2. Sterile surgical drapes
3. Sterile gloves
4. Antiseptic lotion (povidone iodine or spirit)
5. Sterile maker (optional)
6. Local anaesthetic agent(1% lignocaine) epinephrine free
7. Needles & syringes,
8. Sterile gauze
9. Adhesive bandage (plaster)
10. Pressure bandage (crepe)
11 . An applicator with the following parts:
i. Needle shield/needle
ii. Applicator seal
iii Cannulo
iv. Obturator support
v. Obturator
12. Sharp proof container (Injection Safety Box)
1 3. Leak-proof container or plastic bag
14. Pregnancy test strip

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Procedure
Pre — Insertion Task
1. Explain procedure to client
2. Encourage client to ask questions
3. Provide privacy
4. Check to ensure that her arm is thoroughly washed if not, swab the
area of insertion with spirit or iodine swab
5. Wash hands, dry and don gloves
6. Place the sterile drape under the arm to be inserted with the
Jadelle rod
7. Mark area of insertion 6 — 8cm above the elbow fold in a ―V‖
pattern
8. Clean area with high level disinfectant e.g. povidone iodine
9. Change hand gloves and replace with another sterile gloves
1 0. Instruct assistant to hold the lignocaine vial
11 . Draw up 2mls of 1% Lignocaine without epinephrine (local
Anaesthetic)
1 2. lnject under skin (subdermal) and raise small wheal
13. Advance needle about 4cm and injects 1mL of local anaesthetic in
each of two sub-dermal tracks
14. Wait for 2minutes before checking for Anaesthetic effect
1 5. Start skin incision if anaesthetic effect is present
Insertion Task
1. Using the new sharper disposable trocar, insert directly sub-dermally
2. While tenting the skin, advances trocar and plunger to mark (1)
nearest hub of trocar

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
3. Remove plunger and load first rod into trocar with forceps (preferably)
or with gloved fingers
4. Reinserts plunger and advance it until resistance is felt
5. Hold plunger firmly in place with one hand and slide trocar out of
incision until it reaches plunger handle
6. Withdraw trocar and plunger together until mark (2) nearest trocar tip
(do not remove trocar from skin)
7. Move tip to trocar away from end to the rod and hold rod out of the
path of trocar
8. Redirect trocar about 150 and advance trocar and plunger to mark (1)
9. Insert second rod using same technique
10. Palpate rod to ensure that two rods have been inserted in a V-shaped
distribution
11. Palpate to check that all rods are at least 5mm clear of insertion (if
rod is protruding through point of insertion remove and reinsert)
12. Remove trocar only after insertion of the last rod
Post Insertion task
1. Remove drape and wipe client skin with antiseptic
2. Apply pressure dressing with bandage
3. Dispose implant trocar, needle, sypringe in a sharp box before you
remove gloves
4. Dispose waste materials (gauze, cotton wool etc). into a leak proof
container or plastic bag.
5. Immerse both glove hands. 0.5% chlorine solution
6. Remove by turning inside out and place in leak proof container or
plastic bag.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
7. Wash hands thoroughly and dry
8. Complete client records (jadelle) card including drawing position of
rods
REMOVAL OF JADELLE IMPLANT
Jadelle implant is a Long Acting Reversal Contraceptive method of
family planning inserted to last for duration of five (5) years. The implant
may be removed at an time of the menstrual cycle for personal or medical
reasons.
Requirement for Removal of Jadelle implant
1. Local anaesthetic
2. Needle and syringes
3. Puncture prove container
4. Scalpel
5. Two different types of forceps (mosquito and Crile
6. Gauze
7. Antiseptic lotions
8. Gallipot
9. Kidney dishes
10. Adhesive
11. Cotton wool
Procedure
1. Explain procedures to patients
2. Obtain consent
3. Provide privacy
4. Provide lamination

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
5. Palpate to locate implant
6. Clean skin using forceps and sterile cotton wool soak into antiseptic
control end
7. Wait for effect of aneasthetic
8. Make an incision of about 2 – 4mm with the scalpel below the end or
bottom of the V
9. Crippen the end of the implant at the point when visible incision with
the mosquito artery forceps
10. Remove the implant very gently (this take time more than inserting
the implant may be nicked, cut or broken off during removal).
11. If removal prove difficult, the patient can be ask to return for a second
visit after the incision have healed
12. Repeat same procedure for the 2nd rod
13. If patient wishes to continue with a new set of implant may be
inserted using the same incision or use of opposite direction or hand
14. Tidy the equipment
3.5 INSERTION AND REMOVAL OF IMPLANON
It is a single thin, flexible and long-acting reversible contraceptive implant. It
is about the size of a match stick and approved for 3 years of continuous
use. It acts by preventing ovulation and thickening of cervical mucus to
block the sperm.
Requirements
1. Examination couch
2. Sterile surgical drapes
3. Sterile gloves
4. Antiseptic solution

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
5. Sterile marker (optional)
6. Local anaesthetic (1% Lignocaine eprephine free)
7. Sterile gauze
8. Adhesive bandage
9. Applicator with the following parts:
(a) Needle shield
(b) Applicator seal
(c) Needle
(d) Cannula
(e) Obturator support
(f) Obturator
(g) Pregnancy test strip
Prior to Insertion
Prior to insertion, carefully read the instruction for insertion and removal as
well as the full prescribing information.
NOTE:
1. Proper implanon insertion facilitaes removal
2. Correct timing of insertion is important
3. Take history and perform physical examination including a
gynaecological examination before implanon insertion
4. Ensure that the patient understands the risks and benefits of
implanon before insertion
5. Provide the patients with a copy of the patient labeling included in
package
6. Have the patient review and complete a consent form
7. Exclude pregnancy before insertion

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Checklist for the implanon Insertion. Getting Reading
1. Check to be sure client has thoroughly washed and rinsed her entire
non-domination arm
2. Tell client what is going t be done and encourage her to ask
questions
3. Position woman’s arm and place clean, dry cloth under her arm
4. Mark position on arm for insertion of rod 6cm to 8cm above the target
insertion point
5. Determine that required sterile or high level disinfected instrument
implanon trocar with one rod is present.
Pre- Insertion Tasks
1. Wash hands thoroughly and dry with clean personalized towel or air
dry
2. Put on sterile gloves on both hands (if powered, remove powder from
gloves fingers)
3. Prepare insertion site in a radial manner with antiseptic solution
4. Place sterile or high level disinfectant drape with a central hole over
arm (optional)
Insertion Tasks
1. Draws 2cc of local anaesthetic (1% lignocaine without epinephrine
and/or adrenaline) and inject just under skin to raise a small wheal
2. Advance needle towards the second marked point (4cm) and inject
about 1ml of local anaesthetic in one sub-dermal track
3. Place used needles and sharps in container
4. Wait for 2 minutes and then check for anaesthetic effect before
marking and then check for anasethetic

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
5. Remove the sterile disposable applicator carrying implanon from
buster pack
6. While keeping the shield on the needle, visually verify the presence of
the implants is not seen. Tap the top of the needle shield against a
firm surface to bring the implant into the needle
7. Following the visual conformation of the presence of the implant, the
implant is lowered back into the needle
8. Remove the plastic needle shield
9. Stretch the skin around the insertion site with thumb and index finger
10. Insert the tip of the needle at about 200 angle
11. Release the skin
12. Lower the applicator to a horizontal position
13. Lift the skin with the tip of the needle, keeping the needle in the sub-
dermal connective tissue
14. While lifting the skin, gently inserts the entire needle in the direction
of the 2nd marked point keep the applicator paralle to the skin
15. Break the seal of the applicator
16. Turn the rounded end of the obturator a quarter turn, about 900
17. Hold the abturator against the client arm with one hand and with the
other hand, slowly draw the needle out of the arm, never pushing
against the obturator
18. Check the needle to make sure the implant is absent,, after retraction
of the cannula, the grooved tip of the obturator should be visible
19. Verify the presence of the implant by palpating the skin. Check to
make sure that the lower end of the implant is at least 5cm from the
insertion point

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
20. Check the insertion site of bleeding (if bleeding put pressure with
gauze)
21. Apply a sterile gauze to insertion point and hold in place with surgical
tape
22. Wrap the arm with pressure bandage
Post Insertion Tasks
1. Before removing gloves, disposed of the applicator, needles, syringe
in a sharp box and any used instrument (Gallipot, bowl, kidney dish
etc) in 0.5% chlorine solution for 10minutes
2. Dispose other waste materials e.g cotton wool, gauze, etc. by placing
in a leak proof containers or plastic bag.
3. Immerse both gloved hands in 0.5% chlorine solution, Remove
gloves, by turning inside, out and place in a leak- proof container of
plastic bag
4. Wash hands thoroughly and dry
5. Fill out the implanon user and give it to the client
6. Complete client record including noting in which arm the implanon
was inserted.
REMOVAL OF IMPLANON
1. Receiver with swabs
2. A cured mosquito artery forceps
3. Surgical blade
4. Lignocaine
5. Syringe and needle
6. Antiseptic lotion e.g Savlon

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
7. Sterile dressing
8. Adhesive
9. Sterile gloves
Procedure
1. Welcome client and make her comfortable
2. Explain the procedure to the client
3. Help her to adopt a comfortable position
4. Put on sterile gloces after washing and drying hands
5. Clean the point of insertion with antiseptic lotion using sterile swabs
6. Using your sterile hands, gentle push the implanon towards the
incision until the tip is visible
7. Then grasp the implant with forceps (curve mosquito artery forceps)
and pull it out gently
8. If it encapsulated, make an incision using a sterile with 1mI lignocaine
into the tissues sheath
9. Then remove the implanon with the forceps
10. Apply pressure on the incision site with sterile swabs
11. Dress the wound with sterile dressings and apply plaster
12. Make the patient comfortable
13. Advice on care of the wound
14. Return your use equipment and dispose the waste as
directed above.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
UNIT 6 FAMILY HEALTH RECORDS
CONTENT
1.0 Introduction
2.0 Objectives
3.0 Main Content
3.1 Family Records and Purposes
3.1.1 Purposes
3.1.2 Criteria for Recording in Family Health Records
3.1.3 Types of Family Health Records
3.2 Filing and Storage of Records
4.0 CONCLUSION
5.0 Summary
6.0 Tutor-Marked Assignment
7.0 References/Further Reading
1.0 INTRODUCTION
In Unit 4 you have learnt about the Family Nursing Intervention which focuses on
assessing the health needs, planning, implementing and evaluating the care. So once
you have done this, you would like to record the case. How do you do it? This is
explained in Unit 5. In this Unit, you will learn about health records; types of health
records which are maintained for family health; what type of information is recorded
and criteria for recording. This would also help you in filing and storing health records.
2.0 OBJECTIVES
In this unit you will learn about family health records and evaluation of family health
service. After going through this unit, you will be able to:

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
explain what family health record means
list the purposes of maintaining family health records
write up in family health records keeping in mind the criteria for recording identify different family health records maintained in the agency you are working
evaluate the importance of information included in family records for further health care planning
arrange family records as per filing and storage system of records in the agency you are working
decide on the type of records which you wish to maintain for the family under your care.
3.0 MAIN CONTENT
3.1 Family Records and Purposes
Maintenance of family health records is one aspect of the total records system of a
health agency. In most of the agencies the record system comprises a mixture of
prescribed and standard forms often identical to those of other agencies, which can be
designed or modified to meet the needs of particular agency. Use of common forms for
records facilitates inter-agency and inter-unit comparisons and makes reporting of
service data easier. Even if these forms are supplemented or modified still they retain
enough similarity to provide a base for comparison.
Maintenance of family health records and evaluation of the family health service are
complementary to each other. Records are necessary for continuation of delivery of
family health care services and its evaluation. And evaluation of family health services is
necessary to identify now and continuing family health needs.
Family records include information based on factual events, observation results or
measurements taken, like height, weight, body circumference or investigations carried
out like hemoglobin, urine test, stool test and sputum examination depending upon the
problem of the family. These also have records of immunization, nutritional status,
medical prescriptions and curative procedures carried out. Demographic data and
individual personal history is also included in the family folders. We shall now discuss
about purposes of records, criteria for recording in family health records and types of
family health records in the following subsections. Let us begin with purposes.
3.1.1 Purposes
Purposes of family health records are:

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
1. to serve as guides to nursing care, 2. to provide the practitioner or community health nurse with data that is required
for improvement of family health care, 3. to provide the staff, administrator or governing body with documentation of
services that have been rendered, and 4. to provide data that are essential for programme planning and evaluation. The purposes of documenting family health history, which is an important component of
family health records, are:
1. to provide facts that are necessary for evaluating health situation of the family; it should also describe the nature and impact on health threat. It should describe the health condition and interacting forces within the family in their daily living,
2. to afford an opportunity for mutual exploration of the health situation by the nurse and by the family so that they can explain to each other their concerns, expectations and probable actions,
3. to provide baseline and periodic data from which to estimate the long-term changes, services provided and response of the family to these changes and services.
Family health records should represent a comprehensive, systematically organised data
and information that are essential for nursing care decisions. The community health
nurse must assure adequate records support for her actions. It is the grassroot level
workers who write most of the family history and progress record. You as a community
health nurse and other grassroot level workers have much to gain if these records are
comprehensive, available and relevant to service needs.
Though each agency has its own system of recording, the community health nurse can
find her own ways of adapting family history and progress record to her own practice,
style and informational needs. Her records may be a valuable resource when agency
records are being revised or the system is being reorganised.
The community health nurse may need to build into the records, methods for
incorporating information necessary for case planning and assessing health service
utilization.
3.1.2 Criteria for Recording in Family Health Records
The criteria should reflect both the purpose and process of community health nursing
practice.

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
1. Record should concentrate on the family and community as focus of care. It should reflect not only the health of the members of the family but also the ways in which the functioning of the family as a unit has an impact on the health of the family as a whole. It should also specify the ways in which family functions within its physical and social environment.
2. Family health cords should serve as guides for comprehensive care. These should include health threats and health behaviours that have significance for family health. For example, an adequately immunized family may have a health threat from emotionally immature and impulsive parents.
3. An apparently healthy family may have poor nutritional habits and poor house keeping practice inviting accidents. It is important that records show the problem as it develops so that the change can be identified.
4. The record should indicate the expected outcomes and also the degree to which outcomes are achieved. This means that the goals of care to a family are also defined in the records.
5. The family health record should have specific actions planned for the family actions actually taken and distribution of responsibility to family and other community resources so that necessary activities are carried out. Action taken should be recorded in such a way that it can be easily located and future planning can be done.
6. The family record should indicate family response to nursing action. 7. Since initial planning and implementation can redefine a problem the record
must show revision in the status of the problem so that further planning can be done accordingly.
8. Record systems should possess sufficient uniformity to make recording, tabulation. and collection easy and to permit inter-unit in-service comparisons and easy reference.
9. Maintenance of records should require minimal amount of time. Unimportant and irrelevant data reading may also require more time and lengthy records may result in errors.
10. Family records should be quickly available to the user. Accessibility is not always easy to achieve. Compiled individual and family records can be made available at a central location for easy reference, only for professional use.
11. Family records require reasonable storage space. As number of individuals are added, the records also increase and require more storage space and facilities.
12. Depending upon the number of years records should be retained, according to agency policies and storage space will be required.
13. Family record system should provide confidentiality of record content. For example, sometimes a mother in the family may not like information about family planning methods she has adopted to be shared with other members of

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
the family or her neighbourhood women. There should be provision for such confidential information and sometimes official records in the agency do not have provisions for such recording. The community health nurse must find her own ways to incorporate such summarization into her recording so that priority needs can be attended to first.
3.1.3 Types of Family Health Records
Different family health records which are commonly used are grouped in different ways.
These may be grouped according to:
Age of family member for whom records are used such as:
1. Newborn care 2. Road to health card 3. Toddler card 4. Adult card 5. Old age or elderly card 6. Mother-child link card Health care requirement cards as per health conditions and morbidity status
Pregnant women or antenatal card
Intranatal care card or labour record
Person with illness: for example - Tuberculosis record
- Diabetic record
- Hypertension care card
- Malaria record.
Drug addicts or alcoholics record
Any chronic care record
Immunization record. Records used in the
Clinic
Home

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
Head Office. These records are in the form of
Cards
Folders
File
Charts, etc. Usually for family health services a family folder including different cards is maintained.
This includes socio-demographic information, children health status (including height,
weight, immunization and feeding habits, etc.) maternal records, morbidity records and
observations -of general health status of family and the environment of the family.
These records have individual formats and styles of recording which is prescribed for
each agency. The method of recording is usually a standard one and general instructions
are provided. Examples of records for infant, toddler, antenatal women, immunization
and family planning are shown in Appendices 1 to.3 (which is given at the end of this
block) and, similar kind of record you may find in the agency where you are working.
3.2 Filing and Storage of Records
We have discussed about the purposes, criteria and types of records. Let us discuss how
these records are filed, as given below.
To have quick access to records for efficient use of records, a proper filing system must
be adopted. In a primary health care set up in community health nursing this aspect
needs special attention. Filing will depend upon the type of records. If it is a family
folder, it is filed as per geographical location or as per house number in the area. These
family folders may be filed as per the name of the head of family. If community
members and the health worker is familiar with house numbers, it is as per house
number in the area. In a rural community where a family is known by the name of the
head of the family, the folder is filed as per the name and arranged alphabetically. Since
these records are preserved for a long period of time and needs frequent handling, they
should be kept in the pro; filing space or in a shelf with labels so that a file can be easily
traced when a family member is visiting the health centre or a family visit is to be
planned.
At a health centre, when cards are maintained as per age groups or type of morbidity
conditions, these may be filed under these headings.The record system requires
reasonable space for storage. The proliferation of records as! well as increase in number

NSC501 PUBLIC-COMMUNITY HEALTH NURSING II
of people under care, may create a serious problem or r storage. The period for which
records are maintained is usually the agency's policy; often the period of retention is as
low as five years. A short retention period does save space but it also presents
problems, since community health needs and methods are changing and the period over
which care is provided to the family is likely to be more prolonged.
4.0 CONCLUSION
In order to assemble in one place the comprehensive family information needed by a
community nurse providing general family care, it is necessary to have a record system
that permits quick and easy transfer of information among the care providing team
members. The individual practitioner on the community health team must be able to
assure adequate record support for her own actions. It is mostly the grassroot level
practitioner who writes most of the family history and progress record. It is she who has
most to gain if records are comprehensive, available and relevant to service needs.
Using of family history and progress records is as important as developing and
maintaining them. It is important to find and read the record as a basis for planning and
taking nursing action for the family. Thus the nurse who uses records can value and
monitor her own recording programme.
6.0 TUTOR-MARKED ASSIGNMENT
7.0 REFERENCES/FURTHER READING







![Het gynaecologisch onderzoek 3BACH.ppt [Compatibiliteitsmodus] · 14/02/2011 2 Onderzoekshouding Stuit tot op de rand Genitalia externa 1. Clitoris 2. Labia majora 3. Labia minora](https://static.fdocuments.net/doc/165x107/5cd3d37488c993de288b48e0/het-gynaecologisch-onderzoek-3bachppt-compatibiliteitsmodus-14022011-2.jpg)