Evaluation of the effect of protamine on human prostate carcinoma PC-3m using contrast-enhanced...
Transcript of Evaluation of the effect of protamine on human prostate carcinoma PC-3m using contrast-enhanced...

32454
Assessment of local pulse wave velocity in arteries using 2Ddistension waveformsMeinders JM, Hoeks AP, Biophysics, University Maastricht,Maastricht, Netherlands
Objective: According to Bramwell-Hill, arterial stiffness can be as-sessed non-invasively by measurement of the pulse wave velocity(PWV). PWV can be estimated from the foot-to-foot delay betweenpressure or blood velocity waveforms recorded transcutaneously in,e.g., the common carotid artery (CCA) and the common femoral artery(CFA). However, interpretation of results is complicated since theCCA-CFA trajectory is composed of arterial segments with oppositeand different pulse wave velocities. Furthermore, arterial sites sensitiveto early development of atherosclerosis are obscured by the relativelylarge CCA-CFA trajectory. It is the objective of this study to developa method assessing local PWV over a short (16 mm) arterial segment,thus allowing regional PWV assessment and possible detection of earlydevelopment of atherosclerosis at specific sites, e.g., the commoncarotid artery.Methods: To assess local PWV, multiple adjacent distension wave-forms are determined simultaneously along a short arterial segment(16 mm), using a 2D-vessel wall tracking system with a high framerate (651 Hz). To this end, the B-mode image scan frequency of anultrasound scanner is enhanced, allowing temporal cross-correlation ofradio frequency (RF) signals, resulting in high accuracy determinationof 16 diameter waveforms, simultaneously. The PWV is obtained bydetermining: 1) the average delay between the 16 diameter waveforms,and 2) the ratio of the temporal and spatial gradient of adjacentdiameter velocity waveforms. Both methods are verified in a phantomand in the common carotid artery (CCA) of 23 humans.Results: Phantom experiments show a high concordance betweenPWV obtained from 2D distension velocity waveforms (4.21 � 0.02m/s) and PWV determined using two pressure catheters (4.26 � 0.02m/s). Assuming linear spatial gradients, the PWV can also be obtainedin vivo for CCA and averages to 5.5 � 1.5 m/s (inter-subject variation).Conclusions: Phantom experiments show a very low variation coeffi-cient (0.5%), whereas in vivo results compare well to values found inliterature. Furthermore, intra-subject PWV compares well with thosecalculated using the Bramwell-Hill equation.
23979
Three dimensional in-vitro thermal lesion monitoring usingvibration sonoelastographyTaylor LS,*2 Wang P,2 Rubens DJ,2,3 Parker KJ,1,2,3 1. Electricaland Computer Engineering, University of Rochester, Rochester, NY,2. Biomedical Engineering, University of Rochester, Rochester, NY,and 3. Department of Radiology, University of Rochester, Rochester,NY
Objective: HIFU and radio frequency (RF) ablation are methods fortreatment of cancerous lesions, which create a coagulation necrosiskilling the undesirable cells. A technique for real-time monitoring ofthermal lesions would be a useful adjunct to these therapies. Sonoelas-tography is being investigated as a real-time monitoring method.Methods: Fresh bovine liver was soaked in saline for 24 to 36 hours,and RF ablation was used to induce a coagulation necrosis in the liver.Three-dimensional (3D) sonoelastography images were acquired. Afterimaging, lesions were dissected to document their size, shape, andvolume.Results: Upon dissection, the induced lesions were all found to bepalpably hard, ellipsoidal in shape, and of differing texture and colorthan the untreated tissue. The mean volume of the 5 lesions determinedby fluid displacement was 4.6 cc. In the sonoelastography images, each
lesion appeared as a dark (low-vibration) region surrounded by a fieldof bright green (higher-vibration). The precise edge of each sonoelas-tography lesion was somewhat ambiguous. The sonoelastography vol-ume for the 5 lesions was found to be 90% of the volume determinedby fluid displacement when only the area of lowest vibration amplitudewas taken to represent the lesion.Conclusions: Real-time monitoring of thermal lesions can be accom-plished in-vitro by making the sonoelastography lesion 10% larger thanthe desired treatment zone.
32402
Three-dimensional fusion of prostate histology withsonoelastography imagesTaylor LS,*2 Porter BC,1 Nadasdy G,4 di’Santagnese PA,4
Pasternack D,4 Messing E,5 Rubens DJ,2,3 Parker KJ,1,2,3 1.Electrical and Computer Engineering, University of Rochester,Rochester, NY, 2. Biomedical Engineering, University of Rochester,Rochester , NY, 3. Department of Radiology, University ofRochester, Rochester , NY, 4. Department of Pathology, Universityof Rochester, Rochester, NY, and 5. Department of Urology,University of Rochester, Rochester, NY
Objective: When using histology to validate the accuracy of a new orexisting imaging modality, a method is needed to assure that thepathology slice being viewed is the same as the scan plane. A wholemount pathology/histology protocol for 3D tissue reconstruction hasbeen developed to compare the geometry, size, and spatial location oftumors (or other lesions) identified in histology data with that from 3Dimages.Methods: Excised cancerous prostate specimens are embedded in anagar gel and imaged in 3D using B-mode and sonoelastography (vi-bration Doppler). The prostate is outlined in each 2D slice of the cinesequence, and 3D surface reconstruction is made. The specimen is thenprepared for whole mount histology and skewered on a 4-prong land-mark device to provide visible markers for subsequent reconstruction.The cancer is delineated by a pathologist, then whole mount slides aredigitally photographed, aligned, and reconstructed into a 3D surface.These two surfaces are then aligned using a 3D correlation algorithmwith six degrees of freedom. After alignment, the tumor delineationdetermined by the pathologist is compared and fused with the tumorimaged using sonoelastography.Results: 3D images showing the resulting surface reconstructions, thefusion of the histology and ultrasound surfaces and the fusion of thehistology and sonoelastography tumors for three cases are presented. Incase 11683, the fusion of the surfaces yielded an intersection overunion of 0.821, the histology tumor within the gland yielded a volumeof 1.22 cc, while the sonoelastography tumor measured 1.49 cc.Conclusions: Image fusion, previously shown to be effective for vesselfusion, is viable for whole gland surface registration. We believe thatthis process should be the standard for validating 3D images in all casesand for 2D images when prior alignment of the image plane andhistology plane cannot be guaranteed.
32251
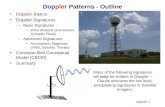
Evaluation of the effect of protamine on human prostatecarcinoma PC-3m using contrast-enhanced Doppler ultrasoundTang J,*1 Li S,1 Li J,1 Zhang Y,1 Li X,1 Dong B,1 Shi H,2 Zhang G,3
1. Department of Ultrasound, Chinese PLA General Hospital,Beijing, China, 2. Department of Pathology, Chinese PLA GeneralHospital, Beijing, China, and 3. Department of Statistic, ChinesePLA General Hospital, Beijing, China
Objective: The aim of this study was to evaluate the ability of contrast-enhanced Doppler ultrasound (CEDU) to demonstrate the changes in
Abstracts S57

tumor vascularity during angiogenesis inhibitive therapy in humanprostate carcinoma PC-3m.Methods: Pieces of human prostate carcinoma PC-3m tumor weretransplanted into 48 male BALB/C nude mice subcutaneously. Prota-mine was injected subcutaneously as an angiogenesis inhibitor. Theanimals were randomly divided into three groups according to theProtamine dose. Color flow signal-pixel rates (SPR) of the images werecalculated by using the number of pixels showing color Doppler signalsas a ratio of the total number of pixels covering the lesion.Results: The SPR of the high- and low-dose groups were significantlylower than that of the control group (P�0.01). The value of SPR in thethree groups was 0.09�0.05, 0.11�0.05, and 0.22�0.10 (mean�SD),respectively. SPR correlated significantly with microvessel density(MVD) (P�0.01, r�0.86–0.94).Conclusions: CEDU can effectively reveal the change of vascularity ina tumor, which has been treated with Protamine. In addition to MVD,CEDU may become one of several independent prognostic indices ofangiogenesis inhibitor therapy.
The Value of SPR and MVD in Three Groups
SPR (mean � SD) MVD (mean � SD)High-dose group 0.09 � 0.05 5.69 � 3.42Low-dose group 0.11 � 0.05 12.31 � 5.82Control group 0.22 � 0.10 24.08 � 7.71
NEW INVESTIGATOR
32930
Contrast-enhanced color Doppler targeted biopsy improvesprostate cancer detectionFrauscher F, Klauser A,* Feuchtner G, Horninger W, Halpern EJ,Bartsch G, Radiology II, Innsbruck, Tirol, Austria
Objective: We conducted a prospective study to determine whether alimited biopsy approach with contrast-enhanced color Doppler ultra-sound (US) targeted biopsy of the prostate could detect cancers as wellas gray-scale US-guided systematic biopsy with a larger number ofbiopsy cores.Methods: We examined 920 male screening volunteers (total PSAequal or greater than 1.25 ng/mL and free PSA � 18%). Two inde-pendent examiners evaluated each subject. One investigator performedcontrast-enhanced targeted biopsies (equal or less than 5) into hyper-vascular regions in the peripheral zone during intravenous infusion ofSonoVue (Bracco, Italy). Subsequently, a second examiner performed10 systematic biopsies of the prostate. Cancer detection rates for thetwo techniques were compared.Results: Cancer was detected in 284/920 subjects (31%). Cancer wasdetected in 230/920 subjects (25%) by contrast-enhanced targetedbiopsy, and in 201/920 patients (21%) with systematic biopsy. Cancerwas detected with targeted biopsy alone in 83 subjects (9%), and withsystematic biopsy alone in 54 subjects (6%). The overall cancer detec-tion rate (by patient) was significantly better for the targeted biopsy(p � 0.32). The odds ratio for detection of cancer by targeted biopsyversus systematic biopsy was 3.8 (p � 0.001).Conclusions: Contrast-enhanced color Doppler targeted biopsy signif-icantly improves cancer detection with fewer than half the number ofbiopsy cores compared with the systematic approach.
32040
Augmentation in lower extremity ultrasound for deep venousthrombus—Is it useful?Lockhart ME,* Sheldon HI, Robbin ML, Radiology, University ofAlabama at Birmingham, Birmingham, AL
Objective: The aim of this study was to determine the usefulness ofvenous flow augmentation in lower extremity evaluation for deepvenous thrombus (DVT).Methods: 1092 consecutive patients were prospectively evaluated byDuplex ultrasound in an ACR accredited laboratory from 7/1/2001 to12/31/2001, using a standard ACR protocol. Augmentation of venousflow was not performed if an ipsilateral thrombus was discovered. Theinitial examination in each person during that time frame was evalu-ated; therefore, 108 follow-up studies were excluded. In 984 examina-tions (1967 lower extremities), the sonographer recorded the sono-graphic findings on a worksheet. Augmentation was graded useful ornot, and the reason it was useful was recorded. Worksheet data wereentered in a database for analysis.Results: Augmentation was described as useful in only 4.2% (41/984)of the patient studies. In those examinations where it was deemedhelpful, it was most often used to demonstrate slow flow in a vein(76%) (31/41), less frequently to help visualize the vein (17%) (7/41),or both (7%) (3/41). The augmentation maneuver did not assist in thedetection of DVT in any patient. In 2 patients with DVT, augmentationhelped improve confidence that no contralateral thrombus was present.Experience level did not affect the frequency of whether augmentationwas judged useful or not. The prevalence of lower extremity DVT was10.6% (104/984). Most of the DVTs were non-occlusive (70.0%)(159/312 segments), and most patients with DVT had more than onesegment involved (53.8%) (56/104). Isolated femoral vein thrombuswas identified in only 0.8% of patients.Conclusions: No additional DVTs were discovered by the augmenta-tion maneuver in this large series of patients. Augmentation was onlyrarely useful, most often to demonstrate slow flow in a vein. The timecost of augmentation is small. However, other factors such as patientdiscomfort or the need for an additional sonographer to perform aug-mentation, combined with its lack of utility, may justify removal ofaugmentation from a standard study. Augmentation may function betteras a diagnostic adjunct in cases of uncertainty.
32301
Percutaneous sonographically guided microwave coagulationtherapy of hepatocellular carcinoma: Results in 234 patientsBaowei D, Ping L,* Xiaoling Y, Department of Ultrasound, ChinesePLA General Hospital, Beijing, China
Objective: The objective of our study was to evaluate the long-termresults of percutaneous microwave coagulation therapy for the treat-ment of hepatocellular carcinoma in a large patient population.Methods: Survival rates were determined in 234 patients with 339nodules of hepatocellular carcinoma who had undergone percutaneousmicrowave coagulation therapy (208 men, 26 women; mean age, 54.8years; mean tumor size, 4.1 � 1.9 cm, range 1.2–8.0 cm, meanfollow-up period, 27.9 months). Patients were those rejected as candi-dates for surgery by the surgery department, who fit our study’s criteria,and who agreed to participate. After baseline imaging studies wereperformed, the patients were followed up using the same combinationof sonography, CT or MR imaging, and/or post-treatment biopsy.Results: After percutaneous microwave coagulation therapy, colorDoppler flow signals disappeared in 92.0% (263/286) of the lesions. Noenhancement was apparent in 89.2% (190/213) lesions and 89.1%(41/46) of the lesions on contrast CT and MR imaging, respectively.Post-treatment biopsies of 194 nodules showed no evidence of surviv-ing tumor tissue in 180 (92.8%). Resections of six lesions revealedcomplete tumor necrosis in five. One, 2, 3, 4, and 5-year cumulativesurvival rates were 92.7%, 81.6%, 72.9%, 66.4%, and 56.7%, respec-tively. There were statistically significant relationships (P�0.021) be-tween survival curves and the degree of hepatocellular carcinoma
S58 Ultrasound in Medicine and Biology Volume 29, Number 5S, 2003