Epilepsy in Munster 2011
description
Transcript of Epilepsy in Munster 2011

1
Epilepsy in Munster 2011
Dr Brian Sweeney Consultant Neurologist CUH

2
Target population Munster 1.2 million Parts of Kilkenny and Wexford If Epilepsy prevalence is 0.65% c. 8000
people have epilepsy in this region 30-40% have drug resistance All need proper counselling and discussion
re diagnosis and its management

3
Irish and UK data Up to 40 000 Irish people have epilepsy At least 2-3 seizures present to CUH Casualty
each day (Audit August/September 2004) UK
160 000 people will require hospital treatment 25 000 > 1 major seizure/month 60 000 > 1 minor seizure/month 20 000 patients have severe disabilities requiring
institutional care

4
Epilepsy
Definition Classification Prevalence Pathogenesis Investigation Treatment Long term prognosis

5
Definition
Recurring unprovoked seizures due to paroxysmal neuronal discharge

6
Classification
Can be based on cause or mode of onset. Mode of Onset
Partial (Focal) onset Generalised Unclassifiable

7
Partial Seizures Partial - onset in a focal region of cortex Simple partial - sensory, motor, autonomic or
psychic - without loss of consciousness Complex Partial - consciousness impaired Complex Partial with Secondary Generalisation -
evolving into a full-blown seizure Temporal, Frontal, Parietal or Occipital in origin

8
Generalised Bilateral synchronous cortical spike and wave
discharge generated by thalamic slow calcium channels
Tonic-Clonic Typical Absence Atypical Absence Myoclonic Tonic Atonic

9
Frequency of different types
1/3 generalised in onset 2/3 partial in onset, most commonly
temporal lobe attacks

10
Status Epilepticus
Recurring seizures without recovery of consciousness in between
Convulsive status Absence status Complex partial status Epilepsia partialis continuans

11
Secondary (‘Symptomatic’) Seizures
Seizures secondary to an acute metabolic, drug-induced or neurological condition
Patients usually not vulnerable in the long term if underlying cause is reversed.

12
Incidence
Developed countries 50/100000/year (range 40-70)Underdeveloped countries - 100-190/year - only 6%of PWE in Pakistan or Phillipines on rx at any one timePatients may not be aware that they have epilepsy

13
Prevalence
5-10/1000 persons Lifetime prevalence is 2-5% As the population ages there will be an
increased incidence and prevalence of epilepsy - at least 20% of new onset cases will be over 60
Febrile seizures prevalence - 5%

14
Aetiology General Data 60-70% no clear cause
(‘Cryptogenic epilepsy) Cerebrovascular disease/Brain tumour/Alcohol-
induced/Post-traumatic With the advent of MRI increasing numbers of
structural lesions such as HS, Cortical dysplasia, Small foreign tissue lesions
Some patients may be reclassifed as having a generalised syndrome with analysis of EEG records
Recent NSE data - up to 60% of a community based MRI series have some structural lesion

15
Pathogenesis Still not fully elucidated Discharges occur in the neocortex and limbic
structures such as the Amygdala and Hippocampus
Large 20-40mV discharges in a group of at least 1000-2000 neurones (‘minimum aggregate zone’
Giant EPSPs - glutamate dependent, voltage-sensitive calcium channels, voltage sensitive sodium channels
Excitatory neurones must be connected into a synaptic network

16
Pathology Seizures complicate many brain diseases eg
Alzheimer disease Hippocampal Sclerosis Cortical dysplasia Lesion-associated - tumours/AVMs Inflammatory, Traumatic, Hypoxic-|schaemic
lesions Conditions and lesions secondary to seizures Dual pathology

17
Investigation
Brain structural imaging -CT and MRI Functional imaging -fMRI/Ictal
SPECT/PET

18
Hippocampal sclerosis

19
Dysembryoblastic Neuroepithelial Tumour

20
Left Temporal AVM

21
Focal Cortical Dysplasia

22
Investigation EEG - only 50% will have interictal abnormalities
- a normal EEG does not exclude Epilepsy! Some patients may never have any EEG findings
Sleep EEG Video-EEG - at least 70% of our recordings do
not have demonstrate attacks With sphenoidal leads Cortical monitoring - Depth electrodes
Therapeutic trial

EEG – 3/s spike and wave
23

24
Bloods/Cardiovascular
FBC/U+E/Calcium/Magnesium/Glucose Toxicology ECG/Holter/ECHO/Syncope studies

25
Differential Diagnosis Cardiovascular Metabolic Psychogenic - ‘Non-Epileptic Attack
Disorder’ aka Pseudoseizures
Up to 1/3 of referrals to an Epilepsy Centre (Walton, Liverpool) were found to have alternative causes for episodes

26
Counselling/Treatment - General principles Generally not if only one episode (but maybe if
+ve EEG/Structural brain lesion/Elderly/Severe episode)
‘Oligo-Epilepsy’ Treatment for at least 2 years Try to keep to once or twice per day Inform patient about side effects and the
possibility of treatment failure Lifestyle issues – alcohol/drugs

27
General Principles Cannot drive until 12 months seizure-free Exceptions:
Sleep attacks only for > 2 years May resume driving in 6 months if seizure
related to medication change or surgery work-up
Simple partial seizures without disturbance of consciousness or motor control
All must be certified by a neurologist

28
Women with Epilepsy
Inform re potential interactions of the specific drug with OCP
Inform re teratogenic risk Potential changes in Pharmacology in
pregnancy Folic Acid 5mg/day Vitamin K supplementation

29
Drug therapy Bromide - Sir Charles Locock - May 11 1857 to
Royal Medical and Chirurgical Society Barbituric acid - Saint Barbara’s Day 1864. AE
properties recognised by Hauptmann - 1912 Phenytoin - Putnam and Merritt using Phenyl
ring containing compounds provided by Parke-Davis - 1938
Trimethadione - 1944 - succeeded by Ethosuximide

30
Drug therapy
Carbamazepine - synthesised by Geigy chemists in 1953
Valproic acid - organic solvent synthesised 1881. AE properties recognised in France 1961 and first marketed in 1967

31
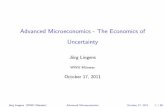
Drug GABA-mediated
Blockade voltage gated Na channels
Blockade voltage gated Na channels
Unknown
PBZ Yes
PHT Yes
CBZ Yes
VALP Yes Yes Yes
ETH Yes
BENZ Yes
VIGA Yes
LAM Yes
GAB Yes
PRE-G Yes
LEV Yes
TOP Yes Yes Yes
OXC Yes

32
Drug Choice?
Age/Gender Need rapid onset of action? OCP/Pregnancy Prior drug history Efficacy vs Side Effects Status Epilepticus - drug has to be soluble

33
Drug Choice?
Broad Spectrum - work in all types Valproate Lamotrigine Topiramate Levetiracetam Zonisamide Phenobarbitone Benzodiazepines

34
Drug Choice? Narrow spectrum
Partial-onset• Carbamazepine• Phenytoin• Vigabatrin• Gabapentin• Tiagabine• Oxcarbazepine• Pre-Gabalin
Absence attacks - Ethosuximide

35
Most commonly used by me!
Carbamazepine Valproate Lamotrigine
Levetiracetam Phenytoin Topiramate

36
Combination Treatment/Polypharmacy
May help some patients Increased risk of interactions
In our QOL study of 90 consecutive patients most important discriminator was seizure freedom and not number of drugs taken

37
Prognosis 60-70% should expect to be seizure-free without
major side effects In these patients the choice of drug may not
matter that much - they might respond any drug they try
However relapse rates as high as 40% if drugs are withdrawn even after good long term control
Major socio-economic effects if seizures relapse Put pros and cons to patient and give them your
assessment of their individual risk

38
Drug-resistance Seizures refractory for more than 2 years of
trying more than 3-4 AEDs 30-40% of patients - pharmacogenomics an
increasing area of interest
Reassess diagnosis and other factors like compliance or lifestyle problems
Video-EEG Repeat imaging

39
If focal onset…. Surgery may be an option High quality MRI Video-EEG - catch at least 2-3 attacks to ensure
consistent seizure focus Neuropsychology Psychiatry review If there is congruence between MRI and EEG
findings surgical resection is possible At least 3000 Irish patients might be suitable for
such surgery

40
Surgery Best results with clear Temporal origin
50% become seizure free 20% significantly improved <1% risk of adverse outcome 10% risk of psychiatric problems
Frontal <50% chance of good outcome Occipital/Parietal - greater risk of surgery causing
deficit

Ictal PET Scan
41

42
Other options…
Vagus nerve stimulation Deep brain stimulation Seizure detection and immediate response
drug delivery systems Gamma knife

43
Prognosis Generally good However SMR x 3 times controls Due to cause of epilepsy/accidents Sudden Unexpected Death in Epilepsy (SUDEP)
Young adults/Early age on onset/Generalised Tonic-Clonic seizures/High seizure frequency/Polypharmacy/Poor compliance