Definition of Coronary Artery Disease
-
Upload
cardiacinfo -
Category
Documents
-
view
671 -
download
0
description
Transcript of Definition of Coronary Artery Disease

Imbalance Between Myocardial Supply and Demand
Irma B.Ancheta,PhD,RN.

Learning Guide:• Pathophysiology of atherosclerosis, arteriosclerosis, Acute
Coronary Syndrome• Modifiable and non-modifiable risk factors for CAD (Coronary
Artery Disease)• Anti-platelet medications:
– aspirin– Plavix (clopidogrel)
• Medications for dyslipidemia:– HMG Co-reductase inhibitors– Niacin– Fibric acid derivatives
• Anti-anginal medications:– Nitroglycerin preparations– Beta blockers
• Calcium channel blocke

Learning Guide:• Assessment of men and women presenting with s/s of angina, or ACS
(Acute Coronary Syndrome)• Definitions and defining characteristics of:
– Decreased cardiac output r/t ventricular damage, dysrhythmias– Acute pain r/t myocardial tissue damage from inadequate blood supply– Risk for bleeding r/t thrombolytic therapy– Risk for peripheral neurovascular dysfunction
• Definition and Indicators of these NOCs:– Cardiac pump effectiveness– Tissue perfusion, peripheral
• Review these NICs:– Cardiac Care– Cardiac care, acute
• Circulatory precautions

Learning Objectives:• Describe assessment strategies (and related nursing
care) for patients with ACS:– Stress tests, echocardiography, cardiac catheterization,
ECG monitoring• Plan, implement and evaluate care for patients
experiencing Unstable angina, NSTEMI, MI• Plan, implement and evaluate care for patients post
interventional cardiology procedures• Describe interventional (cath lab)/surgical
interventions for myocardial revascularization• Describe health promotion strategies (and teaching
plans) for patients at risk of CAD/ACS.

Cardiac Review

A&P Review
Layers of the HeartPericardiumEpicardiumMyocardiumEndocardium

A&P Review
Cardiac ChambersAtriaVentricles


Cardiac Valves
Atrioventricular Valves
Tricuspid and mitral
Semilunar ValvesPulmonic and aortic

A&P ReviewConduction System
AtriaSinoatrial nodeInternodal pathwaysIntraatrial bundle
AV Node to Bundle of HIS
VentriclesRight and left bundle branchesPurkinjie fibers

Electrical Conduction System

A&P Review
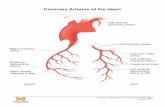
• Coronary Blood Supply
– Coronary Arteries• Left coronary artery divides into left anterior
descending and left circumflex• Right coronary artery perfuses the right side of the
heart and in most people the SA and AV nodes• In 70% of the population the RCA perfuses the
posterior coronary artery

Right coronaryartery
Coronary Arteries

A&P Review
• Venous Return from the Heart– Coronary sinus– Thebesian vessels drain directly into the chambers
of the heart and produce physiologic shunt

A&P Review
• Systemic Circulation– Arterial system of resistance vessels– Capillary bed: tissue perfusion– Venous system of capacitance vessels

A&P Review
• Physiology– Properties of cardiac tissue• Excitability• Conductivity• Automaticity• Rhythmnicity• Contractility• Refractoriness

A&P Review
• Electrical Activity– Action potential

A&P Review
• Cardiac Cycle– Ventricular systole– Ventricular diastole– Cardiac Output

A&P Review
• Regulation of Heartbeat – Nervous control– Intrinsic regulation

A&P Review
• Control of Peripheral Circulation– Intrinsic Control– Extrinsic control

Ejection Fraction

Ejection Fraction
Normal = 50% or higher
Low = < 40%

Ejection Fraction
[1] MUGA (multiple-gated acquisition) Scan
[2] echocardiogram
[3] Cardiac Catheterization
[4] Nuclear tests

Risk Factors associated with Coronary Artery Disease

Objectives:
• Definition of CAD• Identifying risk factors (a) effects (b) treatments (c) management• Latest developments

CAD Statistics
• Affects nearly 13 million people in the USA• Causes 500,000 deaths each
year

Framingham Heart Study (FHS)


Definition of Coronary Artery Disease
• A narrowing of the inside diameter of arteries that supply the heart with blood.
• The condition arises from the accumulation of plaque and greatly increases the risk of having a heart attack or myocardial infarction (Cooley, 1996).

Modifiable Risk factors
• Pathophysiologic factors:
Hypertension Diabetes Hyperlipidemia
• Life style factors Smoking Obesity Physical
Inactivity Stress

Nonmodifiable risk factors
• AGE• GENDER• RACE/ETHNIC BACKGROUND• HEREDITY

Emerging Risk Factors• Homocysteine= blocks NO production < elastic Blood vessels permit plaque
formationTTT= B complex Folic acid, Niacin• LDL-C = mechanical injury• Prothrombotic state (e.g., high fibrinogen or plasminogen activator inhibitor–1 in
the blood)• Proinflammatory state (e.g., elevated C-reactive protein in the blood causes
inhibition of NO)• Low Adiponectin levels increase CRP production

Five Major Risk Factors
• 1.Smoking• 2.Hypertension• 3.High cholesterol• 4.Diabetes• 5.Family History

Smoking
Effects of Smoking• Roughening effect of inside diameter of
the arterial wall>formation of plaque,constriction of arteries>HPN
• Increases heart rate and produces irregular heartbeats>clots>stroke
• Decrease HDL levels and increase LDL > increase risk CAD

Management of Smoking
• Quit Smoking• Avoid secondary smoke

Hypertension:
• Or high blood pressure.. SBP >120 mm Hg ..DBP>80 mm Hg• Indicates a problem in the mechanism that
regulates blood pressure in the circulatory system
• “hyper” too much “tension” pressure

Hypertension
Effects of HPN• [Mechanical Injury] Causes thickening or hardening
of the walls off the arteries>causes narrowing >decrease blood flow to coronary arteries>MI.
• Thickening of left ventricle >decrease Cardiac output > causes CHF
> kidney damage>Renal dialysis• In the diabetic population, HPN>retinal
damage(retinopathy)>BLINDNESS

For persons over age 50, SBP is a more important than DBP as CVD risk factor.
Starting at 115/75 mmHg, CVD risk doubles with each increment of 20/10 mmHg throughout the BP range.
Persons who are normotensive at age 55 have a 90% lifetime risk for developing HTN.
Those with SBP 120–139 mmHg or DBP 80–89 mmHg should be considered prehypertensive who require health-promoting lifestyle modifications to prevent CVD. (JNC 7, 2003)
New Features and Key Messages

New Features and Key Messages (Continued)
Thiazide-type diuretics should be initial drug therapy for most, either alone or combined with other drug classes.
Certain high-risk conditions are compelling indications for other drug classes.
Most patients will require two or more antihypertensive drugs to achieve goal BP.
If BP is >20/10 mmHg above goal, initiate therapy with two agents, one usually should be a thiazide-type diuretic. (JNC 7, 2003)

Blood Pressure Classification
Normal <120 and <80
Prehypertension 120–139 or 80–89
Stage 1 Hypertension
140–159 or 90–99
Stage 2 Hypertension
>160 or >100
(JNC 7, 2003)
BP Classification SBP DBP

Benefits of Lowering BP
Average Percent ReductionStroke incidence 35–40%
Myocardial infarction 20–25%
Heart failure 50% (JNC 7, 2003)

BP Control RatesTrends in awareness, treatment, and control of high
blood pressure in adults ages 18–74
National Health and Nutrition Examination Survey, Percent
II1976–80
II(Phase 1)1988–91
II(Phase 2)1991–94 1999–2000
Awareness 51 73 68 70
Treatment 31 55 54 59
Control 10 29 27 34
Sources: Unpublished data for 1999–2000 computed by M. Wolz, National Heart, Lung, and Blood Institute; JNC 6.

Summary:

Treatment Overview
Goals of therapy• Lifestyle modification• Pharmacologic treatment– Algorithm for treatment of hypertension
• Classification and management of BP for adults
• Follow-up and monitoring (JNC 7, 2003)

Management of hypertension
• Exercise• Proper stress management• Quit Smoking• Healthy diet• Decrease sodium intake.• Anti- HPN Medication

Lifestyle Change: What Difference Does it Make ?
• Weight loss. (decreases SBP*1.6 mm Hg for each kg lost)
• Dietary Approaches to Stop Hypertension: DASH diet:– (decreases systolic BP 8-14 mmHg)
• Reducing salt in the diet.(decreases SBP 2-8 mmHg)
• 30-45 minutes daily aerobic exercise– (decreases systolic BP 4-9 mmHg)
• Limit alcohol. (decreases SBP* 2-4 mm Hg)
• Avoidance of tobacco products.(*SBP = systolic blood pressure)

Medications for HPN
• Diuretics• Beta-Blockers• Calcium channel Blockers• ACEI• Vasodilators

Diabetes
• Causes vasoconstriction of coronary arteries
>decrease blood flow > decrease oxygen supply
>increase risk of heart attack or MI

Management of Diabetes
Healthy diet. Exercise Stress Management Medications Check Blood sugar regularly

CHOLESTEROL
Effects of Increased Cholesterol levels
• Causes plaguing of the coronary walls, narrows coronary arteries,creates blockage of coronary arteriesless blood flow to heart cells >MI

Cholesterol
• LDL cholesterol• HDL cholesterol• Total cholesterol• Triglycerides

Serum cholesterol levelsLDL Cholesterol –Primary Target of therapy<100 Optimal100-129 Near optimal/above optimal130-159 Borderline high160-189 High190 > Very HighTotal cholesterol < 200 Desirable 200 - 239 Borderline 240 > High HDL<40 Low>60 High (NCEP/ATP III Guidelines, 2004)

Management of Cholesterol Levels
DIET
MEDICATION NON-SMOKING EXERCISE

Family History
• Parent or sibling that died of CAD less than 60 years of age...

Medications for CAD
[1] Anti-platelet medications
[2] Medications for dyslipidemia
[3] Anti- anginal medications

Anti-platelet medications
[1] Aspirin
[2]Clopidogrel (Plavix)

Medications for dyslipidemiaHMG CoA-reductase inhibitors Nursing Interventions(statins)[1] Rosuvastatin No grapefruit[2] Simvastatin Monitor liver enzymes[3] Atorvastatin Instruct pts. mm tenderness[4] Pravastatin Take at night Niacin[1] Niaspan,Niacin With meals/Flushing/?medFibric Acid Derivatives[1] Lopid 30 minutes before or with meals[2] Zetia

Anti- anginal medications
[1] NTG preparations
[2]Beta-blockers
[3] Calcium channel blockers

Summary of risk factors for CAD
[1] ?[2] ?[3] ?[4] ?[5] ?

How many risk factors for CAD do you have?

Coronary Artery Disease

Coronary Artery Disease (CAD)
• CAD is a broad term that includes stable angina pectoris and acute coronary syndromes. When blood flow through the coronary arteries is blocked, ischemia or infarction of the myocardium may result.

Ischemia and Infarction
• Ischemia occurs when insufficient oxygen is supplied to meet the requirements of the myocardium
• Infarction (necrosis of the cells, cell death) occurs when sever ischemia is prolonged and irreversible damage to tissue results.

Acute Coronary Syndromes• Angina- coronary ischemia- a temporary imbalance
between the coronary arteries ability to supply oxygen and the cardiac muscle’s demand for oxygen (no permanent damage to myocardial tissue).
• Stable Angina- predictable; fixed lesions
• Unstable Angina- more intense, may occur at rest or with exertion and causes marked limitations of activity. Attacks increase in intensity and pain. Includes new-onset angina, variant (Prinzmental’s) angina, pre-infarction angina and crescendo angina

Angina
• Location• Duration• Quality• Radiation• Precipitating Factors• Medication Relief

Myocardial Infarction
• Irreversible necrosis due to an abrupt decrease or total cessation of coronary blood flow.– Plaque rupture– New thrombus in coronary artery

Process of Infarction
• Tissue Ischemia• Hypoxemia• Autonomic Nervous System Influences• Metabolic Derangement• Acid-base imbalances• Hemodynamic disturbances• Electrolyte disturbances• Fiber stretch

Zone of Infarction
• Dependent on Three Factors:– Collateral circulation– Anaerobic metabolism– Workload demands

Types of Infarction• Subendocardial Infarction (non-Q wave)(multifocal areas of necrosis confined to the inner 1/3-1/2 of the
left ventricular wall. These do not show the same evolution of changes seen in a transmural MI. )
• Transmural Infarction (Q wave)(involving the entire thickness of the left ventricular wall from
endocardium to epicardium, usually the anterior free wall and posterior free wall and septum with extension into the RV wall in 15-30%).
Physiologic response = ventricular remodeling (change in shape and size of L ventricle causing decrease L V F leading to HF)

Zones of Infarction
Zone of Ischemia = T-wave inversion
Zone of Injury = ST elevation
Zone of Necrosis = Abnormal Q wave


Classification of MI by Location
Inferior: Abnormalities that appear in leads II, III, and F (called the inferior leads) indicate pathology on the inferior or diaphragmatic surface of the heart.
Lateral: Leads I, F, and V5-V6 are called lateral leads. Abnormality in these leads indicates pathology on the lateral, upper surface of the heart.
Anterior: Anterior pathology is seen in leads V1-V4, and often in lead I.
Posterior: Problems on the posterior surface of the heart are difficult to diagnose using the standard 12 ECG leads. The pathology may be seen as “reflected” through V1 and V2.
Combination: Abnormalities may not be limited to one of the four areas above. Inferolateral damage will show up in a combination of the inferior and lateral leads. Anterolateral damage will be seen in both the anterior and the lateral leads.

Normal 12 lead EKG

? MI????


Identify which coronary artery is affected?
[1] severe crushing chest pressure/pain/radiating to neck
[2] chest pressure/pain with radiation to L arm
[3] chest pressure radiating to the back/scapula.

Cultural Considerations• Black and Hispanic women have a higher incidence of
CAD risk than white women with comparable socioeconomic status
• Native Americans/American Indians/Alaskan Natives >18 years of age have greater incidence of HTN, smoking, high cholesterol, excess weight, and/or diabetes mellitus
• Leading cause of death in men and women in the most prevalent ethnic groups is cardiac disease even though there are genetic predispositions to develop risk factors (AHA, 2003)

Cultural Considerations
• Higher incidence of HTN in Black community and in whites in the South
• Black individuals experience longer delays in seeking treatment
• Symptom may be dyspnea and not chest pain
• Symptoms in older adults may not be associated with acute chest pain

Women and Heart Disease
• More women than men have angina but many women experience atypical angina.– What does atypical mean?
• Women have MI at older ages than men• Lack of education in women that CAD is the leading
cause of death in women• Pathophysiology in women is different than men i.e.
smaller vessels, less collateral circulation than men• Impaired glucose tolerance seriously increase risk

Heart Disease: The Leading Cause of Death for American Women
American Heart Association

Cardiovascular Disease Mortality Trends United States: 1979-2001
Source: CDC/NCHS.

Why The Gender Gap?
• Women present to emergency rooms or chest pain centers 1- 2 hours later than men.
• Do the multiple roles a woman takes on delay care because of her responsibilities to others?
• Do women delay care because they perceive that heart disease is something that happens to one’s father, brother, or spouse?

Differences in Heart Attack Symptoms
Men• Sub-sternal
chest pain or pressure
• Rest pain• Pain down left
arm and shoulder
• Weakness
Women• Pain in chest,
upper back, jaw or neck
• Shortness of breath
• Flu-like symptoms: nausea or vomiting, cold sweats
• Fatigue or weakness
• Feelings of anxiety, loss of appetite, malaise

Postmenopausal Hormone Therapy (HT)
• Postmenopausal HT is no longer recommended as a strategy to prevent heart disease.
• Hormone therapy, generally short term, may still be used to treat symptoms of menopause - this is a decision between a woman and her healthcare provider.

The Red Dress Campaign

Cardiac Management

Collaborative Management• History
• Pain Assessment
• Cardiovascular Assessment
• Psychosocial Assessment
• Laboratory Assessment
• Radiographic Assessment
• Other Diagnostic Assessments

History/ Pain Assessment
• Historical data• If chest pain present, describe and find out for
how long (time is muscle)• Attempt to differentiate between angina pain
and infarction pain
• Associated symptoms patient describes i.e. N/V, diaphoresis

Cardiovascular and Physical Assessment
• Vital signs• Monitor for dysrhythmias• Distal peripheral pulses• Heart and Lung sounds

Cardiac Auscultation

Psychosocial Assessment
• Denial• Fear • Anxiety• Anger

Laboratory Assessment• Troponin T and I- myocardial muscle protein released into the
bloodstream with injury to the myocardial muscle (not found in healthy clients)
• Creatine kinase- MB (CK-MB) is an enzyme specific to cells of the brain, myocardium and skeletal muscle. Indicates tissue necrosis or injury, Cardiac specificity is determined by measuring the isoenzyme activity CK-MB is found in myocardial muscle CK-MM (skeletal) CK-BB (brain)
• Myoglobin early marker of MI is a low-molecular-weight heme protein found in cardiac and skeletal muscle, appears as early as 2 hours after an MI with rapid decline after 7 hours
• C-Reactive Protein is a marker of inflammation. Any inflammatory process can increase CRP in the blood

Additional Laboratory Tests
• Homocysteine• Serum Lipids• PT, PTT, INR• Arterial Blood Gases• Serum Electrolytes• CBC

Radiographic and Other Diagnostic Tests
• Chest X-ray• ECG- what are we looking for?• Stress Tests- exercise tolerance testing with or
without pharmacologic agents• Myocardial Perfusion Imaging- Thallium scans• Cardiac Catherization

Cardiac Catherization
• This procedure is performed to determine the extent and exact location of obstruction of the coronary arteries. Helps to identify course of therapy for patients i.e. PTCA/stent or CABG



Nursing Diagnosis & collaborative problems.
• Acute pain related to biologic injury agents• Ineffective tissue perfusion related to
interruption of arterial blood flow• Activity intolerance related to fatigue• Ineffective coping related to effects of acute
illness and major changes in lifestyle• Potential for dysrhythmias• Potential for heart failure• Potential for recurrent symptoms and
extension of injury

NICs/NOCs• NIC– Pain Management– Drug Therapy
• NOC– Ineffective Tissue Perfusion- expect to have
adequate blood flow to maintain heart function• Ejection fraction• Pulmonary wedge pressure• Apical heart rate• Systolic and diastolic blood pressure

Collaborative Management
• MONA- M=morphine O= oxygen N= nitroglycerine A= aspirin• Thrombolytic Therapy• Beta Blockers or Calcium Channel Blocker)• ACE Inhibitors• Antiplatelet Agents- ASA, Plavix, Ticlid

Potential Complications and Interventions
• Dysrhythmias- ventricular in origin
• Ventricular Failure- Class I- IV
• Cardiogenic Shock- Intra-Aortic Balloon Pump (IABP)
• Thrombolytic Therapy- Fibrinolytics and/ or Glycoprotein IIb/IIIa inhibitors
• PTCA