Coronary Artery Anatomy
-
date post
14-Apr-2015 -
Category
Documents
-
view
89 -
download
0
Transcript of Coronary Artery Anatomy

AJR:188, June 2007 1665
AJR 2007; 188:1665–1674
0361–803X/07/1886–1665
© American Roentgen Ray Society
Kini et al.CT Angiography of Coronary Arterial and Venous Anatomy
C a rd i a c I m ag i n g • P i c t o r i a l E s s ay
Normal and Variant Coronary Arterial and Venous Anatomy on High-Resolution CT Angiography
Sunil Kini1, 2
Kostaki G. Bis2
Leroy Weaver2, 3
Kini S, Bis KG, Weaver L
Keywords: anatomy, anomalies, arteriography, cardiac imaging, coronary arteries, CT angiography, heart, MDCT
DOI:10.2214/AJR.06.1295
Received September 30, 2006; accepted after revision January 15, 2007.
1Present address: Quantum Medical Radiology, Atlanta, GA 30339.
2Department of Diagnostic Radiology, William Beaumont Hospital, 3601 W 13 Mile Rd., Royal Oak, MI 48073. Address correspondence to K. G. Bis ([email protected]).
3Present address: Elkhart General Healthcare System, Elkhart, IN 46514.
CMEThis article is available for CME credit. See www.arrs.org for more information.
OBJECTIVE. This article displays the normal and variant anatomy of the coronary arteriesand subjacent cardiac veins using a high-resolution 64-MDCT scanner.
CONCLUSION. Knowledge of the anatomy of the coronary arteries and subjacent car-diac veins as displayed with maximum intensity and volume-rendered projections is importantfor correct image interpretation of coronary CT angiography examinations.
ontrast-enhanced CT angiography(CTA) of the coronary arteries isbecoming feasible as temporal andspatial resolution improves with
the availability of MDCT. Detection, charac-terization, and quantification of coronary ar-tery disease and elegant delineation of coro-nary anatomy are possible using 2Dmultiplanar reformation (MPR), 3D maxi-mum-intensity-projection (MIP), and 3D vol-ume-rendered postprocessing techniques. Fa-miliarity with coronary artery and venousanatomy and anatomic variants is important forcorrect image interpretation. This anatomy andthe arterial variants have been well describedusing conventional angiographic techniques[1, 2]. However, the cross-sectional nature ofCT has the benefit of more precisely display-ing the spatial relationships of coronary arterialand venous anatomy with respect to cardiacstructures. This article highlights this anatomywith a variety of MIP and volume-renderedtechniques (Figs. 1–18).
Subjects and MethodsCoronary CTA protocols usually image the heart
using cranial-to-caudal acquisition [3]. However,caudal-to-cranial scanning acquisitions are imple-mented when concomitant imaging of the pulmo-nary arteries is desired in patients with atypicalchest pain [4]. We describe both of these protocolsbecause the cardiac venous anatomy may be dis-played with variation in enhancement depending onthe type of data acquisition.
The patients who participated in our study wereimaged after the institutional review board had ap-proved the study, which complies with the Health In-surance Portability and Accountability Act, and after
they had provided written informed consent. Patientswere recruited from October 2004 to June 2005.
Imaging was performed on a 64-slice (32-detec-tor) MDCT scanner (Sensation Cardiac 64, Sie-mens Medical Solutions) after the patient was pre-medicated with oral atenolol (50–100 mg), IVmetoprolol (5- to 10-mg boluses, up to 50 mg), orboth. An upper extremity 20-gauge IV catheter wasused for venous access. Sublingual nitroglycerin(0.4 mg) was provided to induce coronary vasodi-latation. Bolus timing was measured in the mid as-cending aorta with 20 mL of iodixanol (320mgI/mL [Visipaque, GE Healthcare]) administeredat a rate of 5 mL/s followed by a 50-mL saline flush,also administered at a rate of 5 mL/s). Alternatively,bolus tracking can be used to trigger data acquisi-tion by placing a region of interest over the mid as-cending aorta and setting the trigger threshold to160 H above baseline.
Single-sector reconstructions of the coronary arter-ies were performed at 65% and 35% of the R-R lengthand were then modified to a different phase start ifthere were motion artifacts. Reconstructions were per-formed on a workstation (Wizard, Siemens MedicalSolutions) and then transferred to another workstation(TeraRecon, TeraRecon) for MPRs and MIPs.
Cases were selected to show the normal coronaryarterial and venous anatomy. MIPs were obtained us-ing various thicknesses (5–30 mm) and were dis-played using standard orientations (right anterior ob-lique, left anterior oblique, axial) with or withoutcaudal or cranial angulation. Volume-rendered im-ages were also obtained using various orientations.
Cranial-to-Caudal AcquisitionCoronary CTA was performed 5 seconds after
aortic peak density; 100 mL of iodixanol (Visi-paque) was administered at 5 mL/s and was fol-
C

Kini et al.
1666 AJR:188, June 2007
lowed by a 50-mL saline flush at 5 mL/s [3]. Retro-spective ECG-gating was used with the followingparameters: collimation, 0.6 mm; tube rotationtime, 0.33 seconds; tube voltage, 120 mV; effectivemAs, 750–850; pitch, 0.2; and scanning time,10–12 seconds.
Scanning coverage was from the level of the car-ina to the bottom of the heart. Reconstruction field ofview, slice thickness and reconstruction increment,and smooth kernel were as follows: 15–22 cm; 0.6and 0.3 mm, respectively; and B25f. ECG pulsing isusually implemented for tube current modulationand is needed to reduce radiation exposure [5].
Caudal-to-Cranial AcquisitionFor the caudal-to-cranial acquisition, a patient
preparation and scanning protocol similar to thatdescribed in the previous section was used. How-ever, contrast injection was performed with ahigher volume of contrast material using a biphasicprotocol: 100 mL of iodixanol was administered at5 mL/s followed by 30 mL of iodixanol at 3.0 mL/sand then a 50-mL saline flush at 3 mL/s. The addi-tional volume of contrast material resulted in a pro-longed time for contrast injection to ensure ade-quate enhancement of the pulmonary arteries [4].As a result, streak artifacts arising from the superiorvena cava and right atrium were present in 37(88%) of 42 studies; however, these artifacts inter-fered with the visualization of the right coronary ar-tery (RCA) in only one (2.4%) of the 42 cases [4].
The thorax from the lung bases to just above(1–2 cm) the aortic arch was scanned with a 12- to15-second acquisition (no ECG pulsing), but scan-ning can include the entire thorax when ECG puls-ing is applied. As with cranial-to-caudal acquisi-tions, ECG pulsing is needed to reduce radiationexposure [5]. Reconstruction field of view, slicethickness and reconstruction increment, and kernelfor the coronary arteries were similar to those forthe cranial-to-caudal acquisition. However, recon-structions were also obtained with a larger field ofview [4] to display the pulmonary arteries, thoracicaorta, lungs, and thoracic soft tissues.
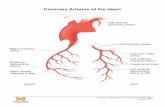
Normal Anatomy of the Coronary Arteries
The right and left coronary arteries origi-nate from the right and left sinuses of Valsalvaof the aortic root, respectively. The posteriorsinus rarely gives rise to a coronary artery andis referred to as the “noncoronary sinus.” Thelocations of the sinuses are anatomic misno-mers: The right sinus is actually anterior in lo-cation and the left sinus is posterior. The my-ocardial distribution of the coronary arteriesis somewhat variable, but the right coronaryartery (RCA) almost always supplies the right
ventricle (RV), and the left coronary artery(LCA) supplies the anterior portion of theventricular septum and anterior wall of theleft ventricle (LV). The vessels that supply theremainder of the LV vary depending on thecoronary dominance, which we explain later.
RCA AnatomyThe RCA arises from the right coronary si-
nus somewhat inferior to the origin of theLCA. After its origin from the aorta, the RCApasses to the right of and posterior to the pul-monary artery and then emerges from underthe right atrial appendage to travel in the ante-rior (right) atrioventricular (AV) groove(Figs. 1 and 2). In about half of the cases, theconus branch is the first branch of the RCA(Fig. 3). In the other half, the conus branch hasan origin that is separate from the aorta. Theconus branch always courses anteriorly to sup-ply the pulmonary outflow tract. Occasionally,the conus branch can be a branch of the LCA(Fig. 3D), have a common origin with theRCA, or have dual or multiple branches.
In 55% of cases, the sinoatrial nodal artery(Figs. 3C, 3D, and 4A) is the next branch ofthe RCA, arising within a few millimeters ofthe RCA origin. In the remaining 45% ofcases, the sinoatrial nodal artery arises fromthe proximal left circumflex (LCx) artery(Figs. 4B and 11). In either case, the sinoatrialnodal artery always courses toward the supe-rior vena cava inflow near the cephalad aspectof the interatrial septum. As the RCA travelswithin the anterior AV groove, it coursesdownward toward the posterior (inferior) in-terventricular septum. As it does this, theRCA gives off branches that supply the RVmyocardium; these branches are called “RVmarginals” or “acute marginals” (Fig. 5).They supply the RV anterior wall. After itgives off the RV marginals, the RCA contin-ues around the perimeter of the right heart inthe anterior AV groove and courses toward thediaphragmatic aspect of the heart.
Coronary DominanceThe artery that supplies the posterior de-
scending artery (PDA) and the posterolateralbranch determines the coronary dominance. Ifthe PDA and PLB arise from the RCA, then thesystem is said to be right dominant (80–85% ofcases) (Figs. 6 and 7). In this instance, theRCA supplies the inferoseptal and inferior seg-ments of the LV [6]. If the PDA and PLB arisefrom the LCx artery, then the system is said tobe left dominant (15–20% of cases) (Figs. 8and 17). In this instance, the LCA supplies the
inferoseptal and inferior segments of the LV. Ifthe PDA comes from the RCA and the PLBcomes from the LCx artery, the system iscodominant (about 5% of cases) (Fig. 9).
In left-dominant and codominant systems,the LCx artery continues in the posterior AVgroove as the left AV groove artery and givesrise to left PLB. In left dominance, the PDA isthe final branch of the AV groove artery. Thedistal RCA divides into the PDA and PLB ina right-dominant system. The nondominantsystem is usually noticeably smaller in caliberthan the dominant system. This difference incaliber can be used as an additional clue to de-termine whether the coronary anatomy isright or left dominant. Usually arising justdistal to the origin of the PDA, the AV nodalartery (Fig. 6) can be recognized by its directvertical course off of the distal RCA. In casesof left dominance, the AV node branch has asimilar appearance and location, but it arisesjust proximal to the (left) PDA.
LCA AnatomyThe LCA normally emerges from the left
coronary sinus as the left main (LM) coronaryartery (Fig. 10). The LM coronary artery isshort (5–10 mm), passes to the left of and pos-terior to the pulmonary trunk, and bifurcatesinto the left anterior descending (LAD) andLCx arteries (Fig. 11). Occasionally, the LMcoronary artery trifurcates into the LAD ar-tery, the LCx artery, and the ramus interme-dius artery (Fig. 12).
Ramus Intermedius ArteryThe most common variation in LCA anat-
omy is the presence of a trifurcation of the LMcoronary artery. In this instance, the LM coro-nary artery trifurcates into the LAD artery, LCxarteries, and an artery between them called the“ramus intermedius” artery (Fig. 12). The ra-mus intermedius artery itself has variablebranching. The ramus intermedius can be dis-tributed as a diagonal branch or as an obtusemarginal branch depending on whether it sup-plies the anterior or the lateral wall, respectively.
LAD ArteryThe LAD artery (Fig. 13) runs in the ante-
rior interventricular sulcus along the ventricu-lar septum. Commonly, the LAD artery may beembedded within the anterior myocardiumforming an overlying myocardial bridge(Fig. 14). Myocardial bridging is seen more of-ten on CT than described in the coronary an-giography literature. Most myocardial bridgesare asymptomatic, although rarely myocardial

CT Angiography of Coronary Arterial and Venous Anatomy
AJR:188, June 2007 1667
bridging can be associated with ischemia. TheLAD artery has branches called “septal perfo-rators” (Fig. 14) that supply the anterior ven-tricular septum. It also has diagonal arteries(Fig. 15) that course over and supply the ante-rior wall of the LV. The diagonals and septalperforators are numbered sequentially fromproximal to distal (i.e., D1, D2, S1, S2).
LCx ArteryThe LCx artery (Figs. 16, 17, and 2, 4B, 8,
11, 12, 15) runs in the posterior AV groove anal-ogous to the course of the RCA on the oppositeside. The major branches of the LCx artery con-sist of obtuse marginals (OMs) (Figs. 16 and17). OM branches supply the lateral wall of theLV. They are numbered sequentially from prox-imal to distal (i.e., OM1, OM2, OM3).
Anomalies of RCA OriginThe RCA can have an anomalous origin. It
is important to be aware of this possibility toavoid misinterpreting coronary CTA. Typi-cally, the anomalous origin of the RCA isfrom the left coronary sinus of Valsalva, witha subsequent course between the aortic rootand right ventricular outflow tract. Depictionof these anomalies is beyond the scope of thisarticle; however, this and other anomalies ofRCA origin are described by Kim et al. [7].An example of an anomalous origin of theRCA is shown in Figure 18.
Anomalies of LCA OriginThe LCA and its branches can have an
anomalous origin. It is important to be awareof this possibility to avoid misinterpretingcoronary CTA. Some of these anomalies areassociated with an increased risk of suddendeath or cardiac arrest (Fig. 18C). Depictionof these anomalies is beyond the scope of thisarticle; however, anomalies of LM, LAD, andLCx origin are reviewed by Kim et al. [7].
Coronary Venous AnatomyThe great cardiac vein (Figs. 4B and
16A) is located in the anterior interventric-ular sulcus, alongside the LAD artery. Itcourses upward from the apex and drainsinto the coronary sinus. The middle cardiac
vein (Figs. 7A and 7C) also begins at theapex, but it courses upward in the inferiorinterventricular sulcus, alongside the PDA.Between the two, there is a variable poster-olateral vein (Fig. 7C) draining the lateralwall of the LV. The coronary sinus(Figs. 7A, 7C, 16A, and 16B) is the widevein that courses in the posterior AV grooveaccompanying the LCx artery and the AVgroove artery. It drains into the right atriumand receives the great cardiac vein proxi-mally and the middle cardiac vein distally.
Reporting System of Coronary Artery Disease
In an attempt to standardize the reportingof coronary artery disease, an ad hoc commit-tee of the American Heart Association devel-oped nomenclature and further divided themain coronary arteries into proximal, middle,and distal segments [8].
The proximal RCA segment is from theostium to one half the distance to the acutemargin of the heart. The middle RCA seg-ment is the RCA from the end of the abovesegment to the acute margin of heart. Thedistal RCA segment is the RCA runningalong the right AV groove from the acutemargin to the origin of the PDA.
The LAD proximal segment is proximalto and includes the origin of the first majorseptal perforator. The middle LAD segmentis the LAD artery immediately distal to theorigin of the first major septal perforatorthat extends to the point where the LAD ar-tery forms an angle (right anterior obliqueview). This angle is often, but not always,close to the origin of the second diagonal. Ifthis angle or diagonal is not identifiable, thissegment ends one half the distance from thefirst major septal perforator to the apex. Theapical LAD segment is the terminal portionof the LAD artery that begins at the end ofthe previous segment and extends to or be-yond the apex.
The proximal LCx segment is the main-stem of the LCx artery from its origin off theLCA to and including the origin of an obtusemarginal. The distal LCx segment is the LCxartery distal to the origin of the obtuse mar-
ginal and travels along or close to the poste-rior AV groove.
ConclusionCoronary CTA is emerging as an essential
imaging tool for evaluating the coronary ar-teries. Knowledge of the CT appearance ofthe coronary anatomy and various coronaryartery anomalies is essential for accurate di-agnosis and proper patient treatment.
References1. Green CE. Coronary cinematography. Philadel-
phia, PA: Lippincott-Raven, 1996
2. Soto B, Russell RO, Moraski RE. Radiography
anatomy of the coronary arteries: an atlas. Mount
Kisco, NY: Fitura Publishing, 1976
3. Raff GL, Gallagher MJ, O’Neil WW, Goldstein JA.
Diagnostic accuracy of noninvasive coronary an-
giography using 64-slice computed tomography. J
Am Coll Cardiol 2005; 46:552–557
4. Vrachliotis TG, Bis KG, Hardary A, et al. Enhance-
ment of coronary, aortic and pulmonary vasculature
using biphasic single-injection 64-slice CT: angiog-
raphy protocol in emergency department patients
with atypical chest pain. Radiology (forthcoming,
May 2007)
5. Jakobs TF, Becker CR, Ohnesorge B, et al. Mul-
tislice helical CT of the heart with retrospective
ECG gating: reduction of radiation exposure by
ECG-controlled tube current modulation. Eur
Radiol 2002; 12:1081–1086
6. Cerqueira MD, Weisman NJ, Dilsizian V, et al.
Standardized myocardial segmentation and nomen-
clature for tomographic imaging of the heart. A
statement for healthcare professionals from the Car-
diac Imaging Committee of the Council on Clinical
Cardiology of the American Heart Association.
Circulation 2002; 105:539–547
7. Kim SY, Seo JB, Do KH, et al. Coronary artery
anomalies: classification and ECG-gated multi-de-
tector row CT findings with angiographic correla-
tion. RadioGraphics 2006; 26:317–334
8. Austen WG, Edwards JE, Frye RL, et al. A report-
ing system on patients evaluated for coronary artery
disease: Report of the Ad Hoc Committee for Grad-
ing of Coronary Artery Disease, Council on Car-
diovascular Surgery, American Heart Association.
Circulation 1975; 51[suppl 4]:5–40

Kini et al.
1668 AJR:188, June 2007
Fig. 1—Anterior schematic diagram of heart shows course of dominant right coronary artery and its tributaries. AV = atrioventricular, PDA = posterior descending artery, RCA = right coronary artery, RV = right ventricular, SA = sinoatrial.
A B
Fig. 2—CT images of normal heart in 53-year-old man. Ao = aortic root, CS = coronary sinus, LA = left atrium, LAD = left anterior descending artery, LCx = left circumflex artery, LM = left main coronary artery, LV = left ventricle, PDA = posterior descending artery, RA = right atrium, RCA = right coronary artery, RV = right ventricle, RVOT = right ventricular outflow tract.A, Axial 5-mm maximum-intensity-projection (MIP) image shows left main coronary artery as it arises from left coronary cusp.B, Axial 5-mm MIP image shows right coronary artery as it arises from right coronary cusp inferior to level of beginning of left main coronary artery.C, Axial 5-mm MIP image shows course of right coronary artery within anterior atrioventricular groove. Left anterior descending artery is shown within anterior interventricular groove, and left circumflex artery is shown in posterior atrioventricular groove.D, Axial 5-mm MIP image shows origin of posterior descending artery from distal right coronary artery.
C D

CT Angiography of Coronary Arterial and Venous Anatomy
AJR:188, June 2007 1669
A B
Fig. 3—Conus branch anatomy variations. Ao = aortic root, LA = left atrium, LAD = left anterior descending artery, LM = left main coronary artery, LV = left ventricle, RA = right atrium, RCA = right coronary artery, RVOT = right ventricular outflow tract, SAN = sinoatrial node branch.A, Left anterior oblique 5-mm maximum-intensity-projection (MIP) image shows conus branch (arrow) in 44-year-old woman as it arises separate from right coronary artery off of right coronary cusp.B, Left anterior oblique 15-mm MIP image shows common origin of conus branch (arrow) and right coronary artery in 40-year-old man. C, Axial 10-mm MIP image shows conus branch (arrow) arising from proximal RCA in 52-year-old man. It then courses anteriorly toward right ventricular outflow tract.D, Axial 10-mm MIP image shows conus branch (arrow) arising from left anterior descending artery in 46-year-old man.
C D
A B
Fig. 4—Sinoatrial node branch variations. Ao = aortic root, D1 = first diagonal, GCV = great cardiac vein, LA = left atrium, LAD = left anterior descending artery, LCx = left circumflex artery, LM = left main coronary artery, OM1 = first obtuse marginal, RCA = right coronary artery, RVOT = right ventricular outflow tract, SVC = superior vena cava.A, Axial 10-mm maximum-intensity-projection (MIP) image in 64-year-old man shows large sinoatrial node branch (arrow) as it arises from proximal right coronary artery. It then courses posteriorly toward cephalad aspect of interatrial septum (arrowheads) posterior to inflow of superior vena cava.B, Axial 10-mm MIP image shows sinoatrial node branch (arrow) in 65-year-old woman as it arises from proximal left circumflex artery: Sinoatrial branch still courses toward cephalad aspect of interatrial septum.

Kini et al.
1670 AJR:188, June 2007
A B
Fig. 5—Marginal branch anatomy. F = foot, LAD = left anterior descending artery, LV = left ventricle, RCA = right coronary artery, RV = right ventricle.A, Right anterior oblique 10-mm maximum-intensity-projection (MIP) image shows large marginal branch (arrow) arising from right coronary artery (RCA) in 40-year-old woman. B, Right anterior oblique volume-rendered image shows marginal branch (arrow) of RCA as it courses over right ventricle in 45-year-old woman.
Fig. 6—Distal right coronary artery anatomy in 34-year-old man. Left anterior oblique 20-mm maximum-intensity-projection image shows course of entire right coronary artery. Distally, posterior descending artery and posterior lateral branch are shown, as is atrioventricular node branch. Ao = aortic root, AVN = atrioventricular node, IMB = inferior marginal branch, LCx = left circumflex artery, LV = left ventricle, PDA = posterior descending artery, PLB = posterior lateral branch, RCA = right coronary artery, RVOT = right ventricular outflow tract.
A B C
Fig. 7—Distal dominant right coronary artery variation on axial projections. CS = coronary sinus, LV = left ventricle, MCV = middle cardiac vein, PDA = posterior descending artery, PLB = posterior lateral branch, PLV = posterolateral vein, RA = right atrium, RCA = right coronary artery, RV = right ventricle.A, Axial 10-mm maximum-intensity-projection (MIP) image in 51-year-old man shows typical tortuous course of posterior descending artery as it arises from distal right coronary artery. Posterior descending artery travels in inferior interventricular groove along side middle cardiac vein. Posterior lateral branch continues along distal coronary sinus to supply inferior wall.B, Axial 10-mm MIP image shows dual posterior descending arteries and dual posterior lateral branches in 44-year-old man.C, Axial 3D volume-rendered projection image shows origin of posterior descending artery, which still courses toward middle cardiac vein, is higher than normal in 49-year-old woman.

CT Angiography of Coronary Arterial and Venous Anatomy
AJR:188, June 2007 1671
A B C
Fig. 8—Dominant left circumflex artery and posterior descending artery anatomy. Ao = aortic root, AVGA = atrioventricular groove artery, CS = coronary sinus, LA = left atrium, OM = obtuse marginal, PDA = posterior descending artery, PLB = posterior lateral branch, RA = right atrium, RCA = right coronary artery.A and B, Left anterior oblique 10-mm maximum-intensity-projection (MIP) images show two examples of dominant left circumflex artery anatomy with typical small nature of right coronary artery: one in 43-year-old woman (A) and one in 44-year-old man (B). Atrioventricular groove artery descends as larger-caliber artery in posterior atrioventricular groove subjacent to coronary sinus.C, Axial 10-mm MIP image shows dual posterior descending arteries as they arise from distal atrioventricular groove artery in 44-year-old man with dominant left circumflex artery.
Fig. 10—Dominant left coronary artery anatomy. Left anterior oblique schematic diagram of dominant left coronary artery anatomy, including left anterior descending artery and left circumflex artery tributaries, is shown. AVGA = atrioventricular groove artery, PDA = posterior descending artery.
Fig. 9—Codominance. Axial 10-mm maximum-intensity-projection image reveals codominant anatomy in which posterior descending artery arises from right coronary artery and posterior lateral branch arises from distal left circumflex artery in 33-year-old man. LV = left ventricle, PDA = posterior descending artery, PLB = posterior lateral branch, RCA = right coronary artery, RV = right ventricle.

Kini et al.
1672 AJR:188, June 2007
Fig. 11—Left main coronary artery bifurcation. Anterior caudal 10-mm maximum-intensity-projection image displays typical bifurcation of left main coronary artery into left anterior descending and left circumflex arteries in 47-year-old man. AVGA = atrioventricular groove artery, D1 = first diagonal, LAD = left anterior descending artery, LCx = left circumflex artery, LM = left main coronary artery, OM1 = first obtuse marginal, SAN = sinoatrial node branch.
A B C
Fig. 12—Ramus intermedius anatomy. LAD = left anterior descending artery, LCx = left circumflex artery, LM = left main coronary artery, RI = ramus intermedius artery.A, Right anterior oblique caudal 10-mm maximum-intensity-projection (MIP) image displays trifurcation of left main coronary artery into left anterior descending artery, ramus intermedius artery, and left circumflex artery in 49-year-old man. B, Axial 10-mm MIP image shows left main coronary artery dividing into left anterior descending artery, left circumflex artery, and ramus intermedius branches in 42-year-old woman. C, Left posterior cranial 3D volume-rendered projection image shows branching ramus intermedius artery, which is mostly distributed as obtuse marginal branch to lateral wall, in 52-year-old man.
Fig. 13—Left anterior descending artery course. Right anterior oblique 10-mm maximum-intensity-projection image reveals entire course of left anterior descending artery within anterior interventricular groove in 44-year-old woman. Distally, it is seen wrapping around left ventricular apex (arrows). LA = left atrium, LV = left ventricle.

CT Angiography of Coronary Arterial and Venous Anatomy
AJR:188, June 2007 1673
A B
Fig. 14—Myocardial bridge and septal perforator branch anatomy in 39-year-old woman. LA = left atrium, LAA = left atrial appendage, LV = left ventricle, S1, S2, S3 = first, second, and third septal perforators.A, Right anterior oblique 10-mm maximum-intensity-projection (MIP) image displays left anterior descending artery and septal perforator branches. Myocardial bridge overlies left anterior descending artery just beyond second septal perforator (arrows).B, Short-axis (left anterior oblique) 5-mm MIP image at level of myocardial bridge shows left anterior descending artery (arrow) deep to right ventricular myocardium junction with left ventricle.
A B
Fig. 15—Diagonal branch anatomy. D1 = first diagonal, D2 = second diagonal, LAD = left anterior descending artery, LCx = left circumflex artery, LM = left main coronary artery, LV = left ventricle, RI = ramus intermedius artery, SP = septal perforator branches.A, Axial caudal oblique 10-mm maximum-intensity-projection (MIP) image reveals two diagonal branches (D1 and D2) from left anterior descending artery in 55-year-old man. Diagonal branches course laterally, and small septal perforator branches course medially.B, Cranial left anterior oblique 10-mm MIP image shows left anterior descending artery and two diagonal branches in 47-year-old man.
A B
Fig. 16—Nondominant left circumflex artery anatomy in 36-year-old man. AVGA = atrioventricular groove artery, CS = coronary sinus, D1 = first diagonal, GCV = great cardiac vein, LAD = left anterior descending artery, LCx = left circumflex artery, OM1 = first obtuse marginal.A, Axial 10-mm maximum-intensity-projection (MIP) image shows left circumflex artery and left anterior descending artery with large first obtuse marginal arising from proximal left circumflex artery. Small left circumflex artery descends in posterior atrioventricular groove as atrioventricular groove artery.B, Left anterior oblique 10-mm MIP image displays left circumflex artery anatomy with its descent as atrioventricular groove artery.

Kini et al.
1674 AJR:188, June 2007
A B
Fig. 17—Dominant left circumflex artery anatomy in 44-year-old man. AVGA = atrioventricular groove artery, LCx = left circumflex artery, LM = left main coronary artery, OM1 = first obtuse marginal, OM2 = second obtuse marginal, PDA = posterior descending artery, PLB = posterior lateral branch, RI = ramus intermedius artery.A, Left anterior oblique cranial 3D volume-rendered image shows dominant left circumflex artery anatomy with two obtuse marginal branches.B, Axial 3D volume-rendered image reveals dual posterior descending artery and posterior lateral branch arising from distal atrioventricular groove artery.
A B C
Fig. 18—Anomalous origin of right coronary artery and left main coronary artery. Ao = aortic root, LAD = left anterior descending artery, LM = left main coronary artery, RCA = right coronary artery, RVOT = right ventricular outflow tract.A, Axial 5-mm maximum-intensity-projection (MIP) image shows anomalous origin of right coronary artery in 43-year-old woman from anterior proximal ascending aorta with subsequent acute rightward course before reaching anterior atrioventricular groove.B, Three-dimensional volume-rendered projection image shows anomalous right coronary artery in same patient as A above level of right coronary cusp (arrow).C, Axial 10-mm MIP image reveals anomalous origin of left main coronary artery in 35-year-old man from right cusp near origin of right coronary artery. It then takes intraseptal course posterior to right ventricular outflow tract near cephalad aspect of interventricular septum.
F O R Y O U R I N F O R M A T I O N
This article is available for CME credit. See www.arrs.org for more information.