Coronary Artery
-
Upload
cardiacinfo -
Category
Documents
-
view
1.239 -
download
4
description
Transcript of Coronary Artery

Cardiac Services
Barts and The LondonNHS Trust
Coronary ArteryYou and Your Heart
Bypass Surgery

This booklet has been written to help you and your family/carers
to understand
• more about coronary artery bypass surgery
• how to prepare for your operation
• your stay in hospital
• your recovery
• the benefits of cardiac rehabilitation.
ContentsPart one Your operation 2
Part two Preparing for your operation 6
Part three In hospital 10Your stay in intensive care 12
Part four Your recovery 15Congestion charges 29
Part five The benefits of cardiac rehabilitation 32
Part six Useful telephone numbers and directions 34
Part seven Cardiothoracic audit 39
Donation of tissue for research 40
Trust data protection statement 40
There is another booklet available entitled ‘You and Your Heart’ whichexplains• how your heart works• how to look after your heart.
If you don’t have a copy, please ask your nurse for one or phone 020 8983 2357 to request a copy.

Part one
Your operation
What are the coronary arteries?
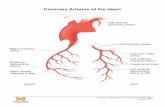
The heart is a muscular pump that sits in the centre of the chest.Although the heart pumps blood, which is rich in oxygen, around thebody, the heart muscle itself needs its own blood supply. It gets thisfrom a network of blood vessels called coronary arteries.
The two main coronary arteries are called the right and left arteries.The left coronary artery divides into two, one part goes to the back ofthe heart (circumflex artery), the other part goes to the front (leftanterior descending (LAD)) giving the impression of three arteries.(See diagram.) Each artery is about 3-4mm wide and spreads out, likethe branches of a tree, into smaller arteries across the heart so that allparts of the heart muscle receive blood.
These arteries can become narrowed or blocked. If this happens theheart muscle doesn’t receive enough blood and oxygen. The pain ordiscomfort that follows is called angina. This pain can be felt asdiscomfort, tightness, or breathlessness and may be felt in the chest, inone or both arms, in the shoulders, in the neck or in the jaw.
2
Aorta
Right coronaryartery
Circumflexartery
Left maincoronary artery
Front view of the heart
Left anteriordescendingcoronary artery

Angina can happen at any time. Strenuous activity like exercise,excitement, anger and cold weather can bring it on. Resting mayrelieve your angina symptoms. You may also need to use a GTN tablet or spray. These usually actquickly to relieve an angina attack. The usual dose is one or two spraysor one tablet under your tongue. (See Angina pain on page 24, ‘Youand Your Heart’ booklet.) You can ask your nurse for a copy.
What is a coronary artery bypass graft?
A coronary artery bypass graft is an operation that is performed toimprove the blood flow to your heart. A blockage or a narrowing inone or more coronary arteries is bypassed. A vein or part of a vein isusually taken from your leg, and in many cases, an artery from yourchest wall, called the internal mammary (thoracic) artery (IMA), isused. Occasionally an artery from the arm, called the radial artery, canbe used. The vein or artery used creates a new route for blood to passthrough and is called a bypass graft. The original coronary arteries arenot removed. There would be no benefit in doing this as it could causedamage to the heart muscle.
3
Internal mammaryartery (branch of aorta)
Aorta
Vein graftfrom leg

The benefit of the bypass operation is that it increases the bloodsupply to the heart muscle. After the operation most people will berelieved of angina. A few people may still experience occasional angina, but this willusually be less severe than they experienced before. If this happensplease let your doctor know.
This operation is not a cure, so it’s important that you reduce the riskof further progression of disease (narrowing) of the coronary arteriesby • not smoking • eating a healthy diet• watching your weight • exercising daily• keeping diabetes under control if you have this condition• taking your medication as prescribed• asking your GP/practice nurse to check your blood pressure and your
cholesterol levels regularly• attending a cardiac rehabilitation course.
The ‘You and Your Heart’ booklet contains useful information on howto look after your heart and some helpful advice on risk factors.
Carotid endarterectomy
Very occasionally you many need to have a carotid endarterectomybefore your bypass operation. This operation is done if your carotidartery/arteries are narrowed or blocked by fatty deposits (calledplaques). These arteries take blood to the head/brain.
4
Site of carotidendarterectomy

The operation helps to reduce the risk of a stroke/cerebral vascularaccident (C.V.A.) in people who are at greater risk during a bypassoperation. It is often performed under a local anaesthetic.
To find out if you have a narrowing or blockage a doctor or pre-admission nurse will examine your neck. If necessary a Doppler Scanwill be arranged. This is done by using a simple ultrasound machine totake special images of the arteries in the neck.
To do this operation the surgeon makes a cut in your neck, opens theblocked artery, removes the fatty deposits, and stitches the arteryclosed again.
5

Part two
Preparing for your operation
When you attend the outpatients department you will see a surgeonwho will put your name on a waiting list. In some cases you may begiven a date for your operation at this visit.
Pre-admission clinic
Approximately one to four weeks before your operation, yourAdvanced Nurse Practitioner (ANP) /clinic coordinator may telephoneyou to arrange an appointment to attend a nurse led pre-admissionclinic. Advanced Nurse Practitioners (ANP) are specialist nurses in heart andlung surgery. They are part of the team who will care for you fromyour first appointment with the surgeon until you are dischargedhome. Most patients will know the name of their ANP before theiradmission.
The purpose of this appointment is to
• identify any medical concerns which need to be addressed before your operation. If a problem is found, appropriate investigations and/or treatment will be arranged
• ensure that all the necessary preparations for your operation have been completed
• answer any questions you may have
• have all or some of the following tests performed:
Chest x-ray To look at the size, shape and condition of your heart and lungs.
Electrocardiogram (E.C.G.)To show the electrical activity of your heart.
Echocardiogram (Echo)To look at an ultrasound picture of your heart.
6

Blood testsTo check your blood count and kidney function.To identify your blood group and to prepare a blood transfusion incase it is needed during, or after, your operation.
Swabs for MRSASwabs will be taken from your nose, throat and groin area to check for MRSA.
Don’t worry if you haven’t been invited to attend a pre-admissionclinic as staff will visit you on the ward and give you any informationyou need. All necessary investigations/tests will be carried out whenyou come into hospital.
If you have any questions about your treatment or care, please contactyour ANP at The London Chest Hospital or at St Bartholomew’sHospital. Please find contact details at the back of this booklet.
Patient activity managers, in conjunction with your surgeon, ANP andsecretary, are responsible for planning surgical admissions. You willfind their contact details at the back of this booklet.
7

Dental care
If you have loose or decayed teeth please ensure that you have visitedyour dentist before your operation. This is to enable your anaesthetistto administer your anaesthetic safely.
What to bring into hospital
• wash bag with toiletries • dressing gown• slippers/comfortable shoes• night-dresses/pyjamas• towels• tissues• your medicines• money for newspapers, telephone calls and your journey home• spectacle case if you wear glasses• hearing aid and spare batteries, if applicable.
Please do not bring large sums of money or valuables into hospitalwith you.
8

Going home
In general, most patients are discharged home within a weekfollowing their operation. If possible, try to have someone to stay withyou for the first seven to 10 days. If this is not possible please tell yournurse when you attend the pre-admission clinic and/or on the day youare admitted to hospital.You will not be discharged home if you need nursing care withoutappropriate arrangements being made with the district nursingservice.
You should arrange your own transport and be accompanied home bya relative or friend. We can only supply transport home in exceptionalcircumstances.
9

Part three
In hospital
Hospital staff who will visit you before your operation
When you arrive on the ward, a nurse will greet you and will showyou around.
A doctor will visit you. He/she will examine you and ask about yourillness and answer any questions you may have. The operation will beexplained to you and the benefits and risks involved will be discussedwith you. You will be asked to sign a consent form, which gives yourpermission for the operation to be carried out. You will be given acopy of this form.
You may also be asked, at this time, to consent to samples of yourtissue to be taken and used for research. Please see ‘Donation of tissuefor research’ on page 38 for more information.
Benefits
The benefits of this operation are to increase your life expectancy, torelieve/improve your symptoms and to reduce the likelihood of a heartattack.
Risks
Minor problems, such as wound or chest infections, may occur. Thoughunlikely the most serious risks associated with this operation are deathand stroke. The surgeon will discuss your individual risks with youbefore you sign your consent form.
The ward nurse will give you any further information you may need tohelp prepare you and your family/carers for your operation. They willgive you advice about your immediate recovery, help you to plan foryour discharge home and rehabilitation.
10

An anaesthetist will visit you. He/she is the person who will give you ageneral anaesthetist and help to look after you during your operationand afterwards in the intensive care unit. Your suitability foranaesthesia will be assessed and you will be told about youranaesthetic.If you have any questions or concerns it is important that you speak toyour Advanced Nurse Practitioner, ward staff, your medical team orone of our cardiac education/rehabilitation team. It is important thatyou and your family understand what is happening to you and why itis happening.
Preparation for your operation
Before your operation you• may need to have some hair removed from your chest, your arms,
legs or all of these areas, using hair clippers, in preparation for your operation
• will be advised by your nurse when you need to stop eating and drinking.
On the day of your operation you may be given tablets or an injection,or both, to prepare you for your anaesthetic. These will help you tofeel relaxed and sleepy. After this you will be expected to stay in beduntil you go for your operation. You will be taken, either on a trolleyor on your bed, to the operating theatre and will be accompanied bythe ward nurse.On arrival in the operating theatre a theatre nurse or operatingdepartment assistant will meet you. The anaesthetist will then prepareyou for your anaesthetic by giving you an injection in the back of yourhand.
During your operation
During most heart operations a heart/lung bypass machine is used.This acts for the heart and lungs during the operation. Blood flowsthrough the machine where it receives oxygen and is then pumpedback to the body, thus bypassing the heart.
11

Your stay in intensive care
Immediately after your operation you will be transferred to theintensive care unit. This is where you will be cared for and closelyobserved, usually for six to 24 hours. After this time, you will usuallybe transferred to the high dependency unit or coronary care unit.
What to expect
You will be asleep to begin with and will be kept asleep withmedication/drugs. During this time you will be connected, by a tube,to an artificial breathing machine called a ventilator. This reduces thework that your lungs have to do in the first few hours during youroperation when you are sleeping. You will breathe through a tubewhich passes through your mouth and into your lungs. When you wake up, the tube may still be in place and you will not beable to talk or drink. You will be able to nod or shake your head inresponse to questions. A nurse will be with you at all times and he/shewill keep you comfortable. He/she is experienced in communicatingwith patients before they are able to speak.
The anaesthetist will decide when the breathing machine can bedisconnected. The breathing tube will be removed as soon as possible.After this, you will be given sips of water and you will be given anoxygen mask to wear to assist you with your breathing.
You will also be attached to a heart monitor. This records your heartrhythm, blood pressure, and temperature. The monitor may ‘bleep’occasionally, but don’t worry, this is to assist the nurse caring for you.
You may be aware of drips in your arms, neck or groin. These allowfluids and medicines to be given and blood samples to be takenwithout the need to continually pierce your skin.
You will also have a urine catheter (tube) in your bladder to allow youto pass urine without having to get out of bed. It also allows yournurse to measure the amount of urine you pass.
12

At the end of the operation, the surgeon will have inserted a numberof tubes into the area around your heart. These will drain away anyblood that may collect following your operation. You may also have adrain in your leg. These are usually removed on the first day after youroperation.
Pain relief after your operation
You will receive pain-relieving drugs through the drips both duringand after your operation. Initially the doctors or nurses give thesedrugs. As soon as you are awake, you may be given a device calledPCA (Patient Controlled Analgesia). This will allow you to control theamount of pain-relieving drug you receive. The PCA device has a safety mechanism which controls the amount ofthe pain relieving drug you are given, so you will not receive toomuch. If this device is used, a full explanation will be given to you. It isimportant that your pain is controlled so that you are able to coughand take deep breaths comfortably. Please tell your nurse if you haveany pain, as he/she will be able to adjust the dose of the drug youreceive. They can also contact the doctor to review your pain relief.
Telephone enquiries and visiting times
To allow the nursing staff to spend more time with you in Intensivecare we suggest that only one person from your family/carers phonesand enquires about your progress. They can then let others know howyou are getting on.
13

Your family/carers are welcome to visit you if they wish. The numberof visitors is limited to two at a time. The length of visits will dependon your condition. Children may visit at the discretion of thesister/nurse in charge of the unit.
Plants and fresh flowers are not allowed in the unit. This is because ofthe risk of infection from the flower water.
The London Chest HospitalThe unit is situated on the first floor. There is an intercom system inthe main hospital corridor. Visitors should press the buzzer and waitfor a member of staff to answer. All visitors should use the intercomsystem prior to visiting the unit.
Visiting is allowed at the discretion of the nursing staff. The directtelephone number is 020 8983 2209.
St Bartholomew’s HospitalThe unit is situated on the second floor (Queen Elizabeth II Building). There is a doorbell on the right hand side at the entrance to theIntensive Care Unit (ICU). Visitors should ring the bell and wait for amember of staff to answer before entering the unit.
Visiting is allowed at the discretion of the nursing staff. The directtelephone number is 020 7601 7728.
Please note these numbers are for the intensive care units only.
Ward numbers are at the back of this booklet.
After a stay in intensive care you may be transferred to a HighDependency Unit (H.D.U.) or Coronary Care Unit (C.C.U.), as you willnot need such close observation. The nurses who work in these areasare specially trained to meet your needs. You will stay there for one ortwo days. These areas provide specialist care for people who are notconnected to a breathing machine, but who still need closesupervision. This is normal after such an operation.From here you will be transferred to one of our wards, as you willrequire less supervision. Here the staff will monitor your progress andhelp prepare you for your discharge home.
Visiting on the wards is normally 3.00pm to 4.30pm and 7.00pm to8.30pm but please check with the individual wards. Children under theage of 12 years may visit at the discretion of the ward sister ifaccompanied by an adult.
14

Part four
Your recovery
Physiotherapy
Patients who have mobility or chest problems will be seen by aphysiotherapist if necessary. There will be a physiotherapist available ifyou require advice. Your nurse can arrange this for you.
Following your operation it is advisable to do breathing exercises. Youwill be encouraged to walk along the ward corridor. The besttreatment for you is to be up and mobile as soon as possible to helpprevent chest infections and to re-expand your lungs. By the time youare ready to leave hospital you should be walking independently.
Guidelines for your recovery
You may experience some pain or discomfort after your operation.Some people may have more pain than others. You will be givenregular pain relieving tablets and/or injections. If you still feel painafter your medication you must let your nurse or doctor know.
Pain is often worse in the morning after waking and when movingyour arms, shoulders and legs. We suggest you take your earlymorning pain relieving tablets before you get out of bed and regularlythroughout the day.You may also experience muscular aches and some soreness in yourneck, your back and bottom from lying in bed. It is not advisable to liein bed, or sit in a chair in one position, for long periods.
15

You may notice numbness and ‘pins and needles’ in your chest, legs orarms if an incision (cut) has been made.
If a vein has been taken from your leg(s), you may notice that the legfrom which it has been taken is more uncomfortable when walking.The ankle may be swollen. Sometimes it can be more painful thanyour chest wound. The length of vein needed can vary from ankle toknee or ankle to groin.
Aches and pains may persist for three months or longer. Muscular paincan sometimes be mistaken for angina. However, if angina re-occurs itis usually the same sensation/type of pain that you had before theoperation. If this happens, please let your General Practitioner (GP)know.
If you have had an internal mammary artery (I.M.A.) bypass graft, youmay be aware of a numb sensation, pins and needles or ‘twinges’ inyour chest. This is due to the way the operation is carried out. Thesefeelings may last for six months or more.
Controlling your pain after the operation
You are strongly recommended to take your pain-relieving tabletsregularly as prescribed by your doctor. Don’t wait until the pain issevere. It is not advisable to reduce or stop taking these tablets toosoon. They will not harm you when taken as prescribed. However,some pain-relieving tablets can cause drowsiness, in which case youshould not drive or use dangerous equipment/machinery.
You may also need to take a laxative for constipation. If this happensafter your discharge your pharmacist will advise you on what isavailable and best suited to you. When you feel ready, after yourreturn home, you can gradually reduce your painkillers from twotablets to one or as advised. If in doubt you can get advice from your GP or pharmacist. To helpreduce any pain when coughing, sneezing or laughing, support yourchest wound as you were shown whilst in hospital.
On discharge from hospital, you will be given a minimum of twoweeks’ supply of your tablets and a copy of your prescription. Afterone week, arrange to get a prescription for more tablets from your GP.
16

Consult your GP or your ANP if • you experience any sudden or severe pain in your chest• you develop pain in your calf muscle (at the back of either leg)• your wound becomes red, inflamed or discharging (weeping) pus.
If your GP is not available you can contact Accident and EmergencyDepartment at your local hospital. For more general enquiries contactthe ward on which you were a patient or your ANP.
It is advisable to visit your GP or practice nurse on a regular basis tohave your blood pressure checked.
Wound healing
After your operation, there will be a scar along the length of yourbreastbone on your chest. Depending on where the artery or vein hasbeen taken from, you may have a wound on your leg(s), arm or both.
At first you may notice some redness, bruising and perhaps a slightdischarge (weeping) from your wound. This discharge will often clearup within the first few days. You may also experience some soreness ornumbness around the wound area. The skin may feel tight. This is allquite normal.
A daily shower will keep your wounds clean and encourage healing.Don’t use soap or scented products on them. Pat them gently with aclean towel to dry.
17

When your wounds have healed, you may expose them to sunlight forshort periods only. It is advisable to use a sunscreen for yourprotection.
If you have diabetes, healing may take longer.
If you have had a vein taken from your leg, you may notice someswelling. Your ankles may also appear swollen. It is advisable to putyour feet up on a stool or chair when sitting down; this should beabove hip level. Don’t cross your legs, as this will reduce the bloodflow.
You will be given support stockings to wear, which will help to reduceswelling, support the wound and help reduce the risk of a blood clot(deep vein thrombosis). The stockings should be worn at all times forfour weeks. You may take them off for a half an hour while youwash/shower. Wash them, by hand, daily with a mild detergent, as thiswill help them stay clean and retain their elasticity.
Lifting weights/heavy loads
It is important that you don’t carry or lift anything that is heavier than5 kilograms or 10 pounds in weight for eight to 10 weeks followingyour operation. This is about the same weight as five bags of sugar (1 kilogram or 2 pound bags ). It takes eight to 10 weeks for thebreastbone to rejoin. Very occasionally you may notice a clicking noise in your breastbone. Ifthis happens contact the ward from where you were discharged oryour Advanced Nurse Practitioner.
18

Your heart beat
It is quite normal to be more aware of your heartbeat after theoperation. You may feel that it is beating irregularly or missing a beat.This often happens after a heart operation. Don’t worry. If thishappens whilst you are in hospital, let your nurse or doctor know. If ithappens when you are at home, contact your GP. If he/she is notavailable and you feel unwell, visit your local Accident and EmergencyDepartment.
If any of the problems mentioned occur, please contact your ANP whowill be happy to call you back. Please don’t think you are being anuisance, we are here to help you.
Medication
After your operation your surgeon will review, and may change, yourmedication. Any changes will be discussed with you before you gohome.
You will probably be advised to take Aspirin and/or Clopidrogel and acholesterol lowering drug (statin) on a long term basis, as this willreduce your risk of further cardiac events. For information on otherlong term heart medication please refer to the ‘You and Your Heart’booklet.
You may be discharged on painkillers and diuretics (water tablets) andwill be given a two week supply. After this your GP will review andadvise you on the need to stop or continue with these. Please refer tothe pain relief section on page 16 for more information.
WarfarinIn some cases your surgeon may prescribe Warfarin after youroperation to prevent blood clots.It may be prescribed if, for example, you have an irregular heart beat.It is given to thin your blood and slow down the time it takes for yourblood to clot. When you are discharged from hospital, you will begiven a booklet containing details of your blood test results andinformation on Warfarin.
If you have any questions or queries regarding your medication pleasespeak or contact your pharmacist, GP or ANP.
19

Diet and appetite
Following your operation it is normal to experience• nausea• lack of appetite• lack of taste.
Try to• eat little and often• eat what you fancy for the first two months after your operation• drink lots of water.
If you have diabetes or are on a special diet, please get advice fromthe dietitian.
Before you leave hospital
Before you leave hospital, you will be invited to attend a group talk,giving information and guidelines to follow when you are at home.This will take place on your ward and your family/carers areencouraged to attend.
Emotional adjustments
There may be times following your operation when you feel low ordepressed. You may be tearful, irritable and unable to concentrate.Often you will not be able to explain why you feel like this. Thesefeelings are known as the ‘post-op blues’ and may persist when youget home. Here are some suggestions to help you:
20

• Try to talk about your feelings with your family/carers. • Try to adopt a positive attitude, resume hobbies when you feel well
enough or take up new ones.• Take regular exercise (see ‘You and Your Heart’ booklet). • Rest and relaxation are also important for your recovery.
You may also be more aware of other emotions such as:• Anger and resentment—you feel that your body has let you down
despite efforts to keep fit. • Worry—due to changes in your body image, perhaps because of
your scar.• Frustration—that to start with your physical activities will be limited.• Fear—that you will need further surgery in the future.
If you experience any of these feelings whilst in hospital, the nursescaring for you are skilled in helping you through these difficulties. Youmay wish to talk to a member of our cardiac education/rehabilitationteam. When you are at home, you may need to talk to your GP, yourpractice nurse or your local cardiac education/rehabilitation nurse.
Resuming regular activities/taking regular exercise
GuidelinesDuring the first three months, you should try to increase youractivities. Introduce new activities gradually and not all at once.During the first few weeks after your operation it is normal to feeltired, after even the smallest amount of effort.
You should try to walk every day, gradually increasing the distanceand the pace. Wear warm clothing when outside on cold, wet orwindy days.
21

By six to seven weeks after your operation, you may be walking one totwo miles daily. This will depend on your previous fitness level, yourrecovery and any other medical conditions that you may have.
The first two to three days at homeTake regular walks around your home. Continue with deep breathingexercises. Get plenty of rest and don’t allow too many well wishers tovisit you, as this can be tiring.
During the first three weeks at home Introduce light tasks into your daily routine, eg light dusting, washingup, cooking light meals. It is recommended that you take daily walks.You may enjoy a quiet evening out.
Don’t do anything more strenuous at this stage. Avoid heavy lifting,pulling or pushing, as this will put a strain on your breastbone, whichwill take eight to 10 weeks to heal. Avoid activities that could causesudden jerking or twisting of your chest, eg walking a dog on a lead.
From four weeks after your operationYou can start to do more demanding tasks such as dusting, preparingvegetables, light shopping, light gardening, making tea/coffee.It is recommended that you walk for 20–30 minutes daily.
From six weeks after your operationIntroduce other tasks into your daily routine, such as hoovering,mowing the lawn with an electric mower, raking leaves, small carrepairs.
From eight weeks after your operation You may start cleaning the windows, cycling,fishing, playing bowls and practising your golfswing.
From twelve weeks after your operationYou should now feel that you are getting back tonormal. You may start to undertake morestrenuous exercise. If you wish to play competitivegames, consult your doctor first.
22

Returning to work
You should be able to return to work depending on the type of workyou do and on your recovery following your heart bypass operation.Most people will be able to return to their previous employment. Please discuss this with your doctors and your employers. You shouldnegotiate with your manager to work shorter hours and shorter weeksto start with.
Sexual relations
When you first return home, you may be worried about returning toyour usual sex life, and your partner may also feel anxious. It is normalto feel like this. Sexual activity can be resumed when you feel ready.Choose a position that you find comfortable and does not place strainon your chest.
In the beginning you may wish to take a less active role. Researchshows that the effort involved during sexual intercourse can becompared to climbing two flights of stairs.
If you suspect that the medication you are taking for your heart iscausing side effects, such as impotence (inability to develop/maintainan erection), you should consult your doctor, who may be able to alterthe dose/type of medication.
Driving
After your operation, your chest will take time to heal. Suddenmovements can bring on pain, soreness or discomfort. Remember thatstrong pain relieving tablets can cause drowsiness and can affect yourconcentration. You should inform your insurance company of the operation. Non-disclosure could render your insurance invalid.
Group one (ordinary) licenseYou don’t normally need to inform The Driver and Vehicle LicensingAgency (D.V.L.A.) if you have had a coronary artery bypass operation.Please see guidelines on page 25 as you may need to inform them ifyou have heart rhythm problems.
23

The D.V.L.A. recommends that you don’t drive for one monthfollowing your operation. In some cases, a longer period may benecessary for example experiencing persistent discomfort or if you aretaking strong painkillers.
If you have had a pacemaker implanted (a mechanical device thathelps control the rate at which your heart beats), you will need toinform them.
Don’t forget to wear a seat belt. Place a small cushion between yourchest and the seat belt if you find this helps to make it morecomfortable.
Group two licensePlease see guidelines for group II licenses.
If your job involves driving, talk to your employer or licensingauthority about conditions of returning to work.
If you are a taxi driver (Black Cab), the Public Carriage Office inLondon asks that you inform them immediately if you have had acoronary artery bypass operation. They would also like you to hand inyour badge, original and copy cab driver’s licence for safekeeping.
24

25
ANGINA
MYOCARDIALINFARCTION (MI)(Heart attack)
Driving must cease whensymptoms occur at rest,with emotion or at thewheel.Driving may recommencewhen satisfactorysymptom control isachieved.
DVLA need not benotified.
After MI, driving mustcease for at least 4/52.Driving may recommencethereafter provided thereis no other disqualifyingcondition.
After a non ST elevationMI, driving mayrecommence 1/52 aftersuccessful angioplasty,provided there is no otherdisqualifying condition.
DVLA need not benotified.
Refusal or revocationwith continuingsymptoms (treatedand/or untreated)Re-licensing may bepermitted thereafterprovided: • free from angina forat least 6/52• the exercise or otherfunctional testrequirements can bemet• there is no otherdisqualifyingcondition.
No driving for at least6/52. Re/licensing maybe permitted thereafterprovided:• the exercise or otherfunctional testrequirements can bemet• there is no otherdisqualifyingcondition.
Medical Condition Group I Group II(ordinary license) (eg PCV/LGV license)
DVLA guidelines which affect your fitness to drive(For complete dvla guidelines please seewww.dvla.gov.uk/medical/ataglance.aspx)

26
PERCUTANEOUSCORONARYINTERVENTION(Angioplasty ±stent)elective
SUCCESSFULCATHETERABLATION
PACEMAKERIMPLANT(includes boxchange)
Driving must cease for atleast 1/52.
Driving may recommencethereafter providedthere is no otherdisqualifying condition.
DVLA need not benotified.
Driving must cease for atleast 2/7.
Driving may bepermitted thereafterprovided there is noother disqualifyingcondition.
DVLA need not benotified.
Driving must cease for atleast 1/52.
Driving may bepermitted thereafterprovided there is noother disqualifyingcondition.
Disqualifies fromdriving for at least6/52.Re/licensing may bepermitted thereafterprovided:• the exercise or otherfunctional testrequirements can bemet• there is no otherdisqualifying condition.
Disqualifies fromdriving for 6/52.
Re/licensing may bepermitted thereafterprovided there is noother disqualifyingcondition.
Disqualifies fromdriving for 6/52.
Re/licensing may bepermitted thereafterprovided there is noother disqualifyingcondition.
Medical Condition Group I Group II(ordinary license) (eg PCV/LGV license)

27
HYPERTENSION
HEART FAILURE
DIabetes MellitusManaged by dietalone
Managed bytablets
Driving may continueunless treatment causesunacceptable sideeffects.
DVLA need not benotified.
Driving may continueprovided there are nosymptoms that maydistract the driver’sattention.
DVLA need not benotified.
Driving is allowed.Need not notify DVLA unless develop relevantdisabilities eg diabeticeye problems.
Driving is allowedprovided symptomsare controlled.
DVLA must be notified.
Disqualifies from drivingif resting BP consistently180 mm Hg systolic ormore and/or 100 mm Hgdiastolic or more.Re/licensing may bepermitted whencontrolled provided thattreatment does not causeside effects which mayinterfere with driving.
Disqualifies from drivingif symptomatic.Re/licensing may bepermitted provided: • the LV ejection fractionis = to or > 0.4• there is no otherdisqualifying condition.Exercise or otherfunctional testing maybe required dependingon the likely cause forthe heart failure.
Driving is allowed.Need not notify DVLA unless develop relevantdisabilities eg diabeticeye problems.
Driving is allowedunless develop relevantdisabilities eg diabeticeye problems.
DVLA must be notified.
Medical Condition Group I Group II(ordinary license) (eg PCV/LGV license)

28
DIabetes MellitusInsulin treated
Driving is allowedprovided symptomsare controlled.
Must recognisewarning symptoms ofhypoglycaemia andmeet required visual standards. 1, 2 or 3 year license.
DVLA must benotified.
New applicants on insulinor existing drivers arebarred in law fromdriving HGV or PCVvehicles from 1/4/1991.Drivers licensed before1/4/1991 on insulin aredealt with individuallyand licensed subject tosatisfactory annualconsultant assessment.
DVLA must be notified.
Medical Condition Group I Group II(ordinary license) (eg PCV/LGV license)

29
Holidays/Flying
A restful holiday in this country may be taken as soon as you feelready. Holidays abroad, by air, may be taken from eight weeks afteryour operation. Avoid strenuous holidays and long journeys at first.Remember to take a supply of your tablets with you in your handluggage. You must inform your travel insurers that you have had heartsurgery. British Heart Foundation can supply a list of insurance companies thatare sensitive to cardiac patients’ needs. There is no reason why you should not travel by air. If you have had apacemaker implanted, it can trigger off metal detectors at airports —carry your identity card with you.
Social workers
Illness and major surgery can cause severe disruption to family andworking life, or it may lead to changes in circumstances. Social workerscan offer advice and help on how to manage some of the effects ofillness or disability. Ask the nurse caring for you to arrange anappointment for you if needed.
Follow-up appointments
On leaving hospital you will be given or sent an appointment to seeyour surgeon—usually six to 12 weeks after your operation.
If you are unable to keep this appointment please ensure that youinform the appropriate department.
Congestion Charges
Congestion charging applies west of Aldgate East tube station. StBartholomew’s Hospital is within this area although patients /visitorsmay be exempt. For more info visit www.cclondon.com.

30
Your relative/friend should be independent on leaving hospitaland must be allowed to resume activities gradually. It isrecommended that, where possible, they have someone with themfor the first seven to 10 days after their discharge home.
It can take time to recover from the operation. Support andencourage them if they feel anxious or depressed. Visitors can betiring, however well meaning and caring, so you may want torestrict them.
It is normal to be anxious about the recovery of a loved one. Ifyou share a bed with someone who is/has been ill or has had anoperation, it is natural to be more aware of them. You may findyourself checking their breathing etc. This is all quite normal.Please remember the helpline service is for you too. You may alsowish to attend the cardiac rehabilitation course to help youunderstand the benefits and to aid the recovery of your lovedone.
Advice to your family/friends

Please use this page for any questions you may have or tomake notes.
31

32
Part five
The benefits of cardiac rehabilitation
Cardiac rehabilitation
After discharge from hospital it is advisable to attend a cardiacrehabilitation course at your local hospital. These courses are designedto be both informative and enjoyable.Please see the page 31 for the number of your local hospital. You cancontact your GP or the hospital concerned for details.
The aim of these courses is to help you resume your normal lifestyleand reduce the risk of ill health. They will help you regain confidenceand assist you to plan a healthy lifestyle programme.They will give you insight into• heart disease and how to manage it• exercising safely• introducing relaxation into your daily life.
Helpline service The cardiac rehabilitation nursing service is available to give you andyour family/carers advice and support.
Helpline numbers (9am to 5pm weekdays) are:
The London Chest Hospital 020 8983 2357
St Bartholomew’s Hospital 020 7601 7891
The Royal London Hospital 020 7377 7344
Whilst you are in hospital, be sure to discuss any queries or concernsyou may have with your nurse or doctor.
If, when you have read this booklet, you have any unansweredquestions, please don’t hesitate to contact either the CardiacRehabilitation Helpline or your Advanced Nurse Practitioner.

33
Cardiac Rehabilitation Programmes
The following hospitals offer cardiac rehabilitation programmes. If you wish to attend one of these centres please contact the hospitalconcerned, or your GP.
Rehabilitation CoordinatorHospitals Telephone Number
Basildon Basildon, Essex 01268 394078
Barnet Barnet, Middlesex 020 8216 4824
Broomfield Chelmsford, Essex 01245 516376
Chase Farm Enfield, Middlesex 020 8375 1887
Clacton Clacton, Essex 01255 201520
Colchester General Colchester, Essex 01206 742794
Great Western Swindon, SN36 01793 604268
Homerton Hackney, E9 020 8510 7642
King George’s Ilford, Essex 020 8970 8460
Newham General Plaistow, E13 020 7363 8422
North Middlesex Edmonton, N18 020 8887 4618
Princess Alexandra Harlow, Essex 01279 827548
Queens Romford, Essex 01708 435000 (ext.3223)
Royal London Whitechapel, E1 020 7377 7344
Southend General Southend on Sea 01702 385028
United Bath Bath, BH1 01225 825028
Whipps Cross Leytonstone, E11 020 8535 6749
Whittington Archway, N19 020 7288 5649

34
Part six
Useful telephone numbers and directions
The London Chest HospitalGround Floor
Outpatient’s Department (OPD) 020 8983 2249
First FloorIntensive Care Unit (ICU) 020 8983 2209High Dependency Unit (HDU) 020 8983 2288Coronary Care Unit (CCU) 020 8983 2354 Leander Ward 020 8983 2233
Second FloorRiviere Ward 020 8983 2341
Patient Activity Manager 020 7377 7000(Bleep 1932)
Pre-admission Clinic 020 8983 2272
Cardiac Rehabilitation 020 8983 2357
Customer Care Manager 020 7601 7811
Accommodation for Patients & Relatives 020 8983 2422(12:30 - 4.30pm)

35
The London Chest Hospital

36
St Bartholomew’s Hospital
Queen Elizabeth II Building
Ground FloorOut Patient’s Department (OPD) 020 7601 7697
Second FloorHigh Dependency Unit (HDU) 020 7601 7731Intensive Therapy Unit (ITU) 020 7601 7728
Third FloorVicary Ward 020 7601 7116
Fourth FloorHarvey Ward/Coronary Care Unit (CCU) 020 7601 7110
Patient Activity Manager 020 7601 8139 Pre-admission Clinic 020 7601 7579
Cardiac Rehabilitation 020 7601 7891
Customer Care Manager 020 7601 7811
Accommodation for Patients & Relatives 020 7601 7208(9am - 1pm)

37
St Bartholomew’s Hospital

38
Useful addresses and telephone numbers
Barts Hearts British Heart FoundationSt Bartholomew’s Hospital 14 Fitzhardinge Street West Smithfield London W1H 9DHLondon EC1 Tel: 020 7601 8132 Tel: 020 7935 0185
www.bhf.org.ukAn association of cardiac patients of St Bartholomew’s Hospital. .
British Diabetic Association Coronary Prevention Group10 Park Way 2 Taviton StreetLondon NW1 7AA London WC1 0BT
Tel: 020 7424 1000 Tel: 020 7927 2125www.diabetesuk.co.uk Provides information on diet,
exercise and stress for healthprofessionals and the public.
Driver and Vehicle Licensing QUITAgency (DVLA ) 211 Old StreetSwansea, SA99 1AR London EC1V 9NRTel: 01792 782341 QUITLINE: 0800 0022008.15am - 4.30pm (freephone)(Monday to Friday)
Information and advice forAsk for medical branch. smokers who want to stop.www.direct.gov.uk/motoring
NHS Smokers Helpline NHS DirectTel: 0800 1690169 Tel: 0845 4647 (local rate)
Information and adviceon healthcare.

39
Part seven
Cardiothoracic audit
During your stay at Barts and The London NHS Trust the cliniciansinvolved in your care will enter information about your operation intoour cardiac surgery audit database. This database consists of a set ofquestions from the Society of Cardiothoracic Surgeons (SCTS). Thisinformation is used to monitor clinical activity and forms part ofindividual Cardiothoracic Consultants yearly appraisals and could beused in cardiac research. This data is also used to calculate the figuresfor Barts and The London shown on the Healthcare Commission’s heartsurgery in Great Britain website.
http://heartsurgery.healthcarecommission.org.uk
The cardiac surgery database is managed by the Cardiac Informationand Audit team who adhere to the Data Protection Act (1998),Department of Health’s code of confidentiality and the CaldicottPrinciples.
Should you wish to discuss how your data is managed or you do notwant your data to be used for research purposes in the future thenplease contact the Cardiac Information and Audit Team using thedetails shown below. All research projects are approved by a ResearchEthics Committee.
Cardiac Information and AuditCardiac Audit Office1st Floor Dominion HouseSt Bartholomew’s HospitalWest SmithfieldLondonEC1A 7BE
Tel: 0207 601 8604Email: [email protected]

40
Donation of tissue for research
The human body is made up of collections of cells which make uptissues. During your treatment or operation, samples of tissue may betaken to help us plan your treatment or to understand your condition.This tissue can then be used for research; by studying tissue, scientistscan understand how diseases start and progress and may be able todevelop new treatments.
Your tissue can only be taken, kept and used for research with yourconsent. Consent will normally be taken at the same time as you giveyour consent for your operation or treatment. Your decision toconsent to, or to refuse, medical research will not affect the standardof care you receive.
The Human Tissue Act 2004 ensures that all tissue donated for researchis used in a safe and ethical manner. A Tissue Use Information Leaflethas been produced by the Barts and the London NHS Trust and wewould encourage you to read this before you make any decision.
For more information visit: www.bartsandthelondon.nhs.uk/research
Trust data protection statement
To enable us to improve the quality of the care that we provide, yourhealth records are kept by the Trust and may be used for teaching,training, audit and research. Further information on how the Trustuses your information can be found on our website athttp://www.bartsandthelondon.nhs.uk/forpatients/knowyourrights.asp.

This booklet has been revised and re-written by Cardiothoracic Nurses:Carmel McCallanPippa Duncan © Cardiac Services 2007