Deep vein thrombosis
-
Upload
madhur-anand -
Category
Health & Medicine
-
view
523 -
download
0
Transcript of Deep vein thrombosis
DEEP VEIN THROMBOSIS
DEEP VEIN THROMBOSIS
SALIENT FEATURES OF VENOUS THROMBOSISA semi-solid coagulum within venous system Occur in the superficial system K/a superficial thrombophlebitis or deep system k/a DVT DVT of leg complicated by immediate risk of pulmonary embolus and sudden death. Subsequently developing a post-thrombotic limb & venous ulceration DVT may occur in upper limb but not like leg
POST THROMBOTIC LEG
SMALL & GREAT SAPHENOUS VEIN
3 pairs of vene commitants accompanies 3 crural arteries ant. & post tibial & peroneal all joins to form popliteal vein along with soleal & gastronomieus veinthrough adductor hiatus enter into subsartorial canal as superficial femoral vein which recieve deep/profunda veins in femoral triangle to form common femoral vein and contineus as ext. Iliac vein below inguinal ligament
Deep vein anterior view
Deep vein posterior view
AetiologyVirchow triad are changes in vessel wall endothelial damage stasis, which is diminished blood flow through veins; coagulability of blood (thrombophilia).Most important factor: hospital admission for treatment of medical or surgical conditions
RISK FACTOR PATIENT FACTOR Age >60ObesityVaricose veinsImmobilityPregnancyPuerperiumHigh-dose oestrogen therapyPrevious deep vein thrombosis or pulmonaryembolismThrombophilia
Disease or surgical procedureTrauma or surgery, especially of pelvis, hipand lower limbMalignancy, especially pelvic, and abdominal (metastatic)Heart failureRecent myocardial infarctionParalysis of lower limb(s) infectionInflammatory bowel disease
Nephrotic syndromePolycythaemiaParaproteinaemiaParoxysmal nocturnal haemoglobinuriaantibody or lupus anticoagulantBehets diseaseHomocystinaemia
A thrombophilic cause should be sought in any patient presenting with an episode of venous thrombosis who gives a family history of deep vein thrombosis / in whom there is no other predisposing factorAlthough development of DVT is probably multifactorial, immobility (and hence stasis) remains one of the most important factors.
CAUSES OF HYPERCOAGULABILITY CongenitalDeficiency of antithrombin III, protein C / SAntiphospholipid antibody/ lupus anticoagulantFactor V Leiden gene defect/activated protein C resistanceDysfibrinogenaemias Acquired Antiphospholipid antibody or lupus anticoagulantHeparin induced thrombocytopenia
12
PATHOLOGY OF DVT1.A thrombus develops in soleal veins initially as a platelet aggregate. 2.Fibrin and red cells form a mesh until lumen of vein wall occludes3. Coralline thrombus then progresses as a propagated loose red fibrin clot containing many red cells 4.Extend up to next large venous branch possible for clot to break off pulmonary embolism
ORGANISED THROMBUS
CLINICAL DIAGNOSISMC presentation of a DVT is pain & swelling, especially in the calf usually in one lower limbBilateral deep vein thromboses are common up to 30 per cent. When swelling is bilateral DVT must be differentiated from other causes of systemic oedemaSome patients may first present with signs of a pulmonary embolism, e.g. pleuritic chest pain, haemoptysis and shortness of breath. Patients may also develop shortness of breath from chronic pulmonary hypertension.
May be white or cyanosed:- Phlegmasia alba dolens (edema increases to a level decrease tissue perfusion seen in pregnancy) Phlegmasia cerulia dolens(complete stasis of arterial &venous commonly in advanced malignancy)l/t venous gangrene
Clinical examination for DVTMild pitting oedema of the ankle, dilated surface veins, a stiff calf and tenderness over the course of the deep veins should be sought Leg pain occurs in about 50 % of patients with DVT but is non-specific Homans sign resistance (not pain) of the calf muscles to forcible dorsiflexion is not specific and should not be elicited. Tenderness occurs in 75 % of patients but is also found in 50 per cent of patients without objectively confirmed DVT
Clinical signs and symptoms of pulmonary embolism occur in about 10 per cent of patients with confirmed DVT. low-grade pyrexia present in a patient having repeated pulmonary emboli. Patients may have signs of cyanosis, dyspnoea, raised neck veins, a fixed split second heart sound and a pleural rub if they are having pulmonary emboli causing right heart strain, although these signs may be subtle or lacking
Diagnosis Diagnosis of DVT and pulmonary embolism should be established by special investigationsWHY:1.Sign & symptoms are nonspecific 2.t/t with anticoagulant is always a risk
Important features of clinical examination
MODIFIED WELLS CRITERIA
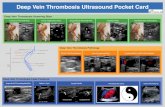
INVESTIGATIONSPatients present to an Accident and Emergency department with an idiopathic thrombosis have a d-dimer measurement . Greater than normal range there is no indication for further investigation if raised duplex compression ultrasound deep veins of limb are located and compressed Filling defects in flow and a lack of compressibility indicate the presence of a thrombosThis is accurate and reliable for femoral and popliteal clots but less certain in tibial vein clots.
Magnetic resonance venography is now as accurate as contrast venography.Pulmonary embolism diagnosed definitively by CT scan of the pulmonary arteries filling defects in pulmonary arteriesPulmonary angiography required if intervention is considered Radionucleotide imaging has now been superceded by CT.
DD OF DVTRuptured Bakers cyst Calf muscle haematomaRuptured plantaris muscleThrombosed popliteal aneurysm and arterial ischaemia.( Duplex scanning detect many of these conditions) The DD of pulmonary embolism includes myocardial infarction, pleurisy and pneumonia.
RISK GROUP DEVELOPING DVT
TREATMENT OF DVT low molecular weight heparin and rapidly anticoagulated with warfarin unless there is a specific contraindication. Warfarin started at a dose of 10 mg on day 1, 10 mg on day 2 and 5 mg on day 3. A taken on days 2 and 3 along with a warfarin guides the maintenance dose of warfarinThrombolysis considered with iliac vein thrombosis, especially seen early and limb is extremely swollen
Surgical venous thrombectomy, accompanied by an arteriovenous fistula attempted in patients with threatened venous gangrene and phlegmasia cerulia dolens. If performed, a venousPulmonary emboli treated by anticoagulation and observation Severe right heart strain &shortness of breath fibrinolytic treatment/ radiologically guided catheter embolectomy Cardiac arrest should undergo surgical pulmonary embolectomy.
HEPARIN DOSE ACCORDING TO BODY WEIGHT
BOLUS 80 units/kgINFUSION @ 18units /kg/hr
MEASURE aPTT AFTER 6hr IF aPTT70
REPEAT BOLUS & increase IV BY 4 units/kg/hr REPEAT BOLUS & increase IV BY 2 units/kg/hrCSTDECREASE IV BY 2units/kg/hrSTOP INFUSION FOR 1 hr REDUCE IV BY 3 units/kg/hr
WARFARIN DOSAGE ADJUSMENTSINRINTERVENTION