Deep vein thrombosis
-
Upload
orthoprince -
Category
Documents
-
view
1.006 -
download
5
Transcript of Deep vein thrombosis


VENOUS THROMBOEMBOLISM Composite term for DVT &PE
The presence of thrombus with in deep veins is termed as deep vein thrombosis
It is a life threatening condition that may lead to sudden death in the short term or long term morbidity due to the development of post thrombotic limb and venous ulceration

1846 virchow recognised association of thrombus in leg and PE.
1916 J McLean ,a medical student discovered heparin
1937 Heparin introduced to clinical practice.
Last 25 years significant progress made in our understanding of DVT.

CLASSIFICATION : PROXIMAL DVT :thrombus formed in veins
above the knee jt (femoral, iliac, popliteal) DISTAL DVT : those formed below the
knee jt (calf veins)

Venous thrombosis are difficult to recognize
clinically. The documented cases probably represent
only tip of the Ice Berg.SILENT KILLER

M:F 1.2:1 Age more than 40 years.VT occur in more than 50% of patient’s
having orthopaedic surgical procedures.10 to 20% of patient with idiopathic DVT
have or develop cancer.1/3rd to 1/4th patient having proximal DVT
may develop PE. About 10% of hospital deaths attributable
to PE (from DVT)

Calf vein - most common Ilio femoral - most symtomatic IVC - most lethal

Blood clots occurring in people sitting at the computer for prolonged periods of time.
AIR TRAVEL AND DVTUp to 1 out of 10 air line passengers develop small
asymptomatic blood clots. Due to hypoxia and reduced cabin pressure.VT occurs in patients regularly without any damaged
to the blood vessels.

VTE Risk StratificationPatient Factors: Clinical
Age Previous VTE Malignancy Advancing age Obesity Prolonged immobility Trauma Surgery (THR, TKR, HFS) Pregnancy/ postpartum Indwelling central venous catheter Thrombophilia Deficiency of anti-thrombin III Protein C or S
Contd...

Paralysis of lower limbs Polycythaemia Paraproteinaemia PNH Antibody or lupus anticoagulant Medical illness
◦ stroke◦ MI◦ CHF◦ pneumonia◦ COPD◦ infections◦ nephrotic syndrome◦ inflammatory bowel disease
Oral contraceptives Varicose veins

Pregnancy and postpartum period. Immoblisation longer than 3 days Major surgery in previous 4weeks Long air or car trips >4hrs in previous 4
weeks

Predisposing Factors :1. Stasis 2. Vascular damage3. Hyper coagulability Imbalance between thrombogenesis &
thrombolytic agents

1. Propagation2. Embolization3. Dissolution4. Organization & recanalisation ORGIN DVT usually originates from veins of
calf around the valve cusps or with in soleal plexus
A minority of cases occurs directly in ilio femoral veins

In practical terms the development of VT is best understood as activation of coagulation in areas of reduced blood flow.
Majority of calf vein thrombus dissolve completely.
Only 20% progress proximally.Propagation occurs before embolisation.

The process of adherence and organisation of venous thrombus does not begin until 5 to 10 days after thrombus formation.
This non adherent thrombus may propagate or embolise.
Propagation or organisation of venous thrombus destruction of valves & varying degree of venous outflow obstruction chronic venous insufficiency.

1. Fatal PE2. Non-fatal PE3. Post-thrombotic syndrome Rate of fatal PE in gen population >65yrs
is .003% In ortho pts (THR,TKR) it is 0.3% 10 fold increase in risk of having fatal PE

Consequence of recanalisation of major venous thrombus
Due to incompetence of valvesLong term morbidityCauses chronic edema &venous ulcers

Swelling/edema most specific sign unilateral Leg pain (50%) non specific Redness/erythema over the thrombus Tenderness(75%) calf or along the involved veins does not correlate size, site, extent Low grade pyrexia Signs and symptoms of PE

Pain or discomfort in leg on forceful dorsiflexion of foot with knee straight
Time honoured signPresent only in 10% of confirmed DVTHighly non-specificPresent in 50%of cases with out DVTMisleading signNo longer used

Pts with superficial thrombophlebitis with out coexisting varicose veins & with no other etiology (IV Catheter) are at high risk of having DVT (40%)
Pts with ST extending to sapheno-femoral jn are at high risk of associated DVT

Painful blue inflammation
PHLEGMASIA ALBA DOLENSPainful white inflammationMassive IVF thrombus with arterial spasm

In approximately 70% of patients with clinically suspected DVT, alternate diagnoses are ultimately found as follows:
ArthritisCellulitis, lymphangitisHematomaLymphedemaMuscle or soft tissue injuryNeurogenic painPostphlebitic syndrome Prolonged immobilization or limb paralysisRuptured Baker cystStress fractures or other bony lesionsSuperficial thrombophlebitisVaricose veins

D-DIMER STUDY D-dimer fibrin fragments are present in fresh fibrin clots
and fibrin dehydration products of cross linked fibrin. Monoclonal antibodies specific to D-dimer fragment are
used to differentiate fibrin specific clots from noncrosslinked fibrin and from fibrinogen. These specific attributes of the D-dimer antibodies account for their high sensitivity for venous thromboembolism.
Elevated in any medical condition where clots form. Rised in trauma, recent surgery, haemorrhage, cancer
and sepsis. It has high sensitivity and low specificity for VTE. Levels elevated in DVT for seven days. After clot organisation and adherence the levels
decrease.

Current evidence strongly supports the use of a D-dimer assay in the clinical algorithm of suspected DVT.
A negative D-dimer assay R/O DVT in patients with low-to-moderate risk (Wells DVT score <2).
All patients with positive D-dimer assay and all patient with a moderate-to-high risk of DVT ( Wells DVT score >=2) require a diagnostic study.

Protein S, protein C, anticromin III, factor V Leyden, prothrombin 20210A mutation, antiphospholipid antibodies and homocysteine levels can be measured.
investigations for these abnormalities are primarily indicated when DVT is diagnosed in patients younger that 35 years or when venous thrombosis is detected in unusual sites.

CONTRAST VENOGRAPHY Gold standard for DVT. Used when other test are inconclusive. It is either contra indicated or non diagnostic in as many as
20-25% of patients. Drawbacks : Allergic reactions, contrast induced DVT,
technical problems, inter observer variability and lack of availability.
It is replaced by non invasive studies as initial diagnostic test.

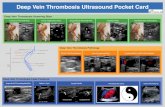
Combination of real – time ultrasonographic imaging with Doppler flow studies.
Sensitivity for proximal DVT is 97% for calf veins is 73%.
Overall specificity is 95%.Helpful to differentiate from
haematoma, baker cyst, abscess and other causes of leg pain and edema.

Primary disadvantage : Inherent inaccuracy in diagnosis of calf vein thrombosis.
Those proximal to the inguinal ligament are also difficult to visualize. Non occluding thrombi may be difficult to detect.
Not able to differentiate to old and new clots in patients with acute recurrent DVT.
Depends on experience of radiologist

Based on recording changes in blood volume of an extremity, which are directly related to venous outflow.
Sensitive and specific for proximal vein thrombosis.
Cannot differentiate between thrombotic occlusion and extra vascular compression of the vein.
Insensitive for calf vein thrombosis, non-occluding proximal DVT and ileofemoral DVT.

Increasingly used. Accuracy approaches to that of contrast
venograghy. Diagnostic test of choice for suspected iliac vein
& IVC thrombosis. 2nd &3rd trimester of pregnancy (gravid uterus
alters doppler flow characteristics). In suspected calf vein thrombosis it is more
sensitive than other non invasive study. Expense, lack of general availability and technical
issues limit its use.

Used for pelvis vein thrombosis.
NUCLEAR MEDICINE IMAGING STUDIES I125 labeled fibrinogen.Takes longer than 24 hrs.No longer used.

PRIMARY OBJECTIVES1. To prevent PE.2. Reduce morbidity.3. Prevent or minimize risk of developing the postphletic
syndrome.
SURGICAL TREATMENT 1. Indicated when anticoagulant therapy is ineffective,
unsafe or contraindicated. 2. Major surgical procedures : clot removal and partial
interruption of IVC to prevent PE.

To restore venous patency and valvular function. Alone it is not indicated because rethrombosis is
frequent. Heparin therapy is a necessary adjunct. Best reserved for patients with massive IF vein
thrombosis when limb viability is at risk.
FILTERS FOR DVT First suggested by Trousseau in 1868. Today introducing intracaval devices percutaneosly and
floating them into position with fluoroscopy is the procedure of choice for filter placement.

Severe hemorrhage complications of anticoagulant therapy.
Absolute contra indications to anticoagulation.
Failure of anticoagulation such us new or recurrent VTE or PE.

Bed rest Affected limb is elevated above the level of
heart.Anticoagulant prevent thrombus
propagation and allow the endogenous lytic system to operate
Pain relief.

Initial bolus 7500 to 10000 IU followed by continuous in infusion to 1000 to 1500 IU/hr.
Infusion rate adjusted so that aPTT is approx twice the control value
Every 6 hrs aPTT monitered till therapeutic range is reached
Duration :5 daysDiscontinue when platelet count <75,000

Effective and better than conventional heparin.
Different preparations available.Administered SC in fixed doses once or
twice daily.Duration -7 to 14 daysAnticoagulant effect by inhibiting the
activated factor X.Hemorrhagic complications doesn’t
occur

LMWHs are individual, distinct compounds that exhibit unique physical, pharmacokinetic and pharmacodynamic profiles
LMWHs exhibit distinct non-antithrombin III-mediated effects, including unique tissue factor pathway inhibition and von Willebrand factor release profiles.

Currently four LMWH are available.EnoxaparinTinazaparinDalteparinNadroparin
Only enoxaparin and tinazaparin are approved by FDA for DVT prophylaxis.

To be taken along with heparin for initial 4 to5 days.
Dose adj to maintain prothrombin time at INR 2.0 to3.0
Continued for 3 to6 months for pts with acute idiopathic DVT
For recurrent DVT/PE low intensity warfarin continued indefinitely maintaining INR 1.5 to2.0

Early administrationa) Prompt resolution of symptomsb) Accelerate clot lysisc) Preserve venous valvesd) Decrease the potential for developing
post-phlebitic syndrome

Does not prevent clot propagation or rethrombosis.
Heparin and oral anti coagulant therapy must follow a course of thrombolysis.
Haemorraghic complications reduced by regionally administering with flouroscopic control.
Streptokinase,urokinase,tPA (alteplase)

Lepirudin or aragatroban Used when heparin is contra indicated due
to HIT(heparin induced thombocytopenia)

LOW RISK: young pts ,minor illness, surgery lasting <30 mt with no risk factors
MODERATE RISK: >40yrs with deblitating illness undergoing major surgery but no risk factors
HIGH RISK: >40 yrs with serious medical condition undergoing major surgery with additional risk factors

YES - Overall reduction in DVT and PE is by 40% to 60%

Three pronged approach Designed to address stasis &
coagulation Usually combination of therapiesI. EARLY MOVT & REHABLITATIONII. MECHANICAL METHODS lower extremity exercises graded compression stockings

intermittent pneumatic compression devices
CPMIII PHARMACOLOGICAL PROPHYLAXISa) ASPIRIN easy to administer low cost few bleeding complications

Most commonly used Takes 36 hrs to start action Started day before surgery Low doses are used LOW MOLECULAR WT HEPARIN More effective than conventional Lesser bleeding

Low molecular wt heparinoid For pts with HIT
Fondaparinux Synthetic pentasaccharide

Graduated compression stockings Exercise Avoid alcohol &sleeping tabletsHIGH RISK PATIENTS LMWH ,single dose SC before the flight

PAGET VON SCHROTTER DISEASE Axillary and sub clavian vein thrombosis Reduced incidence Thoracic outlet synd &cervical ribs Thrombolytic therapy is treatment of
choice Since restoring venous patency more
important in upper limb

Early - Progression Pulmonary embolism Paradoxical embolism Acute compartment syndrome venous gangrene
Late - Rec DVT, Post phlebitic syndrome

Special group of pts very high risk for DVT & may reach up to 60 to
80% with out prophylaxis (THR) Assymptomatic DVT common in >50% of all
patients PE develop in 10 to 20 %of pts Even with prophylaxis DVT & PE remains the
most common cause for emergency readmission and death in joint replacement pts

•Pre-op Immobilization (stasis)
•Trigger of tissue factor
reamed products (THR)
tissue debris ,fat activation of
coagulation
• Distortion of Femoral and Poplietal viens
retraction,twisting,manipulation – damage to vessel wall
•Prolonged post-op Immobilization.

THR, TKR Hip fracture surgery Spine surgery [ malignancy, neurological
deficit]

Although thromboprophylaxis is routinely given to patients who undergo major orthopedic surgery, it is usually stopped at discharge.
Coagulation cascade remains abnormal upto 4 weeks.
Risk of propagation of the DVT, and PE, remains active during this period.
Patients undergoing THA TKA or HFS receive Thromboprophylaxis with LMWH Fondaparinux or VKA for a minimum of ten days. [can be cont. for 4 – 5 wks]

Not an uncommon condition in clinical practice DVT OCCURS ONLY IN POST-OP PATIENTS’ IS A MYTH Awareness is most important for early diagnosis Prompt treatment can prevent lethal
complications Diagnosis can be made using noninvasive
methods Long term follow up is necessary to identify
patients who develop chronic venous insufficiency.