Deep Vein Thrombosis
-
Upload
dr-nazeera -
Category
Health & Medicine
-
view
388 -
download
3
description
Transcript of Deep Vein Thrombosis

DEEP VEIN THROMBOSIS
History Taking

1) Do you have any pain or tender spots in your legs?
2) Have you noticed any new swelling in your legs?
3) Does the pain or swelling get worse when you stand, sit, or walk?
Classical symptoms of DVT include swelling, pain, warmth, and redness in the involved leg

4) Have you ever had a blood clot?
• People who had a history of previous DVT or
PE (Pulmonary Embolism) are more likely to
develop recurrent DVT and PE.

5) What medications are you taking?
Patient who are on oral contraceptive pill and hormone replacement
therapy which contain estrogen
Oestrogen causes the blood to clot slightly more easily, so your risk of
getting DVT is slightly increased.
First generation OCCP - lynestrenol.
Second generation pills - levonorgestrel or, less often, norgestrel.
Third generation pills - desogestrel or gestodene.

6) Have you had surgery recently?• As a patient, the risk of developing DVT depends on the type of treatment
they are having. Patient may be at higher risk of DVT if any of the
following apply:
1. Having an operation that takes longer than 90 minutes, or 60 minutes if
the operation is on the leg, hip or abdomen.
2. Having an operation for an inflammatory or abdominal condition such as
appendicitis.
3. Confined to a bed, unable to walk, or spending a large part of the day in a
bed or chair for at least three days.

7) Do any of your relatives have blood clotting problems?
• The risk of DVT is increased if patient have an inherited condition that
causes the blood to clot more easily than normal.
• These conditions include:
1. Cancer.
2. Heart and lung disease
3. Infectious diseases such as hepatitis
4. Inflammatory conditions such as rheumatoid arthritis
5. Thrombophilia (a genetic condition that makes your blood more likely to
clot) and
6. Hughes syndrome (when your blood becomes abnormally "sticky")

8) Have you been on any long trips recently?
• If patient are immobile (unable to move) for a long period of
time, such as during a long journey, their blood flow can slow
down considerably.
• Reduced blood flow to vein increase likelihood of blood cells
sticking together which causes clotting.

9) Have you had any recent injuries?
• Having a recent minor leg injury, was found to be associated with a
threefold increase in the risk of serious blood clots, such as deep
vein leg clots and pulmonary embolism (clots that travel to the
lung).
• Example :
1. Paralysis from a spinal cord injury
2. Broken hip or leg
3. Fracture

10) Do you have varicose veins?
• Varicose veins, because they occur in superficial
veins, are not generally linked to a serious condition
called deep vein thrombosis (DVT). However, with
severe varicose veins, there is a small increased
chance of developing DVT.

PHYSICAL EXAMINATION

Homan’s sign
• Homans's sign is often used in the diagnosis of deep venous thrombosis of the leg.
• A positive Homans's sign is thought to be associated with the presence of thrombosis.
• However, Homans's sign has a very poor predictive value for the presence or absence of deep vein thrombosis, like any other symptom or clinical sign of this disease.
• Other isolated clinical findings such as calf tenderness, swelling, and redness have been shown not to have diagnostic value for detecting DVT.

• To assess Homan’s sign, the patient’s knee is in an
extended position and the examiner forcefully
dorsiflexes the patient’s ankle
• A positive sign is indicated when pain in the popliteal
region and the calf is elicited as the foot is dorsiflexed.
• A negative Homan’s sign, on the other hand, doesn’t
automatically conclude an absence of DVT. Thrombosis
that develops in the thigh and pelvic veins are often
difficult to detect and patients can often remain
asymptomatic
• Homan’s test still remains an important tool for use in
the health care setting. Thus, it can be to our
advantage to apply Homan’s test in conjunction with
other detected clinical symptoms correlated with DVT
such as: unexplained fever or tachycardia, muscle pain,
tenderness, swelling, temperature change and venous
dilation

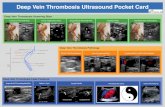
Wells Rule
• To rule out DVT
• The Wells Rule was used by the examining GP
to assess likelihood of DVT. Patients with a
high likelihood (Wells score >1) were referred
straight for ultrasound.

Clinical Decision Rule Developed by Wells and Colleagues29.
Riddle D L , and Wells P S PHYS THER 2004;84:729-735
Physical Therapy

• Score interpretation:
1. ≤0 =probability of proximal lower-extremity deep vein thrombosis
(PDVT) of 3%,
2. 1 or 2=probability of PDVT of 17%
3. ≥3=probability of PDVT of 75%
• Tenderness along the deep venous system is assessed by firm
palpation in the center of the posterior calf, the popliteal space, and
along the area of the femoral vein in the anterior thigh and groin.
• Most common alternative diagnoses are cellulitis, calf strain, and postoperative swelling.