Deep Vein Thrombosis
-
Upload
myra-snyder -
Category
Documents
-
view
27 -
download
0
description
Transcript of Deep Vein Thrombosis

DR. SRINIVAS RAJKUMAR THIRAVIARAJ

• DVT is the formation of thrombus deep veins predominantly in the legs

• Also
• Upper Limb
• Paget Schrotter Syndrome – Ax V Thrombosis• May Thurner Syndrome - LIV compression by
RIA

contents
• Importance• Anatomy • Pathophysiology• Risk Factors• Diagnosis• Management• Follow Up/ Complications• Prevention

Venous thromboembolism (VTE),
• Deep venous thrombosis (DVT) and Pulmonary embolism (PE),
One of the three major cardiovascular causes of death, along with myocardial infarction and stroke

PE – most common preventable cause of death among hospitalized patients.
PE and DVT occurring after total hip or knee replacement are unacceptable "never events" and are no longer reimbursable.

• The long-term effects of nonfatal VTE lower the quality of life.
• Postphlebitic syndrome, which eventually occurs in more than one-half of DVT patients – No effective management possible

ANATOMY

PATHOPHYSIOLOGY
• Virchow’s Triad
• Venous Stasis• Hypercoagulabilty• Endothelial Damage

ACQUIRED RISK FACTORS•Older age•Major surgery and orthopedic surgery•Cancers, especially of the bone, ovary, brain, pancreas, and lymphomas•Inactivity and immobilization, as with orthopedic casts, sitting, travel, bed rest, and hospitalization•Pregnancy and the postpartum period•Antiphospholipid syndrome•Trauma, minor leg injury, and lower limb amputation•Previous VTE

• Combined oral contraceptives• Hormonal replacement therapy• Central venous catheters• Inflammatory diseases/some autoimmune diseases• Nephrotic syndrome• Obesity• Infection• HIV• Polycythemia vera• Chemotherapy• Intravenous drug use

• INHERITED– Antithrombin deficiency– Protein C deficiency– Protein S deficiency (type I)– Factor V Leiden– Prothrombin G20210A– Dysfibrinogenemia – Non-O blood type

OTHERS:•Low free protein S•Activated protein C resistance•High factor VIII levels•Hyperhomocysteinemia•High fibrinogen levels•High factor IX levels•High factor XI levels

DIAGNOSIS
• Clinical Examination
• Only 1/4th of DVT Produces Clinical Signs & Symptoms
• Most important Physical Sign – Swelling of Limbs• Muscles Become Stiff & Hard – M/I than
Tenderness

• Homan’s Sign – Forcible Dorsiflexion
• Moses Sign – Squeezing from side to side
• May Dislodge the Clot & Increase PE Risk


Two-level DVT Wells score
Clinical feature PointsActive cancer (treatment ongoing, within 6 months, or palliative) 1Paralysis, paresis or recent plaster immobilisation of the lower extremities
1
Recently bedridden for 3 days or more or major surgery within 12 weeks requiring general or regional anaesthesia
1
Localised tenderness along the distribution of the deep venous system
1
Entire leg swollen 1Calf swelling at least 3 cm larger than asymptomatic side 1Pitting oedema confined to the symptomatic leg 1Collateral superficial veins (non-varicose) 1Previously documented DVT 1An alternative diagnosis is at least as likely as DVT −2
Clinical probability simplified scoreDVT likely 2 points or moreDVT unlikely 1 point or lessa Adapted with permission from Wells PS et al. (2003) Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. New England Journal of Medicine 349: 1227–35




• The sensitivity of the d-dimer is >80% for DVT (including isolated calf DVT) and >95% for PE.
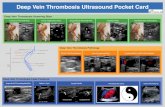
• With Suspected DVT, Doppler/Duplex USG should be preferred to D-Dimer

COMPLICATIONS


postphlebitic syndrome
• A late effect of DVT -occurs in more than one-half of DVT patients.
• Causes the venous valves of the leg to become incompetent and exude interstitial fluid.
• Chronic ankle or calf swelling and leg aching, especially after prolonged standing.
• Severe postphlebitic syndrome causes skin ulceration, especially in the medial malleolus of the leg. There is no effective medical therapy for this condition.

DVT & CANCER

• Patients undergoing surgery for cancer have a higher risk of postoperative deep vein thrombosis (DVT) than those having surgery for nonmalignant diseases.
• Longer time to recover from Surgery & Additional Functional limitation due to cancer also increases the risk.

Tumors Strongly Associated With Thrombosis
• Autopsy studies and retrospective reviews suggest that cancers of the pancreas, lung, and stomach, and adenocarcinomas of unknown primary, are most strongly associated with thrombosis, adding to the view that mucin-producing cancers are the most often associated with VTE.

• Lung cancer accounted for 21% of cases
• Colon cancer for 18%, and
• Prostate cancer for 17%

NON PHARMACOLOGICAL MANAGEMENT
• Leg Elevation• Ambulation• Fitted Graduated Compression Stockings
Special Situations• IVC Filters• Embolectomy


• Mini-UFH, mini-dose unfractionated heparin, 5000 units subcutaneously twice (less effective) or three times daily (more effective); LMWH, low-molecular-weight heparin, enoxaparin, 40 mg once daily, or dalteparin, 2500 or 5000 units once daily;
• IPC, intermittent pneumatic compression devices.

• Minimum distance of walking required daily to prevent venous thromboembolism was 398 m
• Wayman Unit= 398m / 0.5 Miles

SURGICAL PROPHYLAXIS
• Low Dose Prophylaxis – UFH
5000 Units Deep S.C 2hrs before
5000 Units 8-12 hrs thereafter as required

For Active Phlebitis•Medium Dose – 20,000 to 60,000 units per day
For PTEHigh Dose-60,000 to 120,000 Units/Day

Weight Based Dosing Regimen
• Initial Therapy
• Bolus – 80 U/Kg• Infusion 18U/Kg/Hr
• UFH

LMWH & Pentasaccharide
• Enoxaparin 1mg/kg/sc q12h or 1.5mg/kg/24h
• Tinzaparin 175 IU/Kg SC Daily• Dalteparin 200 Iu/Kg SC Daily
• Fondaparinux 5.0 mg sc daily(50 kg) 7.5mg(50-100kg) 10 mg sc (100+kg)

To Continue Treatment ?
Reversible risk factors – 3months
Isolated Calf vein DVT – Serial Imaging 2 wks If Extension – Anticoagulation
With Cancer, Decision to be IndividualisedUsually Active Cancer + DVT = 6 months Tx

It is ideal to continue OP treatment with LMWH as OD (Dalteparin 200 IU/Kg OD 1 m.o continue 150 IU/Kg for 5 months)
Warfarin – INR 2.5(2-3) – Higher incidence of complications and futher VTE episodes compared to LMWH.