Deep Vein Thrombosis
-
Upload
gauhar-azeem -
Category
Health & Medicine
-
view
281 -
download
0
Transcript of Deep Vein Thrombosis

Jeopardy
• A quiz competition in which contestants are presented with general knowledge clues in the form of answers, and must phrase their responses in question form.

Jeopardy
This condition is the major cause of Pulmonary Embolism…

Deep Venous Thrombosis
• A review by
• Dr. Tehreem
• Dr. Asif Sarwar
• Dr. Gauhar Mahmood

Deep Venous Thrombosis
• Deep vein thrombosis (DVT) is a condition in which a blood clot (thrombus) forms in one or more of the deep veins in your body, usually in your legs.
• Deaths from DVT associated PE are 300,000 annually in the USA.
• 3 DVT in ward right now.

Goals
• Early recognition and appropriate treatment of DVT and its complications can save many lives.
• The goals of knowledge about and then administering proper pharmacotherapy for DVT are to reduce morbidity, prevent postthromboticsyndrome (PTS) and prevent dreaded Pulmonary Embolism.

Venous Anatomy Lower Limbs
• Superficial Veins:• Suprafacial• Primary collecting veins of lower extremity• Passive, thin walled, distensible
• Deep Veins:• Subfacial• Secondary conduit veins• Thicker, less distensible• Surrounded by dense tightly bound tissues• 2 systems, below and above knee

Venous Anatomy lower limb

Blood Flow
• Superficial to deep veins
• 100-150ml blood fills in calf (Peripheral Heart) and deep veins
• Calf contracts, valves in perforators close and blood goes up the deep veins
• Coming up next: Pathophysiology

Jeopardy
• Is the famous scientist who recognized the association between venous thrombosis in legs and pulmonary embolism…

Rudolf Virchow

Pathophysiology
• Is a manifestation of Venous Thromboembolism
• Virchow’s triad:
• Venous StasisBy anything obstructing or slowing flow of venous blood
• Activation of Coagulation(hypercoagulable state)
Biochemical imbalance between circulating factors
• Vein Damage
Intrinsic or Extrinsic

Development of Thrombosis
• Microscopic thrombus formation and dissolution is continuous process
• Increased stasis (more microthrombi not washed away by movement), procoagulant factors, endothelial injury, favors coagulation more than fibrinolysis, thus a thrombus
• Coagulation is by Intrinsic or Extrinsic pathway

Anticoagulant mechanisms
• heparin-antithrombin III (ATIII), protein C
• thrombomodulin protein S
• tissue factor inhibition pathways
• Trauma or surgery cause decreaed ATIII levels in blood.
• ATIII levels are decreased and reduced longer in Total Hip Replacement than in general surgery.
• More Coagulation, less fibrinolysis.

Venous Insufficiency
• Thrombus organization by inflammatory cells
• Fibro-elastic intimal thickening
• Valvular Dysfunction, incompetence and wall fibrosis
• Chronic venous insufficiency develops in 29-79% of patients with an acute DVT
• Most acute DVTs evolve to complete or partial recanalization, and collaterals develop in a few months
• residual evidence of thrombus or stenosis is observed in half the patients after 1 year. But damage stays.
• Hemodynamic venous insufficiency is the underlying pathology of postthrombotic syndrome (PTS)

Retrograde flow
• If adequate collaterals exist affect may be minimal
• If not Pain and swelling occurs and flow is retrograde
• Calf muscle contracts and dilation of feeding perforators occurs, valves non functional
• May produce superficial venous incompetence

Etiology

Virchow’s Triad

Summary of risk factors
• A summary of risk factors is as follows:• Age 30 year old x 30= 80 year old• Immobilization longer than 3 days• Pregnancy and the postpartum period• Major surgery in previous 4 weeks• Malignancy (abnormal coagulation, pressure,
chemotherapy)• Long plane or car trips (> 4 hours) in previous 4
weeks• Cancer• Previous DVT• Anatomical Variations

May-Thurner or Cockett syndrome

Summary of risk factors
• Stroke• Acute myocardial infarction (AMI)• Congestive heart failure (CHF)• Sepsis• Nephrotic syndrome• Ulcerative colitis• Multiple trauma• CNS/spinal cord injury• Burns• Lower extremity fractures, injury• Systemic lupus erythematosus (SLE) and the lupus anticoagulant• Behçet syndrome• Homocystinuria• Polycythemia rubra vera

Summary of risk factors
• Thrombocytosis• PICC Line> CVC• Inherited disorders of coagulation/fibrinolysis• Antithrombin III deficiency• Protein C deficiency• Protein S deficiency• Prothrombin 20210A mutation• Factor V Leiden• Dysfibrinogenemias and disorders of plasminogen activation• Intravenous (IV) drug abuse• Oral contraceptives• Estrogens• Heparin-induced thrombocytopenia (HIT)

Even a few hours journey if…

History
• Pain• Limb Edema• Tenderness• Warmth or Erythema
• Can be present or absent, unilateral or bilateral, mild or severe
• Presentation can be of Pulmonary Embolism, sudden coughing, haemoptysis, sharp chest pain, rapid breathing or shortness of breath, light headedness.

Physical Examination
• Homan’s sign
Calf pain on dorsiflexion of foot
Positive in less than 33% of DVT patients and more than 50% in patients without DVT

Physical Examination
• Warmth on area of the clot
• Tense leg
• Red or discolored skin
• The most common abnormal hue is reddish purple from venous engorgement and obstruction. Can be cyanotic or white.
• Signs and symptoms depending upon the cause.

Differential Diagnosis
• Cellulitis• Primary DVT often develop a secondary cellulitis,
while patients with primary cellulitis often develop a secondary DVT.
• Baker Cyst• Budd-Chiari Syndrome• Cellulitis• Heart Failure, Congestive• Pulmonary Embolism• Thrombophlebitis, Septic• Thrombophlebitis, Superficial

Workup
• Wells Score

Low pretest probabilty
• Go for a D Dimer test
• D-dimer levels remain elevated in DVT for about 7 days
• Negative value rules out in low pretest probability
• Negative result in high pretest probability, has no value, start anti coagulation nonetheless and go for ultrasound.

Intermediate to High Pretest
Probability of DVT
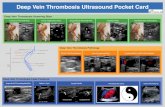
• Ultrasonography is recommended
• Doppler Ultrasound can depict absent or abnormal flow even if clot isn’t visible in normal ultrasound.

Venography
• Radiography of a vein after injection of a radiopaque fluid.
• Conclusive diagnosis historically required invasive and expensive venography, which is still considered the criterion standard. Since 1990, the diagnosis has been obtained noninvasively by means of sonographic examination.

CBC and Coagulation Profile
• Can look for
• Polycythemia
• Leucocytosis
• Thrombocytosis
• Low PT, APTT, hypercoaguable state

Further Imaging
• CT Scan and MRI if required
• Suspecting iliac vein or inferior vena cavalthrombosis

Who to manage inpatient
• Suspected or proven PE• Significant CV or pulmonary comorbidity• Ileofemoral DVT• Contraindication to anticoagulation• Disorder of Coagulation• Pregnancy• Morbid obesity 150kg+• Renal Failure• No compliance, far from hospital, resistance to
therapy, no close follow up.

Leg Elevation


Treatment
• The primary objective for the treatment of DVT are to prevent a PULMONARY EMBOLUS.
• The mainstay of treatment is ANTICOAGULATION
• Heparin, Vit K antagonists (Warfarin), and Factor Xa inhibitors(Fondaparinux)
• Anticoagulation resolves immediate symptoms, intervention is often to reduce 75%long term risk of PTS

Who not to anticoagulate
• Intracranial Bleeding
• Severe Active Bleeding
• Recent brain, spinal cord, eye surgery
• Pregnancy
• Malignant hypertension
• Relative contraindications include Recent Major surgery, recent CVA, severe Thrombocytopenia

Guidelines for Anticoagulation
• Admitted patients are treated with LMWH, Unfractionated heparin (UFH), Fondaparinux.
• Warfarin 5mg PO is initiated and overlapped for about 5 days until the INR is >2 for 24 hours.

Unfractionated Heparin
• Standard of care in admitted patients with DVT before LMWH.
• Prevents extension of thrombus and reduce PE risk
• Heparin must be overlapped for 4-5 days with warfarin till INR>2
• Because of initial transient hypercoaguable state induced by Warfarin

IV heparin Protocol
• Initial bolus of 80U/kg
• Constant maintenance of 18u/kg/hr
• Half life 60-90 min
• 1ml contains 5000u
• Check the aPTT or heparin activity level 6 hrs after bolus and adjust infusion rate accordingly
• Continue to check the aPTT or heparin every 6 hrs, until 2 successful values therapeutic
• Monitor aPTT, hematocrit, Platelets every 24 hrs (HIT)
• aPTT is 21-35 sec usually, therapeutic is 1.5 times 50+

LMWH
• Clexane (Enoxaparin)
• Increased Bioavailability, prolonged Half Life.
• Treatment of choice in eligible patients.
• 1mg/kg q12 hours leading to therapeutic peak 0.5-1 iu/mL
• Antagonist?

Fondaparinux
• Inhibits factor Xa interrupts blood coagulation• Generally does not increase PT or PTT
• Dose: <50kg: 5 mg SC once daily• 50-100 kg: 7.5 Sc once daily• >100kg 10mg SC once daily• Patients not responding to Heparin• Prophylaxis of DVT in patient of HIT until patient
can switch to Warfarin 2.5 mg SC daily• Antagonist?

Warfarin
• Warfarin interferes with hepatic synthesis of vitamin K–dependent coagulation factors.
• Initiate warfarin on day 1 or 2 of LMWH or unfractionated heparin therapy and overlap until desired INR, THEN discontinue heparin
• Start 10 mg PO for 2 days in healthy individuals, 2-5 mg PO/IV qDay for 2 days
• Check INR after 2 days and adjust dose according to results
• Typical maintenance dose ranges between 2 and 10 mg/day
• Maintain an INR of 2.0-3.0

Treatment duration
• Maintain an INR of 2.0-3.0
• Surgery-provoked DVT or PE: Treatment duration of 3 months
• Transient (reversible) risk factor-induced DVT or PE: Treatment duration of 3 months
• First unprovoked proximal DVT or PE with low or moderate bleeding risk: Extended treatment consideration with periodic (ie, annual) risk-benefit analysis
• First unprovoked proximal DVT or PE with high bleeding risk: Treatment duration of 3 months

Treatment duration
• First unprovoked distal DVT regardless of bleeding risk: Treatment duration of 3 months
• Second unprovoked DVT or PE with low or moderate bleeding risk: Extended treatment
• Second unprovoked DVT or PE with high bleeding risk: Treatment duration of 3 months
• DVT/PE and active cancer: Extended treatment, with periodic risk-benefit analysis (ACCP recommends LMWH over vitamin K antagonist therapy)

Treatment follow up
• Regular check up on INR, around a week
• Warning signs prompting immediate contact with doctor, stopping warfarin.
• Bleeding from any site in body.
• it is generally considered dangerous to have an INR above 4.0. An INR above 5.0 may require a medical dose of vitamin K to bring the INR down to a lower level.

Endovascular Intervention
• Indications for intervention include the relatively rare phlegmasiaor symptomatic inferior vena cava thrombosis that responds poorly to anticoagulation alone, or symptomatic iliofemoral or femoropopliteal DVT in patients with a low risk of bleeding.
• The goals of endovascular therapy include reducing the severity and duration of lower-extremity symptoms, preventing pulmonary embolism, diminishing the risk of recurrent venous thrombosis, and preventing postthrombotic syndrome.

Endovascular Intervension Procedures
• Percutaneous transcatheter treatment of patients with deep venous thrombosis (DVT) consists of thrombus removal with catheter-directed thrombolysis, mechanical thrombectomy, angioplasty, and/or stenting of venous obstructions.

Surgical Thrombectomy
• Surgical thrombus removal has traditionally been used in patients with massive swelling and phlegmasia cerulea dolens

Inferior Vena Cava Filters
• Inferior vena cava to trap emboli and minimize venous stasis. Inferior vena cava filter is a mechanical barrier to the flow of emboli larger than 4 mm.
• Confirmed acute proximal DVT or acute PE in patient with contraindication for anticoagulation (this remains the most common indication for inferior vena cava filter placement)
• Recurrent thromboembolism while on anticoagulation
• Active bleeding complications requiring termination of anticoagulation therapy

• Early ambulation on day 2 after initiation of outpatient anticoagulant therapy in addition to effective compression is strongly recommended.
• The regular use of graduated elastic compression stockings reduced the incidence of PTS by 50%

DVT Prophylaxis

Post Thrombotic Syndrome
• PTS can affect 23-60% of patients in the two years following DVT of the leg.
• Signs and symptoms of PTS in the leg may include:• pain (aching or cramping)• heaviness• itching or tingling• swelling (edema)• varicose veins• brownish or reddish skin discoloration• ulcer

Prevention
• prevention of initial and recurrent DVT
• early ambulation
• use of compression stockings
• Electrostimulation devices
• anticoagulant medications.

Treatment
• proper leg elevation
• compression therapy with elastic stockings
• wound care for leg ulcers
• angioplasty and vascular stents in proximal thrombosedveins by an experienced physician can provide significant relief of swelling and healing of skin ulcers
• Compression bandages are useful to treat edemas


AT treated by butanedione and selected for its high heparin affinity (AT-BD)