CORONARY ARTERY PERFORATION DURING PCI
-
Upload
vishal-vanani -
Category
Health & Medicine
-
view
536 -
download
5
Transcript of CORONARY ARTERY PERFORATION DURING PCI
CORONARY ARTERY PERFORATION DURING PCI
DR. VISHAL VANANIJASLOK HOSPITAL AND RESEARCH CENTRE
MUMBAI14 MARCH 2016
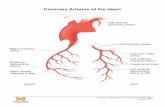
Coronary Perforation• Coronary artery perforation is defined as evidence
of extravasation of contrast medium or blood from the coronary artery, during or following percutaneous intervention.
• Anatomically, perforation is categorized as –• Proximal or mid vessel• Usually more profound with greater likelihood of
significant sequelae• Distal vessel• There the aetiology is often the guide wire (WIRE
EXIT) and the clinical course is frequently benign
Other classifications• Fukutomi1
• Type I: Epicardial staining without a contrast extravasation• Type II: Epicardial staining with a visible jet of contrast
extravasation
• Kini2
• Type I: Myocardial staining without contrast extravasation• Type II: Contrast extravasation into pericardium,
coronary sinus, or cardiac chambers
1.Fukutomi T, Suzuki T, Popma JJ, et al. Early and late clinical outcomes following coronary perforation in patients undergoing percutaneous coronary intervention. Circ J 2002;66:349-56.2.Kini AS, Rafael OC, Sarkar K, et al. Changing outcomes and treatment strategies for wire induced coronary perforations in the era of bivalirudin use. Catheter Cardiovasc Interv 2009;74:700-7.
First data…• Ellis and colleagues reported first large scale series derived
from data obtained from 11 centres, from 1990 and 1991.• Of 12,900 procedures performed, 62 were complicated by
coronary perforation (0.5%).• They observed that the use of ‘new devices’ increased risk
of perforation.
Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era: incidence, classification, management, and outcome. Circulation 1994;90:2725-30.
• Only 14 out of 62 perforations (23%) occurred following POBA, others from debulking techniques.• Complication rate –• POBA - 0.1%• Excimer laser - 1.9%• Rotational atherectomy - 1.3%
• Predesposing patient characteristics –• Female gender• Increasing age
• Over sizing of the angioplasty balloon was one of the key causes for perforation.• The development of cardiac temponade was associated
with appreciable mortality (20%)particularly if it occurred in catheter laboratory as a result of brisk
extravasation (Type III)
• The incidence of Coronary Artery Perforation (CAP) has not changed significantly over two decades.• It is reported between 0.2% and 0.9%.
Sequelae of CAP• Caused by CAP• Blood loss• Distal ischemia• Pericardial Temponade• Cardiogenic shock• Death
• Caused by management strategies• Myocardial Ischemia• Acute vessel occlusion• Myocardial infarction• Operative morbidity and mortality• Death
Diagnosis• Not all perforations are immediately visible on coronary
angiography.• Remarkable proportion of patients may develop temponade
more than 2 to 6 hours after procedure.• The clinical manifestation may be non-specific, and the
patient may simply develop progressive hypotension.• A high index of suspicion should be maintained in order to
secure the correct diagnosis in a timely fashion.
Outcomes• In various studies, outcomes depend largely upon the
severity of perforation.• The outcome is worse if the temponade develops abruptly
within the catheter laboratory, rather than in the delayed fashion in the recovery room or ICU.• Outcomes also depend upon associated co-morbidities.• Chronic renal dysfunction• Pre-procedural impairment of LV function• Older patient
• Cavitary spilling type III perforation
Lesion characteristics• Calcification• Tortuosity• Eccentric plaque• AHA/ACC class B or C lesions• Small calibre vessel
• A study1 of 38559 patients with 72 perforations reported that more than 40% of perforations were seen in vessels of less than 2.5mm diameter.
• The authors describe that the device-lumen mismatch is more important than the vessel reference diameter.
• Other study2 of 8932 patients with 35 perforations showed that balloon induced perforation was more likely where the balloon to artery ratio was 1.3±0.3 compared with a ratio of 1.0±0.3 where no problem ensued.
1.Javaid A, Buch AN, Satler LF, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2006;98:911-4.2.Ajluni S, Glazier S, Blankenship L, et al: Perforations after percutaneous coronary interventions: clinical, angiographic, and therapeutic observations. Catheter
Cardiovasc Diagn 32:206– 212, 1994.
Use of GP IIb-IIIa inhibitors• Studies comparing outcomes of CAP in patients with or without use of
GPI reported a modest adverse influence where GPI were used.• In a study* of 16,298 patients with 95 perforations, GPI were used in 33
cases.• When these 33 cases were compared with the other 62 cases (where
GPI were not used), they found no difference in• Mortality and• Myocardial Infarction
• But, GPI use was associated with• Higher incidence of temponade and• Greater requirement of emergency surgery
*Fasseas P, Orford JL, Panetta CJ, et al. Incidence, correlates, management, and clinical outcome of coronary perforation: analysis of 16,298 procedures. Am Heart J 2004;147:140-5.
GPI and perforations• Great caution should be exercised if any perforation is identified, even if
seemingly trivial, where GPI is used.• Abciximab binds irreversibly to platelet receptors, rendering platelet
activity almost negligible for 24 – 36 hours.• In case of perforation with Abciximab, unlike the small molecules
Tirofiban and Eptifibatide, simply discontinuing the infusion of Abciximab will not reverse its effect.
• Platelet transfusion may be required to restore bleeding time.• The strategy should be case based, balancing the stoppage of life
threatening haemorrhage with the importance of maintaining crucial revascularization in a given case.
BIVALIRUDIN• This study compared the consequences of CAP in patients who
underwent anticoagulation with bivalirudin to those in patients who underwent anticoagulation with heparin at time of CP.
• From 33,613 procedures, 69 patients (0.2%) had CAP, Bivalirudin was used in 41 patients, while Heparin in 28.
• The primary end point for this analysis was the composite of in-hospital death, cardiac tamponade, or emergency cardiac surgery.
• The primary composite end point was similar between groups.• However, there was a lower rate of cardiac surgery requirement in BIV-
treated patients.• The study suggests that choice of procedural anticoagulant agent does
not influence outcome when CP occurs.
BIVALIRUDIN• A pooled analysis of patients treated with PCI in three randomized trials
including REPLACE-2, ACUITY, and HORIZONS-AMI.• Among a total of 12,921 patients, CAP occurred in 35 patients (0.27%).• Baseline creatinine clearance was the only independent predictor of CA
perforation.• Patients assigned to BIVALIRUDIN versus UFH plus a GPI had
• non significantly lower rates of death,• similar rates of MI,• significantly lower rates of TVR, and• similar rates of the composite end-point of death/MI/TVR.
• In three PCI trials, treatment of patients experiencing CA perforation with bivalirudin monotherapy was not associated with worse outcomes compared to treatment with UFH plus GP IIb/IIIa inhibitors.
Atherectomy• Use of either atherectomy or laser ablative technology is
associated with a higher incidence of perforation than in convention balloon and stent PCI.• However, the increased complication rate using these devices
is strongly influenced by the complexity of the coronary disease being treated.• Ellis1 and colleagues reported that the incidence of
perforation with balloon angioplasty was 14 out of 9080 cases (0.1%), whereas that of debulking techniques collectively was 48 out of 3820 cases (1.3%).• Later reports suggested CAP rate of 0.4% (1990)2 and 0.3%
(2002)3 for rotablation.1.Ellis SG, Ajluni S, Arnold AZ, et al. Increased coronary perforation in the new device era: incidence, classification, management, and outcome. Circulation 1994;90:2725-30.
2.Gruberg L, Pinnow E, Flood R, et al. Incidence, management, and outcome of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2000;86:680-2, A8.3.Fejka M, Dixon SR, Safian RD, et al. Diagnosis, management, and clinical outcome of cardiac tamponade complicating percutaneous coronary intervention. Am J Cardiol 2002;90:1183-6.
Guide Wires• Several authors have clearly pin-pointed the hydrophilic
wire as a more risky equipment for perforation.• Javaid et al1 found that 13 out of 15 wire associated
perforations had hydrophilic coating.• Ramana el2 at found that the majority of 25 perforations
were caused by guide wires and these were usually hydrophilic and stiff.• Witzke3 and group found that 51% of perforations were wire
mediated
1.Javaid A, Buch AN, Satler LF, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2006;98:911-4.2.Ramana RK, Arab D, Joyal D, et al. Coronary artery perforation during percutaneous coronary intervention: incidence and outcomes in the new interventional era. J
Invasive Cardiol 2005;17:603-5.3.Witzke CF, Martin-Herrero F, Clarke SC, Pomerantzev E, Palacios IF. The changing pattern of coronary perforation during percutaneous coronary intervention in the new
device era. J Invasive Cardiol 2004;16:257- 301.
Guide Wires• Wires are much less likely to cause a breach in the proximal
or mid vessel, but more likely to do so distally, in the terminal sub branches.• They are also less likely to cause frank rupture of the vessel
than a high pressure balloon barotrauma.• Hence, the appearance of angiography is more subtle when
the wire is the culprit.• Fasseas classified 86% of guide wire mediated ruptures as
Ellis type I or II on angiography.
Fasseas P, Orford JL, Panetta CJ, et al. Incidence, correlates, management, and clinical outcome of coronary perforation: analysis of 16,298 procedures. Am Heart J 2004;147:140-5.
Guide Wires• A proportion of such patients may go on to develop
pericardial temponade.• In some instances this only becomes manifest late (between
2-26 hours post procedure)• One way to minimize distal trauma is to create loop at the
end of the wire, rendering it less likely to inadvertently puncture the vessel wall.• The adjunctive use of GPI may potentiate prolonged
bleeding from a seemingly minor blemish in the vessel.
Chronic Total Occlusions• In CTO intervention, there is always a high risk of coronary perforation,
and more so with the heavy weight, stiff tipped wire.• If there is no balloon inflation where the wire is incorrectly positioned,
there is minimal extravasation of contrast and blood.• Use of GPI should be withheld until the occlusion is safely crossed and
the operator is confident that the distal tip of the wire is seated intraluminally.
• Shimony* and colleagues studied 9568 procedures and compared 57 patients having CAP with 171 patients who had no CAP and found that CTO intervention is the strongest independent predictor of CAP, followed by calcified lesions and NSTEMI.
*Shimony A, Zahger D, Van Straten M, et al. Incidence, risk factors, management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2009;104:1674-7.
• Most important step is to recognize and identify presence of a perforation.
• High index of suspicion• Subtle signs: Unusual migration of wire tip, dye
staining, unexplained hypotension
Strategy• Strategy depends upon –• Site of the perforation• Severity of the insult• Hemodynamic stability of patient• Persistent bleeding
• Supportive measures• Intravenous fluids• Oxygen• Analgesia• Inotropic support• Atropine• Intra aortic balloon counterpulsation
• Type I perforations usually respond to conservative measures.• In any case, indispensable measures are:• Fastidious post-procedural care• Cautious monitoring of hemodynamic parameters• At least one, and if required, serial echocardiographic
assessment.
Javaid A, Buch AN, Satler LF, et al. Management and outcomes of coronary artery perforation during percutaneous coronary intervention. Am J Cardiol 2006;98:911-4.
• Type II or III perforations• Initial management is similar.• First objective is to stop bleeding.• Immediate step is to inflate a balloon at the site of bleeding
if it is in the mid or proximal vessel, and more distally for a remotely situated wire perforation to buy the time for further strategy making.• This prevents the development of temponade, and
favourably alters the outlook of the situation.
• In significant proportion of cases, prolonged balloon dilatation is all that is required.• Balloon inflation for upto 30 min is required.• If the patient can not tolerate ischemia, then perfusion
balloon, if available may be helpful.• Fukotomi reported excellent results using perfusion balloon
for Ellis type III rupture
Fukutomi T, Suzuki T, Popma JJ, et al. Early and late clinical outcomes following coronary perforation in patients undergoing percutaneous coronary intervention. Circ J 2002;66:349– 356.
• A number of authors advocated deployment of standard intracoronary stents to secure perforation site.• This may involve the deployment of a number of layers of
stent over the point of rupture before it can be sealed off.
Anticoagulant therapy and platelet inhibitors• Important question –• Whether dealing with the perforation signals the end of the
procedure or the operator wants to continue the procedure after control of bleeding is achieved.• If the case is to be discontinued, reversal of the heparin with
protamine has been shown to be effective alongside other measures.• But this should be deferred till balloons and wires are still in
the artery.
GPI• Intravenous GPI should be discontinued in majority of cases
where perforation is identified.• Even seemingly trivial blush of extravasation may progress
to severe problems if these agents are ongoing.• Abciximab counteraction with fresh platelets transfusion, as
earlier discussed, should be executed with precaution on case by case base.
ACT• There is no clear recommendation regarding which level of
the heparin anticoagulant effect should be maintained after CAP.• Because intervention devices remain in the patient, the
heparin effect should not be completely reversed, and it might be acceptable to maintain the ACT at 150–250 s.• The ACT should be measured immediately after CAP.• Further treatment is dependent on the bleeding level and
hemodynamic status.
Cardiac Temponade• Immediate Echocardiography, urgent drainage by
pericardiocentesis is must.• Drainage not only alleviates hemodynamic problem, but
also allows for an active evaluation of the rate of ongoing bleeding from the perforation site.• Sometimes, accumulation of very small amount of
pericardial blood may result in profound hemodynamic suppression or cardiac arrest.• Deploying a drain in such situation is very difficult.• At least a clear rim of fluid should be visible on
echocardiography before putting a drain, otherwise there is a risk of puncturing RV free wall.
Pericardiocentesis• Analgesia• Removal of full volume• Blood products transfusion• Auto transfusion• Goal should be to dry out the pericardial cavity
Pericardiocentesis• Once the space is completely dry, the volume which is
further accumulated should be counted every minute to know the success of local treatment at perforation site.• If there is no resolution of bleeding at 30 minute, further
action is required.• This may include Surgery.• Pericardial temponade in this situation carries mortality of
20-50%.
Covered Stents• Frank rupture of proximal or mid coronary artery often
constitute a tear in the vessel, upto 5 mm in length.• Deploying a covered stent isolates the point of haemorrhage
from the circulation.• The most widely used device is PTFE covered stent.• Sandwich design• Inflexible, difficult to deliver in certain areas
Covered Stents• Briguori1 and colleagues reported 11 cases treated in this
fashion and compared them with other 17 cases treated with BMS.• In both groups, balloon temponade and reversal of
anticoagulation failed.• MACE rate was 18% in covered stent group compared to
88% in BMS group.• Stankovic2 reported reduction in MACE rate for TYPE III
perforations using PTFE covered stents but no benefit was gained in type II perforations.
1.Briguori C, Nishida T, Anzuini A, Di Mario C, Grube E, Colombo A. Emergency polytetrafluoroethylene-covered stent implantation to treat coronary ruptures. Circulation 2000;102:3028 –3031.
2. Stankovic G, Orlic D, Corvaja N, Airoldi F, Chieffo A, Spanos V, Montorfano M, Carlino M, Finci L, Sangiorgi G, Colombo A. Incidence, predictors, in-hospital, and late outcomes of coronary artery perforations. Am J Cardiol 2004;93:213–216.
Covered Stents• On the other side, Ly and colleagues achieved successful
seal of the perforation using PTFE in 71% of cases, but there was no statistically significant reduction in the development of temponade, nor the requirement of emergency surgery when it was compared to prolonged balloon dilatation.• Difficulty in delivery of this inflexible device is most
troublesome in the calcified, tortuous vessel which is usual substrate in the perforated vessel.
Covered Stents• Additional late concern is of in-stent restenosis.• Although poorly quantified, a small number of patients
undergoing angiographic follow-up showed 29% restenosis rate.
Briguori C, Nishida T, Anzuini A, Di Mario C, Grube E, Colombo A. Emergency polytetrafluoroethylene-covered stent implantation to treat coronary ruptures. Circulation 2000;102:3028 –3031.
Distal Perforation• Covered stents are of no benefit.• Most of them are caused by angioplasty guide wire.• Objective is to seal off the leaking branch.• Little concern for ischemia to the small region of myocardium
supplied by it.• If conventional measures fail, vessel may be occluded by –
• Platinum microcoils (Trufill – Terumo)• Injection of Thrombin• Autologous clotted blood• Subcutaneous adipose tissue• Tris-Acryl gelatin microspheres• Polyvinyl alcohol foam
Emergency Surgery• Cases not responding to conventional measures are sent for
emergency surgery.• These perforations are frank ruptures, and not modest distal
perforations.• Ellis reports 63% of type III perforations had to go for
surgery, while very few of type I or type II underwent surgery.
Surgical outcomes• The results are disappointing.• The mortality of emergency surgery in reports of
both Fejka and Witzke was 50%.
So, why is an operation such a poor optionfor these cases?
Because….• These are cases with• Other treatment options failed• Ongoing bleeding• Hemodynamic compromise• On inotropic support• Coagulopathy• Myocardial infarction• Deterioration of renal function
No surgery…• Some operators send remarkably few patients for an
operation, and their overall mortality figures are impressively low.• Fukutomi1 and colleagues reported 69 cases of CAP, 29
progressing to temponade.• The mortality was zero.• Only two of the 69 underwent surgery.• Therefore, either conservative or percutaneous treatment
options were successful in vast majority of patients.
1.Fukutomi T, Suzuki T, Popma JJ, et al. Early and late clinical outcomes following coronary perforation in patients undergoing percutaneous coronary intervention. Circ J 2002;66:349– 356.
Surgery, when….• But, it is always sensible to keep surgical team ready to take
patient on operative table at any moment.• If the bleeding from pericardial tube is persisting at a rate
above 10mL per minute despite all other action being taken, mechanical and pharmacological, it is prudent to call a surgeon.
Special measures• A case report of LAD CTO intervention complicated
by Type III perforation with Conquest pro wire over Finecross Microcatheter.• Immediate removal of wire and applying negative
pressure of 2-3 mmHg for 3-5 minutes through microcatheter while preparing the fat emboli sealed the perforation successfully.
TCTAP C-031, Case from Indonesia
Dual guiding catheter technique• Retrieving the balloon and inserting a covered stent may
require some time and it is possible that the stent will not reach or cross the lesion.• Hence, the perforation may be without sealing for an
unpredictably long period of time.• Use of a dual guiding catheter approach reduces the
duration of uncontrolled hemorrhage through the perforation.
Dual guiding catheter technique• After placing a second guiding catheter and guide wire, the
covered stent can be advanced and placed immediately proximal to the sealing balloon.• In a rapid maneuver, the sealing balloon can be retracted
and the covered stent advanced and implanted.• If initial delivery of the covered stent fails, re-insertion of
the blocking balloon can be performed quickly which provides time to consider options for a second attempt (smaller covered stent, additional guide wire, upsizing the guiding catheter, etc.).
Balloon occlusion types• Persistent Complete Occlusion• Persistent Partial Occlusion• Intermittent Complete Occlusion• Intermittent Partial Occlusion
Persistent Complete Occlusion• More than 20 min – unacceptable• Heparin can not be reversed with protamine at the
perforation place
Persistent Partial Occlusion• Controlled Hypotension• Severity of stenosis with Pressure drop with FFR
with Distal pressure with TIMI flow• Short length, highly compliant balloon inflation at
the location of CAP
Intermittent Complete Occlusion• An intermittent, nonfatal complete ischemic model is found to improve
tissue tolerability to reperfusion injury after long-term ischemia and to delay cell death.
• This phenomenon is known as “ischemic preconditioning (IPC)”• A 10 min ischemia/1 min reperfusion model is optimal.• If necessary, this procedure can be repeated three or four times.• Notably, IPC can attenuate ischemia reperfusion injury during cardiac
surgery, which is the ultimate method to treat CAP.• However, this model may not be satisfactory for patients with
preexisting cardiac dysfunction.• To avoid cardiac function deterioration, a shortened ischemic time or
prolonged reperfusion time (such as 5 min/5 min) model should be an alternative in these patients.
Intermittent Partial Occlusion• To verify whether a CAP has been sealed during partial occlusion, a
balloon must be deflated for angiography, which results in reperfusion.• If the perforation is not sealed, further occlusion is needed (i.e., the
intermittent partial occlusion model).• This process can also induce ischemia reperfusion injury, in which the
ischemic myocardium shifts from stunned to hibernating.• Because of the heavy total ischemic burden, hibernating cardiomyocytes
are damaged more severely than stunned cardiomyocytes are; therefore, the remarkably prolonged recovery time is usually a few days to several months.
Cunclusion• It is favourable that CAP remains a rare complication.• High index of suspicion.• Immediate diagnosis and localization of perforation• Urgent and serial echocardiographic monitoring• “Stop the bleeding” first• Prolonged balloon dilatation always• May need covered stent• Quick Pericardiocentesis• Worse outcomes if emergency surgery is warranted