Cerebral (encephalopathy) associated with ascariasis
-
Upload
usha-sharma -
Category
Documents
-
view
220 -
download
3
Transcript of Cerebral (encephalopathy) associated with ascariasis

Indian 3. Pedia#. 41 $56, 1974
CEREBRAL (ENCEPHALOPATHY) ASSOCIATED WITH ASCARIASIS*
USHA SHARMA, S. SAXENA AND S. KANGHAN
3 ipu
Encephalopathy has been defined by Brain and Walton (1970) as cerebral dis- turbance occurring chiefly in children, characterised pathologically by toxic changes in the nervous system and clinically by delirium, coma, convulsions and symptoms of meningeal irritation. The term "parasitic encephalopathy" appears quite justified. The various neurological symptoms described by different authors from time to time include irritability, apathy, restlessness, throwing of the limbs, grimacing of the face, delirium, convulsions simulating grandmal epilepsy, grinding of teeth and even peripheral circulatory failure. This simulates the clinical picture of encephalitis or meningitis.
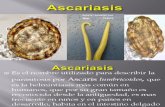
There is widespread parasitic infesta- tion by Ascaris lumbricoidis all the world over. Almost every fourth man in the world suffers from round worm infection. The central nervous system manifestations are not frequent. However, we encountered 25 such cases of encephalopathy during a short period of 6 months, hence it was considered worth while reporting our expe-
rience.
Material and Methods
The clinical material consisted of 25 children admitted to the Paediatric Medical Unit, S.M.S. Hospital, Jaipur, during the period January, 1973 to June
*From the Department of Paediatrics, S.M.S. Medica l College, Jaipur. Received on May 29, 1974.
1973. The cases were selected on the basis of a positive history of having passed para- sites in the stool or vomitus, symptoms suggestive of parasitic infestation and positive stool examination or passage of worms in the stool or vomitus after adminis- tration of anthelminthic drug immediately or within 6-8 weeks.
A thorough clinical examination was done after taking a detailed history. Laboratory investigations included routine blood examination, stool examination by routine smear as well as concentration methods for parasitic ova, and C.S.F. examination.
Observat ions
The patients were classified according to their age (Table 1).
80~o of the patients were males while
there were only 5 females.
Socio-economic status by Prasad's method of classification is shown in Table 2.
Duration of illness : 15 (60%) children had passed an adult parasite just one day prior to admission. In 5 cases (20%)the worms were passed in the stool after anthelminthic treatment in the hospital. In 4 cases the worms were passed at the residence of the patients 4 days prior to admission. One patient passed a bunch of worms in the stool 15 days prior to admis- sion and went on passing 1-2 worms daily till admission and up to 1-2 days afterwards as a result at the administration of anthel-
minthic drugs.

SHARMA ET AL.~CEKEBRAL COMPLICATIONS (ENCEPHALOPATHY) A$$OC~IA.T~D WrrH A B ~ I A S ~ ~ 7
T a b l e I. Distribution by age.
Age (years) No. of patients Percentage of the total
0-1 2 8
1-3 8 32
3-4 4 16
4-5 8 32
5-6 2 8
6-7 1 4
T a b l e 2. Socio-economic status.
Social Class Number of cases Percentage Group
I 0 0
II 0 0
III 11 44
IV 10 40
V 4 16
The symptoms, signs and complications are given in Tables 3, 4 and 5.
Laboratory investigations The C.S.F. was normal in the 23 cases
(92%). In only 2 patients (8%) the C.S.F. proteins were raised (50 mg.%) just above the normal limits. In the rest, the chemistry and cell count were normal. Stool examination revealed Ascaris lurnbri- coidis ova in all; 5 to 6 ova/per high power field in the 18 cases (72%), and 2-3 ova/per
high power field in 7 cases (28~ Routine
examination of blood and urine were normal.
In all patients, symptoms and signs regressed after giving anthelminthic treat- ment. Decaris (Ethnor) was given in almost all cases in a dose of 5 mg.]kg, body weight as a single dose. Rest of the treat- ment was symptomatic depending on the
condition of the patient.

i 3 5 8 NDIAN JOURNAL OF PEDIATKIC$
T a b l e 3. Symptomatology.
VOL 41, No. 322
Symptoms Total cases Percentage
Vomiting 15 60
Headache 14 56
Fever 12 48
Irritability 25 100
Restlessness (characterised by throwing of limbs) 25 100
Delirium 12 48 Grimacing of face 3 12
Grinding of teeth 20 80
Pain in abdomen 12 48
Convulsions 25 100
Table 4. Signs.
Sign Total No. of cases Percentage
Meningism
Cranial nerves unaffected Muscular tone increased
Motor power normal Neurological deficit left
5 20
25 100 22 88
25 100 Nil
Table 5. Associated complications.
Complication Total No. of cases Percen ta ge
Asthmatic bronchitis
Urticarial rash
Peripheral circulatory failure
Gastroenteritis with pain
Mortality
3
1
12
12
2
12
4
48
48
8

SHARMA ]~T AL.--CEREBRAL COMPLICATIONS (ENCEPHALOPATHY) ASSOCIATED WITH ASCARIASIS 359
Discuss ion
Ascariasis in the tropics as a clinical problem is fundamentally different from ascariasis in the West (De Silva 1957). This variability has been attributed to differences in socioeconomic and cultural factors rather than to those of geographic or climatic influences. Toxic cerebral symptoms simulating encephalitis or meningitis have been reported by various workers in different parts of the world (Crowell 1920, Fulleborn, 1920, Chatterjee 1952, De Silva 1957, Jain et al. 1961). A recent survey published by the W.H.O. (1968) also mentions C.N.S. affection. Arean (1958) and Dashmohapatra (1971) reported the occurrence of nervous system manifestations associated with ascariasis in their cases.
This syndrome of toxaemia with nervous symptomatology so often associated with ascariasis has been attributed to either the adverse effect of toxins produced by the larval or adult worms or their metabo- lites like acetaldehyde (Chatterjee 1952, De Silva 1957, Brown 1965)or to larval migration to the brain, causing blockade of the cerebral arteries (Jain et al. 1961, Dashmohapatra 1971) or producing vary- ing degrees of neural degeneration, oedema, haemorrhage or even glial proliferation (Join et al. 1961). However, Jayawardena (quoted by De Silva) dissected the brains of patients dying of round worm toxaemia with completely negative results. Yet Fulleborn (1920) was able to produce granulomatous lesions in the brain by visceral larva migrans of T. canis. Arean (1958) also published an experimental study of ascaris granulomatous lesion in the brain.
Another hypothesis extended is an allergic or immune mechanism involving
an antigen-antibody type of reaction in hypersensitive nervous tissue (Sprent 1955, De Silva 1957). Mac Farlane (1969) also mentions the role of anaphylatoxin, haemo- lysin, neuro or endocrinotoxin present in the parasite as suggested by Girges (1954)
and Brown (1965) but the exact mechanism involved still remains far from clear.
It is apparent fi'om Table 1 that all age groups are affected. The great pre- ponderance of males (20 cases or 80%) seen by us is slightly higher than the report of Shrivastava etal. (1962) and Dashmo- hapatra (1971). Perhaps it can be explained by male children having more chances of coming in contact with contaminated street soil or being given eatables more often, even contaminated ones.
These cases were from grade III, IV and V low income groups, corroborating the role of malnutrition, poor sanitation and hygienic measures, in the pathogenesis of ascariasis.
The time interval between toxic symp- toms and the passage of worms was very short i.e. only one day preceding the onset of symptoms in 60% of cases and in some cases, the worms were continuously being passed even after hospitalisation.
Irritability and restlessness associated with throwing of limbs was present in a
large number of cases in the present series which corroborates the observations made by De Silva (1957) and Marcial Rojas (1971) but contradicts Kakkar (1972) who could notice such symptoms only in 33.3% of cases and Einhorn and Miller (1946) who also noticed this as an uncommon compli- cation. Grinding of teeth was the next most common symptom encountered in about 80~/o of the patients. Vomiting was another quite frequently encountered symptom noticed in 60% cases and all of

360 mDXAN JOURNAL OF PEDIATRICS VOL. 41, NO. 322
them vomited adult parasites either through the month or through the nose.
A stuporous state was noticed in 60% of cases and almost all of them had convul- si.ons (100%) which were generalised tonic and clonic in nature lasting for a few seconds to a few minutes and were of variable frequency. These signs were noticed more frequently as compared to previous workers (.lain et al. 1961) and Dashmohapatra et al.
(1971) and in great contrast to the study ofPohowalla etal. (1959) and Srivastava ct al. (1962) who encountered such symptoms in a negligible percentage of cases. The latter attributed convulsions in these patients to associated factors like dehydration and hyperpyrexia 'rather than to the parasite itself.
Pain in the abdomen was noted in 50% of cases which is in concordance with the reports of Einhorn and Miller (1946) but in marked contradiction to Srivastava et al. (1962) who could find it in 8% cases only. Grimacing of the face was least frequently observed i.e. in 2 cases only, constituting 8% incidence in this series.
The abnormal physical findings included evidence of meningism in 5 cases (20%) and increased muscle tone in 22 patients (88O/o).
The cranial nerves, motor power, superficial reflexes and fundi were normal in all these cases. No neurological deficit could be encountered.
Dehydration was a frequent complica- tion observedin almost all the cases (100%) in varying grades of severity and could be attributed to diarrhaea, vomiting or deficient intake of fluids due to a stuoorous or comatose state of the patient. This complication has also been reported by other workers (De Silva 1957, Srivastava et al. 1962).
Asthmatic bronchitis could be seen in 10% cases only, which is much higher than the figures quoted by Shrivastava et al. (1962) who observed asthma only in 2.6% cases and Dashmohapatra (1971) who
reported it in 4% cases. This difference may partly be explained on the basis of a greater number of patients included in their study.
Allergic manifestations, especially urticarial rash, is well known to be associated with ascariasis so much so that in endemic areas the very appearance of rash is taken to be highly suggestive of parasitic pathology unless proved otherwise. This was observed in 5% in the p.resent series, a figure in close proximity to the one observed by Shrivastava et al. (1962).
Gastroenteritis with pain in the
abdomen and peripheral circulatory failure was noticeable in 50% of cases. Although
this complication has not been described frequently by other workers, it needs the serious attention of paediatricians for giving immediate treatment without which the patient may die soon.
As far as the investigations are concerned the routine blood and urine tests were normal and noncontributory. C.S.F. examination was normal in 92%
of the cases while 2 patients (8%) had a
protein content of 59 mg.% which was slightly above the normal limit. The chlorides, sugar and cell count values were within the normal range. These findings are in consistance with those of De Silva 41957) Jain and Sharma (1961) and Dashmohapatra (1971).
Stool examination was the main investigation of diagnostic and therapeutic importance. A majority of the patients (72%) in the present series revealed the presence of 5-6 ova of Ascaris lumbrivoides
per high power.

SHARMA ET AL.--CEREBRAL COMPLICATIONS (ENCEPHALOORAPHQ) ASSOCIATED WITH ASCARIASIS 361
T h e dea th ra te has been quite low
especially so in compar i son with the figure
34.8% quoted by De Silva (1957) and 20%
by K a k k a r ( ,972). T w o patients (8%) died o f per iphera l
c i r cu l a to ry failure in spite o f v igorous t he r apy including vasopressors (Mephen- tine), steroids, b r o a d base antibiot ics and
in t ravenous fluid t he r a py supplemented
wi th p lasma expanders . Convuls ions were
m a n a g e d by immedia te admin i s t r a t ion o f
p a r a l d e h y d e and phenobarb i tone . I t is
qui te interest ing to note tha t no recur rence fol lowed after admin is t ra t ion o f ant ihe lmin-
thic t rea tment . T h e r e were no neurologi-
cal sequelae among the survivors.
S u m m a r y
25 cases hav ing nervous system mani - festations compl ica t ing ascariasis were
encounte red dur ing a shor t per iod o f 6
months . Almost all o f t h e m presented
wi th symptoms o f i rr i tabi l i ty, restlessness, g r ind ing of teeth and most o f them had cephalgia , convulsions a nd a s tuporous
state s imula t ing encephal i t is or meningit is
jus t i fy ing the term "Ascar i s encephalo-
l~athy ' ' o f toxic/allergic type. T h e hypo-
theses o f its pathogenesis have been dis- cussed. T h e present ing symptoms and signs, r e l evan t l abora to ry investigations, and t r ea tmen t have been discussed.
We are thankful to Prof. R.P. Sharda, Superin- tendent and Professor and Head of the upgraded department of Ophthalmology, S M.S. Hospital, Jaipur for allowing these cases to he published.
References Arean, V.M. (1958). Ascaridic granuloma. An
experimental study. Arch. Pat~. 63, 427. Belding, D.L. (1964). Text Book of Parasitology.
Appleton Century Crofts, Division of Meredith Publishing Co. New York.
Brain, L. and Walton, J.N. (1970). Brain's Diseases of the Nervous System. Oxford Unive, sity Press, London. Page 387.
Brown, R.E. (1966). Neurological manifestations associated with ascariasis. Trop. Dis. Bull 63, 568.
Chatterjee, K.D. (1952). Human Parasites and Parasitic Diseases, Saraswathi Press, Calcutta.
Crowell, B.C. (1920). The dangers of ascariasis. Am. 07. Med. Sei. 159, 380.
Dashmoha•atra, G.S, Mohanty, B. and Patnaik, Gokulanand. (1971). Clinical appraisal of 200 cases of ascariasis with special reference to surgical compli- cations. 7. Indian Med. Assnc. $7, 284.
De Silva, C.C. (1957). Tropical ascariasis. ft. Trop. Pediat. 3, 62.
Einhorn, N.H. and Miller, J.F. (1946). Intes- tinal helminthiasis--A clinical survey of 618 cases of infection with common intestinal helminths in children. Arner. 9~. Trop. Med. 26, 497.
Fulleborn, F. (1020). Uber die Anpassung der Nematodes an den Parasitismus Und den Infektion- sweg Bei Askaris Und andergens Fadewarmeir des Manschen. Arch. Sehihs. Trophen. Hyg. 24, 340.
Girgos, R. (1934). Pathogenic factors x~i aseariasis. 07. Trop. Med. Hyg. 37, 209.
Jain, S.C. and Sharma, B.K, (1961). A typical manifestations of Ascariasis. Current Med. Praet. 5, 405.
Kakkar, K. (1972). Personal Communication.
MacFarlane, L.R.S. (1969). Human Protozoo- logy and Helminthology, Livingston,
Martial Rojas, R.A. (1971). Pathology of Protozoal and Helminthic Diseases. Williams & Wilkins Co. Baltimore.
Pohowalla, J.N. and Singh, S.D. (1959). Worm infestation ininfants and children of preschool age in India. Indian 07. Pediat. 26, 459.
Srivastava, B.N. and Gupta, M.L. (1962). Ascariasis in infancy and childhood: A mlutidiscip- linary study of 500 cases. Indian Pract. 15, 967.
W.H.O. Chronicle. (1968). Control of Ascariasis. 22, 3.