Bone phisiology
-
Upload
parag-deshmukh -
Category
Education
-
view
915 -
download
1
description
Transcript of Bone phisiology

GOOD MORNING

PRESENTED BY – DR. PARAG S. DESHMUKH

CONTENTS• Introduction
• Function
• Classification of bone
• Bone composition
• Bone morphology
• Bone ossification
• Bone physiology
• Conclusion
• Refrence

INTRDUCTION
The Adult human skeleton has a total of 206 bones, excluding the sesamoid bone.
Each bone constantly undergoes modeling during life to help it adapt to changing biomechanical forces as well as remodeling to remove old, microdamaged bone and replaced it with new, mechanically stronger bone to help preserve bone strength.
206 BONES
AUDITORY 6
AXIAL 74APPENDICULAR SKELETON 126

Functions of Bone
Supports & protects soft tissues
Store minerals (Ca & P) – mineral homeostasis
Blood cell production (hemopoiesis) in red bone marrow.
Energy storage -- yellow bone marrow
Buffering action – buffers blood by absorbing or releasing alkaline salts.
Detoxification – Bones can store heavy metals and foreign elements, removing them from blood and reducing there effects on other organs.

Bones are Classified based on shape and structure


Based on location
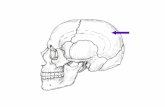
AXIAL SKELETON
• Bones of skull, vertebral column, sternum and ribs
APPENDICULAR SKELETON
• Bones of pectoral griddle, pelvis gridle and limbs
ACRAL
SKELETON
• It’s a part of appendicular skeleton and includes bones of hands and feets.

Epiphysis : End of long boes. Metaphysis = area between epiphyses & diaphysis includes epiphyseal plate in growing bones
Diaphysis = Shaft of long bones.
Medullary cavity = marrow cavity
Physis = epiphyseal growth plate
Gross structure of long bones
Articular cartilage = covers joint surfaces, reduces friction and absorbs shock

• Endosteum = lining of marrow cavity
• Periosteum = tough membrane covering bone
Fibrous layer: Fibrous and
madeup of dense irregular CT Osteogenic layer: contains
many osteoblasts & blood vessels that nourishes bone

TYPES OF BONE TISSUE
Based on texture of cross sections
Compact bone(dense bone or cortical bone)
Spongy bone(trabecular bone, cancellous bone)

Cortical bone
Represents 80% of skeletal mass
• Has slower turnover rate and high resistance to bending and torsion
Contains series of adjacent and overlapping bulls eye formations known as, haversian system or osteon.
Between each osteons are interstitial lamellae(concentric layer of mineralized bone)
Haversian canals communicate with medullary cavity through spaces in spongy bone and with the surface of bone by oblique or transverse channels called as VOLKMAN’S CANAL.

Compact Bone

Compact Bone

Haversian system / Osteon

Located along the epiphyses of long bonesSite of Erythrocyte (RBC) formation
Collagen fibers are not arranged in concentric rings. But the lamellae form rods called TRABACULAE. No Osteons or Haverian Systems are present.
Found in short, flat, irregular bones & epiphyses of long bones. Supports and protect red bone marrow
SPONGY BONE
It is less dense, more elastic and has a higher turnover rate
Trabeculae follows lines of stresses and can realign if the lines of stress changes.

Trabeculae of Spongy Bone

BASED ON MATRIX ARRANGEMENT LAMELLAR BONE
(SECONDARY BONE TISSUE)
• Matur bone with collagen fibers that are arranged in lamellae
• In spongy bone lamellae are arranged parellel to each other.
• In compact bone lamellae are concentrically organized around vascular canal.

WOVEN BONE (PRIMARY BONE TISSUE)
• It is immature bone, in which collagen fibers are arranged in regular random arrays and contain smaller amounts of mineral substance and higher proportion of osteocytes than lamellar bone
• It is temporary bone.
• Eventually gets converted to lamellar bone.

BASED ON MATURITY IMMATURE BONE (Primary bone tissue)
It is woven bone.
Mature bone(Secondary bone tissue)
It is charectiristically lamellar bone
Almost all bone in adults are lamellar bone

Bone: CT of widely-spaced cells separated by matrix
Histology of Bone Tissue
Matrix = 25% water, 25% collagen fibers, & 50% crystallized mineral salts
4 types of cells in bone :
- osteogenic cells
- osteoblasts
- osteocytes
- osteoclasts

Matrix
Contains inorganic mineral salts & protein
- mostly hydroxyapatite ( calcium phosphate )
- some calcium carbonate, K, Mg
- collagen fibers
Mineral salts deposited in a framework of collagen fibers
- calcification (=mineralization) gives bone hardness
- collagen fibers give bone great tensile strength
–

BONE Organic Framework
Osteoblasts, osteocytes, osteoclasts
Collagen Other organic molecules
Inorganic Salts calcium and phosphorus keep
bone rigid Bone stores minerals and ions
for body functions

Non – collagenous organic componentsOsteonectin – Phosphorylated glycoprotein secreted by osteoblasts, binds to collagen & hydroxyappatite, play a role in hydroxy appatite crystallization.
Osteocalcin – Glycoprotein synthesized by osteoblasts, binds hydroxyappatite & Ca, used as a marker of new bone formation.
Bone proteoglycans biglycan & decorin may bind transforming growth factor–β (TGF-β).
Bone sialoproteins, osteopontin & thrombospondin mediate osteoclast adhesion to bone surfaces via binding to osteoclast integrins.

Bone matrix also contains many growth factors, proteases & protease inhibitors which are secreted by osteoblasts, often in a latent form.
Transforming growth factor-β (TGF-β), secreted by osteoclasts as well as osteoblasts, is activated in the acid conditions of the ruffled border zone of the osteoclast, & may be a coupling factor for new bone formation at resorption site.


Osteoprogenitor or Osteogenic cells Appearance
pale staining, small, spindle shaped
Location present on all non-
resorbing surfaces in lacunae within bone.
Extends protoplasmic processes into small canaliculiin intercellular matrix.
periosteum and endosteum
Functiongive rise to osteoblasts in vascularized regions chondroblasts in avascular regions

Osteoblasts
Appearance large, nondividing
cells, eccentric nucleus, basophilic
cytoplasm, cytoplasmic
processes Function
synthesize and secrete organic constituents of bone matrix (osteoid)
aid in calcification

Osteocyte
Appearance smaller and less
basophilic than osteoblast,
have interconnecting processes
Function keeps bone matrix in
good repair release calcium ions from
bone matrix when calcium demands increase

Osteoclasts Appearance
multinucleated, non-dividing cells, acidophilic. Have a ruffled
border and a clear zone on front of resorption side.
Origin From blood
monocytes/ macrophages
Function move around on
bone surfaces, resorbs bone
matrix Focal
decalcification and extracellular digestion by acid hydrolases and uptake of digested material


Blood & Nerve Supply of Bone

BONE FORMATION (OSSIFICATION)• . It is a process of formation of bone and it
includes proliferation of collagen and ground substance with subsequent deposition of calcium salts.
Two types Intramembranous ossification Endochondral ossification


INTRAMEMBRANOUS OSSIFICATION
It is the direct laying down of bone into the primitive connective tissue(Mesenchym).
It results in formation of cranial bones of the skull and the clavicles
All bones formed this way are flat bones
It is also an important process during natural healing of bone fractures

Stages of Intramembranous Ossification

Stages of Intramembranous Ossification

Stages of Intramembranous Ossification

Stages of Intramembranous Ossification

Endochondral Ossification Results in the formation of all of the rest
of the bones Begins in the second month of
development Uses hyaline cartilage “bones” as
models for bone construction Requires breakdown of hyaline cartilage
prior to ossification

1. Development of Cartilage Model
Mesenchyme forms cartilage model of bone during development
There is an aggregation of mesechymal cells
Mesenchymal cells differentiate into chodroblasts.
These chondroblast secret hyaline cartilage matrix

2. Growth of Cartilage Model
Cartilage grows by both :
interstitial (mostly in length) Appositional(mostly in width)
Sometimes during growth of cartilage model some of Inner perichondral cells gives rise to osteoblast instead of chondroblast (as a result fomer perichondrium is now called the periosteum).
Newly formed osteoblast secret osteoid forming bone collar around cartilage model.

3. Development of Primary Ossification Center Chondrocytes differentiate and become hypertrophic.
Then it deposits mineralized matrix.
Cartilage calcification is initiated by matrix vesicles
Calcified matrix is partially resorbed by osteoclast.
After resorption osteoblast differentiate into this area
forming woven bone layer.
Blood vessels enter in this area.
And penetrate bone to allow seeding of bone marrow.

4. Development of the Medullary ( Marrow) Cavity
Osteoblasts deposit matrix over calcified cartilage form trabeculae of spongy bone
Osteoclasts form medullary cavity

5) Development of Secondary ossification centre

6. Formation of Articular Cartilage & Epiphyseal Plate
• Cartilage on epiphyses remains as articular cartilage
• Epiphyseal (growth) plate also remains as cartilage

- source of interstitial growth

4 Zones of Epiphyseal Plate: - Zone of resting cartilage - Zone of proliferating cartilage - Zone of hypertrophic cartilage - Zone of calcified cartilage


Zone of resting cartilage
- anchors growth plate to bone
- Zone of proliferating cartilage
- rapid cell division (stacked coins) Zone of hypertrophic cartilage
- cells enlarge & remain in columns
Zone of calcified cartilage
- thin zone of mostly dead cells
- osteoclasts remove matrix
- osteoblasts & capillaries build bone over calcified cartilage

Factors Affecting Bone Growth
Nutrition: need adequate levels of minerals & vitamins - Ca & P for bone growth
- vitamin C for collagen synthesis
- vitamins K & B12 for protein synthesis
Need adequate levels of specific hormones - insulinlike growth factor ( IGF) needed during
childhood
- promotes cell division at epiphyseal plate
- also need hGH, thyroid (T3 & T4) , & insulin
- sex hormones needed at puberty (estrogen & testosterone):
- stimulate growth & male/female skeletal modifications

BONE PHYSIOLOGY
Eugene Roberts referred orthodontists as craniofacial bone specialist and hence torough knowledge about bone physiology will help us to treat patients more effectively and efficiently.

BONE REGULATORSENDOCRINE REGULATORS:
PTH harmone
Calcitonin
Vitamin D
Vitamin A
Estrogens
Androgens

Growth factors
Paracrine regulators
Autocrine regulators
Neurotransmitters
• Bone morphogenetic protein(BMP)
• Insulin-like growth factors• Transforming –growth factors• Platelet derived growth factor• Fibroblast growth factor
• RANKL (produced locally)
• OPG
Produced intracellularly.

WOLF’S LAWWolff's law is a theory developed by the German anatomist and surgeon Julius Wolff (1836–1902) in the 19th century that states that
Bone reacts to mechanical functional stress through an adaptive process resulting in a change of its external and internal architecture to better withstand this stress.
If loading on a particular bone increases, the bone will remodel itself over a period of time to become stronger to withstand greatest strength with least amount of material

MechanotransductionThe remodeling of bone in response to loading is achieved via mechanotransduction, a process through which forces or other mechanical signals are converted to biochemical signals in cellular signaling.
The specific effects on bone structure depends on the duration, magnitude and rate of loading, and it has been found that only cyclic loading can induce bone formation
When loaded, fluid flows away from areas of high compressive loading in the bone matrix

Mechanotransduction
Osteocytes are the most abundant cells in bone and are also the most sensitive to such fluid flow caused by mechanical loading
Upon sensing a load, osteocytes regulate bone remodeling by signaling to other cells with signaling molecules or direct contact
Additionally, osteoprogenitor cells, which may differentiate into osteoblasts or osteoclasts, are also mechanosensors and may differentiate one way or another depending on the loading condition.[

Example: Weightlifters often display increases in
bone density in response to their training.
Martial artists who strike objects with increasing intensity (e.g., repeated elbow strikes), display increases in bone density in the striking area. This process is termed cortical remodeling

Frost’s Mechanostat ConceptAccording to the Mechanostat, bone growth and bone loss is stimulated by the local mechanical elastic deformation of bone. The reason for the elastic deformation of bone is the peak forces caused by muscles
The Adaptation of bone according to the maximum forces is considered to be a lifelong process. Hence bone adapts its mechanical properties according to the needed mechanical function – bone mass, bone geometry and hence bone strength is adapted according to the every-day usage / needs.

Strain : Deformation per unit length.
It is a dimensionless parameter that is expressed as percent strain or micro strain.
For instance, when a bone of 100 mm in length is elongated by 2 mm, the associated strain is expressed as 2% strain, 0.02 strain, or 20,000 micro strain.Normal=200-2500µ£=0.02%-0.25%
Atrophy=<200µ£=<0.02%
Hypertrophy =2500-4000µ£=0.25%-0.4%
Fatigue failure=>4000µ£=>0.4%
Spontaneous fracture=25000µ£=2.5%
Ultimate strength of bone=25000µ£=2.5%
Frost’s Mechanostat Concept

Benninghoff’s Stress Trajectories It states that lines of orientation of bony trabeculae corresponds to the pathways of maximal pressure and tension that bony trabeculae are thicker in the region where the stress is greater.

In Maxilla – frontonasal buttress, malar Zygomatic buttress,pterygoid buttress
In Mandible - Condyle, Gonial angles, Coronoid process

Modeling & Remodeling
The modern physiologic concept of bone remodeling is largely attributed to Harold Frost.
He differentiate Bone “modeling”(change in shape, size, and position of bones)
FROM
Bone “remodeling”(coupled turnover sequence)

Modeling & RemodelingBoth trabecular & cortical bone grow, adapt & turn over by means of these two fundamentally distinct mechanisms
MODELING Changes the
shape, size, or position of bones in response to mechanical loading or wounding.
Independent site of resorption & formation change the form of a bone.
REMODELING Physiologic term for
internal turnover of a mineralized tissue, without a change in its overall form.
It is a coupled sequence of catabolic and anabolic events to support calcium homeostasis and repair / renew aged or damaged mineralized tissue.

Modeling & Remodeling
Modeling Remodeling
Independent site of resorption & formation change the form of a bone
Specific coupled sequence of resorption & formation occurs to replace previouslyexisting bone

An example of this process long bone increases in length and diameter.
Bone modeling occurs during birth to adulthood and is responsible for gain in skeletal mass and changes in skeletal form.
After peak bone mass has been approached, remodeling becomes the final common pathway by which bone mass is adjusted throughout adult life.
Dominant process of facial growth & adaptation to appliedloads such as head gear, RPE,functional appliance.
Take place at thesame time, butapparent only at the microscopiclevel .
Changes can be seen on the ceph tracings.
seen in bone scans and /or histology.

Modeling & Remodeling
Where bone strains exceed bone's modeling threshold range, modeling can switch on to strengthen the bone.
whereas when bone strains stay below a lower threshold range, disuse-mode remodeling can turn on to reduce whole bone strength by removing some trabecular and endocortical bone.

Growth factors that regulate bone remodelling
1. Insulin – like growth factors (IGF) I & II
2. Transforming growth factor –b (TGF – b) superfamily, including the bone morphogenetic proteins (BMPs)
3. Fibroblast growth factors (FGF)4. Selected cytokines of the
interleukin (IL), tumour necrosis factor (TNF), & colony – stimulating factor (CSF) families

REMODELING:GOALS : • It provides a way for the body to alter the
balance of essential minerals by increasing or decreasing the concentration of these in serum.
• It provides a mechanism for the skeleton to adapt to its mechanical environment reducing risk to fracture

Basic multi-cellular unit (bmu)
The process of bone resorption and formation are closely linked within discrete temporary anatomic structures called as ‘basic metabolizing units’(by Frost)later called as basic multicellular unit
They are readily present in cortical bone but there are evidence for the same concept in cancellous bone.
The cellular components of a BMU maintains the same spatial & temporal relationship to each other while moving through or across the bone.

BASIC MULTICELLULAR UNIT

REMODELING IN CORTICAL BONE Axially oriented cutting & filing cones are the mechanism
underlying internal remodeling of dense compact bone.
The cutting/filling cone has a head of osteoclasts that cuts through the bone & a tail of osteoblasts that forms a new secondary osteon.
10 osteoclasts dig a circular tunnel followed by thousands of osteoblasts that fill the tunnel .
It requires about 29 days to create resorption cavity (200-250µm in diameter) and 134 days to refill it .
Remodeling rate 2%-10% per year.

REMODELING IN TRABECULAR BONE
Due to much larger surface to volume ratio it is more actively remodeled than cortical bone, with remodeling rate 10 times higher .
In trabecular bone 151days ; remodeling here is surface event.
Here osteoclasts digging a trench rather than tunnel and resulting structure that is formed is called a hemi cutting/filling cone .
Remodeling rate 20%-30% per year.

Hemi cutting/filling cone in showing the mechanism for coupling bone resorption to formation

Summary of remodelling processMicro cracks in bone causes
Release of inflammatory cytokines cells(prostaglandins,interleukin)&exposure of mineralised collagen to extracellular fluid
T- cells produce RANKL which induces osteoclasts histogenesis
RANKL stimulates preosteoclasts from circulatory blood through RANKL receptors to form osteoclasts
Bone resorption takes place
Growth factors are produced & they stimulate preosteoclasts to produce OPG
Mononuclear cells coat the irregular or scalloped resorbing surface with cementing surface
Perivascular cells migrate & differentiate to preosteoblast
Osteoblasts form new bone

Control of Remodeling Two control loops regulate bone
remodeling
Homeostasis in the blood (negative feedback)
Hormonal mechanism maintains calcium
Mechanical and gravitational forces acting on the
skeleton

Hormonal Mechanism
Rising blood Ca2+ levels trigger the thyroid to release calcitonin
Calcitonin inhibits bone resorption and stimulates calcium salt deposit in bone
Falling blood Ca2+ levels signal the parathyroid glands to release parathyroid hormone (PTH)
PTH signals osteoclasts to degrade bone matrix and release Ca2+ into the blood










Fracture & Repair of Bone
Healing is faster in bone (vascular) than in cartilage (avascular)Repair is still slow due to BV damage
Clinical treatment
- closed reduction: restore pieces to normal position by manipulation
- open reduction: realignment during surgery





Aging & Bone Tissue The loss of Ca+2 from bone
matrix (demineralization)
may result in osteoporosis
rapid in women age 40-45
( when estrogen levels decrease )
begins after age 60 in men
Decreased rate of protein synthesis
less collagen production
less growth hormone
brittle bones more likely to fracture

CONCLUSION Bone physiologic concepts have important clinical
applications in orthodontics & dentofacial orthopaedics
A detailed knowledge of the dynamic nature of bone physiology is important for successful orthodontic practice.
Mechanical adaptation of bone to forces used in Orthodontics is the physiologic basis of Orthodontics and dento-facial orthopedics.

REFRENCE:
• Physiology- Robert M. Berne Fifth Edition
• Physiology- sembulingam
• Anatomy- gray’s anatomy
• Craniofacial growth- Sridhar premkumar
• Wikipedia, the free encyclopedia

THANK YOU