Anemia Hemolitik
-
Upload
winda-a-panjaitan -
Category
Documents
-
view
10 -
download
0
description
Transcript of Anemia Hemolitik
-
HEMOLYTIC ANEMIA:OVERVIEWSri MulatsihHematology-oncology, Pediatric Department, Sardjito Hospital, Faculty of Medicine, Gadjah Mada University2004
-
OVERVIEW
Normal RBC life span is 110-120 days
-
OVERVIEW
With age:Decreased membrane lipid componentSpherocytic shapeLess pliable and deformableTrapped and removed by the RE system
-
CLINICAL PRESENTATIONPatients may present with a variety of symptoms due to anemia
Related to tissue hypoxiaFatigue, weakness, lightheadedness, CP, SOB
Related to cardiovascular compensationTachycardia, palpitations
Related to underlying etiology
-
CLINICAL PRESENTATION
JAUNDICE
SCLERAL ICTERUS
SPLENOMEGALY
-
LABORATORY EVALUATIONInitialCBCP with MCVReview peripheral blood smearReticuloctye count (retic. count)LDHBillirubin-direct and indirectConsider haptoglobin, urinalysis
-
LABORATORY EVALUATIONAdditional / Directed studiesCoombs testUnderlying disordersOsmotic fragility testHgb electrophoresisG-6PD assaysEnzyme assaysBone marrow aspirate / biopsyReversed M:E ratio
-
DEFINITIONHemolysisAny situation resulting in accelerated destruction of RBCs (lifespan < 120 days)
Anemia may or may not be present
-
Site of Hemolysis
Extravascularvs.Intravascular
-
EXTRAVASCULARHEMOLYSIS90% OF CASES
Inappropriate removal of RBCs by the RE system
Exaggeration of the normal removal of RBCs
-
EXTRAVASCULARHEMOLYSIS
-
INTRAVASCULARHEMOLYSIS10% of all cases
Red cells are disrupted in the general circulation
Free hemoglobin is released into the plasma
-
INTRAVASCULARHEMOLYSIS
-
INTRAVASCULARHEMOLYSISBy products of intravascular hemolysis include:
HemoglobinemiaHemoglobinuriaHemosiderinuriaLow haptoglobin
-
HEMOLYSIS
Most hemolytic anemias have an element of both extravascular and intravascular destructionEx. sickle cell anemia
-
MECHANISM OF HEMOLYSIS
INTRINSICVS.EXTRINSIC
-
INTRINSICReason for hemolysis is intrinsic to the RBC itself:
membrane disordersmetabolic disordershemoglobin variants
-
Membrane Disorders:Hereditary SpherocytosisMost common cause of hereditary hemolytic anemia in Caucasians
1/5000 incidenceHeterogeneous molecular basisMost commonly AD inheritanceDeficiency of membrane proteinsSpectrin, ankyrin, band 3
-
Membrane Disorders:Hereditary Spherocytosis
-
Membrane Disorders:Hereditary Spherocytosis
Often the hemolysis is well compensated
Very diverse clinical presentation
History of gallstones is common
Splenectomy often very effective
-
Membrane Disorders:Hereditary Spherocytosis
-
Hereditary Spherocytosis Common
Diverse clinical presentationSometimes diagnosed in adulthood
Diverse molecular defects
Spherocytes, osmotic fragility test
-
Paroxysmal Nocturnal Hemoglobinuria (PNH)Acquired stem cell disorder:
Anemia, leukopenia, thrombocytopeniaHypocellular bone marrowIntravascular hemolysisRisk for thrombosis
-
PNHDefect leads to the lack of a phosphatidylinositol-glycan (PIG) anchor protein
Lack of multiple related surface proteins which depend on the missing anchoring protein
Make rbc more prone to lysis by complementChronic intravascular hemolysis
-
PNHPreviously diagnosed by:Hams testSucrose hemolysis test
Now use flow cytometry to detect cells missing various cell surface antigens /proteinsCD-59
-
INTRNSICReason for hemolysis is intrinsic to the RBC itself:
membrane disordersmetabolic disordershemoglobin variants
-
INTRINSICMature RBC requires glucose metabolism for energy requirements (ATP):Maintenance of protein integrity, cell deformability, shapePreservation of heme iron in ferrous formModulation of oxygen affinity of hemoglobin
Main playersGlycolytic pathway-90% of RBC ATPHMP shunt- generates reduced glutathioneNucleotide salvage pathways
-
Metabolic DisordersDue to defects in:
Glycolytic pathwayPyruvate kinase deficiency most commonPurine metabolismPyrimidine metabolismHexose-monophosphate shunt
-
Metabolic Disorders: G-6PD DeficiencyHMP shunt functions to maintain glutathione in a reduced stateGeneration of NADPH
Essential co-factor for detoxifying H2O2Essential for ability of RBC to withstand oxidant stressFailure leads to oxidation and damage to hemoglobin, enzymes, and membrane
-
Metabolic Disorders: G-6PD DeficiencyG-6PD catalyzes the first step in the HMP shunt
X-linked recessive inheritance
Most common metabolic disorder of RBCsEsp. in African American males (10-15%)
-
Metabolic Disorders: G-6PD DeficiencyHallmark is acute hemolysis following exposure to a variety of oxidant drugs or stressorsAntimalarial- AcidosisSulfonamides- InfectionNitrofurantoin- Fava beanVitamin K
-
Metabolic Disorders: G-6PD DeficiencySuspect when bite cells seen on peripheral smear in the presence of acute hemolytic anemia
Heinz body staining is often positive
More definitive tests available
Dont send during acute crisis
-
INTRINSICReason for hemolysis is intrinsic to the RBC itself:
membrane disordersmetabolic disordershemoglobin variants
-
Hemoglobin variantsNumerous inherited abnormalities in the hemoglobin molecule or synthesis make theRBC prone to premature hemolysis
Sickle cell syndromesThallassemiasUnstable hemoglobins
-
INTRINSICReason for hemolysis is intrinsic to the RBC itself:
membrane disordersmetabolic disordershemoglobin variants
-
EXTRINSICReason for hemolysis has nothing to do with intrinsic properties of RBC itself
Immune mediated
Red cell fragmentation
Infection
-
EXTRINSIC:IMMUNE MEDIATEDShortened RBC survival due to antibody or complement coating the red cell surface
AutoimmuneWarmCold agglutinin disease
DrugsMultiple mechanisms
-
AUTOIMMUNE HEMOLYTIC ANEMIA (AIHA)Typically either IgG or IgM / complement coat the RBC surface:
Recognized as abnormal by RE system
Leads to hemolysis (IgG)
Agglutination (IgM / C3)
-
AUTOIMMUNE HEMOLYTIC ANEMIA (AIHA)
Spherocytes (IgG) or agglutination (IgM) typically noted on the peripheral blood smear
-
AIHAWarm autoimmune hemolytic anemiaRBCs coated with IgG Reactive at room/warm temperaturesAcute and severeYounger age groupFix complement poorlySpleen is primary site of destructionSpherocytes seen on blood smearIdiopathic, collagen vascular, lymphoproliferative disorders
-
WARM AIHA :BANYAK SFEROSIT
-
AIHAWarm autoantibody hemolytic anemiaTreatment is primarily steroids Splenectomy is often second line
Other immunosuppressants are second/third line
-
AIHACold agglutinin diseaseRBCs coated with IgM which fixes complementReactive at cold temperaturesOlder age groupIntravascular site of destructionAgglutination noted on blood smear unless warmedPost infectious, lymphoma, idiopathic
-
Agglutination
-
AIHACold agglutinin diseaseTreatment includes avoidance of cold
Usually need to try catatonic therapy if persistent
Plasmapheresis in refractory cases
-
AIHACoombs testCritical in the evaluation of AIHA
Anti-globulin reagent prepared by injecting human globulin into animals-antibody isolated
IgGC3
Mixed with patient rbc or serum and test for clotting in the test tube
-
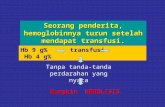
Yang di tes :Eritrosit penderita
-
Coombs ResultsExamplesDAT: warm antibodyIgG3+ (strong)C3negative or weak
DAT cold agglutininIgGnegative /weakC33+
-
ExtrinsicReason for hemolysis has nothing to do with the RBC itselfImmune mediated
Red cell fragmentation
Infection
-
RBC FragmentationMicroangiopathic Anemias
Schistocytes and microspherocytes noted on the blood smear
High shear stress leads to intravascular hemolysisMicrovascular diseaseDIC, TTP etc.Heart valveTrauma / implanted devices
-
RBC FragmentationMicrovascular disease
DIC-microvascular thrombosis due to activation and consumption of platelets, clotting factors
RBCs hemolyzed as they flow through the micro-environment of the damaged vasculature
Almost always secondary to underlying catastrophe
Present with bleeding or clotting
Treat underlying disease with blood product or anticoagulant support
-
RBC FragmentationMicrovascular disease
Thrombotic Thrombocytopenic Purpura (TTP)Microangiopathic hemolytic anemiaThrombocytopeniaMental status changesRenal failureFevers
Treatment is plasma exchange procedures
-
ExtrinsicReason for hemolysis has nothing to do with the RBC itselfImmune mediated
Red cell fragmentation
Infection
-
ExtrinsicInfectionClostridia sepsisParasitesmalariaVirusesBacterial
-
SUMMARYLocation of defect:
Intrinsicvs.Extrinsic
Membrane Hb Metabolic Immune Infectious Mechanical
-
SUMMARYLocation of hemolysis:
Extravascularvs.Intravascular
-
SUMMARYInitial evaluation and labs similar:CBC, MCV, Retic count, review blood smearLDH, billirubin, haptoglobin, UA
Further workup and treatment are specific to the suspected cause of hemolysisEx. DAT, electrophoresis, osmotic fragility test
BM usually not necessary, unless you need to rule out and underlying lymphoprolifera-tive or primary BM disorderReversed or decreased M:E ratio
-
CaseA woman in her thirties has a long history of SLE. She has had many complications of her disease. She now presents with worsening dyspnea, shortness of breath, and chest pain. Cbc shows a hgb of 7.3 gm/dl, hematocrit of 24%, normal wbc and platelets. You suspect AIHA. Which of the following lab data would not support this diagnosis?a. Macrocytosis / elevated MCVb. Elevated indirect billirubinc. Positive Direct Coombs testd. Elevated LDHe. Low reticulocyte count
-
CaseA previously healthy 34 year-old African American female was treatedwith bactrim (trimethoprin/sulfamethoxazole) for a UTI. She presents 4 days later with extreme fatigue, lethargy and weakness. Lab evaluation reveals a marked hemolytic anemia. You suspect G-6PD deficiency and request to review the peripheral blood smear. Which of the following findings would most support your diagnosis?
a. bite cellsb. schistocytesc. spherocytesd. sickle cellse. target cells
-
CaseA previously well 34 year old male presents with fever, mental status changes, thrombocytopenia, hemolytic anemia, and renal failure. You suspect TTP, with a microangiopathic intravascular hemolytic anemia as the underlying diagnosis. All of the following could be expected on laboratory evaluation except:a. low serum haptoglobinb. schistocytes on peripheral blood smearc. positive direct Coombs testd. hemoglobinuriae. elevated LDH
-
CasesA 45 year-old male is referred for evaluation of a hemolytic anemia. He has no obvious underlying infection, malignancy or vasculitis. You suspect he has a AIHA. You order a direct Coombs test and are told it is strongly positive with IgG, but negative with complement at room temperature. This data:a.) supports the diagnosis of cold agglutinin diseaseb.) supports the diagnosis of warm autoimmune hemolytic anemiac.) supports both diagnosisd.) supports neither diagnosis as no underlying disease is identified