Adrenal Glands Incidental Om A
-
Upload
rapid-surgeon -
Category
Documents
-
view
237 -
download
0
Transcript of Adrenal Glands Incidental Om A
-
8/4/2019 Adrenal Glands Incidental Om A
1/48
Adrenal Incidentaloma
By Wichien Sirithanaphol
-
8/4/2019 Adrenal Glands Incidental Om A
2/48
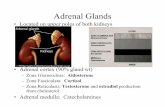
Adrenal Glands
Paired, mustard-
colored structures Retroperitoneal space
Superior and slightly medial to the kidneys
Level of the 11th ribs
Measures 5 x 3 x 1 cm and weighs 4 to 5 g
Blood flow of 2000 mL/kg/min
-
8/4/2019 Adrenal Glands Incidental Om A
3/48
-
8/4/2019 Adrenal Glands Incidental Om A
4/48
Embryology
Outer : cortex Inner : medulla
Adrenal cortex
- Mesodermal tissue near the gonads on the adrenogenital ridge
- Ectopic adrenocortical tissue : ovaries, spermatic cord and testes
Adrenal medulla
- Ectodermal in origin
- Arises from the neural crest
-Migrate to the para-aortic and paravertebral areas andtoward medial aspect of adrenal cortex to form the medulla
- May also be found in neck, urinary bladder, and para-aortic
-
8/4/2019 Adrenal Glands Incidental Om A
5/48
Neural creast
adrenal medulla
ganglia of the sympathetic trunk
sympathetic plexus
adrenal cortex
undifferentiated gonad
-
8/4/2019 Adrenal Glands Incidental Om A
6/48
The Adrenal Incidentaloma
Incidentally discovered adrenal masses Discovered through imaging
CT and MRI
Unrelated/nonadrenal disease
First described in the early 1980s
1
4 % of abdominal imaging studies > 60 years: greater than 4 %
-
8/4/2019 Adrenal Glands Incidental Om A
7/48
Differential diagnosis
-
8/4/2019 Adrenal Glands Incidental Om A
8/48
-
8/4/2019 Adrenal Glands Incidental Om A
9/48
Diagnosis
Signs and symptoms : hypersecreting hormone
Conn syndrome
Cushing syndrome
Pheocgromocytoma
If no signs and symptoms
Non-functionig VS Functioning tumor
Benign VS malignant
Need Biochemical studies or imaging studies?
Follow up VS adrenalectomy
Open VS laparoscopic adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
10/48
-
8/4/2019 Adrenal Glands Incidental Om A
11/48
Diagnostic hormonal test
Low dose (1mg) dexamethasone test 24-hour urine cortisol level
24-hour urine
Catecholamines
Metanephrines
Vanillylmandelic acid
Plasma metanephrine
Serum electrolytes
Plasma aldosterone
Plasma renin
Subclinical Cushing's syndrome
Pheochromocytoma
Aldosteronoma
-
8/4/2019 Adrenal Glands Incidental Om A
12/48
Imaging studies
CT scan
Homogenous and well-encapsulated
Smooth and regular margins
Hypoattenuating lesions (< 10 Hounsfield units)
Hyperattenuating (> 18 Hounsfield units)
Inhomogeneous
Irregular borders
Evidence of local invasion
Adjacent lymphadenopathy
Adrenal adenoma
Adrenal cancer
-
8/4/2019 Adrenal Glands Incidental Om A
13/48
Aldosteronoma
-
8/4/2019 Adrenal Glands Incidental Om A
14/48
Aldosteronoma
-
8/4/2019 Adrenal Glands Incidental Om A
15/48
Left adrenocortical cancer
-
8/4/2019 Adrenal Glands Incidental Om A
16/48
Left-sided pheochromocytoma
-
8/4/2019 Adrenal Glands Incidental Om A
17/48
Right-sided pheochromocytoma
-
8/4/2019 Adrenal Glands Incidental Om A
18/48
Imaging studies
MRI(T2-weighted imaging)
Low signal intensity when compared to the liver
Adrenal mass : liver ratio less than 1.4
Adrenal mass : liver ratio 1.2 - 2.8
Adrenal mass : liver ratios greater than 3
Adrenal adenoma
Adrenal cancer
Pheochromocytomas
-
8/4/2019 Adrenal Glands Incidental Om A
19/48
Right adrenal pheochromocytoma
Left adrenal pheochromocytoma
with central cystic change
-
8/4/2019 Adrenal Glands Incidental Om A
20/48
Radionuclide imaging
NP-59 (131I-6-iodomethyl-19-norcholesterol) Uptake of NP-59 : benign lesion (adenoma)
Absence of imaging : non-adenomatous lesion
Need to be given cold iodine 1 week before the study
MIBG (I131 metaiodobenzyl guandine)
Pheochromocytoma
-
8/4/2019 Adrenal Glands Incidental Om A
21/48
-
8/4/2019 Adrenal Glands Incidental Om A
22/48
FNA biopsy
Under CT guidance
Widespread use for the diagnosis of many endocrine lesions
Cannot be used to distinguish adrenal adenomas from carcinomas
Useful in patient with a Hx of cancer and a solitary adrenal mass
Pheochromocytomas : Hypertensive crisis
-
8/4/2019 Adrenal Glands Incidental Om A
23/48
Management algorithm for Adrenal incidentaloma
-
8/4/2019 Adrenal Glands Incidental Om A
24/48
Management algorithm for Adrenal incidentaloma
-
8/4/2019 Adrenal Glands Incidental Om A
25/48
Adrenal surgery
-
8/4/2019 Adrenal Glands Incidental Om A
26/48
Choice of procedures
Laparoscopic Adrenalectomy
Lateral Transabdominal Approach
Posterior Retroperitoneal Approach
Open Adrenalectomy
Anterior Approach
Posterior Approach
Lateral Approach
-
8/4/2019 Adrenal Glands Incidental Om A
27/48
Laparoscopic Adrenalectomy
First by Gagner (1992)
Less pain, mortality, hospital stay
New gold standard
Indication
Small hormone-secreting adrenal tumor
Samlll virilizing adenomna
Conn syndrome
Cushing syndrome
Incidentaloma larger than 5 cm
Contraindication
Previous surgery
Large adrenal gland (larger than 10-15 cm)
Suspected carcinoma of adrenal gland
Malignancy risk
-
8/4/2019 Adrenal Glands Incidental Om A
28/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
29/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
30/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
31/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
32/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
33/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
34/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
35/48
Laparoscopic Adrenalectomy: Lateral Transabdominal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
36/48
Laparoscopic Adrenalectomy: Posterior Retroperitoneal Approach
More direct access to the adrenal gland
Avoids abdominal adhesions
Bilateral adrenalectomy
Working space is limited vascular control difficulty
Unsuitable for large (>5 cm) lesions
-
8/4/2019 Adrenal Glands Incidental Om A
37/48
Laparoscopic Adrenalectomy: Posterior Retroperitoneal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
38/48
Laparoscopic Adrenalectomy: Posterior Retroperitoneal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
39/48
Laparoscopic Adrenalectomy: Posterior Retroperitoneal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
40/48
Transperitoneal VS Retroperitoneal Approach
-
8/4/2019 Adrenal Glands Incidental Om A
41/48
-
8/4/2019 Adrenal Glands Incidental Om A
42/48
Open Adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
43/48
Open Adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
44/48
Open Adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
45/48
Open Adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
46/48
Laparoscopic VS open Adrenalectomy
-
8/4/2019 Adrenal Glands Incidental Om A
47/48
-
8/4/2019 Adrenal Glands Incidental Om A
48/48
Thank You