Anatomy of adrenal glands
description
Transcript of Anatomy of adrenal glands

Diseases of adrenal glands and hypophysis. Еthiology, pathogenesis, Diagnostics. Clinical pattern. Complications. Principles of treatment. The role of a doctor-dentist in early diagnostics and prophylaxis.

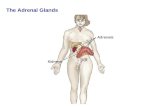
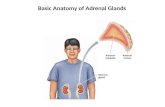
Anatomy of adrenal glands
Location: the top of the kidney and weighting approximately 5 g each.
Vascularization: a. suprarenalis superior (from a. phrenica inferior), a. suprarenalis media (from aorta abdominalis), a suprarenalis inferior (from a. renalis).
Innervation: n. splanchnicus major (through plexus celiacus and plexus renalis), fibrae n. vagus and n. phrenicus.
kidney
Left renal artery
a. suprarenalis inferior
Left adrenal veinLeft adrenal gland
Left ovaria vein
Ovaria arteries
Right ovariavein
Rena vein
Rightadrenal vein
Vena cava inferior
a. supranenalis superior
Aorta
a. suprarenalis mediaa. phrenica inferior

Anatomy of adrenal glands
The adrenals are divided into:1) outer area or cortex,
which includes three zones: - Glomerular (glomerulosa)- Fascicular (fasciculata)- Reticular (reticularis)
2) inner area or medulla

The pituitary gland is the “master gland”, which lies in a bony structure, the sella turcica, located at the base of the skull. The gland is a small organ about I cm long; it weighs 500 mg and is divided into two parts, anterior (adenohypophysis) and posterior (neurohypophysis).
The anterior pituitary secretes- corticotropin (ACTH)- Prolactin- Somatotropin (growth hormone (GH)- gonadotropins [follicle-stimulating (FSH)
and luteinizing (LH) hormones]- thyrotropin (TSH)- melanocyte-stimulating hormones (MSH).In the nerve endings of the posterior
pituitary are stored - Vasopressin (antidiuretic hormone, ADH)- Oxytocin

The hypothalamus plays an important role in hormone regulation by secreting a series of small peptides which stimulate or inhibit the synthesis and release of hormones by the anterior
pituitary Realising Inhibiting- CRG- TRG- LGRG- FSRG- GRH - GIH (somatostatin)- PRG - PIF (dopamine)- MRG - MIH

Action of mineralocorticoids:regulation of electrolyte balance in the organism:
increasing the level of sodium (by sodium retention in distal nephron, colon, salivary gland)
decreasing the level of potassium (by excretion).

Action of glucocorticoids: increasing of glycogen synthesis in liver
and decreasing of glucose utilization by peripheral tissues, increasing gluconeogenesis;
increasing of protein synthesis in liver and decreasing of its synthesis in muscles and increasing of protein destruction in muscles;
increasing of lipolisis; anti-inflammatory function and
immunomodulation; cardiovascular regulation (increasing of
blood pressure).

Regulation FEEDBACK:
Hormone secretion → delivery to target cells → hormone recognition by receptors in target cells → biologic effect → hormone degradation → signal from target cells to stop further hormone secretion

Regulation of secretion
glucocorticoids’ and androgens’ secretion is regulated by hypothalamic – pituitary system

mineralocorticoids’ secretion is regulated by the renin – angiotensin system, the level of Na+, K+ in blood, and to a lesser extent of ACTH

Action of catecholamines: modulate vascular tone; increase heart rate; antagonize insulin action.

CHRONIC ADRENOCORTICAL INSUFFICIENCY.
It is an insidious and usually progressive disease resulting from adrenocortical hypofunction.

Classification.
1. Primary adrenocortical insufficiency (Addison’s disease).
2. Secondary adrenocortical insufficiency .

Etiology of adrenal insufficiency:Primary:
autoimmune processes (50 – 65 %); tuberculosis; neoplasm, metastatic carcinoma; inflammatory necrosis; amyloidosis; heamochromatosis; bilateral adrenal hemorrhage or infarction, intra –
adrenal hemorrhage (Waterhouse – Friedrichsen syndrome following meningococcal septicemia);
bilateral adrenalectomy; Secondary:
hypothalamic or pituitary disease (primary injury of these organs leads to insufficiency of ACTH secretion that cause the two – side atrophy of adrenal glands);
glucocorticoid therapy.

Pathogenesis.
Deficiency of adrenal hormones contributes to the hypotension and produces disturbances in carbohydrate, fat, and protein metabolism, and severe insulin sensitivity.

Symptoms and signs. Presentation may be acute and chronic.
Frequently clinical signs of the primary chronic adrenocortical insufficiency are manifested in that time when adrenocortical tissue is destroyed on 70-90 %.
The most common complaints are:- weakness,- malaise,- weight loss,- anorexia,- depression.

Objective examination:1. Hyperpigmentation (in patients with
primary adrenal insufficiency) is characterized by diffuse tanning of both exposed and nonexposed portions of the body, especially on pressure points (bony prominences), skin folds, scars, and extensor surfaces, black freckles over the forehead, face, neck, and shoulders; bluish – black discoloration of the areolas and the mucous membranes of the lips, mouth, rectum and vagina are common. After compensation hyperpigmentation will decrease. Patients in 15 – 20 % of cases may have areas of vitiligo (depigmentation) as the sign of autoimmune process.


Objective examination:1. Hypotension or postural hypotension (88 – 90 %) with
syncopal attacks can occur.2. Tachycardia.3. Weight loss (due to dyspeptic syndrome, true muscle
tissue catabolism, dehydration).4. Anorexia, nausea, vomiting, abdominal pain, diarrhea
are often. Gastritis, ulcer disease can occur.5. Decreased cold tolerance, with hypometabolism may
be noted.6. Sexual disorders.7. Neurologic and psychiatric disorders: decreasing of
the memory, mental activity, concentration of attention, depressions, hallucinations can occur due to chronic hypoglycemia which leads to changes of metabolism in brain tissue.
8. Hypoglycemia.There are three stages of severity: mild, moderate and
severe.

Laboratory findings.1. A low serum Na level and a high serum P level
together with a characteristic clinical picture suggest the possibility of Addison’s disease.
2. Adrenal insufficiency can be specifically diagnosed by: low levels of plasma glucocorticoids and
mineralocorticoids, or urinary 17 – hydroxycorticosteroid (17 – OHCS) or 17 – ketogenic steroid (17 – KGS);
demonstrating failure to increase plasma cortisol levels, or urinary 17 – OHCS or 17 – KGS excretion, upon administration of ACTH (in patients with primary adrenal insufficiency, those with secondary adrenocortical insufficiency will have a significant increase in plasma cortisol or 24 - h urinary corticosteroid levels.)
3. To distinguish between primary and secondary adrenal insufficiency, me have to find the level of plasma ACTH: primary shows increased, and secondary shows decreased level.

Instrumental findings.
1. The ECG may decreased voltage and prolonged P – R and Q – T intervals.

Treatment.I. Etiologic: appropriate treatment of
complicating infections (e.g., tuberculosis).II. Pathogenic:1. Diet (enough quantity of proteins, vitamins,
salt and water).2. Glucocorticoids (normally, glucocorticoids are
secreted maximally in the early morning hours, little being secreted at night).
Average dosage is: cortisol: 20 – 25 mg daily; prednisolone 5 – 7.5 mg daily; hydrocortisone 30 – 40 mg orally daily. 2/3 of the dose can be given in the morning
and 1/3 in the afternoon. Night doses should be avoided, as they may produce insomnia.

3. Mineraloocorticoids. DOCSA 5 mg orally daily should be used in
patients with severe and moderate duration or fludrocortisone 0.1 – 0.2 mg orally once a day is recommended (this mineralocorticoid replaces aldosterone)
4. Intercurrent illnesses (e.g., infections) should be regarded as potentially serious and the patient should double his dosage until he is well.
5. If nausea or vomiting preclude oral therapy, medical attention should be sought immediately and parental therapy started.

Adrenal crisis -
is a medical emergency caused by sudden marked insufficiency of adrenocortical hormones.

Precipitating factors.1. stress (infection (especially with
septicemia), trauma, surgery, prolonged fasting, salt loss due to excessive sweating during hot weather);
2. sudden withdrawal of adrenocortical hormone therapy in patients with chronic insufficiency.

Clinical features. An adrenal crisis is characterized by- profound asthenia, - severe pains in the abdomen, lower
back or legs; - nausea, vomiting, diarrhea; - peripheral vascular collapse; - renal failure with azotemia. - Body temperature may be subnormal,
through severe hyperthermia due to infection is often seen.

Treatment.
Therapy should be instituted immediately once a provisional diagnosis of adrenocortical failure has been made.
Substitution therapy Rehydration Treatment of complications
(hyperpyrexia, psychotic reactions).

Treatment. hydrocortisone 100 – 150 mg as a water –
soluble ester (usually the succinate or phosphate) is injected IV or acetate IM
followed by infusion of 1 L of 5 % glucose – in – saline solution containing 100 mg hydrocortisone ester given over 2 h.
Hydrocortisone acetate 50 – 75 mg IM each 4 – 6 h
Hydrocortisone therapy is given continuously to a total dosage in 24 h of 400 – 600 – 800 mg.
After stabilization of BP (>100 mm Hg) we decrease the dosage of hydrocortisone acetate to 25 - 50 mg IM to 2 - 4 times a week

Treatment. Mineralocorticoids are not required
when high – dose hydrocortisone is given
In a case of prominent hypotension DOKSA (5 mg), ftorhydrocortisone (cortinef 0,05 – 0,2 mg), fludrocortisone acetate (0.1 mg) have to be used
Total infusion of saline and 5 % glucose - 2,5 – 3,5 l during first day

Prognosis. With a substitution therapy, the
prognosis is excellent and a patient with Addison’s disease should be able to lead a full life.

PHEOCHROMOCYTOMA.It is a tumor of chromaffin cells that secrete catecholamines
- Rare: 5 per 100 000 hypertensives- Sporadic: 75 – 85 %- Hereditary: 15 – 25 %- Malignant: 3 – 36 %- Occurs equally in men and women- Peaks in 3rd – 5th decades

The term pheochromocytoma
(phios means dusky, chroma means color, and cytoma means tumor) refers to the color the tumor cells acquire when stained with chromium salts

Etiology is unknown
- In about 80 – 90 % of cases, pheochromocytomas are found in the adrenal medulla, but may also be found in other tissues derived from neural crest cells (e.g., tumors may be found in the paraganglia of the sympathetic chain, retroperitoneally along the course of the aorta, in the carotid body, at the aortic bifurcation, in the GU system, in the brain, and in the dermoid cysts.

Classification.1. Paroxysmal form (45 %).2. Permanent form (50 %): with crisis; without crises.3. Latent or silent form
(nonsymptomatic).

Clinical features- hypertension, - Tachycardia, diaphoresis, postural
hypotension, tachypnea, - flushing, - cold and clammy skin, severe headache,
angina, palpitation, - visual disturbances, dyspnea, parasthesias- nausea, vomiting, epigastric pain,
constipation or diarrhea and a sense of impending doom are common; some or all of these symptoms and signs may occur in any patient.

Symptoms “The 5 P’s”- Pressure increase
(hypertension )- Palpitation (tachycardia)- Perspiration - Pain (abrupt onset of
throbbing headache, chest (angina), abdominal pain)
- Pallor (due to vasoconstriction) cold and clammy skin

Other signs- postural hypotension or shock
(epinephrine secretion)- tremor- visual disturbances- dyspnea- parasthesias- nausea, vomiting, - severe constipation or diarrhea
and a sense of impending doom are common;
- weight loss- anxiety- some or all of these symptoms
and signs may occur in any patient.

Paroxysmal attacks may be
- spontaneousor provoked by
- palpation of a tumour, - postural changes, - abdominal compression or massage,- induction of anesthesia, - emotional trauma,- β – adrenergic blocking agents,- rarely, micturition.

Duration of hypertensive crisis is variable
- from a seconds or few minutes to hours,- but 50 % of the paroxysms last less than 15
min.
- Permanent form of the disease’s duration looks like malignant hypertension.
- Nonsymptomatic form of the disease is rare.

Physical examination- hypertension- retinopathy - cardiomegaly - (but last two are
often less extensive than might be expected for the degree of hypertension present)

Investigations1. An increased 3-h (24-h) urinary
excretion of epinephrine, norepinephrine and their metabolic products (VMA or metanephrines).
2. Increased plasma epinephrine, norepinephrine.
3. CT scanning, MRI of the abdomen for the localization of the tumor.
4. A scan with iodine I 131–labeled metaiodobenzylguanidine (MIBG) is useful for extra – adrenal tumors.

Treatment1. Surgical removal of the tumor
is the treatment of choice.2. During crisis a combination of α- and β-
adrenergic blocking agents- phentolamine (tropaphen) 2 - 4 mg every
5 - 10 min till stopping of the crisis,- phenoxybenzamine 10 – 20 mg 3 – 4
times daily, - propranolol 30 – 60 mg/day- and infusion of sodium nitroprusside.

Etiology of hypothalamo – pituitary disorders
1.Trauma2. Infectious diseases:- acute (scarlet fever, influenza)- chronic (tuberculosis, malaria, toxoplasmosis)3. Tumor or metastasis4. Vascular damaging (thrombosis, thromboembolia)5. Metabolic disorders (xanthomathosis)6. Congenital pituitary hypo – or aplasia (syndrome
of “empty sella turcica”7. Genetic predisposition8. Idiopathic

Pituitary tumors Slow – growing (benign) 10 – 15 % of all brain tumors
Clinical presentations:1. Mass effect:- Visual deffects - Headaches- Seizures- Facial pain or numbness- Apoplexia - Nausea, vomiting 2. Hormonal effects (overproduction or deficiency)

Classification of hypothalamo – pituitary disorders Adenohypophysis disorders1. Secretion of GH- overproduction: acromegaly, giantism- dificiency: pituitary dwarfism2. Secretion of ACTH- overproduction: Cushing’s syndrome, hypothalamic
syndrome3. Secretion of Prolactin- overproduction: hyperprolactinemia, galactorhea-
amenorhea4. Secretion of TSH5. Secretion of Gonadotropines: adiposogenital-dystrophy6. Hypopituitarism7. Hypothalamic obesity Neurohypophysis disorders1. Deficiency of vasopresin: diabetes insipidus2. Inapropritiative secretion of vasopresin

GROWTH-HORMONE EXCESS(acromegaly and gigantism)
Chronic, debilitating disorder resulting from excessive secretion of GH and resulting in production of insulin-like growth factor 1 (IGF-1), which lead to typical picture: gigantism before puberty and to acromegaly after puberty

Etiology1. Adenoma (acidophilic or chromophobe)
of the pituitary2. Ectopic GH-producing tumors (cancer of
lungs, mamma glands, pancreatic gland)
3. Regulatory hypothalamus disturbances (overproduction of somatoliberin or deficiency of somatostatin)
4. Ectopic GRH-producing tumors (carcinoid tumor of intestine,lungs)

Clinical manifestations of gigantism
Mass effects Overproduction of GH- height more than 190 cm in
women and 200 cm in men- Hypersecretion of GH prior
to closure of epiphysis leads to proportional growth of bones; both length and width of bones are increased
- May be blood hypertension, mycardial dystrophy, atrial fibrillation

Acromegaly
- Named “acromegaly” by Pierre Marie in 1886 from Greek akron (extremities) and megas (large)
- Rare disease- 3 – 4 new cases per million
population per year- Affects both sexes equally- Peak ages 40 – 60 years- Mortality 10 times higher
than in control group mostly due to cardiovascular disorders

Clinical manifestations of acromegaly
Syndromes connected with influence of GH on organs and tissues:
1) periostal overgrowth:- overgrowth of the
mandible leads to protrusion of the jaw (prognatism)
- there is an overbite and the teeth become separated (diastema).

2) cortical thickening(characteristic coarsening of the facial features)

3) Hypertrophy of soft tissues of hands and feet (the hands are widened and the fingers become broad, requiring a larger ring size. Similiar changes in the feet require a larger shoe size)4) arthropathy, carpal tunnel syndrome 5) Hypertrophy of tongue, sleep apnoe
6) The skin is thickened, andfemales may note hypertrichosis, excessive sweating

II. Changes from the inner organs:- Hepatomegaly and cardiomegaly- Hypertension is present in 40 % of patients - The kidney may also become enlarged, and renal clearance
of phosphate is frequently impaireIII. Syndrome of reproductive disturbances:- Amenorrhea, which occurs in as many as two-thirds of
female patients, may be the chief complaint. Decreased libido, impotention is experienced by one-third of the patients (due to prolactin – like effects of GH)
IV. Syndrome of endocrine disorder- thyromegaly is present in about 25 % of the patients
(hyper- and hypothyroidism occurs rarely) - the abnormalities in glucose metabolism (diabetes mellitus)- hyperfunction or deficiency of other pituitary trophic
hormonesV. Mass effects (headaches, vision field disorders)

Diagnosis of acromegaly is usually suspected from:
1. The patient's history2. Physical examination3. Laboratory investigations:- The level of GH (0,5 – 5,0
ng/ml)- Somatomedin-C- Test with glucose suppression
of growth-hormone secretion- Test with TRH- GTT

Value of old pictures

3. Enlargement of the sella turcica (90 % of patients) X-ray, CT,MRT
4. Visual - field defects (bitemporal hemianopsia)

Pharmacologic therapy1. A dopaminergic agonist and ergot
derivative, 2a-bromergocriptine (bromocriptine 10 to 60 mg/day, (clinical remissions in 73 % patients, normalization of GH level in 22 % of patients).
2. Comatostatin analogues: octreotide, sandostatin (clinical remissions in 90 % patients, normalization of GH level in 50 % of patients).

Treatment Surgery: - Transsphenoidal hypophysectomy is the procedure of
choice. Advantages: effectivity in nearly 90 % of the patients, simplicity
and low morbidity. Side effects: hypupituitarism, diabetes insipidus, recurrence of symptoms.- Craniotomy is reserved for large tumors with
suprasellar extension and involvement of the optic chiasm.
- Cryohypophysectomy (destruction of the pituitary by cold injury) can reduce the secretion of GH (without causing hypopituitarism) in 88 % of the patients.
External irradiation:- External beam- Gamma knife

HYPOPITUITARISM It is the syndrome, which is
characterized by deficiency of one or more anterior pituitary hormones.
Epidemiology- affects mostly women at age 20 - 40

EtiologyPrimary:- pityitary aplasia, hypoplasia, - tumors (chromophobe adenomas,
craniopharyngiomas, pituitary cysts) - postpartum uterine hemorrhage (Sheehan's
syndrome)- autoimmune and infiltrative (hemochromatosis,
sarcoidosis) processes- Infectious (tuberculosis, fungi)- pituitary irradiation or surgery- traumatic or surgical destruction of the
hypothalamic-pituitary areaSecondary: Hypothalamic disorders

Classification Total or
panhypopituitarism Partial
hypopituitarism with isolated deficiency of one or two hormones

The symptoms of hypopituitarism mimic those of many diseases.
Watch for pituitary insufficiency: 1. In women who fail to lactate following pregnancy
and delivery. (Involution of breasts and sparse axillary and pubic hair would suggest the diagnosis.)
2. In females with unexplained arnenorrhea, particularly if symptoms of ACTH and TSH deficiency or increased intracranial pressure are present.
3. In males with decreased libido and loss of axillary and pubic hair.
4. In patients with unexplained anemia. 5. In diabetic patients who experience a reduction in
insulin requirements.)

Clinical manifestations
are not present unless 75 % of the gland is destroyed.
1) Hypogonadism (early symptom)2) Hypothyroidism3) Hypocorticism4) In children: growth retardation; in
adult weakness, muscle atrophy, cachexia
5) Neuro – psychiatric changes, hypothalamic disorders (vegetative crises, thermoregulation disorders)
6) Mass effects

Diagnosis 1. Physical examination 2. Laboratory findings anemia, hypercholesterolemia, tendency to
hypoglycemia hormonal assessment (decreased levels of
pituitary and peripheral endocrine glands) 3. Instrumental investigations X-ray of cella turcica (the upper limits of normal for
sellar dimensions are length 17mm, depth 13mm, and width 15mm ) CT,MRT
Cerebral angiography Ophthalmologist (fields of vision, retina)

Treatment - eliminating the underlying cause - replacing the deficient hormones- Pituitary tumors should be removed surgically,
although irradiation and drug therapy (bromocriptine) are also available.
- Treatment of acute and chronic infection Hypothalamic peptides or pituitary hormones are not
suitable for hormone replacement : (1) The human hormones are difficult to oblain in pure form; (2) because of their nature and short halh-life they have to be given parenterally and frequently; (3) since they stimulate antibody formation, their activity is lost a few weeks after initiation of therapy.
Under these circumstances the usual practice is to administer the hormones produced by the target glands. They are available in pure form and are relatively inexpensive.

Replacement therapy Hydrocortisone 20 - 30 mg/day, prednisolone 5 -
15 mg/day Replacement with gonadal steroids is never
indicated until puberty normally occurs. These agents in high doses can fasten bone maturation and epiphyseal closure, thereby limiting the height which may ultimately be reached.
- In males testosterone therapy is recommended. - Premenupausal females with ovarian failure
should be treated with estrogens. Thyroid drugs (L-thyroxin, euthyrox) Vitamines, anabolic hormones

DIABETES INSIPIDUS is a clinical disorder characterized by the excretion of large quantities of diluted urine and caused either by failure of ADH release
(hypothalamic diabetes insipidus) or by lack of response of the tubules to normal
quantities of circulating ADH (nephrogenic diabetes insipidus).

Etiology. Causes of hypothalamic diabetes insipidus:1. Surgery2. Trauma 3. Tumors (craniopharyngioma) or metastatic
(carcinoma of the breast).4. Infiltration of the hypothalamus by leukemic
cells, granuloma (sarcoidosis, tuberculosis), histiocytes (Hand-Schuller-Christian disease), or infections..
5. Idiopathic.6. Familial.
Causes of nephrogenic diabetes insipidus1. Hereditary factors: X-linked transmission with
predominance in males.2. Acquired factors (Drugs: Lithium carbonate,
demeclocycline. methoxyflurane. and amphotericin. Renal disease)

Clinical picture
1. The hallmark of diabetes insipidus is the excretion of large quantities of urine (usually 5 to 10 L/day, but the amount can be more). In mild forms of diabetes insipidus, polyuria may be minimal with urine volumes of 2 to 4 L/day.
2. Polydipsia (ingesting of large amounts of mostly cold water).
3. Insomnia, decreasing of appetite, dryness of skin and mucous membranes, pharyngitis, gastritis, constipation are common in patients.
4. In situations in which the patient has no access to water, is unconscious, or has an abnormality of the thirst mechanism, severe dehydration may ensue.

Diagnosis1. The patient's history2. Physical examination3. Laboratory signs:- a specific gravity of less than 1,005 - an osmolality is less than 100 mosmol/kg- serum osmolality is increased. - level of ADH can be decreased4. Instrumental, neurological,
ophthalmoscopic examination

Treatment Etiologic Pathogenetic- Hypothalamic DI- Adiurecrin powder nasal spray0,03 g 1 – 3 times a day- Adiuretin in drops 1 – 3 times a day- Synthetic lysine vasopressin, desmopressin 1 to 2 sprays
three or four times a day.- Pituitrin 0,5 – 1 ml subcutaneous 2 – 3 times a day.- Nephrogenic DI- chlorpropamide 100 to 500 mg/day- Tegretol (400 mg/day)- diuretics (thiazide diuretic (50 to 100 mg/day of
hydrochlorothiazide) is added to enhance the sodium depletion and impair the ability of the tubules to generate a dilute urine)

Thank you!