Using Diagnostic Wax-Ups and Preparation Guides to...
Transcript of Using Diagnostic Wax-Ups and Preparation Guides to...

INSIDE DENTISTRY JULY/AUGUST 2008
insideFSTHetlCS
"...diagnostic wax-ups and preparation guides
can be invaluable tools to help ensure esthetic,functional, and restorative success..."
Using Diagnostic Wax-Ups and PreparationGuides to Facilitate Accurate and EstheticDiastema Closure and Functional Bite AlterationThomas E. Dudney. DMD
Closing a didStema can be a chal-lenging and difficult task that may find theclinician restoring or working with multi-ple teeth to ensure the equalization of space,or removing some tooth structure—suchas from the distal surface of teeth—to beable to "move" subsequent teeth mesially.'Unfortunately, in some instances, dentistsmay attempt to close diastemas withoutremoving sufficient tooth structure fromthe surrounding dentition, or without al-tering or adjusting the gingival zeniths ofthose teeth. The result could be the crea-tion of an awkward and unwanted trian-gular appearance of the teeth, or leavingthe teeth with an inappropriate width-to-length ratio that compromises their effortsto create the more pleasing and durablesmile their patients wanted.2 To avoid suchscenarios, diagnostic wax-ups and pre-paration guides can be invaluable tools tohelp ensure esthetic, functional, and res-torative success by facilitating and en-hancing the treatment planning process.3
For example, when closing a diastemaand creating the illusion of tooth move-ment with indirect porcelain/ceramic res-torations, it is important for ceramists tobe able to "wrap" the porcelain interproxi-mally through the entire thickness of thetooth, as opposed to just halfway throughthe interproximal space. This need arisesfrom the fact that the darkness of themouth will create a shadowy effect in thespace between the teeth, thereby neces-sitating thicker ceramic material. As a re-sult, clinicians may need to perform slicepreparations on the distal aspects of theselected teeth and, consequently, movethe gingival zeniths in a mesial direction
to help maintain the proportionality ofthe teeth.
Such a plan of action may seem to becommon sense. However, in the midst oftreatment planning, the value of a diag-nostic wax-up is the ability to visualizewhat will be needed to execute a successfulclinical and treatment protocol to achievethe desired end result.3 This article demon-strates the use of a diagnostic wax-up andpreparation guides during the treatmentof a patient who presented primarily for es-thetic concerns (ie, midline diastema, toothcolor, ceramometal crown) and who alsorequired alteration of his bite (ie, chang-ing the end-to-end bite relationship of hisanterior teeth to a normal overbite andoverjet, with anterior guidance within thepatient's envelope of function).
CASE PRESENTATIONA 47-year-old man presented for consul-tation because he was unhappy with theappearance of his smile. Specifically, hedid not like the midline diastema, the colorof his teeth, or the ceramometal crownon tooth No. 9 (Figure 1 and Figure 2). Aninitial examination was performed thatincluded radiographs and diagnostic rec-ords, full-arch polyvinyl siloxane impres-sions (Aquasil Ultra, DENTSPLY Caulk,Milford, DE), a centric relation bite rec-ord, and a facebow transfer (Artex® Face-bow, Jensen Industries, North Haven, CT).It was during this examination that itbecame apparent that the patient demon-strated an end-to-end bite relationshipof his anterior teeth (Figure 3); any treat-ment plan developed would need to alterthis relationship to one with a normal
Thomas E. Dudney, DMDPrivate PracticeAesthetic, General, and Restorative Dentistry
Alabaster, Alabama
overbite and overjet. Multiple photographsshowing the teeth in full-facial smile, oc-clusal (Figure 4 and Figure 5), and re-tracted views were also obtained.4 All ofthis information was forwarded to thelaboratory so that the ceramist could cre-ate a diagnostic wax-up, putty matrix,and preparation guides.
TREATMENT PLANNINGAfter the initial examination and afterreviewing all of the recorded informa-tion, the treatment goals were developed.These included addressing the patient'sconcerns and additionally changing theend-to-end bite relationship of his ante-rior teeth to one with a normal overbiteand overjet, with anterior guidance with-in his envelope of function. Specifically,the diastema would be closed, which re-quired that the size and shape of his teethbe altered,5 and he would be given a whiter,brighter smile. Therefore, the diagnosticwax-up—and the related clinical tools (eg,putty matrix and preparation guide)—were imperative to the success of the case.The resulting treatment plan called for 10maxillary and 10 mandibular restorations(ie, teeth Nos. 4 through 13 and 20 through29 with feldspathic porcelain veneers[Ceramco®, DENTSPLY Prosthetics, Bur-lington, NJ] and a feldspathic all-porce-lain crown on tooth No. 9).
The diagnostic wax-up enabled thepreoperative visualization of the proposed
changes (Figure 6), as well as the creationof the provisional restorations that wouldsimulate the proposed changes intraorally.To accomplish that, a putty matrix wasfabricated (Sil-Tech putty, Ivoclar Viva-
Figure 1 and Figure 2 Preoperative full-
facial and close-up views of trie patient and his
smile.The midline diastema is obvious, as is the
tooth discoloration, particularly of tooth No. 9.
Figure 3 This preoperative retracted view of the patient demonstrates his end-to-end bite relation-
ship. This would be altered to a normal overbite and overjet, with anterior guidance within the patient's
envelope of function.

INSIDE DENTISTRY JULY/AUGUST 2008
dent, Amherst, NY) from the diagnosticwax-up. Furthermore, the diagnostic wax-up was used to create incisal reductionand facial reduction preparation guidesthat aided in idea] tooth preparation (Fig-ure 7A and Figure 7B). Such guides areespecially beneficial in a case such as thiswhen a diastema is being closed and abite is being changed.
PREPARATION PROTOCOLDuring preparation, a .05-mm depth-cut-ting bur (843-016, Brasseler USA, Savan-nah, GA) was used to establish uniformdepth of the preparations, after which a6844-016 bur (Brasseler USA) was usedto complete the preparations. All marginswere equi-gingival at the facial aspect andslightly subgingival interproximally toallow for the proper emergence profile ofthe restorations6 (Figure 8 and Figure 9).
A soft tissue diode laser (Twilight, Bio-lase Technologies, Irvine, CA) was used tocreate ideal gingival symmetry and movethe gingival zenith in a mesial direction toavoid the appearance of restorations withan excessive mesial-axial inclination and/or an exaggerated triangular shape.7'8 Theliterature has demonstrated that if themesiodistal spaces are not symmetrical andthe gingival scallops are not in alignment,the esthetics associated with diastema clo-sure can be compromised (Figure 10).'
It is important to note that in cases suchas this with a large midline diastema, it isoften necessary to reduce the distal aspectof all the anterior teeth slightly to ensuresufficient room for widening each sub-sequent tooth in a mesial direction, assuggested earlier. When this is not ac-complished and space is closed only byadding porcelain to the mesial aspect ofthe central incisors, it is very difficult toachieve an ideal length-to-width ratio(ie, 75% to 80%); the final result will beteeth that appear too wide and unesthetic.2Rather, in this case a slice preparation inthe form of a feather edge was extended ina palatal direction to the mesio-lingualor disto-lingual line angle of the toothto allow the ceramist to wrap porcelainthrough the interproximal contact area.9When the preparations were completed,they were verified using the preparationguides to ensure proper incisal and facialreduction and sufficient spacing for thediastema closure.
Full-arch polyether impressions (Im-pregum™, 3M ESPE, St. Paul, MN) weretaken, along with an occlusal record (Van-illa Bite Registration, Discus Dental, Cul-ver City, CA), stick bite, a facebow transfer(Artex Facebow), and a shade of pre-pared teeth (stumpf shade 9). In additionto the preoperative photographs, addi-tional images of the preparations weretaken for use by the dental laboratory infabricating the definitive restorations. Adetailed laboratory prescription discus-sing the goals for the case, the patient'sconcerns, and the final desired shade wasalso sent. Feldspathic porcelain was cho-sen because the prepared tooth color was
Figure 4 and Figure 5 Maxillary and mandibular occlusal view photographs were taken of the
patient as part of the initial examination and forwarded to the laboratory for creation of the diagnostic
wax-up. Note the midline diastema.The size and shape of the patient's teeth would be changed in the
final restorations.
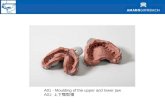
Figure 6 Photograph illustrating how a diag-
nostic wax-up is used to demonstrate how a
patient's smile would be changed. A putty
matrix/reduction guide is in place on this wax-
up. Note: this wax-up is not of the current case.
Figure 7A and Figure 7B Facial and palatal photographs illustrating how a preparation guide is used
to assist in the reduction of the affected teeth. Note: this putty matrix/reduction guide is not of the current case.
Figure 8 Facial view of the completed maxil-
lary and mandibular preparations.
Figure 9 Occlusal view of the mandibular prepa-
rations demonstrating the reduction and movement
effect of the slice-preparation technique.
fairly light, and powder/liquid ceramicsare highly translucent yet very durablewhen bonded to the tooth;10 in the handsof a talented ceramist, they can create verynatural, life-like esthetics.
PROVISIONALIZATIONThe provisional restorations were creat-ed using a putty matrix of the diagnosticwax-up and a temporary material (Luxa-temp®, Zenith DMG, Englewood, NJ) inshade Bl. The margins were finished, thegingival embrasures opened, and the oc-clusion adjusted, after which the temporarieswere polished (Figure 11). The provis-ionals were critical to the success of thiscase because they served as a blueprint forthe final restorations and allowed the pa-tient to evaluate a simulated result andoffer feedback. Furthermore, the patientwas able to return for a post-provisional-ization appointment to evaluate func-tion and esthetics, at which time the newbite (Figure 12) was evaluated in all ex-cursive movements; the length was alsoverified with phonetics.
The goals for the occlusion were equal-intensity centric stops, no posterior con-
Figure 10 Occlusal view of the maxillary prepa-
rations after alteration of the gingival zeniths. Note
that the gingival zeniths have been moved in a
mesial direction to allow for the new position of
the restorations.
tact in lateral and protrusive movements,and anterior guidance within the patient'senvelope of function." By simulating thefinal result in the provisional restorations,it was possible to achieve the desired re-sults and then communicate this informa-tion to the laboratory for the fabricationof the definitive restorations. All of thisinformation was transferred to the labo-ratory with impressions and photographsof the approved provisional to furtherfacilitate communication.
CEMENTATION OF THEFINAL RESTORATIONSAt the insertion appointment, the provi-sional restorations were carefully removed,and the preparations were cleaned withhydrogen peroxide and disinfected with achlorhexidine rinse (Consepsis®, Ultra-dent Products, Inc. South Jordan, UT).The definitive restorations were tried inwith water individually and then alto-gether to evaluate fit, marginal integrity,color, and esthetic integration. After ap-proval from the patient, the restorationswere set aside to be etched, rinsed, dried,and silanated in preparation for cemen-
Figure 11 View of the provisional restorations,
which are critical to the success of trie case because
they serve as a blueprint for the final restorations.
tation while the teeth were isolated witha rubber dam.
The restorations were bonded to theteeth using a total-etch technique with afifth-generation bonding agent (Prime &Bond® NT™, DENTSPLY Caulk) and alight-cured luting cement (Variolink® Ve-neer, Ivoclar Vivadent) in shade +1. Excesscement was cleaned from the facia] surfaceswith cotton rolls and brushes. The restor-ations were then tacked in place at thegingival margin using a 3-mm curing lighttacking tip for 5 seconds per tooth. Excesscement was then removed interproximallywith dental floss, after which the restora-tions were light-cured for 1 minute eachfrom the facial and lingua] surfaces usingan LED curing light (bluephase® 16i,Ivoclar Vivadent).
The interproximal contacts were pol-ished using diamond finishing strips (Bra-sseler USA), and the occlusion was checkedand adjusted where necessary. Finally, therestorations were polished using rubberpoints (Ceramiste™, Shofu Dental Cor-poration, San Marcos, CA) and polishingpaste (Porcelize™, Cosmedent, Chicago,IL) on a felt wheel.

INSIDE DENTISTRY JULY/AUGUST 2008
Figure 12 Close-up retracted view of the pro-
visional restorations demonstrating the new bite
relationship of the overbite and overjet that were
copied from the diagnostic wax-up.
Figure 13 Final postoperative full-facial view
of the patient in natural smile.
Figure 14 Final postoperative close-up view of
the patient in natural smile. Note the natural-look-
ing and esthetic length-to-width ratio of the teeth
and seamless color blending of the restorations.
Figure 15 Final postoperative retracted
view demonstrating the patient's corrected
bite relationship.
The patient returned for a postopera-tive follow-up appointment, at which timeminor occlusal adjustments were madeand the restorations were repolished. Thepatient was able to function normally,with both lateral and protrusive guidance,was able to speak normally, and statedthat he was very happy with the appear-ance of his smile and his appearanceoverall. It was determined that the goalsof the case had been achieved (Figure 13through Figure 15).
CONCLUSIONThe primary objectives of this case in-cluded dosing the maxillary midlinediastema while maintaining the propor-tionality of the teeth, thereby ensuringthat they would not appear too wide orartificial. Additionally, the crown on toothNo. 9 needed to match seamlessly withthe surrounding veneer restorations torestore the patient's happiness with thecolor and appearance of his smile. There-fore, a whiter, brighter smile was createdfor the patient. Finally, the patient's end-to-end bite was corrected to a proper biterelationship, one with an overbite andoverjet and anterior guidance that wouldgive him long-term function. Paramountto the successful completion of this casewas proper communication between thedentist and the laboratory technician/cer-amist, as well as between the dentist andthe patient. To this end, the diagnosticwax-up, preparation guides, and puttymatrix used to create the provisional res-torations were essential to the communi-cation process, proving instrumental inaiding both dentist-laboratory and den-tist-patient communication during thetreatment planning stages.12 By develop-ing an ideal treatment plan with propercommunication and execution, the goalsof treatment were met and patient satis-faction was achieved.
ACKNOWLEDGEMENTThe author wishes to acknowledge AdrianJurirn from Jurim Dental Studios in GreatNeck, NY, who fabricated the ceramicrestorations featured in this article.
REFERENCES1. Jones LA, Robinson MY. A case study: es-
thetic and biologic management of a diastema
closure using porcelain bonded restorations
for excellent and predictable results. Journal
of Cosmetic Dentistry. 2002;18{3):72-83.
2. Gurel G. The Science and Art of Porcelain
Laminate Vfeneers. Chicago, IL: Quintessence
Publishing. 2003.
3. Garcia LT, Bohnenkarnp DM. The use of diag-
nostic wax-ups in treatment planning. Compend
Cont/n Educ Dent. 2003;24{3):210-214.
4. Snow SR. Strategies for successful esthetic
dental treatment. J Calif DentAssoc. 2007;
35{7):475-484.
5. Kinderknecht KE, Kupp LI. Aesthetic solu-
tion for large maxillary anterior diastema and
frenum attachment. Pract Per/odontfcs Aes-
thet Dent. 1996 ;8{1):95-102.
6. Gurel G. Predictable, precise, and repeatable
tooth preparation for porcelain laminate ven-
eers. Pract Proced Aesthet Dent. 2003;15
{!): 17-24.
7. StabholzA, ZeltserR.Sela M, Peretz B,etal.
The use of lasers in dentistry: principles of
operation and clinical applications. Compend
Contm Educ Dent. 2003;24{12):935-948.
8. Kokich VO, Kokich VG, Kiyak HA. Perceptions
of dental professionals and laypersons to
altered dental esthetics: asymmetric and
symmetric situations. Am J Orthod Dento-
facia! Orthop. 2006;130{2):141-151.
9. Rouse JS. Full veneer versus traditional
veneer preparation: a discussion of inter-
proximal extension. J Prosthet Dent. 1997;
78{6):545-549.
10. Nash RW. Ultrathin porcelain veneers: es-
thetics without aggressive tooth reduction.
Contemporary Esthetics and Restorat/Ve
Practice. 2007;11(11):12-17.
11. Parker MW. The significance of occlusion in
restorative dentistry. Dent din North Am.
1993;37{3):341351.
12. Chaimattayompol N, Wong SX. Diagnostic
management of interdental spacing. J Pros-
thet Dent 2000;84(4):467-469.