tissue Changes in Patients Following spinal Cord Injury ...€¦ · typically include weight and...
Transcript of tissue Changes in Patients Following spinal Cord Injury ...€¦ · typically include weight and...

34 ostomy wound management® February 2014 www.o-wm.com
Feature
tissue Changes in Patients Following spinal Cord Injury and Implications for wheelchair Cushions and tissue Loading: a Literature review Amit Gefen, PhD
abstractPersons using wheelchairs, especially those with spinal cord injuries (SCI), may be susceptible to tissue changes that affect their risk for pressure ulcer (PU) development. To examine the complexity of the problem of designing, selecting, and prescribing an optimal cushioning solution to help prevent PUs, a literature search was conducted examining factors that affect the biomechanical interactions of the seated buttocks with the cushion and how these factors may change over time. The majority of publications retrieved were preclinical studies and case studies, and just a small fraction was randomized clinical trials. The literature indicates that external and internal anatomy and tissue structure and function change considerably in the months and years following the loss of sensation and mobility. Specifically, these changes typically include weight and fat mass gain, skeletal muscle atrophy and fat infiltration into muscles, bone loss and bone shape adaptation at the pelvis, vascular perfusion changes, and microstructural changes in skin and muscle that are as-sociated with disuse and affect the biomechanical behavior of these tissues. Support surfaces, particularly wheelchair cushions, should be designed to accommodate microchanges that occur for a seated person throughout the day (eg, changes in posture and position or muscle tone) as well as macrochanges in anatomy, tissue composition, and long-term tissue (patho)physiological changes. Cushions must be tailored to, and adapted for, each individual patient on a regular basis. A promising and practical bioengineering approach to fit cushions to different patient conditions is to use computer simulations (finite element [FE] modeling). As understanding about PU risk in this population increases, study designs can be refined to develop a much-needed evidence-base for the appropriate use of support surfaces in general and wheelchair cushions in particular.
Keywords: review, spinal cord injuries, pressure ulcer, tissues, durable medical equipment
Index: Ostomy Wound Management 2014;60(2):34–45
Potential Conflicts of Interest: Dr. Gefen’s efforts to investigate the effects of cushioning materials and designs on buttocks tissues during weight-bearing were funded by ROHO, Inc, Belleville, IL. The author is also the Chair of ROHO’s Scientific Advisory Board.
Dr. Gefen is a Professor in Biomedical Engineering, Department of Biomedical Engineering, Faculty of Engineering, Tel Aviv University, Tel Aviv, Israel; and President, European Pressure Ulcer Advisory Panel. Please address correspondence to: Prof. Amit Gefen, Department of Biomedical Engineering, Faculty of Engineering, Tel Aviv University, Tel Aviv, 69978 Israel; email: [email protected].
the current, most fundamental guidelines for prevention of sitting-acquired pressure ulcers (PUs) are to use a soft
cushion on the wheelchair that is thick enough to allow ad-equate immersion to distribute buttocks-support loads while preventing undesirable bottoming-out.1 Patients who suffer a spinal cord injury (SCI) are routinely prescribed cushions for their wheelchair as part of their rehabilitation process, with the aim of avoiding PUs and particularly the severe type deep tis-sue injury (DTI), which is a PU with an internal onset, typical-ly in skeletal muscle tissues near the ischial tuberosities (ITs).2
Healthcare providers agree that use of appropriate cushions is critical for protecting SCI patients from PUs and DTI, but what exactly is “appropriate” is unclear. The abundant variety of cushioning solutions includes flat foams, segmented foams, contoured foams, water/gel-filled cushions, honeycomb-like cushions, and air-cell-based cushions. Analysis of the current literature in an attempt to understand which cushion technol-ogy is superior or most cost-effective is inconclusive. This is not surprising, given the difficulties and costs involved in ran-domized clinical trials for isolating the efficacy of a cushion. DO N
OT DUPLIC
ATE

February 2014 ostomy wound management® 35www.o-wm.com
tIssue Changes In wheeLChaIr users
Perhaps the most thorough and rigorous cushion trial was conducted by Brienza et al.3 This group published extensive randomized clinical trials and secondary data analyses from trials4,5 of nursing home populations (not SCI patients). However, as they stated in their own work, a key problem in these trials is the ability to isolate the effect of the cushion from that of the wheelchair. If the cushion is ideal but the wheelchair does not fit properly or is improperly adjusted, the patient will sit in a compromised posture (eg, posterior pelvic rotation or pelvic obliquity), increasing the risk for PUs. In their 2010 study, Brienza et al3 finally were able to eliminate this problem by fitting and adjusting wheelchairs to each of their participants (180 subjects, all nursing home residents who reached the study endpoint of a 6-month fol-low-up), which is a remarkable achievement involving sub-stantial cost and effort. The authors tested several segmented foam or skin protection cushions that were randomly allo-cated to the study participants. The skin protection cushions were assigned within that category based on clinical needs and preferences, and included air, viscous fluid plus foam, and gel plus foam cushions. Given the incidence rate of PUs was higher in the patient group prescribed segmented foam cushions than the group given skin protection cushions, the researchers concluded the segmented foam cushions were less protective against PUs. A commentary by Beeckman and Vanderwee6 notes several additional factors are extremely difficult to control in such large-scale cushion trials — eg, standardizing the method of assessing skin viability/dam-age, handling interobserver differences, and standardizing repositioning in the wheelchair. Taken together, these studies illustrate the challenges of conducting clinical trials in this area and underscore the need for complementary research methods, particularly bioengineering laboratory studies and computer simulations, to help prioritize cushion technolo-gies and products. That said, current research highlights the primary biomechanical goals quality therapeutic and preven-tive cushions should definitely meet: minimization of inter-face pressures (IP),4 minimization of internal sustained tissue deformations, and particularly, minimization of localized de-formations in skeletal muscles under the ITs.7-10
To examine the complexity of the problem of designing, selecting, and prescribing an optimal cushioning solution to help prevent PUs, a literature search was conducted focusing on factors that affect the biomechanical interactions of the seated buttocks with the cushion and how these factors may change over time. The relevant English language literature from the last 20 years was searched using PubMed for terms such as pressure ulcers, sitting, buttocks tissues, support surfaces and cushions, spinal cord injury, deformation injury, and biome-chanics. The majority of publications retrieved were preclinical studies and case studies, and just a small fraction was random-ized clinical trials. The focus of the literature search was on SCI patients who typically undergo dramatic changes in struc-tural anatomy and tissue physiology following their injury that
evolve and progress throughout life. However, some of these structural and physiological changes, particularly adaptation of muscle and skin tissues to disuse, are also relevant to the elderly and infirm. These complex and interacting changes are reviewed and then analyzed as to how they could theoretically influence the considerations for cushion design and selection for the SCI patient population. It is expected that nurses, phys-ical therapists, rehabilitation practitioners, and other medical professionals will find this information relevant to their day-to-day patient care and practice.
microchanges that affect tissue Loading As used here, microchanges affecting tissue loading refer to
changes that relate to the daily functioning of SCI patients — eg, changes in posture or movements, the individual adher-ence to guidelines for PU prevention such as the frequency of postural changes and performance of push-up maneuvers, and factors that concern the pathophysiology of the SCI con-dition, such as the muscle tone around the regions at risk.
Sitting posture and use of the upper extremities. Even without considering any SCI-specific pathoanatomy or pathophysiology, the factor with the most fundamental effect on soft tissue loading during wheelchair sitting is wheelchair position and momentary posture. Shabshin et al11 was the only group to investigate in vivo buttocks tissue compressive deformations near the ITs in healthy volunteers during sitting in various body tilts utilizing weight-bearing seated magnet-ic resonance imaging (MRI). The tissue deformations were digitally measured in a coronal T1-weighted MRI sequence. Each image was evaluated for thickness of fat tissues between the skin and the gluteus muscles and of muscle tissues be-tween the ITs and fat. Measurements in the weight-bearing
Key Points• Theauthorreviewedtheavailableliteratureaboutthe
biomechanical interactions of the seated buttocks with cushions, especially among spinal cord injury patients, and how these factors may change over time.
• Theliteratureshowsexternalandinternalanatomyand tissue structure and function change consider-ably over time, which may increase the risk of tissue and skin damage.
• Anidealwheelchaircushionshouldbecarefullytai-lored to the individual and be adequately adjustable to accommodate the (patho)physiological changes that occurr over time.
• Evidencealsosuggestscushionswearout,soindi-viduals should be assessed and the cushion evaluat-ed and replaced regularly to protect the person from pressure ulcers and deep tissue injury.
ostomy wound management 2014;60(2):34–45
DO NOT D
UPLICATE

36 ostomy wound management® February 2014 www.o-wm.com
Feature
and non-weight-bearing positions were compared per par-ticipant for calculation of compressive tissue deformations in each trunk tilt. Mean muscle compressive deformation in their study, from highest to lowest, was 20˚ lateral-tilt (ex-tent of deformation = 87%); lateral 10˚ (85%), anterior 20˚ (79%), anterior 40˚ (74%), and neutral (72%). Fat compres-sive deformation was highest (and statistically similar) with anterior tilts of 20˚ and 40˚ (42%), followed by lateral 20˚ tilt (41%), lateral 10˚ (39%), and neutral (35%). Hence, a slight tilt of the trunk to the side as in imbalanced sitting or during a lateral reaching movement in healthy persons can increase mean muscle deformation by at least 15% and fat deforma-tion by at least 7%. This is a considerable added extent of de-formation, particularly because soft tissue deformations are already substantial during balanced sitting.12 Any additional unilateral excessive loading that persists may push these tis-sues above tolerance levels and cause cell and tissue death in insensate individuals, as demonstrated in animal (rodent) and tissue-engineered in vitro models.13,14 These biomechani-cal data highlight the rationale for preferring cushions that support the body in a balanced, stable posture and that allow maintaining a posture that is as balanced as possible through-out the day. Maintaining a balanced posture is particularly important in individuals with SCI, because these persons typically have less-than-optimal postural alignment, as indi-cated in a study of four Brazilian participants with paraplegia and an additional four with tetraplegia.15 Nevertheless, this does not necessarily overlap the goal of maximizing tissue protection against PUs. In other words, even if the posture appears to be balanced in the wheelchair, it does not auto-matically mean the cushion also is optimizing tissue loads; theoretically, even a completely rigid support can provide balanced sitting but produce extremely large tissue deforma-tions in both sides of the buttocks, which would compromise tissue viability.
Another critically important factor the cushion affects is the patient’s ability to use his/her upper extremities, such as when performing reaching movements. Results of a study16 that tested balance and time to reach a target in 11 indi-viduals with SCI versus six individuals without SCI showed that patients with a SCI had more difficulties reaching than healthy individuals and that it takes persons with a SCI more time to accomplish activities, which has been attributed to a postural control deficit. Hence, SCI patients need special at-tention in terms of providing a sitting solution that will not just protect them from PUs, but also will allow adequate daily functioning. On the one hand, a stable pelvis and trunk are required as a base for steady upper extremity movements; on the other hand, functional range of motion increases by allowing the pelvis and trunk to move (up to a certain ex-tent). Therefore, as shown in a randomized, controlled test17 designed to monitor the sitting pressures and forces in nine individuals with SCI during reaching tasks, a good cushion should provide both pelvis and trunk support and sufficient
trunk mobility. Attention to these issues holds important consequences for patient quality of life.17,18 In a study exam-ining reaching movements in 22 American patients with SCI who used different cushions, Sprigle et al18 observed sitting with increased posterior pelvic tilts enhanced body stabil-ity and permitted greater reach. In general, because patients adopt different postures when using different cushions (and backrests), posture needs to be assessed along with the func-tional reach capacities on the selected cushion. These factors then should be considered with respect to the cushion’s ca-pacity to accommodate changes in position throughout the day, while keeping tissue deformation as minimal as possible.
Individual risk and prevention behavior. Individual awareness of PUs and cooperation with rehabilitation guide-lines, which essentially also affect the biomechanical inter-actions with the cushion, are additional considerations. In a preclinical computational simulation study, Levy et al19 in-vestigated buttocks tissue loading when sitting down after completing a push-up maneuver, as SCI patients often are taught to do. The research found substantial differences be-tween the loading curves of skin and fat when sitting on flat foams. Although fat tissues were loaded at a nearly constant rate during the sitting-down process, skin loads increased nonlinearly, with a greater load/time slope around the early skin-support contact — ie, the more sensitive period with respect to pressure is at initial skin-support contact when sit-ting down. Inclusion of scars associated with a history of PUs in their simulations indicated that, as expected, individuals with scars are more susceptible to further tissue damage. Spe-cifically, the study found risk for skin damage during sitting down is greater when a hypertrophic scar is present. Despite the fact that this was a theoretical modeling study with associ-ated limitations, it points to two important issues in the con-text of the present paper. The first is proper guidance of how to avoid PUs, which needs to accompany the prescription of the cushion, is required — ie, patients need to be trained to reposition themselves gradually and gently rather than “fall” back into the wheelchair after finishing a push-up maneu-ver. In other words, educating patients to use their cushion properly is a critical component of the sitting solution; a wheelchair cushion is probably not meant to be bought off-the-shelf without fitting and guidance. The second is, as re-flected in the Levy article19 and the literature reviewed within, the risk for PUs depends on the individual, his/her medical condition, and his/her history, and these need to be assessed rigorously while taking a holistic approach, tailoring the sit-ting solution to the individual.
Muscle tone. As already indicated, the SCI population needs special attention when considering sitting solutions, given the substantial tissue changes that occur from the time of injury and throughout life. One such fundamental change involves skeletal muscle tone. Spasticity, the exaggeration of normal reflexes that occurs in response to stimulation of the sensory system, is one of the most common neuromuscular
DO NOT D
UPLICATE

February 2014 ostomy wound management® 37www.o-wm.com
tIssue Changes In wheeLChaIr users
changes seen in SCI, affecting approximately 70% of this population within a year post injury.20 In able-bodied per-sons experiencing skin stimulation, a sensory signal is sent to the reflex arch in response. This signal travels to the brain via the spinal cord and is assessed in the brain. If the signal received does not indicate danger, such as from heat, injury, and the like, a subsequent inhibitory signal will be sent by the brain back through the spinal cord to cancel the reflex of the musculature. However, in individuals with SCI, inhibitory signals are blocked by the structural damage in the spinal cord; hence, the natural reflex is allowed to continue, result-ing in continuous muscle contractions (spasms). The imme-diate biomechanical implication is the stiffening/contraction of weight-bearing muscles (eg, the gluteal muscles) during the spastic event, inflicting greater mechanical stresses when supporting the body weight, with stress proportional to stiff-ness. However, Sopher et al21 investigated the effects of spastic events on muscle exposure to mechanical stresses by means of a biomechanical computer model and found increases in gluteal muscle stresses due to spasticity were mild. These findings correlated with a human study where no correlation was found between SCI-related-spasticity and occurrence of PUs.22 In fact, based on a cross-sectional study23 in 13 patients with an incomplete SCI from whom a spasticity score and MRI-derived muscle/fat masses were recorded, some authors suggested spasticity may be an important factor in defending skeletal muscle size and indirectly preventing intramuscular fat (IMF) accumulation early after incomplete SCI.
The other extreme of SCI-associated changes in muscle tone is flaccidity (ie, lack of muscle tone) that causes muscles to be limp and soft. This change is also theoretically hazard-ous because the muscles are less able to resist deformations, subsequently increasing the extent and exposure to intra-muscular deformations whenever in a weight-bearing pos-ture. As such, patients with flaccid paralysis may expose their muscles to greater deformation levels than persons with nor-mal muscle tone or persons with spastic paralysis. Interest-ingly, early in recovery from an injury to the central nervous system, muscles may gain tone and move from being flaccid to spastic (which is detected in neurological examinations as a velocity-dependent increase in stretch reflex in the absence of volitional activities).24 Hence, post the acute phase of SCI, muscle tissues in the buttocks may change tonus, either in continuous processes (gradual changes from flaccidity to spasticity) or transiently (during spastic episodes). An ap-propriate cushioning solution needs to consider and ideally accommodate these changes in muscle tone, considering the more flaccid the muscle tissue, the greater the intramuscular deformation levels are under weight-bearing circumstances.
macrochanges affecting tissue Loading
Macrochanges to tissues associated with the chronic phase of SCI and relevant to the risk for PUs and DTIs typically include increases in body weight and fat mass, bone shape
adaptation, muscle atrophy, and increase in IMF, as well as disuse-induced skin adaptation and changes to the macro- and microvasculature. These changes and their impact on the structural and functional anatomy of the buttocks are depicted in Figure 1.
Body weight. The literature presents considerable evi-dence demonstrating a tendency for major weight gain dur-ing the first year after a SCI. A retrospective chart review study25 in a US Department of Veterans Affairs SCI Unit (N = 85) showed the body mass index of two out of three pa-tients increases to overweight or obesity levels within this timeframe. It appears the majority of patients are unable to adequately decrease their caloric intake to match their lower level of activity and metabolic caloric needs. This can result in a weight gain of 1.3 to 1.8 kg per week for SCI patients undergoing rehabilitation (shown in 22 patients in their early rehabilitation phase),26 which occurs after the initial weight loss of 5.3 to 9.1 kg these patients experience shortly after the acute SCI due to hypercatabolism; nutrient deficiencies such as albumin, carotene, transferrin, ascorbate, thiamine, folate, and copper typically are documented at 2 weeks post
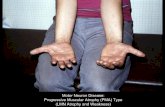
Figure 1. A schematic description of changes in the structural anatomy of the buttocks characteristic of the chronic phase of spinal cord injury (SCI). With respect to the baseline (healthy) seated anatomy of the buttocks a), within several months to a few years, a SCI patient is expected to gain bodyweight and fat mass, lose gluteal muscle mass, and experience flattening of the ischial tuberosities (IT) due to bone loss and adaptation, and also thinning of the skin around the IT regions; b) ad-ditionally, pathological increases in intramuscular fat contents are observed after the SCI, which is depicted as white stripes on the glutei and indicates a decrease in effective tissue stiffness under the ITs. S=skin, F=fat, GI=gluteus muscle.
DO NOT D
UPLICATE

38 ostomy wound management® February 2014 www.o-wm.com
Feature
injury.27 This weight change infers the size of the buttocks and weight of the trunk are changing over time and typically start to increase after the first few weeks post acute injury, which has implications for sitting. Elsner and Gefen28 and So-pher et al29 investigated the biomechanical consequences of this gradual weight gain on deformations in the gluteal mus-cles during sitting. It could be hypothesized that a high body (or trunk) mass may lead to a greater risk for PUs, particu-larly DTIs, due to the increase in compressive forces from the ITs on overlying deep soft tissues in the buttocks. Conversely, it is possible the extra body fat associated with overweight or obesity may reduce the risk for PUs by providing enhanced subcutaneous cushioning that redistributes high IP. The El-sner and Sopher computer simulation studies28,29 clearly and consistently showed being overweight, particularly when co-existing with muscle atrophy (which is typical in SCI as well), contributes to a state of elevated deformations in the glutei, which may increase the likelihood of PUs in general and DTI in particular in the overweight SCI population. However, on-going changes to the surface shape and size of the buttocks, as well as to internal anatomy (eg, thickness of fat tissue layers) in the SCI population in terms of the prescribed cushion also should be considered, but research addressing this specific problem still is lacking.
Skeletal changes. Bone adaptation due to disuse in SCI is clearly documented in the literature; primary adaptations include demineralization of epiphyses and thinning of the diaphyseal cortical walls below the injury level, with greater severe bone loss occurring in individuals with tetraplegia.30,31 Biomechanically, the bone loss is promoted by the absence of muscular loading via tendons, which is the primary stimulus for bone mass homeostasis in the able-bodied.32,33 In Giangre-gorio et al’s34 case study of two pairs of twins, where one of the twins suffered a SCI (at 7 years old, more than 20 years be-fore the data collection), the authors used computed tomog-raphy to measure volumetric bone mineral density (BMD) and bone geometry and found lower BMD in the hip, distal femur, proximal tibia, and (to a lesser extent) in the spine of the SCI twins. Lower moments of inertia were evident at the mid-femur and calf of the SCI twins, indicating cortical bone loss. Studying twins makes a powerful comparison because it eliminates the potential effects of age and genetics. Small co-hort prospective studies35 using dual X-ray absorptiometry, peripheral quantitative computerized tomography, and bio-mechanical test methods have demonstrated these catabolic changes in bone mass and shape occur within 2 years of the SCI, bone loss is more severe in tetraplegia than in paraple-gia, large variability exists with respect to anatomical site and across individuals, and gender-dependent differences also may exist.36 The consequences of lower BMD and thinner cortical tissues are (after several years) more fragile bones that, much like in metabolic syndromes, tend to break as a result of non-traumatic loading, including when trans-ferring to and from a wheelchair.30 Specifically with respect
to sitting, Linder-Ganz et al12 used MRI scans of seated SCI subjects and found shape adaptations of the ITs, which tend to flatten in SCI patients, possibly due to the chronic expo-sure to the sitting loads coupled with the ongoing loss of cor-tical bone mass. The Linder-Ganz data12 revealed 1.8-times greater radii of curvature of the ITs in the SCI patient group with respect to the controls. Hence, ideally, a sitting solution should consider the ITs are gradually changing shape (typi-cally flattening) in a SCI patient, which inevitably affects the load transfer from the weight-bearing ITs to the overlying soft tissues in the seated buttocks.
Disuse-induced muscle atrophy. Atrophy of skeletal muscle tissues is a well-known consequence of SCI. The at-rophy occurs below the injury level and at the muscle fiber scale. It includes thinning of the fibers, reduction in the num-bers of slow-twitch fibers, and an increase in fast-twitch fi-bers, which start as early as 4 to 6 weeks after the acute injury (inter-patient variations are considerable).37 The progressive process lasts at least several months and stabilizes between 1 and 6 years after the acute stage, with substantial variations across individuals. The lack of neuromuscular activity leads to microvascular changes as well, which generally cause a re-duced oxidative capacity and a greater risk for deformation-induced ischemia.
At the macroscopic scale, the denervation causes rapid muscle wasting. In a group of patients with incomplete SCI (ie, where damage to the spinal cord was not absolute), mus-cular cross-sectional area in the thighs decreased by one third 6 weeks after the acute injury, and this was accompanied by more than doubling of the IMF contents.38 In Giagregorio et al’s twin study,34 the averages of the cross-sectional areas of the thigh and calf muscles in the SCI twins were as low as approximately 30% of the values for their non-SCI twins. As could be expected, the extent of loss of skeletal muscle tissues depends on whether the spinal cord lesion is incomplete or complete. For example, at a mean time of 13 months from an acute incomplete injury, a reduction of 24% to 31% (tibi-alis anterior and quadriceps femoris muscles, respectively) was reported in Shah et al’s39 MRI study in 17 people, with a weak correlation with respect to use of a wheelchair. In Cas-tro et al’s study,40 where muscle biopsies were taken from 12 patients at 6, 11, and 24 weeks after a complete SCI, it was shown that complete spinal cord lesions can lead to muscle mass loss twice that found in the Shah et al39 study of incom-plete injuries.
Based on supine pelvic computed tomography scans with contrast in 10 able-bodied and 10 participants with SCI, Wu and Bogie41 recently reported gluteal muscle atrophy is rela-tively greater at the level of the ITs, which highlights the need to especially protect that region by means of a cushion dur-ing wheelchair sitting. Lastly, it should be noted muscle atro-phy also occurs with normal aging, partly due to neurological and endocrinal changes and partly due to cachexia and the reduced physical activity.42 Accordingly, as a SCI patient ages,
DO NOT D
UPLICATE

February 2014 ostomy wound management® 39www.o-wm.com
tIssue Changes In wheeLChaIr users
the disuse-induced muscle atrophy is superimposed with the aging-related atrophy.
Tissue composition and mechanical behavior. Muscle/fat. IMF normally functions as dynamic adipose
storage depots that are close to muscle fibers and hence ac-cessible for muscular metabolism. These depots can expand when lipids are available, and they tend to increase in non-SCI overweight or obese individuals (the percentage of IMF typically assessed in humans using MRI).43 In able-bodied individuals, the normal IMF level is 1% to 2% of the total fat stored in the body.44 In SCI patients, IMF can increase pro-gressively up to three to four times the healthy levels; after 8 to 10 years of denervation, the adipose tissues are nearly one third of the area in some muscle biopsies.38,45 Using compu-tational modeling, Sopher et al21 demonstrated how internal muscle tissue loads under the ITs are elevated during sitting by the increase in IMF contents, implying the more severe the IMF, the higher the risk for a DTI. The authors explained the rise in skeletal muscle loads observed with the increasing IMF contents by the greater intramuscular shear stresses at interfaces between muscle and IMF tissues. Wu and Bogie41
reported the IMF depots are not homogeneously distributed across SCI muscles but tend to concentrate proximally (so gluteal tissues near the ITs are prone to have excess IMF), and also that high IMF levels correlated with a history of severe and/or repeated PUs, which supports and complements the Sopher21 study. Wu and Bogie41 emphasized skeletal muscle quality and particularly IMF levels in the glutei need to be assessed in SCI individuals because they are an important measure of the risk for severe PUs, keeping in mind the IMF contents evolve and tend to accumulate with time after the acute injury.
From a biomechanical perspective, the build-up of IMF acts to decrease the effective stiffness of the glutei fat tis-sues (from animals) tested in vitro are less stiff than skeletal muscle.46,47 Computer simulations48 have shown this phe-nomenon gives rise to greater deformations in the glutei under a given body weight. In other words, the decrease in stiffness of the glutei due to the progressing increase in IMF contents causes the glutei to gradually bear greater sus-tained deformations, which then increases the risk for PUs and DTIs in particular, even if the patient does not become substantially heavier.
Skin. As previously discussed, disuse adaptation of the skin secondary to SCI is analogous to the degenerative processes in bone and muscle. In a study in Turkey employing high-frequency ultrasound, Yalcin et al49 compared skin thickness in the buttocks of 32 SCI patients to 34 controls and found the skin was substantially thinner over the ITs and sacrum in the SCI group (although the skin of individuals with SCI can thicken at other anatomical sites). Thinning of the skin at the load-bearing sites of a seated body appears to occur together with stiffening of the remaining skin tissues. In a study conducted in South Korea using a noninvasive suction
testing device in 48 male participants with chronic SCI and 48 age-matched healthy controls, Park et al50 demonstrated the skin was significantly less distensible in the SCI group (P <0.05). This change in the skin’s biomechanical behavior oc-curs in conjunction with, and as a result of, deficient vascular reactions, decreased fibroblast activity, and primarily higher collagen catabolism. The loss of stability of intermolecular collagen cross-links, which is evident in increased urinary ex-cretion of the biochemical residues of the disintegrated colla-gen in SCI, occurs months before these patients develop vis-ible PUs (demonstrated in analyses of 24-hour urine samples from 60 men with SCI who were followed-up prospectively in the US).51 These are all changes associated with the disuse of skin tissues. The Park et al50 study also reported the dura-tion of the SCI had a substantial impact on the changes in distensibility, elasticity, and viscoelasticity — ie, biomechani-cal skin properties. Taking the Yalcin49 and Park50 studies to-gether, the thinner and stiffer SCI skin tissues, particularly at the weight-bearing sites of sitting, must cause the mechanical stresses (eg, when a patient moves or is being moved) in the deformed SCI skin to increase. At the same time, the strength of the SCI skin should decrease due to the loss of the colla-gen cross-links at the material level and the loss of thickness of the skin structure.49-51 This places SCI patients at high risk for superficial (tension- and shear-related) PUs (in ad-dition to DTI) as a direct result of these skin changes. Inter-estingly, although not as widely reported as the degenerative musculoskeletal changes in SCI previously described, these skin changes are progressive and develop from the time of the acute injury,50 much like the disuse-induced musculo-skeletal changes.
Tissue perfusion. Autonomic impairments may lead to increased prevalence of cardiovascular abnormalities in SCI patients, which manifest in the macro- and microcirculation (the impaired microvascular reactivity in SCI is largely due to the sympathetic dysfunction over the cardiovascular sys-tem). With respect to macro-circulation, which was studied in a retrospective chart review,52 hypotension was found to occur more in patients with a high level SCI. Additionally, a meta-analysis53 showed individuals with a cervical SCI ex-hibit a lower resting systolic blood pressure in the seated ver-sus a supine position. Literature reviews summarizing data from muscle biopsies further report a gradual pathological decrease in numbers and sizes of capillaries that feed muscle fibers in skeletal muscle tissue of SCI patients.54,55 The fewer, narrower capillaries in SCI make the deformed skeletal mus-cles more prone to ischemia, particularly during episodes of low blood pressures. Although ischemic damage in weight-bearing muscles is now recognized to occur subsequent to direct deformation damage,9 it should be taken into account that muscle tissue in the SCI population becomes more sus-ceptible to ischemic damage with the time that elapses post acute injury, which is a consequence of the disuse-induced muscle atrophy. The author’s conclusion, based on the above
DO NOT D
UPLICATE

40 ostomy wound management® February 2014 www.o-wm.com
Feature
findings, is that when adding the systemic cardiovascular impairments, a given level of sustained muscle deforma-tions in the SCI patient causing obstructions of the intra-muscular vasculature will trigger ischemia sooner than in non-SCI subjects. This is yet another reason why skeletal muscle deformation should be minimized, especially in seated SCI individuals.
Skin, like skeletal muscle, also pathologically adapts in structure and function to conditions of disuse. The reactive hyperemia (ie, the microvascular response to re-establish-ment of blood flow after a period of a reduced flow due to, for
example, sustained tissue deformations) differs between SCI patients and healthy individuals. In a laser Doppler perfu-sion study,56 eight SCI patients experienced greater perfusion to the buttocks skin tissues following a period of pressure-induced obstruction of the skin vasculature than eight con-trol subjects. This probably indicates the skin of SCI patients experiences more severe ischemic conditions when loaded compared to a healthy skin response to the same loading con-ditions. Hence, the above-mentioned studies suggest muscle, as well as the skin of SCI patients, undergoes micro- and macro-structural changes over time. These changes, together with systemic cardiovascular changes, eventually cause these tissues to become more sensitive to development of ischemia when sitting for prolonged periods.
Interpreting Changes in tissue-loading Levels with respect to safe sitting times
Shabshin et al8 evaluated the impact of foam and gel wheel-chair cushion materials on deformations in the glutei during sitting in a group of healthy persons using a seated MRI set-ting that employs a “double-donut” MRI configuration. This configuration allows persons to sit in the magnet between the two donut-shaped structures that facilitate the imaging. The authors found the foam and gel cushions were able to decrease muscle deformations by 10%, with rather small dif-ferences in that parameter across the tested cushion materi-als (two foam and two viscoelastic types). At first glance, this may lead one to conclude there is little clinical significance between these two materials. However, putting these data in the context of the cell and tissue injury thresholds obtained for skeletal muscle by Linder-Ganz et al13 and later by Ge-fen et al14 clarifies that decreasing internal muscle deforma-tions, even to a mild extent, may contribute to a considerable increase in “safe” sitting time. The procedures used for ex-perimentally obtaining these cell/tissue injury thresholds are depicted in Figure 2. Specifically, the aforementioned papers determined “safe” and cell-death-inducing deformation lev-els and time exposures for skeletal muscles by applying com-pressive deformations to muscles of anesthetized rodents13 and tissue-engineered muscle constructs.14 The existence of deformation-induced damage was determined using histo-logical staining at the tissue scale13 or through fluorescent staining of the tissue-engineered constructs over time, which allowed researchers to identify and quantify damage at the cell level14 (see Figure 2). The latter study indicated cells in the constructs that experienced compressive deformations exceeding approximately 80% died almost immediately, but cells subjected to lower levels of deformation — eg, cells de-formed to the 50% level — survived longer (ie, they died after approximately 3 hours). In the animal as well as in the tissue-engineered model systems, cell survival time emerged as con-siderably sensitive to the magnitude of the sustained defor-mation level; even a mild decrease in the level of deformation added a substantial survival time for the cells (see Figure 2;
Figure 2. Development of cell/tissue injury thresholds for skeletal muscle, based on either animal models (left column) or tissue-engineered model studies (right col-umn), involves the delivery of sustained deformations at pre-set levels and for pre-determined time periods, using a rigid indentor which directly deforms the tis-sues. The onset and extent of damage, if such is de-tected, then is evaluated using histology (for the animal models) or fluorescent staining for cell death (for the tissue-engineered model system). The methodology and quantitative empirical results from these studies are described in detail for the animal model work13 and for the tissue-engineered model studies.14
DO NOT D
UPLICATE

February 2014 ostomy wound management® 41www.o-wm.com
tIssue Changes In wheeLChaIr users
bottom frame). Because hierarchical (multiscale) computer modeling has shown high deformations at the tissue (mac-roscopic) scale (as occurring in the soft tissues of the but-tocks during sitting due to weight-bearing12) are associated with high cell deformation levels,57 reduction in macroscopic deformation levels also will alleviate cell deformations. This is achievable using proper cushioning solutions.8
To illustrate the mechanism for the function of wheelchair cushions: A completely rigid support, allowing no immer-sion and hence only minimal envelopment of the buttocks by the support, will cause body weight loads to transfer from the spine to the ITs and then outward to the support surface through a smaller soft tissue region with respect to a situa-tion where the support is able to deform. The loads, concen-trated in the more limited tissue volume, subsequently will
cause high internal tissue deformations, as demonstrated in the computational (finite element [FE]) simulation in Fig-ure 3, particularly in gluteal skeletal muscle tissues overlying the ITs (see Figure 3b). The greater tissue deformation levels (see Figure 3b) dictate a shorter time for normal cell viability and an earlier onset of cell and tissue damage based on the aforementioned animal and tissue-engineered model data13,14 (see Figure 2; bottom frame). This is the reason why using a completely rigid or even a relatively stiff sitting support is potentially harmful and will lead to a pressure-related injury within a relatively short period of time, particularly for SCI patients who are insensitive and cannot respond to discom-fort or pain (see Figure 4; case a). A cushion placed under the buttocks that allows the buttocks to immerse and distort the unloaded shape of the cushion distributes tissue loading through deformation of the cushion. Through envelopment of the buttocks structure by the cushion, the area for transfer of body loads from the buttocks to the cushion, as well as for transfer of internal tissue loads, increases. This correspond-ingly decreases the levels of internal tissue deformations, because body weight forces now can spread and flow over greater tissue volumes. The outcome, in terms of tissue toler-ance to the loading, would be a longer safe sitting time (see Figure 4; case b). In fact, the greater the immersion and envel-opment, the longer the safe sitting time, where importantly, relatively mild reductions in internal sustained tissue defor-mations can increase the safe sitting time considerably due to the nonlinearity of the threshold curve, as quantitatively described by Shabshin et al8 (see Figure 4; case c versus b). However, this behavior holds only as long as no bottoming-out of the cushion occurs, because bottoming-out essentially
Figure 3. Example of computer modeling of internal tissue deformations in the seated buttocks: a) compu-tational representation of a slice through the buttocks at the ischial tuberosities (IT) region, with the overly-ing glutei, fat tissues, and skin; b) the intensity of soft tissue deformations when seated on a rigid support, where red colors indicate the greatest deformations - in gluteal tissues under the ITs. A magnified region under one IT is shown, which also demonstrates the compu-tational modeling approach that divides the complex geometry into simple structural elements (called finite elements) that can be dealt with, computationally, for calculating local deformation levels in the buttocks structure. The red regions indicate local compressive deformations in the glutei that are approximately 80%. S=skin, F=fat, GI=gluteus muscle.
Figure 4. Illustration of the effects of the level of envel-opment of the cushion on internal tissue deformations and hence on trends of safe sitting times, based on the cell/tissue injury thresholds for skeletal muscle tissues subjected to sustained compressive deformations, as reported in Linder-Ganz et al13 and Gefen et al.14
DO NOT D
UPLICATE

42 ostomy wound management® February 2014 www.o-wm.com
Feature
places the buttocks very near or perhaps on the surface on which the cushion is placed (eg, the exposed wheelchair seat) which is typically stiff, causing a loading state close to the one illustrated in Figure 3b and Figure 4: case a. To sum-marize this point, a cushion that provides better immersion and greater envelopment without any bottoming-out effects theoretically should provide safer sitting times for patients by maintaining the shape of the body and minimizing tissue deformations. Given the pathoanatomical and pathophysi-ological changes in SCI (which, from a biomechanical per-spective, make SCI patients more prone to PUs and DTIs by generally acting to increase sustained muscle deformations), these considerations are critical. Hence, the above consider-ations should be taken into account with regard to the SCI population by guiding the design, selection, and prescription of cushions for these patients.
Implications for the Future design and selection of wheelchair Cushions
Beyond striving to utilize a cushion that 1) achieves good envelopment of the buttocks without bottoming-out at the specific time point of the fitting of the cushion and 2) dem-onstrates the ability of the cushion to comply to the body and maintain the shape, one needs to appreciate the SCI patient’s unstable characteristics and consider the ongoing pathoana-tomical and pathophysiological changes. Any cushion solu-tion for this population ideally should adapt to the progres-sive changes in the patient’s body over time. A blog regarding important reimbursement changes to consider when choos-ing a wheelchair cushion (http://blog.therohogroup.com/index.php/tag/medicare/) notes regular replacement of cush-ions over short time intervals would be a valid strategy from a medical preventive point of view, but this is probably not a cost-effective approach. According to the Medicare website (www.cms.gov), US Medicare and medical insurance com-panies are acting to increase, rather than decrease, the reim-bursement time intervals between replacements of a cushion, which used to be 3 years until recently but is now changing to 5 years. If the cushion is not able to respond to the changes to the individual’s body throughout that timeframe, the PU risk inevitably increases. Although the intention here is not to ad-vocate for or oppose specific, commercially available cushion technologies, the example of using contoured foam cushions for SCI patients is presented to illustrate current problems that need to be addressed by the cushion industry based on scientific knowledge and understanding of the etiology and risk factors related to PUs and DTIs.
Manufacturing a contoured-foam cushion that fits the individual’s buttocks shape appears to be initially appealing with regard to the importance of envelopment, because that will create the greatest possible buttocks-cushion contact area. The literature58,59 to date reports IP were lower on custom-contoured shapes as opposed to flat foams, which is not sur-prising considering the contoured cushions were fitted to the (able-bodied) subjects just before the measurements. Tasker et al’s study59 included 30 able-bodied participants who sat with restricted movement for 30 minutes in three sessions in order to evaluate two contoured cushion shapes against a flat sup-port. In addition to IP recordings, the researchers evaluated discomfort levels using a visual analog scale; participants were found to be more comfortable on the contoured cushions. Nevertheless, considering that within several months to a few years, a SCI patient is expected to gain body weight and fat mass; lose gluteal muscle mass; and experience flattening of the ITs due to bone adaptation, thinning of the skin around the IT regions, and accumulation of IMF (see Figure 1), the indi-vidual’s anatomy is changing progressively and remarkably. As these changes take place and progress over time, the cushion’s contoured design becomes irrelevant to the altered anatomy, both in terms of the adapted external buttock surfaces and the internal pathoanatomy (see Figure 5).
Figure 5. A scheme depicting the problem of using a non-adapting, contour-shaped foam cushion prepared at an early stage after the spinal cord injury (SCI) for a patient whose tissues continuously respond to the dis-use conditions. a) A cushion prepared early after the SCI may fit for a short time period, providing potentially adequate envelopment; but b)as the remarkable patho-anatomical and pathophysiological changes that occur at the chronic phase of SCI take place and progress over time, the cushion’s contoured design becomes irrelevant to the altered anatomy, both in terms of the adapted external buttock surfaces (see arrows in b) and the internal pathoanatomy.
DO NOT D
UPLICATE

February 2014 ostomy wound management® 43www.o-wm.com
tIssue Changes In wheeLChaIr users
In addition to the changes that occur in the patient’s body, the cushions may present wear-related changes, as recently noted in a study by Sprigle60 in which 202 cushions used for an average of 2.7 years were inspected. This research revealed more than 60% of the foam cushions showed signs of per-manent deformation, and in nearly half, the foam exhibited granulation or brittleness. Even if not causing complete bot-toming-out, these wear-and-tear effects can increase tissue loads considerably by giving the cushion a flatter and thinner shape and particularly by compacting the foam at the regions supporting the bony prominences.
Hence, the patient and cushion both are changing over time. In the SCI population, these changes will typically act to increase the risk for PUs and DTIs by increasing sustained subcutaneous tissue deformations, particularly in skeletal muscle tissues. One of the fundamental problems of the available cushion testing methods is their tendency to focus on new cushions (which were not yet influenced by daily use and wear) and apply surrogate body shapes61 or some simple artificial indentors62 that do not consider the changes the pa-tient’s body may be undergoing. Analysis of IP data63 pub-lished more than 20 years ago notes extreme caution must be taken when using nondisabled participants as substitutes for people with SCI due to the inherent differences between the groups, illustrating how far the artificial phantoms (or inden-tors) are from the complexity of the biomechanical interac-tions of a human patient with a cushion and how they vastly oversimplify research. Hence, cushion developers, evaluators, and prescribers need new technologies for investigating, test-ing, and fitting cushions, particularly with regard to the high-risk SCI population and desirably based on the individual patient conditions at the time of the fitting and the projected changes that will occur to the individual over time.
The most promising and practical bioengineering ap-proach to overcome the aforementioned problems in eval-uating and fitting cushions is to use computer simulations based on FE modeling, which is very likely to be adopted as a design standard by the wheelchair cushion industry,64,65 much as it is currently used by car manufacturers for design-ing car seats. These computer simulations allow researchers to capture pathoanatomical and pathophysiological changes that directly reflect on the biomechanics of sitting in SCI patients and the internal tissue deformations occurring in their buttocks.19,65 Moreover, the simulations allow for the influence of microclimate factors and incontinence on tis-sue loads and tolerances.66 Recent major conferences in the field, such as the US National Pressure Ulcer Advisory Panel and the European Pressure Ulcer Advisory Panel conference in 2013, clearly indicated this to be the direction of the sup-port surface industry. However, in the more distant future, individualization of the design and fitting of cushions based on internal tissue loading conditions in a specific patient also may occur. This may take the form of subject-specific model-ing that will consider the individual anatomy of a patient at
a given time point, as well as changes that occur with time and captured by means of imaging in follow-ups or through a simulated prognosis for the individual.67
To summarize: the most ideal situation for the health of weight-bearing tissues is to avoid localized intensified ex-ternal and internal deformations relevant to activity. An ex-ample involves soft tissues during diving, where tissues are loaded by hydrostatic pressures. Such diving pressures can sometimes be extreme, but because they are uniformly dis-tributed over the body surfaces and without any external shear, no load-related discomfort or pain occurs, and cer-tainly no PUs. Of course, it is extremely difficult to reproduce this body-suspension-in-water effect by means of a cushion. However, if implementing this concept, it is clear a good cushion needs to adapt to posture and movement and to lon-ger-term pathoanatomical changes to keep tissue contours of the buttocks as close as possible to their undeformed shapes, as would occur if the body were floating in a liquid medium and maintaining tissue shapes, regardless of its position. For fluid-containing cushions, this implies a mechanism needs to exist to allow the cushion to respond to movements and lon-ger-term changes through transfer and regulation of the air or liquid pressures in-between the components of the cush-ion in response to changes in the weight-bearing configura-tion. This should eliminate build-up of localized (internal) cushion pressures acting as nearly rigid support sites and the development of corresponding concentrated tissue deforma-tions. This underscores a need for the cushion to be respon-sive rather than passive and to allow these cushion responses to be rapid enough to accommodate daily microchanges as well as the long-term macrochanges without compromising upper body mobility.
ConclusionProtecting individuals with SCI who use wheelchairs from
PUs and DTIs is complex and challenging. Microchanges (eg, changes in posture and position, use of the upper extremi-ties, performance of pushups, and changes in muscle tone) and macrochanges (mostly attributed to the disuse of tis-sues, which affects the body habitus and internal anatomy, the microarchitecture, composition and stiffness properties of tissues, and their [patho]physiology) must be considered. Most of the literature available today, which was rigorously reviewed here, consists of retrospective and prospective co-hort studies, case studies, and computer simulations, as well as a few randomized clinical trials. Together, these reports suggest important cushion design, selection, and prescrip-tion implications. Specifically, the cushion should promote a posture that is as balanced as possible but that allows ad-equate functional reach capacities that do not compromise the cushion’s capacity to minimize internal tissue deforma-tions to the greatest possible extent at any transitory or sed-entary posture. The cushion needs to be tailored to the indi-vidual based on a rigorous risk assessment conducted by an
DO NOT D
UPLICATE

44 ostomy wound management® February 2014 www.o-wm.com
Feature
expert clinician. The patient should be educated with respect to proper use of the cushion and be made aware of the life expectancy of the cushion, especially if the cushion is foam-based. Envelopment appears to be a key feature in evaluat-ing cushion performances in laboratory settings, with greater immersion and envelopment most likely providing more protection against DTIs, as long as there is no bottoming-out or near bottoming-out; this contributes directly to maintain-ing the shape of the body and minimizing tissue and cellular deformations.67 The patient’s external and internal anatomy and tissue structure and function will change considerably in the months and years following the SCI, typically along a trend that makes tissues progressively more fragile and the risk for PUs increasingly greater. A review68 of medical re-cords of 7,489 Iranian patients revealed the time that passed since the SCI had a statistically significant association with the prevalence of developing PUs (though the authors of that paper were careful to also stress SCI patients are a heteroge-neous group and the risk factors associated with PUs may vary in specific subgroups). Accordingly, a cushion that can-not adapt to the individual’s conditions throughout the day and over time will soon be less able to protect the patient from PUs and DTIs, even if that cushion was initially suitable for the individual.
The most promising and practical bioengineering ap-proach in providing and fitting cushions to different patient conditions is to use computer simulations (FE modeling), which already is being adopted by the wheelchair cushion industry. Computer simulations and individualized com-puter-based biomechanical risk assessments in particular are expected to play a key role in development and evaluation of current and future cushion products. FE computer model-ing adds critically important information on biomechanical interactions internally in the body, which can be individual-ized to represent person-specific (patho)anatomical condi-tions and the corresponding internal tissue deformations. Such understanding, which clearly cannot be achieved by IP measurements per se, may facilitate the development of bet-ter cushion products and guidelines. Although understand-ing of the pathophysiology of PU risk in individuals with SCI is increasing, studies to evaluate the efficacy, effectiveness, and cost-effectiveness of cushions are needed, particularly because it appears reimbursement policies internationally will be increasingly driven by evidence of efficacy from both laboratory and clinical studies. n
references1. EPUAP/NPUAP International Guidelines 2009. Available at: www.
epuap.org or www.npuap.org. Accessed January 22, 2014. 2. Gefen A. The biomechanics of sitting-acquired pressure ul-
cers in patients with spinal cord injury or lesions. Int Wound J. 2007;4(3):222–231.
3. Brienza D, Kelsey S, Karg P, Allegretti A, Olson M, Schmeler M, et al. A randomized clinical trial on preventing pressure ulcers with wheelchair seat cushions. J Am Geriatr Soc. 2010;58(12):2308–2314.
4. Brienza DM, Karg PE, Geyer MJ, Kelsey S, Trefler E. The relation-
ship between pressure ulcer incidence and buttock-seat cushion interface pressure in at-risk elderly wheelchair users. Arch Phys Med Rehabil. 2001;82(4):529–533.
5. Geyer MJ, Brienza DM, Karg P, Trefler E, Kelsey S. A randomized control trial to evaluate pressure-reducing seat cushions for elderly wheelchair users. Adv Skin Wound Care 2001;14(3):120–132.
6. Beeckman D, Vanderwee K. Skin protection wheelchair cushions for older nursing home residents reduce 6-month incidence of is-chial tuberosity pressure ulcers compared with segmented foam cushions. Evid Based Nurs. 2011;14(3):79–80.
7. Linder-Ganz E, Gefen A. Stress analyses coupled with damage laws to determine biomechanical risk factors for deep tissue injury dur-ing sitting. J Biomech Eng. 2009;131(1):011003.
8. Shabshin N, Zoizner G, Herman A, Ougortsin V, Gefen A. Use of weight-bearing MRI for evaluating wheelchair cushions based on internal soft-tissue deformations under ischial tuberosities. J Reha-bil Res Dev. 2010;47(1):31–42.
9. Loerakker S, Manders E, Strijkers GJ, Nicolay K, Baaijens FP, Bader DL, et al. Oomens CW. The effects of deformation, ischemia, and reperfusion on the development of muscle damage during pro-longed loading. J Appl Physiol. 2011;111(4):1168–1177.
10. Oomens CW, Zenhorst W, Broek M, Hemmes B, Poeze M, Brink PR, Bader DL, et al. A numerical study to analyse the risk for pressure ulcer development on a spine board. Clin Biomech (Bristol, Avon). 2013;28(7):736–742.
11. Shabshin N, Ougortsin V, Zoizner G, Gefen A. Evaluation of the ef-fect of trunk tilt on compressive soft tissue deformations under the ischial tuberosities using weight-bearing MRI. Clin Biomech (Bris-tol, Avon). 2010;25(5):402–408.
12. Linder-Ganz E, Shabshin N, Itzchak Y, Yizhar Z, Siev-Ner I, Gefen A. Strains and stresses in sub-dermal tissues of the buttocks are greater in paraplegics than in healthy during sitting. J Biomech. 2008;41(3):567¬580.
13. Linder-Ganz E, Engelberg S, Scheinowitz M, Gefen A. Pressure-time cell death threshold for albino rat skeletal muscles as related to pressure sore biomechanics. J Biomech. 2006;39(14):2725–2732.
14. Gefen A, van Nierop B, Bader DL, Oomens CW. Strain-time cell-death threshold for skeletal muscle in a tissue-engineered model system for deep tissue injury. J Biomech. 2008;41(9):2003–2012.
15. Metring NL, Gaspar MI, Mateus-Vasconcelos EC, Gomes MM, de Abreu DC. Influence of different types of seat cushions on the static sitting posture in individuals with spinal cord injury. Spinal Cord. 2012;50(8):627–631.
16. de Abreu DC, Takara K, Metring NL, Reis JG, Cliquet A Jr. Interfer-ence of different types of seats on postural control system during a forward-reaching task in individuals with paraplegia. Int J Rehabil Res. 2012;35(3):208–213.
17. Aissaoui R, Boucher C, Bourbonnais D, Lacoste M, Dansereau J. Effect of seat cushion on dynamic stability in sitting during a reach-ing task in wheelchair users with paraplegia. Arch Phys Med Reha-bil. 2001;82(2):274–281.
18. Sprigle S, Wootten M, Sawacha Z, Thielman G. Relationships among cushion type, backrest height, seated posture, and reach of wheelchair users with spinal cord injury. J Spinal Cord Med. 2003;26(3):236–243.
19. Levy A, Kopplin K, Gefen A. Simulations of skin and subcutane-ous tissue loading in the buttocks while regaining weight-bearing after a push-up in wheelchair users. J Mech Behav Biomed Mater. 2013;28:436–447.
20. Adams MM, Hicks AL. Spasticity after spinal cord injury. Spinal Cord. 2005;43(10):577–586.
21. Sopher R, Nixon J, Gorecki C, Gefen A. Effects of intramuscular fat infiltration, scarring, and spasticity on the risk for sitting-acquired deep tissue injury in spinal cord injury patients. J Biomech Eng. 2011;133(2):021011.
22. Lamid S, El Ghatit AZ. Smoking, spasticity and pressure sores in spinal cord injured patients. Am J Phys Med. 1983;62(6):300–306.
23. Gorgey AS, Dudley GA. Spasticity may defend skeletal muscle size and composition after incomplete spinal cord injury. Spinal Cord. 2008;46(2):96–102.
DO NOT D
UPLICATE

February 2014 ostomy wound management® 45www.o-wm.com
tIssue Changes In wheeLChaIr users
24. Gracies JM. Pathophysiology of spastic paresis. II: Emergence of muscle overactivity. Muscle Nerve. 2005;31(5):552–571.
25. Crane DA, Little JW, Burns SP. Weight gain following spinal cord injury: a pilot study. J Spinal Cord Med. 2011;34(2):227–232.
26. Cox SA, Weiss SM, Posuniak EA, Worthington P, Prioleau M, Hef-fley G. Energy expenditure after spinal cord injury: an evaluation of stable rehabilitating patients. J Trauma 1985;25(5):419–423.
27. Chen Y, Henson S, Jackson AB, Richards JS. Obesity intervention in persons with spinal cord injury. Spinal Cord. 2006;44(2):82–91.
28. Elsner JJ, Gefen A. Is obesity a risk factor for deep tissue injury in patients with spinal cord injury? J Biomech. 2008;41(16):3322–3331.
29. Sopher R, Nixon J, Gorecki C, Gefen A. Exposure to internal mus-cle tissue loads under the ischial tuberosities during sitting is el-evated at abnormally high or low body mass indices. J Biomech. 2010;43(2):280–286.
30. Dudley-Javoroski S, Shields RK. Muscle and bone plasticity after spinal cord injury: review of adaptations to disuse and to electrical muscle stimulation. J Rehabil Res Dev. 2008;45(2):283–296.
31. Garland DE, Adkins RH, Stewart CA. Five-year longitudinal bone evaluations in individuals with chronic complete spinal cord injury. J Spinal Cord Med. 2008;31(5):543–550.
32. Be’ery-Lipperman M, Gefen A. Contribution of muscular weakness to osteoporosis: Computational and animal models. Clin Biomech (Bristol, Avon). 2005;20:984–997.
33. Rittweger J, Gerrits K, Altenburg T, Reeves N, Maganaris CN, de Haan A. Bone adaptation to altered loading after spinal cord injury: a study of bone and muscle strength. J Musculoskelet Neuronal Interact. 2006;6(3):269–276.
34. Giangregorio LM, Craven BC, Webber CE. Musculoskeletal chang-es in women with spinal cord injury: a twin study. J Clin Densitom. 2005;8(3):347–351.
35. de Bruin ED, Dietz V, Dambacher MA, Stüssi E. Longitudinal changes in bone in men with spinal cord injury. Clin Rehabil. 2000;14(2):145–152.
36. Maggioni M, Bertoli S, Margonato V, Merati G, Veicsteinas A, Testo-lin G. Body composition assessment in spinal cord injury subjects. Acta Diabetol. 2003;40(suppl 1):S183–S186.
37. Carda S, Cisari C, Invernizzi M. Sarcopenia or muscle modifications in neurologic diseases: a lexical or pathophysiological difference? Eur J Phys Rehabil Med. 2013;49(1):119–130.
38. Gorgey AS, Dudley GA. Skeletal muscle atrophy and increased intramuscular fat after incomplete spinal cord injury. Spinal Cord. 2007;45(4):304–309.
39. Shah PK, Stevens JE, Gregory CM, Pathare NC, Jayaraman A, Bickel SC, et al. Lower-extremity muscle cross-sectional area after incomplete spinal cord injury. Arch Phys Med Rehabil. 2006;87(6):772–778.
40. Castro MJ, Apple DF Jr, Hillegass EA, Dudley GA. Influence of complete spinal cord injury on skeletal muscle cross-sectional area within the first 6 months of injury. Eur J Appl Physiol Occup Physiol. 1999;80(4):373–378.
41. Wu GA, Bogie KM. Not just quantity: Gluteus maximus muscle characteristics in able-bodied and SCI individuals — implications for tissue viability. J Tissue Viability. 2013;22(3):74–82.
42. Roubenoff R. The pathophysiology of wasting in the elderly. J Nutr. 1999;129(1 suppl):256S–259S.
43. Kovanlikaya A, Mittelman SD, Ward A, Geffner ME, Dorey F, Gilsanz V. Obesity and fat quantification in lean tissues using three-point Dixon MR imaging. Pediatr Radiol. 2005;35(6):601–607.
44. Shaw CS, Clark J, Wagenmakers AJ. The effect of exercise and nu-trition on intramuscular fat metabolism and insulin sensitivity. Annu Rev Nutr. 2010;30(Aug):13–34.
45. Kern H, Boncompagni S, Rossini K, Mayr W, Fanò G, Zanin ME, et al. Long-term denervation in humans causes degeneration of both contractile and excitation-contraction coupling apparatus, which is reversible by functional electrical stimulation (FES): a role for myo-fiber regeneration? J Neuropathol Exp Neurol. 2004;63(9):919–931.
46. Palevski A, Glaich I, Portnoy S, Linder-Ganz E, Gefen A. Stress re-laxation of porcine gluteus muscle subjected to sudden transverse deformation as related to pressure sore modeling. J Biomech Eng.
2006;128(5)[AU: Number?]:782–787.47. Gefen A, Haberman E. Viscoelastic properties of ovine adipose tis-
sue covering the gluteus muscles. J Biomech Eng. 2007;129(6):924–930.
48. Loerakker S, Solis LR, Bader DL, Baaijens FP, Mushahwar VK, Oo-mens CW. How does muscle stiffness affect the internal deforma-tions within the soft tissue layers of the buttocks under constant loading? Comput Methods Biomech Biomed Engin. 2013;16(5):520–529.
49. Yalcin E, Akyuz M, Onder B, Unalan H, Degirmenci I. Skin thickness on bony prominences measured by ultrasonography in patients with spinal cord injury. J Spinal Cord Med. 2013;36(3):225–230.
50. Park JW, Seo CH, Han SH, Lee YG. Sympathetic influence on bio-mechanical skin properties after spinal cord injury. Spinal Cord. 2011;49(2):236–243.
51. Rodriguez GP, Garber SL. Prospective study of pressure ulcer risk in spinal cord injury patients. Paraplegia. 1994;32(3):150–158.
52. Zhu C, Galea M, Livote E, Signor D, Wecht JM. A retrospective chart review of heart rate and blood pressure abnormalities in veterans with spinal cord injury. J Spinal Cord Med. 2013;36(5):463–475.
53. West CR, Mills P, Krassioukov AV. Influence of the neurological level of spinal cord injury on cardiovascular outcomes in humans: a me-ta-analysis. Spinal Cord. 2012;50(7):484–492.
54. Scelsi R. Skeletal muscle pathology after spinal cord injury, our 20 year experience, and results on skeletal muscle changes in paraplegics, related to functional rehabilitation. Basic Appl Myol. 2001;11(2):75–85.
55. Ruschkewitz Y, Gefen A. Cellular-scale transport in deformed skel-etal muscle following spinal cord injury. Comput Methods Biomech Biomed Engin. 2011;14(5):411–424.
56. Thorfinn J, Sjöberg F, Sjöstrand L, Lidman D. Perfusion of the skin of the buttocks in paraplegic and tetraplegic patients, and in healthy subjects after a short and long load. Scand J Plast Reconstr Surg Hand Surg. 2006;40(3):153–160.
57. Shoham N, Gefen A. Deformations, mechanical strains and stress-es across the different hierarchical scales in weight-bearing soft tissues. J Tissue Viability. 2012;21(2):39–46.
58. da Silva FP, Beretta EM, Prestes RC, Kindlein Junior W. Design and milling manufacture of polyurethane custom contoured cushions for wheelchair users. Australas Med J. 2011;4(9):500–506.
59. Tasker LH, Shapcott NG, Watkins AJ, Holland PM. The effect of seat shape on the risk of pressure ulcers using discomfort and in-terface pressure measurements. Prosthet Orthot Int. 2014;38(1):46-53.
60. Sprigle S. Visual inspections of wheelchair cushions after everyday use. Assist Technol. 2013;25(3):176–180.
61. Akins JS, Karg PE, Brienza DM. Interface shear and pressure characteristics of wheelchair seat cushions. J Rehabil Res Dev. 2011;48(3):225–234.
62. Sprigle S, Chung B, Meyer T. Assessment of the ISO impact damp-ing test for wheelchair cushions. Assist Technol. 2010;22(4):236–244.
63. Hobson DA. Comparative effects of posture on pressure and shear at the body-seat interface. J Rehabil Res Dev. 1992;29(4):21–31.
64. Bader DL. Editorial. J Tissue Viabil. 2013;22(2):2–24.65. Gefen A. State-of-the-art bioengineering technologies for evaluat-
ing support surfaces. Proceedings of the 16th European Pressure Ulcer Advisory Panel (EPUAP) Annual Conference, Vienna, Austria. August 28-30 2013.
66. Shaked E, Gefen A. Modeling the effects of moisture-related skin-support friction on the risk for superficial pressure ulcers during pa-tient repositioning in bed. Front Bioeng Biotechnol. 2013;1(9):1–7.
67. Levy A, Kopplin K, Gefen A. An air-cell-based cushion for pres-sure ulcer protection remarkably reduces tissue stresses in the seated buttocks with respect to foams: Finite element studies. J Tissue Viability. 2013; in press (available online). doi: 10.1016/j.jtv.2013.12.005.
68. Eslami V, Saadat S, Habibi Arejan R, Vaccaro AR, Ghodsi SM, Rahi-mi-Movaghar V. Factors associated with the development of pres-sure ulcers after spinal cord injury. Spinal Cord. 2012;50(12):899–903.
DO NOT D
UPLICATE