The white coat effect is not associated with additional increase of target organ damage in true...
Transcript of The white coat effect is not associated with additional increase of target organ damage in true...
Med Clin (Barc). 2013;140(1):1–5
Original article
The white coat effect is not associated with additional increase of target organdamage in true resistant hypertension
Valeria Nasser Figueiredo a, Luiz Claudio Martins a, Leandro Boer-Martins a,b, Ana Paula Cabral de Faria a,Carolina de Haro Moraes a, Rodrigo Cardoso Santos a, Armando R. Nogueira c, Heitor Moreno Jr.a,*a Cardiovascular Pharmacology Laboratory, Faculty of Medical Sciences, University of Campinas (Unicamp), Campinas, SP, Brazilb Cardiovascular & Metabolism Unit, Pharma Sector, Novartis Biociencias S.A., Sao Paulo, Brazilc Hypertension Program, University Hospital Clementino Fraga Filho, Medical School, Federal University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil
A R T I C L E I N F O
Article history:
Received 25 January 2012
Accepted 19 April 2012
Available online 17 September 2012
Keywords:
Resistant hypertension
White coat effect
Left ventricular hypertrophy
Renal dysfunction
A B S T R A C T
Background and objective: White coat effect (WCE) (i.e., the difference between office blood pressure
[OBP] and awake ambulatory blood pressure monitoring [ABPM]) may be present in hypertensive
individuals. The relationship between occurrence of WCE and target organ damage (TOD) has not yet
been assessed in true resistant hypertension (RHTN).
Patients and methods: RHTN patients were divided into two groups: RHTN with WCE (WCE, n = 66) and
RHTN without WCE (non-WCE, n = 61). All patients were submitted to OBP measurement, ABPM,
echocardiography and renal function evaluation in three visits.
Results: No differences were observed between the WCE and non-WCE groups regarding age, body mass
index or gender. OBP were 169.8 � 15.8/95.1 � 14.0 (WCE) and 161.9 � 9.0/90.1 � 10.4 mmHg (non-WCE),
ABPM = 143.0 � 12.8/86.1 � 9.9 (WCE) and 146.1 � 13.6/85.1 � 14.9 mmHg (non-WCE). No statistical
differences were observed between WCE and non-WCE subgroups with respect to left ventricular mass
index (LVMI) (WCE = 131 � 4.7; non-WCE = 125 � 2.9 g/m2), creatinine clearance (WCE = 78 � 4.7; non-
WCE = 80 � 3.6 ml/min/m2) and microalbuminuria (MA) (WCE = 44 � 8.4; non-WCE = 49 � 6.8 mg/g Cr).
Conclusions: This finding may suggest that WCE is not associated with additional increase of TOD in true
RHTN subjects.
� 2012 Elsevier Espana, S.L. All rights reserved.
El efecto de bata blanca sobre la presion arterial en pacientes con hipertensionresistente verdadera no se asocia con incremento adicional de lesiones enorganos diana
Palabras clave:
Hipertension arterial resistente
Efecto de bata blanca
Hipertrofia ventricular izquierda
Enfermedad renal
R E S U M E N
Fundamento y objetivo: El efecto de bata blanca (EBB), es considerado cuando la diferencia entre la PAS/
PAD medida en consulta medica y aquella obtenida por monitorizacion ambulatoria de la presion arterial
(MAPA) y puede estar presente durante la consulta medica en pacientes con hipertension arterial
resistente (HTA-R). La relacion entre la presencia del efecto bata blanca y danos en organos diana aun no
ha sido evaluada en individuos con HTA-R verdadera.
Pacientes y metodo: En este estudio, sesenta y seis pacientes con HTA-R verdadera presentaron EBB y
otros 61 no lo hicieron. A todos los sujetos se les practico una monitorizacion ambulatoria de la presion
arterial durante 24 horas (MAPA). La afectacion de organos diana se determino mediante la realizacion
de ecocardiograma y evaluacion de la funcion renal.
Resultados: Los valores de PAS y PAD en consulta medica fueron: 169,8 � 15,8/95,1 � 14,0 (pacientes con
EBB) y 161,9 � 9,0/90,1 � 10,4 mmHg (pacientes sin EBB), respectivamente y mediante MAPA los valores
promedios de PAS y PAD de 24 horas fueron: 143,0 � 12,8/86,1 � 9,9 (pacientes con EBB) y 146,1 � 13,6/
85,1 � 14,9 mmHg (pacientes sin EBB), respectivamente. No se observaron diferencias significativas entre los
pacientes con o sin EBB con respecto al ındice de masa ventricular izquierda (con EBB = 131 � 4,7; sin
ww w.els evier .es /med i c in ac l in i c a
* Corresponding author.
E-mail address: [email protected] (H. Moreno Jr.).
0025-7753/$ – see front matter � 2012 Elsevier Espana, S.L. All rights reserved.
http://dx.doi.org/10.1016/j.medcli.2012.04.031
V.N. Figueiredo et al / Med Clin (Barc). 2013;140(1):1–52
EBB = 125 � 2,9 g/m2), aclaramiento de creatinina (con EBB = 78 � 4,7; sin EBB = 80 � 3,6 ml/min/m2) y
microalbuminuria (con EBB = 44 � 8,4; sin EBB = 49 � 6,8 mg/g Cr).
Conclusiones: Este hallazgo sugiere que el EBB no se asocia a incremento adicional de danos en organos
diana en pacientes con HTA-R verdadera.
� 2012 Elsevier Espana, S.L. Todos los derechos reservados.
Introduction
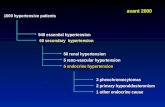
Resistant hypertension (RHTN) is defined as being presentwhen a therapeutic plan, including attention to lifestyle modifica-tion and the prescription of at least three antihypertensive agentsof different classes in adequate doses, fails to lower systolic bloodpressure (SBP) and diastolic blood pressure (DBP) sufficiently.1 Inaddition, patients whose blood pressure (BP) is controlled but whorequire four or more medications to reach the goal (of which isBP < 140/90 mmHg) should be considered resistant to treatment.1
ABPM is one of the valid methods to differentiate ‘‘isolated officeRHTN’’ (or pseudo-RHTN) from ‘‘true RHTN’’, providing higherprognostic value than OBP measurements in the evaluation ofsubjects with RHTN.2
The BP measurement at the physician’s office can lead to a highOBP when compared with other out-of-clinic measurements, suchas ABPM in hypertensive patients. This is known as the ‘WCE’3;some theories have been put forward suggesting that it issignificantly related to mental stress,4 emotional hyperrespon-siveness or hyperreactive response on the part of the patient whilebeing examined by the physician.5 Thus, WCE may be related to analerting reaction mediated by the sympathetic nervous systemthat is associated with greater variability in BP.4 Moreover,sustained hypertension is associated with sympathetic predomi-nance or decrease in parasympathetic activity, which has aninfluence on heart rate as well as BP.6 Some authors have foundthat WCE does not entail increased cardiovascular risk7 tohypertensive subjects, while it is associated with decreased hazardratios for all-cause mortality.8
The prognostic significance of WCE in RHTN patients isunclear.9 It is known that pseudo RHTN patients with manifestingWCE have less severe TOD when compared to those with trueRHTN during ambulatory monitoring,2 meaning that the latterhave a poorer prognosis than the former. However, no study hasevaluated the influence of WCE on TOD in true RHTN. The aim ofthe present study was to assess whether WCE is associated withTOD in true RHTN.
Patients and methods
Patient population
We evaluated patients referred to the Resistant HypertensionService of the University of Campinas for difficult-to-controlhypertension. All individuals completed a medical history ques-tionnaire and were submitted to physical examinations, electro-cardiography and laboratory tests. Patients with secondary formsof hypertension, liver disease, coronary heart disease, strokes,peripheral vascular disease or any other major diseases, as well assmoking patients, were excluded. Patients were evaluated con-cerning adherence to treatment and underwent clinical optimiza-tion of antihypertensive therapy.10 Daytime ABPM (Spacelabs90207, Spacelabs Inc., Redmon, WA, USA) is an auxiliary method tocharacterize RHTN and in our study it was used to exclude causesof pseudoresistance, including white coat hypertension (WCH).After a 6-month period (five to six visits), 127 patients wereidentified with true RHTN and included in the study. They weredivided into two groups: RHTN with WCE (WCE, n = 66) and RHTN
without WCE (non-WCE, n = 61). The mean duration of hyperten-sion was 8.3 years in both groups. This study was approved by theResearch Ethics Committee of the University of Campinas, SaoPaulo, Brazil and written informed consent was obtained from eachpatient before study participation.
Study design
Nonpharmacologic therapies were optimized, including dietarysalt control, which were confirmed by the measurement of urinarysodium excretion (<100 mEq/24 h). All patients were submitted toOBP measurement, ABPM, echocardiography and renal functionevaluation in three visits. WCE was defined as measurement ofSBP > 20 mmHg and/or DBP > 10 mmHg, in the physician’s office,in comparison with daytime ABPM.3
Measurements
Office blood pressure
With the patients in a seated position with the arm comfortablyplaced at heart level, BP level after resting for 5 min and OBP levelwere obtained according to American Heart Association.10 OBP wasmeasured three times from each patient using a digital BP monitor(HEM-907 XL Omron). We used the mean value of the two lastmeasurements as the final OBP level.
Ambulatory blood pressure monitoring
All participants underwent 24-h ABPM on a usual working day.They were instructed to act and work normally. The Spacelabs90207 ambulatory blood pressure monitor (Spacelabs Inc., Red-mon, WA) was used.11 The appropriate size cuff was placed aroundthe nondominant arm. Readings were obtained automatically at20-min intervals throughout the 24-h monitoring period. Allparticipants of the study had at least 80% of the total measure-ments validated. Ambulatory blood pressure parameters includedmean daytime SBP and DBP. All participants were instructed todescribe their sleep period in a personal diary. The daytime andnighttime periods were defined individually for each record inaccordance with bedtime reported by the patient. Also, WCH wasextensively excluded as cause of pseudoresistance by ABPM,allowing that only true RHTN patients were included in this study.
Echocardiography
Measurements of left ventricle (LV) dimensions were per-formed according to the American Society of Echocardiography(ASE) recommendations, using a two-dimensional targetedM-mode echocardiography. LV mass was calculated by therecommended ASE formula.12 LV mass index (LVMI) wascalculated dividing the LV mass by the body surface. Left ventriclehypertrophy (LVH) was defined as LV mass index > 115 g/m2 formen and >95 g/m2 for women. Echocardiography measurementswere evaluated by two blinded investigators.
Laboratory assessment
Baseline blood samples for measurement of glycemia (mg/dl),total cholesterol (mg/dl), LDL cholesterol (mg/dl), triglycerides(mg/dl) and creatinine (mg/dl) were collected at 8 a.m. afterovernight fasting, during which time individuals rested in thesupine position for 8 h, followed by 1 h in an upright position in an
Table 2Anti-hypertensive (anti-HTN) drugs distribution.
Characteristic/variable WCE
(n = 66)
Non-WCE
(n = 61)
p-Value
Total anti-HTN drugs 5.2 � 0.3 4.1 � 0.2 0.02
Thiazide diuretic 96.1% (63) 92.3% (56) 0.24
Aldosterone receptor inhibitor 7.3% (5) 5.1% (3) 0.46
b-Blockers 60.0% (39) 72.7% (44) 0.41
Angiotensin-converting enzyme inhibitors 70.0% (47) 45.4% (27) 0.01
Angiotensin receptor blocker 64.7% (43) 42.4% (26) 0.03
Calcium channel blocker 83.3% (55) 63.6% (39) 0.04
Centrally acting anti-hypertensive drug 16.6% (11) 13.6% (8) 0.34
Abbreviations: WCE: white coat effect patients. Values are means � SD.
V.N. Figueiredo et al / Med Clin (Barc). 2013;140(1):1–5 3
air-conditioned room (22–24 8C). Urinary sodium (mEq/24 h),creatinine clearance (ml/min/1.73 m2) and MA (mg/g Cr) rate wereevaluated in 24-h sterile urine. The glomerular filtration ratewas also calculated through the Cockroft-Gault formula (140 �age � weight/creatinine � 72 for men and for women, multipliedby the correction factor of 0.85). The U-Alb level was measured asthe albumin to creatinine excretion ratio (mg/g Cr) in the urine. MAwas defined as U-Alb level between 30 and 300 mg/g Cr.
Statistical analysis
The Statistical Analysis System, version 8.02 (SAS Institute Inc.,Cary, NC, USA), was used for all statistical analyses. The statisticalanalysis was performed descriptively and interpreted in anexplorative way. Unpaired groups were compared using Mann–Whitney U test. Fisher exact test was used to determine whethercertain group had significantly different proportion of a particularcharacteristic. A value of p < 0.05 indicated significance. Samplesize was calculated to fit statistical power of 0.80 and two-tailedsignificance level of 0.05 for all studied variables. All values areexpressed as mean � SD (standard deviation).
Results
The general characteristics of the two RHTN subgroups arelisted in Table 1. No differences were observed between the WCEand non-WCE groups regarding age, body mass index or gender.
As shown in Table 1, although a trend for higher office SBP(169.8 � 15.8 mmHg) and DBP (95.1 � 14.0 mmHg) values wasobserved in WCE group, the difference was not significant. However,the BP delta values (i.e., difference between physician’s office anddaytime ABPM) registered were 28 � 4 vs. 16 � 3 mmHg for SBPand 16 � 5 vs. 7 � 2 mmHg for DBP in WCE and non-WCE groups,respectively (p < 0.05).
WCE patients received more anti-hypertensive drugs than non-WCE (5.2 � 0.3 vs. 4.1 � 0.2, respectively) (Table 2).
Table 1Baseline characteristics of true RH patients.
WCE (n = 66) Non-WCE (n = 61) p-Value
Clinical data
Female gender (%) 64.1 69.2 0.38
Age (years) 55.0 � 9.1 57.9 � 10.5 0.46
BMI (kg/m2) 30.5 � 3.4 30.8 � 2.8 0.45
Blood pressure
Office SBP (mmHg) 169.8 � 15.8 161.9 � 9.0 0.22
Office DBP (mmHg) 95.1 � 14.0 90.1 � 10.4 0.83
Daytime SBP (mmHg) 143.0 � 12.8 146.1 � 13.6 0.79
Daytime DBP (mmHg) 86.1 � 9.9 85.1 � 14.9 0.61
DSBP (mmHg) 28 � 4 16 � 3 0.003
DDBP (mmHg) 16 � 5 7 � 2 0.006
Laboratory parameters
Glycemia (mg dl�1) 100 � 8.3 99 � 7.2 0.65
Cholesterol (mg dl�1) 189 � 14.1 185 � 16.7 0.45
HDL-c (mg dl�1) 50.1 � 14.2 49.9 � 16.1 0.69
LDL-c (mg dl�1) 107.4 � 18.9 110.3 � 20.5 0.55
Triglycerides (mg dl�1) 119.9 � 76.6 121.9 � 86.2 0.58
Creatinine (mg dl�1) 1.1 � 0.2 1.0 � 0.3 0.78
Uric acid (mg dl�1) 5.8 � 1.0 6.0 � 0.7 0.66
Sodium (mEq l�1) 140.9 � 1.6 140.7 � 2.6 0.79
Potassium (mEq l�1) 4.0 � 0.2 4.1 � 0.3 0.89
Abbreviations: n: number of patients; WCE: white coat effect; BMI: body mass
index; SBP: systolic blood pressure; DBP: diastolic blood pressure; LDL and HDL:
low- and high-density lipoproteins, respectively; eGFR: estimated glomerular
filtration rate; DSBP: difference between office systolic blood pressure and systolic
daytime ABPM; DDBP: difference between office diastolic blood pressure and
diastolic daytime ABPM. Values are means � SD.
LVH was present in 75% of RHTN, with no significant differencesbetween WCE and non-WCE groups. LVMI was similar in bothgroups (131.7 � 4.7 and 125.9 � 2.9 g/m2 in WCE and non-WCEpatients, respectively [p = 0.19]).
Renal function measured by creatinine clearance was similar inboth groups (78.5 � 4.7 and 80.6 � 3.6 ml min 1.73 m�2 in WCE andnon-WCE patients, respectively [p = 0.52]). MA was found in 45% ofWCE and 50% non-WCE groups (p = 0.37) [44.6 � 8.4 and49.8 � 6.8 mg/g Cr in WCE and non-WCE patients, respectively(p = 0.74)].
Discussion
In the present study, we compared LVH and renal dysfunction intwo true RHTN subgroups: those with and without WCE. The mainfinding of this study is that TOD, evaluated by LVH, creatinineclearance and MA, were similar.
First of all, WCH should not be confounded with WCE. The WCHoccurs when BP levels exceed 140/90 mmHg during office readingsdespite of normal levels when assessed through ABPM and/orhome blood pressure monitoring. Differently, the WCE is strictlycharacterized by an increase in BP with the presence of the healthcare professional and a higher OBP independently of the diagnosisof hypertension and normotension.13
In the present study, we found a higher prevalence of WCE inRHTN individuals (52%) in comparison with other authors (20–30%).14 This difference may be due to the stricter inclusion criteriafor RHTN used in our study. Most studies define RHTN asOBP > 140/90 mmHg and 24-h BP < 135/85 mmHg.10,14 Our studygroup only comprised RHTN patients who had both increaseddaytime ABPM and OBP levels. This observation is importantbecause the proportion of patients with clinical target-organdamage is greater in subjects with true RHTN than in those withwhite coat resistant hypertension (WCRH) (pseudo-RHTN).15
Several measures of TOD, including left ventricular mass andMA, have been compared among normotensives, white coathypertensives, and sustained hypertensives. The prevalence ofTOD is very high in resistant hypertensive subjects.16 In general,TOD in WCH is less than that in sustained hypertension, but theWCE is not associated with increased target organ involvement.17
Conversely, Hernandez-delRey and colleagues have shown ahigher proportion of patients with clinical TOD with true RHTNthan those with pseudo-RHTN (WCRH).15 This difference may beexplained by the fact that we included only RHTN patientscharacterized by increased BP levels in both ABPM and OBP. Thus,in these truly RHTN subjects, the presence of WCE was notassociated with a higher degree of LVH or renal damage.
We found that LVH was present in 75% of RHTN, with nosignificant differences between WCE and non-WCE groups. It iswell known that the extent of BP rise seems to be independentlyassociated with LVH and left ventricular mass in hypertensivepatients18 and long-term antihypertensive treatment may inducereductions in LVMI and in the clinic-daytime differences for SBP
V.N. Figueiredo et al / Med Clin (Barc). 2013;140(1):1–54
and DBP; however, no significant relationship between these twoparameters was found when tested by multiple regressionanalysis.19 This study provided the first longitudinal evidencethat clinic-daytime differences in BP have no substantial value inpredicting the regression of TOD, such as LVH, which hasprognostic relevance in RHTN.20 In addition, CV risk is moretightly correlated with out-of-office BP than clinic BP21 and amongpatients with RHTN. Twenty-four-hour ABPM is an independentpredictor of CV morbidity and mortality, whereas OBP has beenfound to have no prognostic value.20 Therefore, based on our ownand other authors’ findings, the occurrence of WCE is notresponsible for higher LVH in RHTN. However, more researchneeds to be undertaken.
One interesting observation is that all the patients who took partin this study were overweight. Recently, we have demonstrated thatbody mass index is higher in uncontrolled RHTN subjects than incontrolled ones, and also it is associated with greater LVH.22
Hypertensive patients with white coat phenomenon have greatersympathetic activation compared with normotensive subjects andhypertensive patients.6 The development of a particularly resistantform of hypertension in metabolic individuals can be partiallyattributed to vasoconstriction from increased sympathetic activa-tion. In general, the sympathetic predominance in hypertension isassociated with deleterious effects on target organs, predicting thedevelopment of cardiovascular complications.23 Our results rein-force the relevance of obesity and a possible enhanced sympatheticactivation in the determination of the increased cardiac mass indexin both RHTN subgroups, but they do not seem to be related to theoccurrence of white coat phenomena, which were not foundassociated with a higher degree of LVH.
MA is an important marker of TOD in patients with essentialhypertension and is associated with higher rates of pressure.24
Furthermore, other authors showed that BP control appears to befundamental for reducing MA.25 In our study, urine albuminexcretion (UAE) was similar in both RHTN groups, suggesting thatthe occurrence of WCE did not aggravate MA in RHTN, as describedby other authors for general hypertension.17
MA correlates with OBP in RHTN,26 and it has a significantlyhigher prevalence in patients with true RHTN when compared withpatients with pseudo-RHTN.27 Furthermore, these authors haveshown MA and office SBP as the only two variables thatindependently predict the occurrence of true RHTN vs. WCE inpseudo-resistant hypertensive patients. RHTN is a common clinicalproblem in older (>75 years) and obese patients which isassociated with an increasing incidence of diabetes and chronickidney disease, and the prevalence of RHTN can be expected toincrease.28 We found that both RHTN groups had a normalglomerular filtration rate (which is usually defined as >60 ml/minper 1.73 m2), and low MA probably because these patients werenot as old and obese as those included in other studies.29
In order to achieve an effective prevention of cardiovasculardisease, RHTN patients require specific therapeutic interventionsbeyond reducing BP levels, such as the control of associatedcomorbidities and other metabolic dysfunctions.30 The WCE grouphad a higher prescription prevalence of angiotensin-convertingenzyme inhibitors, angiotensin receptor blocker and calciumchannel blocker than the non-WCE group. This difference mightexplain the greater protection against TOD in WCE patients. Also,long-term antihypertensive treatment may cause reductions inLVMI and WCE, but no significant relationship between theseparameters was found when tested by multiple regressionanalysis.19 We also did not find this association for RHTN subjectsas well as between reduced creatinine clearance or MA andoccurrence of WCE.
Some limitations are important to note. First, this is a cross-sectional study and the potential implications of long-term
crossovers between WCE and non-WCE groups do not allow usto extrapolate our results to prognostic outcomes. Second, sincediabetes, smoking, dyslipidemia and all pseudo RHTN patientswere excluded in order to minimize, as much as possible, anyfactors that could skew the results, a small number of RHTNpatients were enrolled in the study. Finally, the possibility ofhaving significant difference between the measured MA of bothgroups (type II statistical error) cannot be completely discardedsince we had a statistical power below the desired value (0.73) forthis particular variable analysis.
Although there is no doubt that both office and ambulatory BPstill have an important role in the diagnosis and follow-up of RHTNpatients and can be used to classify the lack of control in patientsinitially misdiagnosed with RHTN hypertension, we demonstratedthat WCE is not associated with additional increase of TOD in trueRHTN subjects. This finding suggests that future longitudinalstudies need to be carried out to prove whether there is anincremental deleterious effect of WCE in TOD and whichpathogenesis is involved in this effect in patients with true RHTN.
Competing interests
Leandro Boer-Martins is an employee of Novartis BiocienciasS.A. (Brazil).
Acknowledgements
This study was supported by the State of Sao Paulo ResearchFoundation (Fapesp), National Council for Scientific and Techno-logical Development (CNPq) and Coordination for Higher LevelGraduates Improvement (Capes), Brazil.
References
1. Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, et al. Resistanthypertension: diagnosis, evaluation, and treatment. A scientific statement fromthe American Heart Association Professional Education Committee of theCouncil for High Blood Pressure Research. Hypertension. 2008;51:1403–19.
2. Muxfeldt ES, Bloch KV, Nogueira AR, Salles GF. Twenty-four hour ambulatoryblood pressure monitoring pattern of resistant hypertension. Blood Press Monit.2003;8:181–5.
3. Pickering TG, Gerin W, Schwartz AR. What is the white-coat effect and howshould it be measured? Blood Press Monit. 2002;7:293–300.
4. Lantelme P, Milon H, Gharib C, Gayet C, Fortrat JO. White coat effect andreactivity to stress: cardiovascular and autonomic nervous system responses.Hypertension. 1998;31:1021–9.
5. Gualdiero P, Niebauer J, Addison C, Clark SJ, Coats AJ. Clinical features, anthro-pometric characteristics, and racial influences on the ‘white-coat effect’ in asingle-centre cohort of 1553 consecutive subjects undergoing routine ambu-latory blood pressure monitoring. Blood Press Monit. 2000;5:53–7.
6. Buchholz K, Schachinger H, Wagner M, Sharma AM, Deter HC. Reduced vagalactivity in salt-sensitive subjects during mental challenge. Am J Hypertens.2003;16:531–6.
7. Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat,masked and sustained hypertension versus true normotension: a meta-analy-sis. J Hypertens. 2007;25:2193–8.
8. Ben-Dov IZ, Kark JD, Mekler J, Shaked E, Bursztyn M. The white coat phenom-enon is benign in referred treated patients: a 14-year ambulatory bloodpressure mortality study. J Hypertens. 2008;26:699–705.
9. Tsai PS. Determinants of the white-coat effect in normotensives and never-treated mild hypertensives. Clin Exp Hypertens. 2003;25:443–54.
10. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. TheSeventh Report of the Joint National Committee on Prevention, DetectionEvaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA.2003;289:2560–72.
11. Groppelli A, Omboni S, Parati G, Mancia G. Evaluation of noninvasive bloodpressure monitoring devices Spacelabs 90202 and 90207 versus resting andambulatory 24-hour intra-arterial blood pressure. Hypertension. 1992;20:227–32.
12. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al.Recommendations for chamber quantification: a report from the AmericanSociety of Echocardiography’s Guidelines and Standards Committee and theChamber Quantification Writing Group, developed in conjunction withthe European Association of Echocardiography, a branch of the EuropeanSociety of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–63.
V.N. Figueiredo et al / Med Clin (Barc). 2013;140(1):1–5 5
13. Myers MG, Reeves RA. White coat effect in treated hypertensive patients:sex differences. J Hum Hypertens. 1995;9:729–33.
14. Brown MA, Buddle ML, Martin A. Is resistant hypertension really resistant? Am JHypertens. 2001;14:1263–9.
15. Hernandez-delRey R, Armario P, Martin-Baranera M, Sanchez P, Cardenas G,Pardell H. Target-organ damage and cardiovascular risk profile in resistanthypertension. Influence of the white-coat effect. Blood Press Monit. 1998;3:331–7.
16. Armario P, Oliveras A, Hernandez Del Rey R, Ruilope LM, De La Sierra A.Prevalence of target organ damage and metabolic abnormalities in resistanthypertension. Med Clin (Barc). 2011;137:435–9.
17. Kristensen KS, Hoegholm A, Bang LE, Gustavsen PH, Poulsen CB. No impact ofblood pressure variability on microalbuminuria and left ventricular geometry:analysis of daytime variation, diurnal variation and ‘white coat’ effect. BloodPress Monit. 2001;6:125–31.
18. Muscholl MW, Hense HW, Brockel U, Doring A, Riegger GA, Schunkert H.Changes in left ventricular structure and function in patients with white coathypertension: cross sectional survey. BMJ. 1998;317:565–70.
19. Parati G, Ulian L, Sampieri L, Palatini P, Villani A, Vanasia A, et al. Attenuation ofthe ‘‘white-coat effect’’ by antihypertensive treatment and regression of targetorgan damage. Hypertension. 2000;35:614–20.
20. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic impact of baselineand serial changes in electrocardiographic left ventricular hypertrophy inresistant hypertension. Am Heart J. 2010;159:833–40.
21. Dolan E, Stanton A, Thijs L, Hinedi K, Atkins N, McClory S, et al. Superiority ofambulatory over clinic blood pressure measurement in predicting mortality:the Dublin outcome study. Hypertension. 2005;46:156–61.
22. Martins LC, Figueiredo VN, Quinaglia T, Boer-Martins L, Yugar-Toledo JC, MartinJF, et al. Characteristics of resistant hypertension: ageing, body mass index,hyperaldosteronism, cardiac hypertrophy and vascular stiffness. J Hum Hyper-tens. 2011;25:532–8.
23. Palatini P, Julius S. The role of cardiac autonomic function in hypertension andcardiovascular disease. Curr Hypertens Rep. 2009;11:199–205.
24. Pedrinelli R, Dell’Omo G, Penno G, Di Bello V, Giorgi D, Pellegrini G, et al.Microalbuminuria, a parameter independent of metabolic influences in hyper-tensive men. J Hypertens. 2003;21:1163–9.
25. Nogueira Ada R, Fernandes AS, Coutinho ES, Salles GF, Muxfeld ES, Bloch KV.Factors associated with microalbuminuria in resistant hypertension. Int JCardiol. 2007;121:86–7.
26. Armario P, Oliveras A, Hernandez Del Rey R, Poch E, Larrouse M, Roca-CusachsA, et al. Prevalence of target organ damage and factors associated with cardi-ovascular events in subjects with refractory hypertension. Med Clin (Barc).2009;133:127–31.
27. Oliveras A, Armario P, Hernandez-Del Rey R, Arroyo JA, Poch E, Larrousse M,et al. Urinary albumin excretion is associated with true resistant hypertension. JHum Hypertens. 2010;24:27–33.
28. Minutolo R, Borrelli S, Scigliano R, Bellizzi V, Chiodini P, Cianciaruso B, et al.Prevalence and clinical correlates of white coat hypertension in chronic kidneydisease. Nephrol Dial Transplant. 2007;22:2217–23.
29. Zheng J, Ye P, Wang X, Xiao WK, Wu HM. The relationship between obesity andmicroalbuminuria among general population in Beijing area. Zhonghua Nei KeZa Zhi. 2011;50:388–92.
30. Camafort M, Coca A. Resistant hypertension: beyond a bad control of bloodpressure. Med Clin (Barc). 2011;137:444–5.