The Power of Nutrigenomics: A Practical Guide for ... White Paper.pdf · The Power of...
-
Upload
duongtuyen -
Category
Documents
-
view
221 -
download
0
Transcript of The Power of Nutrigenomics: A Practical Guide for ... White Paper.pdf · The Power of...
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 1
The Power of Nutrigenomics:
A Practical Guide for Application in the Treatment of Chronic Illness Advances in the understanding of genetics are changing the way healthcare professionals think about disease causes and prevention. It's now accepted that a person's state-of-health arises from the dynamic interaction of environmental factors with his or her genetic uniqueness. And, nutrition has emerged as a primary environmental factor that can positively or negatively impact the extent to which a person will realize his or her genetic potential. Nutrition research in the past has focused on nutrient deficiencies and impairment of health.1 But the Human Genome Project has led to the concept of “personalized medicine” not only with drugs (pharmocogenetics), but with nutritional modalities as well.1-4 Nutritional genomics—or nutrigenomics—is the “junction between health, diet, and genomics.”1 In other words, nutrigenomics is the effect that nutritive substances and phytochemicals have on genetic expression within human cells. As a growing field of research, nutrigenomics is the recognition of the ability to optimize nutrition for maintaining and extending a state of optimal health.5 This growing field of research has demonstrated the effects that nutrients and botanicals can have on modifying gene expression, prompting the development of research-based nutraceuticals, functional foods, and dietary approaches to address disorders in genetically pre-disposed individals.2,3,5 The Future of Health Care…Here Today New developments in nutrigenomic research are predicted to offer enormous potential for the development of dietary optimization approaches.5 But you won’t have to wait for therapies applying basic and advanced nutrigenomic principals to benefit the health of your patients. They’re already here. Nutrigenomics in clinical practice entails using specified, defined nutrients and nutritional programs to target genetic expression for improved patient outcomes without serious adverse effects. These new, patient-centered approaches to health care rely upon nutrition and other modifiable lifestyle factors to help people achieve optimal genetic expression.
White Paper
Clinically effective modalities for applying nutrigenomics are already in use in a variety of healthcare practices.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 2
Table of Contents The Nutrigenomics Matrix……………………………………………........... 3
3-Phase Plan for Implementing Nutrigenomics……………………......... 4
Phase 1A—Changing Primary Dietary Signals with TLC…………….. 6
Help for Implementing Dietary Signal Changes…………………... 7
Cardiovascular & Insulin Resistance Conditions…………….........8
Inflammatory, Gastrointestinal, Autoimmune & Fatigue
Disorders............................................................................... 8
Hormone Imbalances & Cycle–related Symptoms…….…………. 9
Phase 1B—Changing Primary Dietary Signals with Medical Foods..10
The SKRM Effect: Creating the Next Generation of Medical
Foods…………………………………………………………… 10
Metabolic Syndrome & Cardiovascular Disease………………....11
Inflammatory Bowel Disease (Autoimmune Support)…………... 13
Type 2 Diabetes…………………………………………………….. 14
Chronic Fatigue Syndrome (Live Detoxification Support)………15
Premenstrual Syndrome ………………………………………….. 16
Leaky Gut Syndrome ……………………………………………. 17
Phase 2—Modulating Kinase Signaling with SKRMs………………..18
Insulin SKRMs………………………………………………………. 19
Inflammation & Autoimmune SKRMs…………………………….. 21
Future SKRMs…………………………………………………........ 23
Phase 3—Recommending Key Nutritional Support…………………. 24
Cardiovascular Support……………………………………………. 24
Blood Sugar Metabolism Support………………………………… 25
Liver Detoxification Support……………………………………….. 25
Intestinal Support…………………………………………………… 26
Joint Inflammation Support………………………………………... 27
Hormone Balance Support ……………………………………….. 27
Putting It All Together…………………………………………………… 29
Appendices
Applying Nutrigenomics for Children & Teens…………………... 30
The Need for Therapeutic Lifestyle Changes…………………… 31
References……………………………………………………………….. 32
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 3
The Nutrigenomics Matrix This chart is provided for your reference as a summary of how nutrigenomics can easily be put into practice for the health of your patients. The combination of healthy dietary choices, medical foods, SKRMs, and other targeted nutrients can be a revolutionary avenue of support for those suffering from a number of chronic illnesses. This is the power of nutrigenomics.
Conditions
Dietary Signal
Modification
Medical Food Support
SKRMs
Key
Nutritional Support
Metabolic Syndrome & Cardiovascular Disease (CVD)
FirstLine Therapy®
UltraMeal® PLUS 360° featuring SKRMs UltraMeal® UltraMeal® PLUS
RIAA & Acacia
CoQ10 EFAs
Inflammatory Bowel Disease (IBD)
FirstLine Therapy®
UltraInflamX® PLUS 360° featuring SKRMs UltraInflamX®
RIAA
Glucosamine Chondroitin MSM
Type 2 Diabetes
FirstLine Therapy®
UltraGlycemX® PLUS 360º featuring SKRMs
RIAA & Acacia
Cinnamon Green Tea
Chronic Fatigue Syndrome (liver detoxification support)
FirstLine Therapy®
UltraClear®
UltraClear PLUS®
UltraClear® Plus pH
Proteomic research in progress
Silymarin Catechins Artichoke Leaf Watercress Ellagic Acid
Leaky Gut Syndrome
FirstLine Therapy®
UltraClear SUSTAIN®
Probiotics
Premenstrual Syndrome (PMS)
FirstLine Therapy®
Estrium®
Kudzu Red Clover Turmeric Resveratrol Stabilized I3C
The principles of nutrigenomics can be applied easily in any healthcare practice.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 4
3-Phase Plan for Implementing Nutrigenomics You can easily tailor and prescribe a program for patients presenting with a variety of common and chronic health conditions. A nutrigenomic approach to wellness can include any or all of the following:
1A. Dietary Signal Modification with TLC Western diets, foods of convenience, and other unhealthy dietary habits can “muddle” the signals sent to cells throughout the body, fostering negative genetic (phenotypic) expression that leads to premature aging and disease. What people eat, therefore, may have a direct influence on how they feel. And addressing those eating patterns allows your patients to manage symptoms and even halt or reverse the progression of their illnesses. You can help them make informed decisions that impact their health by offering therapeutic lifestyle changes (TLC). TLC can provide food plans that incorporate nutrigenomic principles for a broad population, then further customize these plans based on patient response, individual concerns, and specific nutritional needs.
1B. Dietary Signal Modification with Medical Foods
Medical foods offer an adjunct approach to dietary recommendations to nutritionally manage specific conditions. A medical food is formulated with macro- and micronutrients that are recognized by scientific principles to support the dietary management of a disease or condition, and is to be administered under the supervision of a physician or licensed healthcare practitioner. Medical foods contain nutrients that typically cannot be acquired through normal dietary measures. Some patients may require a level of nutritional support that simply cannot be met by even a food plan with the best intentions. Medical foods offer a powerful tool, yet can be very simple to implement in your practice.
2. Selective Kinase Response Modulators (SKRMs)
Dietary signals are translated by enzymes known as kinases at the cellular level, helping to direct genetic expression. Selective kinase response modulators—or SKRMs—are nutritional substances that can work to modulate kinase signaling back into balance, helping to restore healthy signaling to genes, favorably affect genetic expression, and reverse the effects of chronic illness.
Adopt a simple, 3-phase plan for applying nutrigenomics in your practice.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 5
Where an unhealthy diet makes the kinase signaling unclear, SKRMs help increase the volume of the message for positive genetic expression and preservation or restoration of health. These research-based nutritional substances offer the newest avenue for a natural approach to wellness that embodies the ideals of nutrigenomics.
3. Targeted Nutritional Support
Even the most comprehensive approach to wellness may require additional nutritional support for maintaining health, addressing specific symptoms, or customizing approaches for patients with multiple health concerns. Outlined here are just a few approaches of the hundreds of possibilities for targeted nutritional applications—from additional support for joint protection and restoring healthy gut ecology to maintaining healthy hormone balance and blood sugar levels.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 6
Phase 1A Changing Primary Dietary Signals with TLC The first step in a nutrigenomics intervention is changing primary dietary signals. Foods contain nutrients serving as dietary signals that travel to cells throughout the body, where they are translated by kinases. Healthy food choices foster healthy signaling. Poor food choices, however, can trigger a disorder of kinase signaling, resulting in poor genetic expression and, ultimately, chronic illness.6,7 In fact, poor nutrition is one of the three leading factors attributed to 70% to 90% of mortalities from chronic illnesses in the U.S. alone.8
Prior to the commercialization of the Western diet, humans (over centuries) developed a relationship with commonly eaten foods. Existing in harmony with these foods meant dietary signals that were adequate to maintain health. Changing the diet with commercialized foods and introducing foreign substances creates a state of cellular stress where messages can be distorted and negatively affect physiological function.6 But these negative dietary signals don’t have to be a part of modern living, nor do the long-term costs of premature aging and chronic disease development.
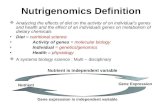
Figure 1. The nutrients (or lack thereof) and other foreign substances (xenobiotics) in a diet can both directly and indirectly influence genetic expression, impacting health.
Unhealthy diets are a leading cause of chronic illness fatalities.
Modifying Genetic Expression
Diet, Exercise & Lifestyle
Nutrients & Xenobiotics
Metabolism
Gene Expression
Cell Phenotype
Signal Transduction
Direct Indirect
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 7
How can you help modify your patients’ dietary signals? This can be accomplished through therapeutic lifestyle changes (TLC). Scientific evidence in support of TLC programs as a fundamental therapy for chronic conditions—including cardiovascular disease (CVD), type 2 diabetes, and obesity—continues to grow.7,9-21 An optimal TLC program should include recommendations for exercise for a comprehensive approach. It should also provide the means and flexibility for further personalization of condition-specific support with nutrients that may not be possible to obtain through dietary measures—or difficult to obtain in therapeutic amounts. Medical foods (Phase 1B on page 10) are designed to complement dietary approaches for the nutritional management of specific conditions. Help for Implementing Dietary Signal Changes The responsibilities of a patient change in the management of chronic disease. Because the patient takes on a caretaker role in the treatment process, greater educational efforts are needed for successful outcomes.22,23 Unfortunately, many practices are set up for acute disease management rather than chronic illness care, and may not be prepared to institute efforts such as lifestyle modification programs.23 FirstLine Therapy® is an example of a TLC program that can help healthcare practitioners teach their patients how to adopt dietary changes that can positively affect kinase signaling to support genetic expression, befitting a longer, healthier life. The FirstLine Therapy food plans are based on a traditional Mediterranean-style eating plan that has an overall low glycemic load (for balancing blood sugar), low in arachidonic acids (anti-inflammatory), and high in phytonutrients. Moreover, the foods have been screened for a history of safe use and for unique molecules that have the ability to modulate kinase signaling in a positive manner. These foods affect signal transduction to help increase the clarity of messages sent to kinases, creating a potential to combat chronic disease and restore optimal wellness. A “disordered” physiology will respond to these new signal conductors, reducing the burden of prior unhealthy eating habits. For optimal support, these dietary changes may be customized—through tailored food plans and medical foods—to meet the specific needs of patients, such as those with conditions related to insulin resistance, cardiovascular disease, autoimmune disorders, inflammatory conditions, fatigue syndromes, and hormone imbalances.
TLC—the first step in harnessing the power of nutrigenomics.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 8
• Cardiovascular & Insulin Resistance Conditions
Many conventional dietary programs recommended by leading health organizations are lowfat, high-carbohydrate diets designed to lower elevated cholesterol levels. However, individuals on these diets may eat high-glycemic-index foods that can cause spikes in blood sugar—increasing hunger, decreasing satiety (feeling of fullness), and fostering insulin resistance and a variety of related health problems. Most importantly, these diets may not produce the desired results.19
Dietary choices causing a high insulin response have been linked to the development of metabolic syndrome, type 2 diabetes, and cardiovascular disease (CVD).12,24-26 Research has demonstrated, for example, that the Western diet—also referred to as the Standard American Diet (SAD)—modulates kinases and insulin signaling.27
Science-based recommendations include reducing consumption of high-glycemic-index foods (e.g., simple sugars, processed and snack foods) and/or replacing them with low-glycemic-index fruits, vegetables, and whole grains.12,28-30 This also adds fiber for a lower overall glycemic load (GL).26
A low-GL food plan promotes healthy blood sugar and energy levels in your patients. Research also links insulin resistance to CVD risk (as is the case in metabolic syndrome), making this an appropriate eating plan for cardiovascular disease.13,19 Low-GL diets have also been shown useful in conditions involving inflammation and oxidative stress, reinforcing its application for CVD patients.21,31
• Inflammatory, Gastrointestinal, Autoimmune & Fatigue Disorders
Diet may also represent a significant immune-modulating part of a patient’s environmental exposure. An increasing body of research suggests that chronic or recurring inflammatory disorders may be reactions to substances that trigger an immune response from the gastrointestinal (GI) tract. Dietary changes may have a noticeable impact on modifying the underlying inflammatory signals that are associated with autoimmune disorders. Scientific studies have demonstrated the effectiveness of dietary therapies in alleviating the symptoms and even in altering the progression of inflammatory and autoimmune conditions.31-49
Research suggests that many common inflammatory and gastrointestinal conditions are triggered by sensitivities or reactions to certain foods and that removing these offending foods may provide relief.32-49 Broad guidelines for eliminating common foods that trigger inflammation can be customized as patients slowly
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 9
challenge the reintroduction of foods to determine those that may exacerbate symptoms. A low-GL diet has also been shown to be beneficial in reducing oxidative stress—the overproduction of damaging free radicals associated with chronic fatigue syndrome and conditions such as rheumatoid arthritis and inflammatory bowel disease (IBD).31 Low-GL foods that are rich in antioxidants—berries, red grapes, garlic, spinach, whole grains—can help restore the body’s balance of antioxidants and combat harmful free radicals generated by environmental toxins, inflammation, and unhealthy lifestyle habits. While a modified elimination diet may provide an approach for long-term condition and symptom management, sometimes a more aggressive, non-fasting dietary approach may be warranted. Some symptoms of chronic fatigue syndrome, for example, may be immediately relieved through a liver detoxification program featuring a more aggressive elimination diet for a shorter term.
Hormone Imbalances & Cycle–related Symptoms In both men and women, unhealthy diets are one of the many factors that influence the body’s ability to balance hormones. Additionally, foods and beverages can include exogenous sources of hormones that overload the body’s natural ability to detoxify and excrete them. Estrogen imbalance in women, for example, may manifest as premenstrual syndrome, irregular menstrual cycles, fibrocystic breast disease, endometriosis, or dysmenorrhea, as well as foster symptoms that impact daily living—hot flashes, night sweats, anxiety attacks, and mood fluctuations. Targeted dietary changes—such as the inclusion of cruciferous vegetables and adaptogenic phytoestrogens like soy—can support the body’s production, use, and excretion of various hormones, particularly estrogen. These dietary changes can positively affect the detoxification of circulating estrogens, thereby creating a positive estrogenic influence on activities at the cellular level.50-55
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 10
Phase 1B Changing Primary Dietary Signals with Medical Foods Food plans and other lifestyle changes may only provide part of the recommendations for changing dietary signals for optimal health support. Medical foods, ever increasing in use, provide an ideal complement to dietary changes to help modify kinase signaling for patients presenting with a variety of conditions, such as those related to dysglycemia and inflammation. Medical foods contain therapeutic levels of nutrients that would be difficult, if not impossible, to achieve through traditional dietary means to support specific conditions. For almost two decades, Metagenics has been one of the few companies to develop and manufacture medical foods. The genesis of these medical foods was based on burgeoning research now known as nutrigenomics. These medical foods are backed by numerous clinical studies and extensive peer-reviewed scientific support. For added assurance and developmental research purposes, these medical foods undergo continual testing in a clinical setting at the Functional Medicine Research CenterSM (FMRC), the clinical research arm of Metagenics. The SKRM Effect: Creating the Next Generation of Medical Foods Medical Foods with the inclusion of SKRMs offer a multi-mechanistic approach to offer even more opportunities for patient success. They represent the latest in medical food development, incorporating nutrigenomic research and technology for a new degree of health support. (For more information on SKRM research, please see Phase 2—Modulating Kinase Signaling with SKRMs on page 18.) The following medical foods are intended to complement dietary recommendations to offer nutritional support for the management of specific conditions. Healthcare practitioners, however, are best qualified to decide on a case-by-case basis when other patients may also benefit from the nutrients provided by formulas designed to address: • Metabolic syndrome • Cardiovascular disease • Inflammatory bowel disease (autoimmune support) • Type 2 diabetes • Chronic fatigue syndrome (liver detoxification support) • Premenstrual syndrome (hormone balance) • Leaky gut syndrome
Medical foods provide powerful signaling nutrients not found in typical diets.
Medical foods containing SKRMs offer a multi-dimensional approach to wellness.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 11
• Metabolic Syndrome & Cardiovascular Disease
UltraMeal® PLUS 360° Medical Food is formulated with the addition of SKRMs—in the form of reduced iso-alpha acids (RIAA, from hops) and acacia extract—to complement the formula’s nutritional support for the management of conditions associated with cardiovascular disease and metabolic syndrome. This advanced formula: o Provides a proprietary soy protein and plant sterol blend that
contains 2 grams of plant sterols (including beta-sitosterol) and 15 grams of soy protein per serving. Foods containing at least 0.65 g per serving of plant sterol esters, eaten twice a day with meals for a daily total intake of at least 1.3 g as part of a diet low in saturated fat and cholesterol, may reduce the risk of heart disease.
o Provides 5-methyl-tetrahydrofolate (5-MTHF)—a body-ready, nature-identical folate—to promote healthy homocysteine levels for cardiovascular health.
o Offers a low-glycemic-index meal option to encourage healthy insulin and blood sugar levels.
o Supplies high quality foundation nutrition for patients with CVD. In individuals with metabolic syndrome and high cholesterol, this advanced medical food formula and accompanying program has been clinically shown to improve the following important cardiovascular risk factors:56 o Lower the apolipoprotein B–to-apolipoprotein A1 (apoB/ApoA1)
ratio o Reduce total cholesterol, LDL cholesterol, and triglyceride levels o Increase HDL (“good”) cholesterol levels o Lower homocysteine levels (See Table 1 on the following page for clinical results.) Also available without SKRMs as UltraMeal® and UltraMeal® PLUS.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 12
* These results are statistically significant. Table 1. The summary of lab value changes from a 12-week, 2-arm study above illustrates the additive affect of a medical food and SKRMs on markers of cardiovascular health. Metabolic outcomes were improved more significantly with a medical food and SKRMs than with a low-GL diet and exercise alone.56
Medical Food with SKRMs Shows Greater Results vs. Dietary Signal Modification & Exercise Alone
Measurement
Arm 1: UltraMeal PLUS 360° with Low-GL Diet
Plan & Exercise
Arm 2: Low-GL Diet
Plan & Exercise Only
Total Cholesterol
-36.74*
-16.33*
Triglycerides
-89.39*
-30.89
HDL-C
2.65*
1.06
LDL-C
-28.38*
-15.06*
TChol/HDL-C
-1.35*
-.61*
TG/HDL
-3.01*
-1.01
ApoA1
-4.00
-8.44
ApoB
-25.70*
-15.06*
ApoB/ApoA1
-.12*
-.05*
Greater Improvement in CV Health Markers
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 13
• Inflammatory Bowel Disease (Autoimmune Support)
UltraInflamX® PLUS 360° Medical Food is formulated with SKRMs—in the form of reduced iso-alpha acids (RIAA, from hops)—to complement the formula’s nutritional support for the management of inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis. This unique medical food: • Provides a low-allergenic-potential protein base in the form of
rice protein concentrate. • Supplies L-glutamine, a valuable energy source for intestinal
mucosal cells. • Provides ginger and rosemary, which may help support healthy
eicosanoid and cytokine metabolism. • Supplies generous levels of turmeric extract, which has been
shown to inhibit the activity of a wide variety of enzymes, cytokines, eicosanoids, and reactive species implicated in pain and inflammation.
• Offers an excellent source of antioxidants with a very high oxygen radical absorbance capacity (ORAC) value.
Advantages of the addition of SKRMs include: • Shown to beneficially influence the function of kinases involved
in inflammatory processes. • Suggested by research to positively influence inflammation-
signaling molecules such as NF-κB, COX-2, and PGE2.
Also available without SKRMs as UltraInflamX® Medical Food.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 14
• Type 2 Diabetes
UltraGlycemX® Medical Food is formulated to meet the specialized nutritional needs of patients with type 2 diabetes, insulin resistance, and hypoglycemia by providing a low-glycemic-index blend that includes high amylose starch (a resistant starch), targeted plant nutrients from green coffee beans and cinnamon, and heart-healthy soy protein and barley ingredients. UltraGlycemX: o Supports healthy heart function by providing 15 grams of soy
protein per serving. Diets low in saturated fat and cholesterol that include 25 grams of soy protein a day may reduce the risk of heart disease.
o Provides 11 grams of specialized dietary fibers per serving to help maintain healthy blood glucose levels in type 2 diabetics.
o Includes green coffee bean extract (containing chlorogenic acid) and barley beta-glucans for support of healthy glucose, lipid, and insulin metabolism.
o Offers a low-glycemic-index meal option to encourage healthy insulin and blood sugar levels.
o Supplies resistant starch that “resists” digestion and is metabolized much like dietary fiber, with positive implications for glucose and insulin metabolism.
o Provides beneficial levels of cinnamon, chromium, biotin, and magnesium to promote healthy glucose uptake and insulin function.
Figure 2. A preliminary, randomized, 2-arm clinical study of 37 insulin-resistant patients showed a greater average decrease when supplementing with an UltraGlycemX formula.57
111
71.5
0
50
100
150
Before Program After 8 Weeks onUltraGlycemX
Program
Insu
lin (μ
IU/m
L)
36% Average Decrease in 2-hr Postprandial Insulin
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 15
• Chronic Fatigue Syndrome (Liver Detoxification Support) UltraClear® Medical Food is formulated to provide readily assimilable macronutrients (protein, carbohydrates, and fats) to help address altered energetic function in patients with chronic fatigue syndrome. o Designed for those patients who may benefit from specific
nutritional support for hepatic detoxification function. o Provides nutrients and antioxidants that support hepatic
detoxification processes. o Provides low-allergenic-potential protein in the form of rice
protein concentrate, which may be beneficial during times of increased hepatic detoxification burden.
o The rice protein concentrate has been prepared via a unique process that reduces its already low allergenic potential.
UltraClear PLUS® Medical Food o Provides the same low-allergenic-potential rice protein base and
macronutrients, but designed for those patients who may benefit from specific nutritional support for Phase II hepatic detoxification function with the addition of:
– Glycine to support Phase II glycine conjugation – Magnesium sulfate and L-cysteine to support Phase II
sulfation o Also provides green tea catechins and mixed carotenoids to
protect against reactive species generated during hepatic detoxification.
UltraClear® Plus pH Medical Food o Provides the same low-allergenic-potential rice protein base and
macronutrients, but designed for those patients who may benefit from specific nutritional support to promote alkalinization of urine and Phase II hepatic detoxification function with the addition of:
– Potassium citrate to promote alkalinization of urine – Sesame (a source of sesamin) to help support Phase II
hepatic metabolism of lipids (including cholesterol) and other substances
– Glycine and taurine to support Phase II amino acid conjugation
– Magnesium sulfate to support Phase II sulfation
Further personalize an approach by identifying those patients with needs for additional detoxification support.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 16
• Premenstrual Syndrome (PMS)
Estrium® Medical Food is formulated to provide specialized nutritional support for premenstrual syndrome by supplying flaxseed, isoflavones, and targeted nutrients. This targeted formula:
o Supports healthy estrogen metabolism and balance with
flaxseed and non-soy isoflavones (from kudzu). o Supplies generous levels of vitamin E, vitamin B6, calcium,
magnesium, and chromium to address particular concerns associated with PMS.
o Offers a low-glycemic-index meal option to help support healthy energy and insulin metabolism.
o Provides turmeric extract, which has been shown in research to inhibit the activities of a wide variety of enzymes, cytokines, eicosanoids, and reactive species implicated in pain and inflammation.
Figure 3. In a clinical study of 40 PMS patients following the Estrium program for two menstrual cycles there was a significant improvement in symptoms as measured by the Shortened Premenstrual Assessment Form (scores from 10 to 30 indicate symptomatology in the last half of the cycle).58
0
20
40
60
Before Program After EstriumProgram
SP
AF
Tota
l Sco
re
59% Reduction in PMS Symptoms
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 17
• Leaky Gut Syndrome
UltraClear SUSTAIN® Medical Food is formulated to provide specialized nutritional support, including L-glutamine and readily assimilable, low-allergenic-potential macronutrients for patients with leaky gut syndrome. o Provides L-glutamine, a valuable energy source for intestinal
mucosal cells. o Addresses dysbiosis associated with leaky gut syndrome by
providing inulin and fructooligosaccharides (FOS) to promote the growth of healthy intestinal bacteria.
o Provides prebiotic factors, which encourage the production of short-chain fatty acids (SCFAs) that promote intestinal mucosal health and a healthy intestinal environment.
o The rice protein concentrate has been prepared via a unique process that reduces its already low allergenic potential.
Medical Food Nutritional Profiles & Research Nutritional information for the medical foods mentioned in this document is available at www.metagenics.com. In addition to extensive developmental research and clinical studies, these medical foods undergo continual testing in a clinical setting at the Functional Medicine Research Center. Individual case management studies with medical foods are available for viewing at www.metagenics.com in the resources section: www.metagenics.com/science/case_studies.asp?sect=2
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 18
Phase 2 Modulating Kinase Signaling with SKRMs Nutrigenomic research, such as that conducted by the MetaProteomics® Nutrigenomics Research Center, attempts to discover highly active substances from food and other natural sources that can serve as potent dietary signaling molecules to positively affect genetic expression. Optimally, this yields the development of unique food ingredient extracts from which individual bioactive molecules can be isolated and tested for their ability to modify cellular function related to various disease processes. Many prevalent health issues have been found to have specific underlying kinase signaling components. This is due to the ability of kinases to translate dietary signals in a positive or negative manner to influence health. For example, research has shown that impaired kinase signaling can lead to impaired insulin response and hyperlipidemia associated with type 2 diabetes.59 Kinases are enzymes that chemically modify other proteins and regulate the majority of cellular pathways—particularly those involved in the transmission of intracellular signals. These enzymes also help regulate eicosanoids, cytokines, reactive oxygen species, and other mediators that may negatively impact the body both locally and systemically.
Figure 4. SKRMs positively affect kinase signaling for optimal genetic and phenotypic expression for wellness. SKRMs are an ideal complement to positive dietary changes for restoration of healthy kinase activities.
Diet, Exercise & Lifestyle
Nutrients & Xenobiotics
Metabolism
Gene Expression
Cell Phenotype
Signal Transduction
Direct Indirect SKRMs
SKRMs provide another nutritional modality to modulate cellular signals.
Modifying Genetic Expression with SKRMS
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 19
As mentioned previously, SKRMs are nutritional substances that can work to modulate kinase signaling back into balance. This balance helps restore healthy signaling to genes for positive genetic expression and reversal of illness. Proprietary research has yielded the discovery of food-derived SKRMs that specifically inhibit kinase-mediated processes associated with insulin resistance and inflammation. SKRMs may offer therapeutic advantages over dietary modifications alone. Insulin SKRMs Groundbreaking preliminary research suggests the identification of SKRMs that have the ability to improve insulin sensitivity by modulating specific kinase enzymes that serve as “hubs” for insulin-signaling processes. More than 200 natural substances and extracts were tested for their influence on insulin responses and adipocyte (fat-storing) cells at the MetaProteomics Nutrigenomics Research Center. A combination of reduced iso-alpha acids (RIAA) derived from hops (Humulus lupulus) and acacia extract (Acacia nilotica) was shown via in vitro testing to inhibit inflammatory markers that influence insulin function.60 Research has implicated dysregulated inflammatory processes in the development of insulin resistance, and several inflammation-induced cytokines have been shown to be expressed during insulin resistance and metabolic syndrome.61-63 Cytokines—such as interleukin-1 beta (IL-1β), tumor necrosis factor alpha (TNF-α), and interferon gamma (IFN-γ)⎯have been shown to play a role in cytokine-induced β-cell dysfunction in diabetes.64,65
In human clinical testing at the Functional Medicine Research Center, supplementation of metabolic syndrome subjects with a combination of RIAA and acacia led to greater reduction of 2 h pp insulin levels, as compared to placebo. Furthermore, greater decreases of fasting insulin, fasting and 2 h pp glucose, fasting triglyceride, and HOMA scores were observed in subjects taking RIAA/acacia supplement versus subjects taking placebo. These collective results indicate RIAA/acacia supplementation might be useful in maintaining insulin homeostasis in subjects with metabolic syndrome.60
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 20
Insulin SKRM Research
Figure 5. The Homeostasis Model Assessment (HOMA) estimates steady state beta cell function and insulin sensitivity, and is a published measure of insulin resistance. A significant decrease was observed for the RIAA/acacia group as compared to the placebo group in an 8-week clinical trial.60
Figure 6. In the same blinded, placebo-controlled study of 91 patients, the RIAA/acacia blend showed a greater improvement in triglyceride levels than placebo.60
-1.48
-48.97-55
-45
-35
-25
-15
-5
Placebo RIAA/Acacia Blend
Trig
lyce
rides
0.16
0.78
0
0.2
0.4
0.6
0.8
1
Placebo RIAA/Acacia Blend
HO
MA
Increased Insulin Sensitivity with SKRMs
Improvement in Triglycerides with SKRMs
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 21
Inflammation & Autoimmune SKRMs Chronic inflammation, nutritional deficiencies, and oxidative stress are believed to be involved in the pathogenesis of autoimmune disorders. Mounting scientific evidence indicates that inflammation is also intrinsic to autoimmune conditions. In fact, during inflammation, an array of cytokines, eicosanoids, reactive oxygen species, and other mediators that can overwhelm and disrupt Th1/Th2 balance are released, which can potentially damage body tissues.66-69
People with chronic inflammation often have excess proinflammatory mediators. The present direction of research is the development of therapeutic agents that modulate the immune system by targeting specific cell types involved in the inflammatory response.
SKRMs in the form of reduced iso-alpha acids derived from hops (Humulus lupulus) have been extensively tested for safety and effectiveness and professionally recommended as a safer option for joint relief for over 5 years—offering a high level of predicted cardiovascular, gastric, renal, and liver safety.70-78
RIAA still offers an excellent SKRM approach to inflammatory and autoimmune conditions. Recent nutrigenomics research, however, has identified even more powerful SKRMs from hops. Like RIAA, these new constituents, tetrahydro-iso-alpha acids (THIAA), offer a safer approach to modulating the arachidonic acid cascade. THIAA have also been extensively researched and tested—demonstrating the ability to modulate specific kinases associated with activities underlying joint tissue health and immune function, such as PGE2 and TNF-α.
THIAA have been shown in scientific testing to provide even greater targeted support with lower clinically effective dosing. In fact, in studies at MetaProteomics, THIAA have been shown to modulate induced PGE2 production with two times greater effectiveness than RIAA, and to modulate induced TNF-α production with three times greater effectiveness.
Additional Support for Autoimmune Conditions
Common nutritional deficiencies associated with abnormal autoimmune response include inadequate vitamin D intake.79-81 The role of selenium and zinc has also been the source of heightened interest because of the role these nutrients play in metabolic processes involving joint tissues and immune system function.82-86
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 22
Inflammation & Autoimmune SKRM Research
PG
E2(
pg/m
l)
Concentration (μg/ml)
0
500
1000
1500
2000
2500
2.5 5.0
ControlTHIAARIAA
PG
E2(
pg/m
l)
Concentration (μg/ml)
0
500
1000
1500
2000
2500
2.5 5.0
ControlTHIAARIAA
Figure 7. Cells were pre-incubated with THIAA or RIAA, followed by lipopoly-saccharide (LPS)-induced stimulation of PGE2 production. The data show that compared to the control and RIAA, THIAA inhibits PGE2 expression more effectively.
Figure 8. Cells were pre-incubated with THIAA and then stimulated with LPS to induce TNF-α production. Results show that THIAA can lead to greater inhibition of TNF-α expression in a dose-dependent manner.
0
500
1000
1500
2000
2500
10.0 20.0
TNF-α(p
g/m
l)
Concentration (μg/ml)
Control THIAA
PGE2 Inhibition with SKRMs
TNF-α Inhibition with SKRMs
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 23
Future SKRMs
Nutrigenomic research continues to focus on naturally derived substances that act as SKRMs to beneficially influence health in other areas, such as liver detoxification, bone resorption, and hormone balance.
For more information on nutrigenomic research and the development of innovative nutritional protocols, please visit: www.metaproteomicslabs.com
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 24
Phase 3 Recommending Key Nutritional Support The following nutrients may provide complementary support for certain patients and offer a flexible and highly customizable nutrigenomic approach to wellness. Cardiovascular Support Coenzyme Q10 (CoQ10 or ubiquinone) and essential fatty acids (omega-3s) are both important for cardiovascular health. In addition to complementing nutrigenomic therapies, they may also play key roles in conventional therapies for CVD. • CoQ10—CoQ10 plays an important role in the body’s energy-
producing process. The body’s endogenous production of CoQ10 decreases with age and dietary availability and absorption of CoQ10 is rather limited, prompting the need for supplementation to correct a deficiency.87-89 CoQ10 deficiency has been observed in patients with a variety of cardiovascular conditions—and patients with more advanced stages of CVD have been shown to possess lower levels of CoQ10 than patients with milder forms of CVD.90-93
CoQ10 levels can be further impacted by drugs in conventional therapies, such as statins that block its synthesis.94-96 Fortunately, statin-induced CoQ10 deficiency can be prevented with supplemental CoQ10 with no adverse impact on the cholesterol-lowering or anti-inflammatory properties of statin drugs.96,97 Scientific studies have also shown that CoQ10 may be recommended as preventive therapy or as a safe and effective adjunct to conventional therapy for CVD.87-92,97
• Essential Fatty Acids (EFAs)—Omega-3 fatty acids, such as those found naturally in cold-water fish (including EPA and DHA), have been examined in previous clinical and epidemiological research that has shown they may: 98-105
o Decrease the risk of fatal arrhythmias o Decrease triglyceride levels o Decrease growth rate of atherosclerotic plaque o Lower blood pressure (slightly) o Decrease the chance of stroke
Note: Clinical tests have also shown that people with diets rich in EPA are less prone to inflammation in joints, intestines, lungs, and skin.
Targeted nutrients offer another means of positive dietary signaling.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 25
Blood Sugar Metabolism Support Ever-growing research continues to show the newly discovered benefits of green tea and cinnamon in complementing dietary approaches to blood sugar management. Insulin resistance conditions can also induce oxidative stress that can lead to vascular complications, such as neuropathy. • Cinnamon—Cinnamon has been shown to display insulin-enhancing
activity in vitro and shown in human clinical trials to positively influence glucose levels.106-108 Extracts of cinnamon have also been shown to activate insulin receptor kinase and inhibit dephosphorylation of the insulin receptor—leading to increased insulin sensitivity.
• Green Tea (EGCG)—Green tea contains epigallocatechin gallate
(EGCG), a bioflavonoid shown to protect pancreatic islet cells and enhance insulin sensitivity.109 Catechins from green tea also provide strong antioxidant protection.110
Liver Detoxification Support
There are two primary phases in the detoxification process. In Phase I, fat-soluble toxins are transformed into intermediate compounds that are more reactive, but will bind more easily to non-toxic, water-soluble molecules in Phase II. In Phase II, formation between the reactive intermediates and water-soluble molecules make the entire compound ready for excretion out of the body. Targeted nutrients can influence detoxification activities in either phase—or sometimes both.
• Silymarin—This active constituent of milk thistle (Silybum marianum) is well-recognized for its beneficial effects on protecting the liver from toxins and stimulating liver regeneration, as well as its antioxidant properties. Preliminary research also indicates that it may influence Phase I and Phase II enzymes, and therefore may be called a bifunctional modulator.111,112
• Catechins—These strong antioxidants have the capacity to
scavenge most oxygen free radicals.110 Also derived from green tea (Camilla sinensis, see above), catechins enhance the induction of Phase II enzymes—glutathione S-transferase and quinine reductase—and inhibit the overinduction of specific cytochrome P450 Phase I biotransformation enzymes.113,114
• Watercress—Glucosinolates found in watercress (Nasturtium
officinale) are precursors of phenythyl isothicynate (PEITC), which effectively inhibits the overinduction of specific sytochrome P450
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 26
enzymes and enhances Phase II glutathione S-transferase and quinine reductase.115-117
• Ellagic Acid—Naturally found in pomegranate fruit (Punica
granatum), ellagic acid beneficially modulates Phase I biotransformation and enhances Phase II glutathione S-transferase and quinine reductase enzyme induction.118-120 Also scavenges superoxide radicals and hydroxyl radicals, reducing hepatic oxidative stress.120,121
Note: Catechins, watercress, and ellagic acid also influence genetic expression of enzymes that control Phase II conjugation reactions.113-120
• Artichoke Leaf—Extracts from artichoke (Cynara scolymus) have a
long history of traditional use in promoting liver function. Research suggests that several constituents of artichoke, including chlorogenic acid and cynarin, have marked antioxidant and hepatoprotective properties.122-124
Intestinal Support Probiotic strains have specific characteristics that determine whether they have the ability to benefit the intestinal environment. But not all genera, species, and strains are suitable for all purposes. Following are beneficial bacteria shown to adhere to the intestinal lining and support a healthy balance of microflora.125-130
• Lactobacillus acidophilus NCFM®—This strain of human origin has
been proven safe and effective by more than 60 scientific studies and almost 30 years of commercial use. It produces lactic acid, hydrogen peroxide, and other natural substances while modulating the activity of enzymes—such as β-glucuronidase, nitroreductase, and azoreductase—to positively influence the balance of intestinal bacteria and support intestinal tissue health.125 It’s also one of a limited number of Lactobacillus species shown to adhere in the intestines.131
• Bifidobacterium—This major group of carbohydrate-metabolizing
bacteria in the intestines (including B. lactis) is 1000 times more abundant than lactobacilli in healthy adults (and some researchers believe more important as well).132 Bifidobacteria have proven effectiveness as immunosupportive agents that enhance host resistance, as well as produce strong acids (e.g., acetic, lactic) that positively affect intestinal pH; thereby, playing a critical role in modulating ammonia, phenol, steroidal, and other toxin levels to maintain health and support intestinal microbial balance.125-127
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 27
Note: Scientific identification of strains is not only an indicator of predicted safety, but assures the means for providing optimal health benefits.
Joint Inflammation Support Many inflammatory and autoimmune conditions are characterized by pain and motility concerns related to the joints. Glucosamine and chondroitin sulfates, as well as MSM, offer widely accepted approaches for maintaining healthy connective tissue and relieving pain associated with concerns that affect a growing number of patients. • Glucosamine & Chondroitin—These nutrients are naturally found in
healthy tissue and work together in forming healthy joint matrix cartilage and enhancing joint lubrication.133,134 They may also promote the incorporation of sulfur into cartilage. Sulfur is necessary for the synthesis of collagen and improves the moisture content of cartilage, supporting its shock-absorbing ability.135 Supplementation with glucosamine and chondroitin can help restore normal joint motility and relieve pain.133,135-138 Continued use is required to maintain benefits.
• Methyl-Sulfonyl-Methane (MSM)—This natural compound
complements glucosamine and chondroitin sulfates, and also provides a highly biologically valuable source of sulfur. MSM has been widely used to support joint health and relieve pain as an effective natural analgesic and anti-inflammatory agent.139 A randomized, placebo-controlled trial showed that MSM improved symptoms of pain and physical function in patients with osteoarthritis.140 Another randomized, double-blind, parallel, placebo-controlled trial also showed that MSM significantly improved the signs and symptoms of osteoarthritis. Furthermore, the combination of glucosamine and MSM showed better efficacy in reducing pain and swelling and in improving the functional ability of joints than the individual agents.139
Hormone Balance Support Phytoestrogens are plant compounds that have structural and functional similarities to estrogen.55,141 Selective estrogen receptor modulators (SERMs—not to be confused with SKRMs) are non-steroidal compounds capable of binding to the estrogen receptors and influencing their activities. Specifically, SERMs are noted as being both agonists (in cases of low estrogen levels, such as with menopause) and antagonists (in cases of high estrogen). Because they support a moderate level of estrogen activity, upon binding to the estrogen receptors they inhibit endogenous estrogen when too much is present, but can still support estrogen’s important functions.142-144
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 28
• Kudzu & Red Clover—Provide a varied profile of non-soy isoflavones and isoflavone glycosides—including daidzein, genistein, puerarin, and fromononetin—that bind to the estrogen receptor and may act as weaker estrogens, resulting in an inhibition of the estrogenic effect.50,144-146
• Turmeric—Curcuminoids, the active component in turmeric
(Curcuma longa), induce glutathione production and glutathione-S transferase activity—helping to protect tissues from reactive estrogen metabolites.147 In combination with isoflavones, curcumin shows in vitro evidence of reducing xenoestrogens-induced growth in estrogen receptor-positive and –negative cancer cells, thereby promoting breast health.55,148
• Resveratrol (from Polygonum cuspidatum)—Classified as a SERM
based on its ability to bond to estrogen receptors and act as both an estrogen agonist and antagonist. Resveratrol provides many other benefits, including cardioprotective properties.149 Resveratrol has been shown to promote healthy cytokine production by influencing the cyclooxygenase and 5-lipoxygenase pathways. It is also associated with reduced activity of nuclear factor kappaB (NF-кB)—a transcription factor that may promote the expression of undesirable genes. Resveratrol has potent antioxidant activity (especially in lipids that are highly concentrated in brain tissue), promotes healthy blood flow, and induces hepatic phase II detoxification activity.
• Stabilized Indole-3-Carbinole (I3C)—This naturally occurring
compound found in cruciferous vegetables protects estrogen-sensitive tissues by promoting the formation of 2-hydroxyestrone, diindolymethane (DIM), and other beneficial estrogen metabolites. It supports the detoxification of estrogens, other steroid hormones, and xenoestrogens by enhancing the activity of enzymes involved in their metabolism and excretion. Research indicates great promise as a natural hormone-balancing agent.150-157
Note: Natural-source I3C may be an important consideration when recommending supplementation to patients.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 29
Putting It All Together The Nutrigenomics Matrix (provided on page 3) gives you a top-line overview of implementing nutrigenomics in your practice for a broad range of patients. Determine the appropriate level of support for your patients, as well as the components that complement the structure of your practice. For further assistance, the FirstLine Therapy program also provides diagnostic tools and assistance in determining appropriate nutritional support based on symptoms and in-office measurements. It also provides helpful materials for educating and motivating patients, as well as monitoring their progress. As always, the Metagenics Technical Support team of professionals is available to answer questions regarding products and clinically tested nutritional protocols. About Metagenics, Inc. Metagenics is a life sciences company and leading developer and manufacturer of professional grade, science-based medical foods and nutraceuticals sold to healthcare practitioners worldwide. For more than 25 years, Metagenics has been a leader in quality, scientific discovery, and innovation, with multiple proprietary formula patents and more than 400 research-based products to optimize health. The company is headquartered in San Clemente, CA, with manufacturing and research facilities located in Gig Harbor, WA, including the MetaProteomics® Nutrigenomics Research Center and the Functional Medicine Research CenterSM for human clinical research. For more information, please visit www.metagenics.com.
FirstLine Therapy® is a registered trademark of Metagenics, Inc.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 30
APPENDIX A Applying Nutrigenomics for Children & Teens A nutrigenomic approach to wellness doesn’t have to wait until adulthood. With the rise of metabolic syndrome and other conditions in children and teenagers, your younger patients may already be in need of some beneficial signal modification. And you can help them now. The following medical food programs offer targeted nutritional support and complementary dietary programs to address the nutritional management needs of children and teens. Customize these programs with other nutrients to address specific needs. Metabolic Syndrome Ultracare First Start™ Medical Food is formulated to provide specialized nutritional support for children and adolescents ages 6-18 with metabolic syndrome, obesity, dyslipidemia, and insulin resistance by supplying a low-glycemic-index blend of macro- and micronutrients, including cinnamon, chromium, and heart-healthy soy protein and isoflavones. This unique formula: • Addresses the protein needs of growing children and teenagers by
providing 6-12 grams of soy protein per serving. • Supplies cinnamon to help maintain healthy glucose and insulin
function. • Provides a good source of dairy-free calcium and magnesium to
support peak bone mass development. Atopic Disorders Ultracare for Kids® Medical Food is formulated to provide specialized nutritional support for children with food allergy-related symptoms and atopic disorders by supplying readily assimilable, low-allergenic-potential rice protein. • Low-allergenic-potential rice protein to complement restricted diets. • The rice protein has been prepared via a unique process that
reduces the already low-allergenic potential of rice protein. • Provides fructooligosaccharides (FOS) to promote the growth of
bifidobacteria, which may help encourage healthy, balanced immune function in young children.
• Supplies dairy-free calcium to support bone health and new bone formation.
• Provides high quality foundation nutrition for children up to 12 years of age.
Comprehensive dietary recommendations and other lifestyle guidelines are available for parents to help implement and monitor.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 31
APPENDIX B The Need for Therapeutic Lifestyle Changes A white paper discussion on the scientific basis for and effectiveness of therapeutic lifestyle changes (TLC) programs has been prepared for your reference. This paper is entitled “The Chronic Disease Epidemic: A Prescription of Primary Prevention and Profitability” and is available upon request at: www.metagenics.com/flt/whitepaper_request.asp Also included are practical tips for evaluating a TLC program to fit the needs of your practice. Further information for patients and practitioners on the FirstLine Therapy TLC program is also available at www.metagenics.com.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 32
References 1. Alffman L, Muller M. Nutrigenomics: from molecular nutrition to prevention of disease. J M Diet Assoc.
2006;106(4):569-576. 2. Subbiah MT. Nutrigenetics and nutraceuticals: the next wave riding on personalized medicine. Transl Res.
2007;149(2):55-61. 3. Mariman EC. Nutrigenomics and nutrigenetics: the ‘omics’ revolution in nutritional science. Biotechnol Appl
Biochem. 2006;44(Pt 3):119-128. 4. Kaput J. Nutrigenomics—2006 update. Clin Chem Lab Med. 2007;45(3):279-287. 5. Ferguson LR. Nutrigenomics: integrating genomic approaches into nutrition research, Mol Diag Ther.
2006;10(2):101-108. 6. Bland JS. What role has nutrition been playing in our health? The xenohormesis connection. 2007 [In press.] 7. Roberts CK, Barnard RJ. Effects of exercise and diet on chronic disease. J Appl Physiol. 2005;98:3-30. 8. Aldan SG, Greenlaw RL, Diehl HA, et al. The behavioral and clinical effects of therapeutic lifestyle changes
on middle-aged adults. Preventing Chronic Disease. 2006;3(1):1-16. 9. Ashley JM, St. Jeor ST, Schrage JP, et al. Weight control in the physician’s office. Arch Intern Med
2001;161:1599-1604. 10. Woollard J, Burke V, Beilin LJ, et al. Effects of a general practice-based intervention on diet, body mass
index and blood lipids in patients at cardiovascular risk. J Cardiovasc Risk 2003;10(1):31-40. 11. Mattila R, Malmivaara A, Kastarinen M, et al. Effectiveness of multidisciplinary lifestyle intervention for
hypertension: a randomized controlled trial. J Hum Hypertens 2003;17(3):199-205. 12. Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N
Engl J Med 2001;345(11):790-97. 13. Case CC, Jones PH, Nelson K, et al. Impact of weight loss on the metabolic syndrome. Diabetes Obes
Metab 2002;4(6):407-14. 14. O’Reilly S, Doherty M. Lifestyle changes in the management of osteoarthritis. Best Pract Res Clin
Rheumatol 2001;15(4):559-68. 15. The North American Menopause Society. Management of osteoporosis in postmenopausal women: 2006
position statement of The North American Menopause Society. Menopause 2006;13(3):340-67. 16. Preuss HG, Bagchi D, Bagchi M. Protective effects of a novel niacin-bound chromium complex and a grape
seed proanthocyanidin extract on advancing age and various aspects of syndrome X. Ann N Y Acad Sci 2002;957:250-59.
17. Gordon NF, Salmon RD, Franklin BA, et al. Effectiveness of therapeutic lifestyle changes in patients with hypertension, hyperlipidemia, and/or hyperglycemia. Am J Cardiol. 2004;94:1558-1561.
18. Aldana SG, Greenlaw RL, Diehl HA, et al. Effects of an intensive diet and physical activity modification program on the health risks of adults. J Am Diet Assoc. 2005;105:371-381.
19. Wannamethee SG, Sharper AG, Whincup PH. Modifiable lifestyle factors and the metabolic syndrome in older men: effects of lifestyle changes. J Am Geriatr Soc. 2006;54:1909-1914.
20. Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2201;344:1343-1350.
21. Esposito K, Marfella R, Ciotola M, et al. Effects of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: a randomized trial. JAMA. 2004;292(12):1440-1446.
22. Holman H. Chronic disease—the need for a new clinical education. JAMA. 2004;292(9):1057-1059. 23. Casalino LP. Disease management and the organization of physician practice. JAMA. 2005; 293(4):485-
488. 24. Roche HM, Phillips C, Gibney MJ. The metabolic syndrome: the crossroads of diet and genetics. Proc Nutr
Soc. 2005;64:371-377. 25. Kendal CW, Augustin LS, Emam A, Josse AR, Saxena N, Jenkins DJ. The glycemic index: methodology and
use. Nestle Nutr Workshop Ser Clin Perform Programme. 2006;11:43-56. 26. Hyman, Mark. UltraMetabolism: The Simple Plan for Automatic Weight Loss. New York: Scribner, 2006. 27. Prada PO. Gottardello, Zecchin H, Lia Gaspaparetti A, et al. Western diet modulates insulin signaling, c-Jun
N-terminal kinase activity, and insulin receptor substrate-1 [ser307] phosphorylation in a tissue-specific fashion. Endocrinology. 2005;146(3):1576-1587.
28. Pins JJ, Keenan JM. Dietary and nutraceutical options for managing the hypertriglyceridemic patient. Prog Cardiovasc Nurs. 2006;21(2):89-93.
29. Deen D. Metabolic syndrome: time for action. Am Fam Physician. 2004;69(12):2875-882. 30. Deedwania PC, Volkova N. Current treatment options for the metabolic syndrome. Curr Treat Options
Cardiovasc Med. 2005;7(1):61-74. 31. Hu Y, Block G, Norkus EP, Morrow JD, Dietrich M, Hudes M. Relations of glycemic index and glycemic load
with plasma oxidative stress markers. Am J Clin Nutr. 2006;84(1):70-76. 32. Stamp LK, James MJ, Cleland LG. Diet and rheumatoid arthritis: a review of the literature. Semin Arthritis
Rheum 2005;35(2):77-94. 33. van de Laar, MA, van der Korst JK. Food intolerance in rheumatoid arthritis. I. A double blind, controlled trial
of the clinical effects of elimination of milk allergens and azo dyes. Ann Rheum Dis 1992;51(3):298-302. 34. Pena AS, Crusius JB. Food allergy, coeliac disease and chronic inflammatory bowel disease in man. Vet Q
1998;20 Suppl 3:S49-52. 35. Stark ME, Tremaine WJ. Maintenance of symptomatic remission in patients with Crohn’s disease. Mayo Clin
Proc 1993;68(12):1183-90. 36. Khan S, Orenstein SR. Eosinophilic gastroenteritis: epidemiology, diagnosis and management. Paediatr
Drugs 2002;4(9):563-70. 37. Ebo DG, Stevens WJ. IgE-mediated food allergy—extensive review of the literature. Acta Clin Belg
2001;56(4):234-47. 38. Sullivan PB. Food allergy and food intolerance in childhood. Indian J Pediatr 199;66(1 Suppl):S37-45. 39. Caffarelli C, Cavagni G, Menzies IS, Bertolini P, Atherton DJ. Elimination diet and intestinal permeability in
atopic eczema: a preliminary study. Clin Exp Allergy 1993;23(1):28-31. 40. Atherton DJ. Role of diet in treating atopic eczema: elimination diets can be beneficial. BMJ
1988;277(6661):1458,1460. 41. Veien NK, Hattel T, Justesen O, Norholm A. Dietary restrictions in the treatment of adult patients with
eczema. Contact Dermatitis 1987;17(4):223-28.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 33
42. Fogg MI, Spegel JM. Management of food allergies. Expert Opin Pharmacother 2003;4(7):1025-1037. 43. Garcia-Careaga M Jr, Kerner JA Jr. Gastrointestinal manifestations of food allergies in pediatric patients.
Nutr Clin Pract 2005;20(5):526-35. 44. Veien NK, Hattel T, Justesen O, Norholm A. Oral challenge with food additives. Contact Dermatitis
1987;17(2)100-103. 45. Burr ML, Fehily AM, Stott NC, Merrett TG. Food-allergic asthma in general practice. Hum Nutr Appl Nutr
1985;39(5)349-355. 46. Atkinson W, Sheldon Tam Shaath N, Whorwell PJ. Food elimination based on IgG antibodies in irritable
bowel syndrome: a randomised controlled trial. Gut 2004;53(10):1459-1464. 47. Hafstrom I, Ringertz B, Spanberg A, et al. A vegan diet free of gluten improves the signs and symptoms of
rheumatoid arthritis: the effects on arthritis correlate with a reduction in antibodies to food allergens. Rheumatology (Oxford) 2001;40(10):1175-1179.
48. Galli E, Cicconi R, Rossi P, Casati A, Brunetti E, Mancino G. Atopic dermatitis: molecular mechanisms, clinical aspects and new therapeutic approaches. Curr Mol Med 2003;3(2):127-138.
49. Darlington LG, Ramsey NW. Review of dietary therapy for rheumatoid arthritis. Br J Rheumatol 1993;32(6):507-14.
50. Cassidy A. Potential tissue selectivity of dietary phytoestrogens and estrogens. Curr Opin Lipid. 1999:10:47-52.
51. Keck AS, Finley JW. Cruciferous vegetables: cancer protective mechanisms of glucosinolate hydrolysis products and selenium. Integr Cancer Ther. 2004;3(1):5-12.
52. Setchell KD. Soy isoflavones—benefits and risks from nature’s selective estrogen receptor modulators (SERMs). J Am Coll Nutr. 2001;20(5 Suppl):354S-362S.
53. Ganry O. Phytoestrogen and breast cancer prevention. Eur J Cancer Prev. 2002;11(6):519-522. 54. Xu X, Duncan AM, Wangen KE, Kurzer MS. Soy consumption alters endogenous estrogen metabolism in
premenopausal women. Cancer Epidemiol Biomarkers Prev. 200;9(8):781-786. 55. Cos P, DeBruyne T, Apers S, Vanden Burrghe D, Pieters L, Vlietinck AJ. Phytoestrogens: recent
developments. Planta Med. 2003;69:589-599. 56. Lerman RH, Bland JS, Darland G, Lamb JJ, Minich DM, Schiltz B, Trip ML. Supplementation with a novel
selective kinase response modulator (SKRM) nutraceutical and medical food significantly enhances the benefits of a diet and exercise program in subjects with metabolic syndrome. Functional Medicine Research Center, Gig Harbor, WA. [In preparation.]
57. Lukaczer D, Lerman R, Schiltz B, et al. A pilot trial comparing the effects of identical weight loss diet programs with or without additional nutrient supplementation in subjects with insulin resistance and hyperinsulinemia. Gig Harbor, WA: Functional Medicine Research Center; Research Report No. 105, 2000.
58. Lukaczer D, Liska DJ, Darland G, et al. Improvement in symptoms and estrogen metabolism in women with premenstrual syndrome using a newly formulated medical food. Gig Harbor, WA: Functional Medicine Research Center; Research Report No. 110, 2001.
59. Luo J, Sobkiw CL. Hirshman MF, Logsdon MN, et al. Loss of class IA PI3K signaling in muscle leads to impaired muscle growth, insulin response, and hyperlipidemia. Cell Metab. 2006;3(5):355-366.
60. Lerman RH, Tripp ML, Bland JS. Double-blind, placebo-controlled trial examining the effects of RIAA/acacia supplementation on insulin homeostasis. Functional Medicine Research Center, Gig Harbor, WA.
61. Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW. C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscle Thromb Vasc Biol. 1999;19:972-978.
62. Mohamed-Ali V, Goodrick S, Rawesh A, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-α, in vivo. Endocrinol Metab. 1997;82:4196-4200.
63. Lundgren CH, Brown SL, Nordt TK, Sobel BE, Fujii S. Elaboration of type-1 plasminogen activator inhibitor from adipocytes. A potential pathogenetic link between obesity and cardiovascular disease. Circulation. 1996;93:106-110.
64. Heitmeier MR, Kelly CB, Ensor NJ, et al. Role of cyclooxygenase-2 in cytokine-induced β-cell dysfunction and damage by isolated rat and human islets. J Biol Chem. 2004;279:53145-53151.
65. McDaniel ML, Kwon G, Hill JR, Marshall CA, Corbett JA. Cytokines and nitric oxide in islet inflammation and diabetes. Proc Soc Exp Biol Med. 1996;211:24-32.
66. Elenkov IJ, Iezzoni DG, Daly A, et al. Cytokine dysregulation, inflammation and well-being. Neuroimmunomodulation. 2005;12(5):255-269.
67. Cook ME. Regulation of eicosanoid pathways: a pathway to health and development. Pakistan J Nut. 2002;1(2):103-105.
68. Kidd P. Th1/Th2 balance: the hypothesis, its limitations, and implications for health and disease. Altern Med Rev. 2003;8(3):223-246.
69. Skapenko A, Leipe J, Lipsky PE, et al. The role of the T cell in autoimmune inflammation. Arthritis Res Ther. 2005;7(Suppl 2):S4-S14.
70. Liska D, Garland G,Tripp M. Proprietary Clinical Research Report. Gig Harbor,WA: Functional Medicine Research Center; 2004.
71. Lukaczer D, Lerman RH, Darland G, et al. Effects of a reduced iso-alpha acids (RIAA), rosemary extract, and oleanolic acid supplement on pain in subjects with osteoarthritis (OA), Proprietary Clinical Research Report. Gig Harbor,WA: Functional Medicine Research Center;2004.
72. Tripp M, Darland G, Lerman RH, et al. Development of Meta050, a natural anti-inflammatory targeting inhibition of cyclooxygenase gene induction instead of direct cyclooxygenase enzyme inhibition, resulting in an anti-inflammatory with low-predicted GI toxicity. Presented at: Fed Am Soc Experimental Biol. 2003: April.
73. Lerman RH, Liska D, Tripp M, et al. Summary of effects of a reduced iso-alpha acids (RIAA), rosemary extract, and oleanolic acid supplement on parameters of cardiovascular health. Proprietary Clinical Research Report. Gig Harbor,WA: Functional Medicine Research Center;2004.
74. Lerman RH, Liska D, Tripp M, et al. Clinical trial evaluating the effect of Meta050 on parameters of platelet function and blood coagulation. Proprietary Clinical Research Report. Gig Harbor,WA: Functional Medicine Research Center;2004.
75. Tripp M, Babish J, Darland G, et al. Hop and modified hop extracts have potent in vitro anti-inflammatory properties. Published Proceedings from 1st International Symposium on Humulus. Editors K.E. Hummer and J.A. Henning. Acta Horiculturae. 668, ISHS 2005.
76. Babish JG, Howell T. Proprietary Research Report. San Clemente, CA: MetaProteomics, Inc. 2003.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 34
77. Lukaczer D, Lerman RH,Tripp M, et al. A randomized cross-over study to assess the effects of a proprietary reduced iso-alpha acid (RIAA), rosemary extract, and oleanolic acid supplement on gastrointestinal integrity using the fecal calprotectin assay. Proprietary Clinical Research Report. Gig Harbor, WA: Functional Medicine Research Center;2004.
78. Yamamoto K, Wang J, Yamamoto S, et al. Suppression of cyclooxygenase-2 gene transcription by humulon of beer hop extract studied with reference to glucocorticoid. FEBS Lett. 2000;465:103-06.
79. Cantorna MT, Zhu Y, Froicu M, et al. Vitamin D status, 1,25-dihydroxyvitamin D3, and the immune system. Am J Clin Nutr. 2004;80(6 Suppl):1717S-1720S.
80. Peterlik M, Cross HS. Vitamin D and calcium deficits predispose for multiple chronic diseases. Eur J Clin Invest. 2005;35(5):290-304.
81. Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135(11):2739S-2748S. 82. Prabhu KS, Zamamiri-Davis F, Steward JB, et al. Selenium deficiency increases the expression of inducible
nitric oxide synthase in RAW 264.7 macophages: role of nuclear factor-кB in up-regulation. Biochem J. 2002;366:203-209.
83. Tarp U. Selenium and the selenium-dependent glutathione peroxidase in rheumatoid arthritis. Dan Med Bull. 1994;41(3):264-274.
84. Zamamiri-Davis F, Lu Y, Thompson JT, et al. Nuclear factor-kappaB mediates over-expression of cyclooxygenase-2 during activation of RAW 264.7 macrophages in selenium deficiency. Free Radic Biol Med. 2002;32(9):890-897.
85. Rosenstein ED, Caldwell JR. Trace elements in the treatment of rheumatic conditions. Rheum Dis Clin North Am. 1999;25(4):929-935.
86. Peretz A, Cantinieaux B, Neve J, et al. Effects of zinc supplementation on the phagocytic functions of polymorphonuclears in patients with inflammatory rheumatic diseases. J Trace Elem Electrolytes Health Dis. 1994;8(3-4):189-194.
87. Bahagavan HN, Chopra RK. CoQ10: absorption, tissue uptake, metabolism and pharmacokinetics. Free Radic Res. 2006;40(5):445-453.
88. Crane FL. Biochemical functions of coenzyme Q10. J Am Coll Nutr. 2001;20(6):591-598. 89. Wolters N, Hahn A. Plasma ubiquinone status and response to six-month supplementation combined with
multivitamins in healthy elderly women—results of a randomized, double-blind, placebo-controlled study. Int J Vitam Nutr Res. 2003;73(3):207-214.
90. Lu WL, Zhang Q, Lee SH, et al. Total coenzyme Q10 concentrations in Asian men following multiple oral 50-mg doses administered as coenzyme Q10 sustained release tablets or regular tablets. Biol Pharm Bull. 2003;26(1):52-55.
91. Singh RB, Niaz MA, Rastogi V, Rastogi SS. Coenzyme Q in cardiovascular disease. J Assoc Physicians India. 1998;46(3):299-306.
92. Weant KA, Smith KM. The role of coenzyme Q20 in heart failure. Ann Pharmacother. 2005;39(9):1522-1526. 93. Mortensen SA. Perspectives on therapy of cardiovascular disease with coenzyme Q10 (ubiquinone). Clin
Investig. 1993;71(8 Suppl):S116-S123. 94. Folkers K, Langsjoen P, Willis R, Richardson P, Xia LJ, Ye CQ, Tamagawa H. Lovastatin decreases
coenzyme Q levels in humans. Proc Natl Acad Sci USA. 1990;87(22):8931-8934. 95. Passi S, Stancato A, Aleo E, Dmitrieva A, Littarru GP. Statins lower plasma and lymphocyte
ubiquinol/ubiquinone without affecting other antioxidants and PUFA. Biofactors. 2003;18(1-4):113-124. 96. Bargossi AM, Battino M, Gaddi A, Fiorella PL, Grossi G, Barozzi G, Di Giulio R, Descovich G, et al.
Exogenous CoQ10 preserves plasma ubiquinone levels in patients treated with 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors. Int J Clin Lab Res. 1994;24(3):171-176.
97. Langsjoen PH, Langsjoen AM. The clinical use of statins and the associated depletion of the essential co-factor coenzyme Q10: a review of the pertinent human and animal data. Biofactors. 2003;18(1-4)101-111.
98. Harris WS, Park Y, Isley WL. Cardiovascular disease and long-chain omega-3 fatty acids. Curr Opin Lipidol. 2003;14(1):9-14.
99. Carroll DN, Roth MT. Evidence of the cardioprotective effects of omega-3 fatty acids. Ann Pharmacother. 2002;36(12):1950-1956.
100. Schrepf, R. Clinical prevention of sudden cardiac death by n-3 polyunsaturated fatty acids and mechanism of prevention of arrhythmias by n-3 fish oils. The Lancet 2004;363:1441-1442.
101. Biscione F, Totteri A, De Vita A, Lo Bianco F, Altamura G. Effect of omega-3 fatty acids on the prevention of atrial arrhythmias. Ital Heart J Suppl. 2005;6(1):53-59.
102. Leaf A, Kang JX, Xiao YF, Billman GE. Clinical prevention of sudden cardiac death by n-3 polyunsaturated fatty acids and mechanism of prevention of arrhythmias by n-3 fish oils. Circulation. 2003;107(21):2646-2652.
103. Mozaffarian D, Psaty BM, Rimm EB, et al. Fish intake and risk of incident atrial fibrillation. Circulation. 2004;110(4):368-373.
104. He K, Rimm EB, Merchant A, et al. Fish consumption and risk of stroke in men. JAMA. 2002;288(24):3130-3136.
105. Siscovick DS, Raghunathan TE, King I, et al. Dietary intake and cell membrane levels of long-chain n-3 polyunsaturated fatty acids and the risk of primary cardiac arrest. JAMA. 1995;274:1363-1367.
106. Khan A, Safdar M, Ali Khan MM, Khattak KN, Anderson RA. Cinnamon improves glucose and blood lipids of people with type 2 diabetes. Diabetes Care. 2003;26(12):3215-3218.
107. Khan A, Bryden NA, Polanshy MM, Anderson RA. Insulin potentiating factor and chromium content of selected foods and spices. Bio Trace Element Res. 1990;24:183-188.
108. Broadhurst CL, Polansky MM, Anderson RA. Insulin-like biological activity of culinary and medicinal plant aqueous extracts in vitro. J Agric Food Chem. 2000;48:849-852.
109. Anderson RA, Polansky M. Tea enhances insulin activity. J Agric Food Chem. 2002;50:7182-7186. 110. Dreosti IE. Bioactive ingredients: antioxidants and polyphenols in tea. Nutr Rev. 1996;54:S51-S58. 111. Saller R, Meier R, Brignoli R. The use of silymarin in the treatment of liver diseases. Drugs.
2001;61(14):2035-2063. 112. Wellington K, Jarvis B. Silymarin: a review of its clinical properties in the management of hepatic disorders.
Bio Drugs. 2001;15(7):465-489. 113. Steel VE, Kelloff GJ, Balentine D, et al. Comparative chemopreventive mechanisms of green tea, black tea,
and selected polyphenol extracts measured by in vitro bioassays. Carcinogenesis. 200;21(1):63-67. 114. Ahmad N, Muktar H. Green tea polyphenols and cancer: biological mechanisms and practical implications.
Nutr Rev. 1999;57(3):78-83.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 35
115. Chen L, Mohr SN, Yang CS. Decrease of plasma and urinary oxidative metabolites of acetaminophen after consumption of watercress by human volunteers. Clin Pharmacol Ther. 1996;60(6):651-660.
116. Rose P, Faulkner K, Williamson G, et al. 7-Methylsulfinylheptyl and 8-methylsulfinyloctyl isothiocyanates from watercress are potent inducers of phase II enzymes. Carcinogenesis. 2000;21(11):1983-1988.
117. Hecht SS. Chemoprevention of cancer by isothiocyanates, modifiers of carcinogen metabolism. J Nutr. 1999;129(3 Suppl):768S-774S.
118. Barch DH, Rundhaugen LM, Pillay NS. Ellagic acid induces transcription to the rat glutathione S-transferase-Ya gene. Carcinogensesis. 1995;16(3):665-668.
119. Ahn D, Putt D, Kresty L, et al. The effects of dietary ellagic acid on rat hepatic and esophageal mucosal cytochromes P450 and phase II enzymes. Carcinogenesis. 1996;17(4):821-828.
120. Ahmed S, Rahman A, Saleem M, et al. Ellagic acid ameliorates nickel induced biochemical alterations: diminution of oxidative stress. Hum Exp Toxicol. 1999;18(11):691-698.
121. Thresiamma KC, George J, Kuttan R. Protective effect of curcumin, ellagic acid and bixin on radiation induced genotoxicity. J Exp Clin Cancer Res. 1998;17(4):431-434.
122. Gebhardt R. Antioxidative and protective properties of extracts from leaves of the artichoke (Cynara scolymus L.) against hydroperoxide-induced oxidative stress in cultured rat hepatocytes. Toxicol Appl Pharmacol. 1997;144(2):279-286.
123. Adzet T, Camarasa J, Laguna JC. Hepatoprotective activity of polyphenolic compounds from Cynara scolymus against CCI4 toxicity in isolated rat hepatocytes. J Nat Prod. 1987;5(4):612-617.
124. Perez-Garcia F, Adzet T, Canigueral S. Activity of artichoke leaf extract on reactive oxygen species in human leukocytes. Free Radic Res. 2000;333(5):661-665.
125. Isolauri E, Kirjavainen PV, Salminen S. Probiotics: a role in the treatment of intestinal infection and inflammation? Gut. 2002:50(3 Suppl):11154-11159.
126. Gill HS, Rutherford KJ, Cross ML, et al. Enhancement of immunity in the elderly by dietary supplementation with the probiotic Bifidobacterium lactis HN019. Am J Clin Nutr. 2001;74(6):833-839.
127. Wagner RD, Pierson C,Warner T, et al. Biotherapeutic effects of probiotic bacteria on candidiasis in immunodeficient mice. Infect Immun. 1997;65(10):4165-4172.
128. Klaenhammer TR, Kullen MJ. Selection and design of probiotics. Int J Food Microbiol. 1999;50(1-2):45-57. 129. Tejada-Simon MV, Lee JH, Ustunol Z, et al. Ingestion of yogurt containing Lactobacillus acidophilus and
Bifidobacterium to potentiate immunoglobulin A responses to cholera toxin in mice. J Dairy Sci. 1999;82(4):649-660.
130. Mutai M, Tanaka R. Ecology of Bifidobacterium in the human intestinal flora. Bifidobacteria Microflora. 1987;6(2):33-41.
131. Kaplan H, Hutkins RW. Fermentation of fructooligosaccharides by lactic acid bacteria and bifidobacteria. Appl Environ Microbiol. 2000;66(6):2682-2684.
132. Mitsuoka T. Intestinal flora and aging. Nutr Rev. 1992;50:438-444. 133. De Los Reyes GC, Koda RT, Lien EJ. Glucosamine and chondroitin sulfates in the treatment of
osteoarthritis: a survey. Prog Drug Res. 2000;55:81-103. 134. Giordano N, Nardi P, Senesi M, et al. The efficacy and safety of glucosamine sulfate in the treatment of
gonarthritis. Clin Ter. 1996;147:99-105. 135. Leffler CT, Philippi AF, Leffler SG, et al. Glucosamine, chondroitin, and manganese ascorbate for
degenerative joint disease of the knee or low back: a randomized, double- blind, placebo-controlled pilot study. Mil Med. 1999;164(2):85-91.
136. Morreale P, Manopoulo R, Galati M, et al. Comparison of the anti-inflammatory efficacy of chondroitin sulfate and diclofenac sodium in patients with knee osteoarthritis. J Rheumatol. 1996;23:1385-1391.
137. Uebelhart D,Thonar EJ, Delmas PD. Effects of oral chondroitin sulfate on the progression of knee osteoarthritis: a pilot study. Osteoarthritis Cartilage. 1998;6(Suppl A):31-36.
138. McAlindon TE, LaValley MP, Gulin JP, et al. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA. 2000;283(11):1469-1475.
139. Usha PR, Naidu MU. Randomised, double-blind parallel, placebo-controlled study of oral glucosamine, methylsulfonylmethane and their combination in osteoarthritis. Clin Drug Investig. 2004;24(6):353-363.
140. Kim LS, Axelrod LJ, Howard P, Buratovich N, Waters RF. Efficacy of methylsulfonylmethane (MSM) in osteoarthritis pain of the knee: a pilot clinical trial. Osteoarthritis Cartilage. 2006;14(3):286-294.
141. Gruber CJ, Tschugguel W, Schneeberger C, Huber JC. Production and action of estrogens. N Engl J M. 2002;346(5):340-351.
142. Setchell KDR. Soy isoflavones—benefits and risks from nature’s selective estrogen receptor modulators (SERMs). J Am Coll Nutr. 2001;20(5):354S-362S.
143. Nestel PJ, Pomeroy S, Kay S, et al. Isoflavones from red clover improve systemic arterial compliance but not plasma lipids in menopausal women. J Clin Endocrinol Metab. 1999;84(3):895-898.
144. Kuiper GG, Lemmen JG, Carlsson BO, et al. Interaction of estrogenic chemicals and phytoestrogens with estrogen receptor b. Endocrinology. 1998;139:4252-4563.
145. Kaufman PB, Duke JA, Brielmann H, et al. A comparative survey of leguminous plants as sources of the isoflavones genistein and daidzein: implications for human nutrition and health. J Altern Complement Med. 1997;3(1):7-12.
146. Davis SR, Dalais FS, Simpson ER, et al. Phytoestrogens in health and disease. Recent Prog Horm Res. 1999;54:185-210.
147. Goud VK, Polasa K, Krishnaswamy K. Effect of turmeric on xenobiotic metabolising enzymes. Plant Foods Hum Nutr. 1993;44(1):87-92.
148. Verma SP, Goldin BR, Lin PS. The inhibition of the estrogenic effects of pesticides and environmental chemicals by curcumin and isoflavonoids. Environ Health Perspect. 1998;106(12):807-812.
149. Bowers JL,Tyulmenkov V, Jernigan SC, et al. Resveratrol acts as a mixed agonist/antagonist for estrogen receptors α and β. Endocrinology. 2000;141(10):3657-3667.
150. Bell MC, Crowley-Nowick P, Bradlow HL, et al. Placebo-controlled trial of indole-3-carbinol in the treatment of CIN. Gynecol Oncol. 2000;78:123–129.
151. Michnovicz JJ. Increased estrogen 2-hydroxylation in obese women using oral indole-3-carbinol. Int J Obes Relat Metab Disord. 1998;22(3):227-229.
152. Michnovicz JJ, Bradlow HL. Altered estrogen metabolism and excretion in humans following consumption of indole-3-carbinol. Nutr Cancer. 1991;16:59-66.
153. McAlindon TE, Gulin J, Chen T, Klug T, Lahita R, Nuite M. Indole-3-carbinol in women with SLE: effect on estrogen metabolism and disease activity. Lupus. 2001;10(11):779-783.
___________________________________________________
Version 1.4 © 2007 Metagenics, Inc. Page 36
154. Taioli E, Bradlow HL, Garbers SV, et al. Role of estradiol metabolism and CYP1A1 polymorphisms in breast cancer risk. Cancer Detect Prev. 1999;23(3):232-237.
155. Rosen CA, Woodson GE, Thompson JW, Hengesteg AP, Bradlow HL. Preliminary results of the use of indole-3-carbinol for recurrent respiratory papillomatosis. Otolaryngol Head Neck Surg. 1998;118(6):810-815.
156. Bradlow HL, Michnovicz JJ, Halper M, Miller DG, Wong GY, Osborne MP. Long-term responses of women to indole-3-carbinol or a high fiber diet. Cancer Epidemiol Biomarkers Prev. 1994;3(7):591-595.
157. Michnovicz JJ, Adlercreutz H, Bradlow HL. Changes in levels of urinary estrogen metabolites after oral indole-3-carbinol treatment in humans. J Natl Cancer Inst. 1997;89:718-723.
MET1547 12/07