Stem Cells TE
-
Upload
rajasekaranm -
Category
Documents
-
view
219 -
download
0
Transcript of Stem Cells TE
-
7/30/2019 Stem Cells TE
1/411 8 NATURE | VOL 414 | 1 NOVEMBER 2001 | www.nature.com
T
issue engineering in a classical sense implies theuse of organ-specific cells for seeding a scaffoldex vivo. The cell-based (but not necessarily stem
cell-based) nature of tissue engineering servedto d efine it, an d to distinguish it from guided
tissue regeneration in which a scaffold is designed toencou rage regenerat ion solely by cells residing at the site
of its transplantation. Irrespective of actual clinicalfeasibility, the experimental design and potential use of
tissue en gineering app roaches are endless, and range fromthe p reclinical gener ation of cardiac valve sub stitutes, to exvivo construction of nasal cartilages, to organ substitutes
such as the u rinary bladder (reviewed in r ef. 1).The list of tissues with the potential to be engineered is
growing steadily. This is du e in large part to recent p rogressin stem cell biology and recognition of the u nique biological
properties of stem cells, although not all stem cell-based
therapies (for example, some th at use n eural stem cells, assummarized by Temple, pages 112117) involve the con-
struction of tissue either ex vivo or in vivo. Non etheless, pilotstud ies in a variety of system s highlight great pr ospects for
future stem cell-based tissue engineering (Table 1). But
translation in to clinical reality has been reached so far in onlya few areas, and notably only in tho se areas in which there has
been lon g-stand ing insight into stem cell biology.Tissues that can now be engineered using stem cells
comprise a diverse range from epithelial surfaces (skin,cornea an d m ucosal mem bran es) to skeletal tissues. These
systems are inh erently different in their r ate of self-renewal
and physical structure, two impo rtant determinants of anyattem pt to reconstru ct tissues using stem cells (as discussed
by Spradling and colleagues on pages 98104). Apprecia-tion o f the inherent diversities of organ systems and cognate
stem cells is essential for developm ent o f adeq uat e str ategies
of inter vention in specific areas.Here we exam ine two ap plications o f stem cells to tissue
engineering. The first case is the regeneration of skin, whichinvolves the structural formation of two-dimensional
sheets. The second, m ore com plex examp le is the form ationof bone, which involves the reconstruction of three-
dim ensional shapes and inter nal architectures.
Engineering skin and other surfacesPermanent restoration of tissues characterized by highand co nt inu ou s self-renewal specifically requ ires extensive-
ly self-renewing stem cells. Haematopoiesis provides the
best paradigm of a stem cell-dependent, steadily self-
renewing system (see review by Weissman and colleagues,pages 105111). Among the hierarchy of haematopoietic
progenitors en dowed with varying capacities to self-renew,
it is only the small comp artm ent of long-term self-renewingstem cells that is necessary for permanent and complete
restoration of haematopoiesis after lethal irradiation 2.Likewise, progenitor cells represented in a keratinocyte
culture are also ran ked in a hierarchy, and u nd er clonogenicconditions form different types of colonies (holoclones,
m eroclones and p araclones) that vary significantly in theirability to self-renew and to generate a differentiated
epiderm is. On ly holoclones are the produ ct of a true stem
cell, as defined by their exceptional self-replication ability(>140 doublings), which is not ascribed to either
m eroclones (a popu lation of tran sient am plifying cells) orparaclones (a population of senescent or differentiating
progenitors) 3. In principle, a small but pure population of
holoclone-generating cells would b e all that is requ ired forgenerating epiderm al grafts. The recent iden tification of a
keratinocyte stem cell marker may provide a new tool forthis approach with respect to epidermis4.
These theoretical prediction s correlate with the clinical
outcom es of skin grafting. Skin auto grafts are produ ced bycultur ing keratinocytes to generate an epiderm al sheet, and
then transplanting this sheet along with a suitabledermis-like substrate (Fig. 1a) 5. But the success of these
procedu res has been variable, with graft failure resulting inmany cases after a promising initial engraftment.
Experimental conditions can cause depletion of the holo-
clone-generating compartment in cell cultures, similar tothe par tial depletion of the epidermal stem cell com part-
men t that can occur in vivo (for example, during ageing).Retention or depletion o f true stem cells in a keratin ocyte
population in vitro is significantly affected b y the n atur e of
the carrier or substrate used for culturing and grafting, andcould account for instances of graft failure in clinical
practice6. The long-term success of a skin graft thusdepends on appropr iate replenishm ent of stem cells in th e
graft. The specific techno logical challenge in r estoration of
epithelial surfaces in turn consists of the definition ofculture conditions, and of carriers that are designed
specifically to m aintain an ad equate stem cell com par tm entin the en gineered graft. Depend ence of epithelial surfaces
on relevant stem cell compartments is further highlightedby the successful recon struction of dam aged corneas using
stem cells derived from the limbus in conjunction with
an amniotic mem brane7,8.
Stem cells in tissue engineeringPaolo Bianco* & Pamela Gehron Robey
*D ipa rt im ento d i M edicin a Sp erim enta le e Patologia, Uni versi ta La S apien za, V iale Regin a Elen a 324, Rom a 00161 , Ita ly
(e-m ail: [email protected])
Craniofacial and Skeletal Diseases Branch, N ational Institu te of Den tal and Cran iofacial Research, N ationa l Institutes of Health, 30 Conv ent
Driv e M SC 4 320 , Bet hesd a, M ary lan d, U SA (e-m ail: probey @dir.n idcr.n ih .gov)
The concept of producing spare parts of the body for replacement of damaged or lost organs lies at thecore of the varied biotechnological practices referred to generally as tissue engineering. Use of postnatalstem cells has the potential to significantly alter the perspective of tissue engineering. Successful long-termrestoration of continuously self-renewing tissues such as skin, for example, depends on the use ofextensively self-renewing stem cells. The identification and isolation of stem cells from a number of tissuesprovides appropriate targets for prospective gene therapies.
insight progress
2001 Macmillan Magazines Ltd
-
7/30/2019 Stem Cells TE
2/4
Engineering the corr ect shape and physical structure o f a graft isrelatively simple in epiderm is and other surface epithelial tissues, and
indeed can be achieved ex vivo. This reflects the essentially two-
dim ensional organization of skin an d oth er epiderm al surfaces, andis in shar p con tra st with system s such as the skeleton, where effective
engineering involves the reconstruction of complex shapes andarchitectures. These directly affect proper function, are normally
generated over a long per iod of time, and can not be achieved ex vivo.
Engineering the skeletonSkeletal stem cells (SSCs; also kn own as bon e-m arrow strom al stemcells, or mesenchymal stem cells) are found in the subset of
clonogenic adherent m arrow-d erived cells, and are able to un dergoextensive replication in culture. Upon ectopic in vivo transplantation
in m odel systems, all of the main tissues foun d in bo ne as an or gan
(bone, cartilage, adipocytes and haematopoiesis-supportingstroma) are formed (Figs 1b and 2a,f) (ref. 9, and reviewed in refs
10,11). SSCs obtained in cu lture mu st be com bined with app ropr iatecarriers before transplantation. These provide a three-dimensional
scaffold in which a vascular bed can be established, and tran splanted
progenitor cells can differentiate and form a bone/marrow organ.Many suitable mater ials are being generated and perfected, including
synthetic hydroxyapatite/tricalcium phosphates (Figs 1b and 2a),
and polyglycolic and polylactic acids12,13
. Most are effective insupporting bone regeneration, either alone or in conjunction with
growth factors such as bone morphogenetic proteins. However, sofar, little attention has been devoted to their compatibility with
long-term maintenance of stem cell properties, or to the ultimatefate of the bonebiomaterial composite being generated at the site
of t ransplantation.In th e sim plest procedure for bon e reconstruction , SSCs isolated
in culture from a limited volume of bone marrow are expanded ex
vivo, loaded onto an appropriate carrier, and locally transplanted(Fig. 1b). This pro cedu re results in th e effective repa ir of critical size
defects, which are larger than what can be repaired by resident cells,either spontaneously or as guided by an osteoconductive device
(Figs 1b an d 2b,c)1417. Convincing pr eclinical stud ies adopting th is
appro ach have led to preliminar y observational stud ies in hu m ans18
,and clinical trials are about to start in a number of centres. An
alternative approach h as led to the generation of fully vascularizedbone flaps of the desired shape in vivo, prior to their use for local
tran splantation ( Fig. 2d, e). In th ese experimen ts, SSCs loaded into
appropriate carriers and transplanted into a non-skeletal sitesurrounding an artery and vein; here they generate a vascularized
segment of bone, the size and shape of which are dictated by thecarrier geometr y19.
All of these applications can be categorized as surgical interven-tion thro ugh t ransplant ation of a biological prosthetic device
for th e cure of ph ysical defects in an o therwise nor m al skeleton. But
the existence of SSCs raises additional hopes and challenges fortreatment of more complex and generalized diseases, such as
crippling genetic diseases. Here, the concept of using SSCs toreplace misfunctioning bone cells with normal ones meets
another set of important obstacles, which further illustrate the
diversity of the skeleton an d its stem cells com pared with oth er stemcell-based systems. One is the route of systemic delivery of the
nu m ber of progenitors n eeded to pro du ce a biological effect. Som e
insight progress
NATURE | VOL 414 | 1 NOVEMBER 2001 | www.nature.com 11 9
(Seed with
dermal
fibroblasts)
Single-cell
suspension
(p63 selection?)
a Epidermis
b
Scaffold
Dermal substituteEx vivoexpansion conditions
to maintain 'holoclones'
(stem-cell population)
Full-thickness skin wounds
Potential
for genetic
engineering
Ex vivoexpansion
Attachment to hydroxyapatite/tricalcium phosphate particles
In vivotransplantation
into segmental defect
Skeletal
stem cell
Epidermal
stem cell
Bone
marrow
Bone matrix
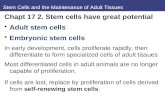
Figure 1 Regeneration of two-dimensional (skin) and three-dimensional (bone)
tissues using stem cells. a , Skin autografts are produced by culturing k eratinocytes
(which may be sorted for p63, the recently described, epidermal stem cell marker)under appropriate conditions not on ly to generate an epidermal sheet, but also to
maintain the stem cell population (holoclones). The epidermal sheet is then placed on
top of a dermal substitute comprising devitalized dermis or bioengineered dermal
substitutes seeded with dermal fibroblasts. Such two-dimensional composites,
generated ex vivo, completely regenerate full-thickness wounds. b, Bone
regeneration requires ex vivoexpansion of marrow-derived skeletal stem cells and
their attachment to three-dimensional scaffolds, such as particles of a
hydroxyapatite/tricalcium phosphate ceramic. This composite can be transplanted
into segmental defects and will subsequently regenerate an appropriate
three-dimensional structure in vivo.
Table 1 Current approaches to tissue engineering
Stem cell-based tissue engineering Non stem cell-based tissue engineering1
Blood vessels23,29 Liver31 Bladder MeniscusBone1417* Pancreas 41 Cartilage (ear, nose Oral mucosaCartilage39 Nervous tissue42* and joints)* Salivary glandCornea7,8* Skeletal muscle24,27 Heart valves TracheaDentin40 Skin5,6* Intestine UreterHeart muscle28,29 Kidney Urethra
*In clinical trials or clinical observational studies.
2001 Macmillan Magazines Ltd
-
7/30/2019 Stem Cells TE
3/4
experimental evidence is available for limited engraftment of
osteogenic progenitors that are infused (as is don e with haem atopoi-
etic stem cells or HSCs) through the systemic circulation 20. Butevidence for a biologically significant effect of the system ic infusion
of SSCs is not available, and cu re of systemic skeletal diseases usingapproaches borrowed simplistically from haematology is not in
sight. D efinitive preclinical work in anim al mo dels, com pliant with
strict criteria for assessment of engraftment, must be conductedbefore these types of procedures reach clinical trials11, although
preliminar y clinical stud ies are under way21.Another p ertinen t point is that renewal in a po stnatal skeleton is
markedly slower than in skin or blood (the whole skeleton being
comp letely replaced only about three tim es in a lifetime, whereas theskin is replaced once a month). Consequently, we would expect
replacem ent o f skeletal tissue with in fused SSCs to occur o ver longertimescales compared to rapidly self-renewing tissues, even if issues
related to efficient cell delivery and systemic engraftment wereresolved. Altern ative mean s for local int ervent ion in genet ic diseases
are conceivable. For examp le, engineered SSCs could b e tran splanted
locally at the site of a clinical event ( such as a fractur e or deform ity) in
genetic diseases of osteogenic cells, such as osteogenesis imp erfecta
(caused by mu tations in genes encoding collagen type I) o r fibrous
dysplasia of bone (caused by activating missense m utation s of theGNAS1 gene). But ho pes for a system ic cure of genetic disorders of
the skeleton will rely on m ore im aginative avenues. In som e casesthese might include in u tero tran splantation, whose feasibility with
SSCs has been shown in preliminar y stud ies22. As with the p reviou sly
described techniques, caveats related to efficiency of engraftmentand biological effects remain to b e addr essed.
Heterotopic stem cells for tissue engineeringThe m arrow is at centre stage for future techno logical developmen ts
in tissue engineering, not o nly as the only organ in which at least twotypes of stem cells (HSCs and SSCs) reside, but also as the organ in
which progenitors for a number of distant tissues can be found.Recent studies indicate that the traditional wall separating the
haem atopoietic and m esoderm al tissue systems and lineages is beingdemolished. Cells capable of regenerating blood vessels, skeletal
mu scle and cardiac mu scle are found in the m arrow2325. The unex-
pected potential for myogenesis and cardiomyogenesis has been
12 0 NATURE | VOL 414 | 1 NOVEMBER 2001 | www.nature.com
insight progress
Figure2 Bone regeneration by
marrow-derived skeletal stem
cells (SSCs). a, SSCs
transplanted in conjunction with
appropriate vehicles (v) such as
hydroxyapatite/tricalcium
phosphate generate an network
of bone (b) and stroma composed
of adipocytes and reticular cellsthat support haem atopoiesis (hp).
b, Critical size defects that do not
heal spontaneously, such as
those as in the calvaria, can be
completely regenerated by
SSCvehicle constructs (c); ft,
fibrous tissue. d,e, In addition, by
wrapping SSCvehicle constructs
around an artery and vein (bv) in
conjunction with Gore-Tex (g) to
prevent collateral vascularization
(dotted box in d), fully
vascularized bone flaps of desired
shape can be constructed.f, Under appropriate conditions,
SSCs can also form c artilage (c)
as demonstrated by alcian blue
staining and type II collagen
immunohistochemistry (not
shown).
2001 Macmillan Magazines Ltd
-
7/30/2019 Stem Cells TE
4/4
ascribed to both H SCs and strom al (mesenchymal) stem cells in th emarrow2629. SSCs can p erhaps give rise to n euron s or glia30, pu rified
m ouse H SCs can regenerate liver cells31, and cells able to r egenerate
bon e are also foun d in blood 32. Perhaps what we have referred to asthe H SC is in itself much m ore a tr ue m ultipotent stem cell with
transgermal potentials2,31, nor m ally devoted to haem atopoiesis as aresult o f local cues.
Marrow cells offer the advantage of being easily harvested and
cultured from an adult organism , and th e HSC can be isolated and
purified ex vivo. Althou gh m ost of these applications are a long wayfrom any immediate clinical use, these studies raise basic scientificissues that are far from being settled or rationalized, similar, for
example, to the issue of plasticity of postnatal stem cells 10,11. Theyprovide insight on how different the scene of tissue engineering could
be in the relatively near futur e. Beyond theoretical considerations,
and p endin g fur ther experim ental proof where needed, the existenceof heterotopic and pleiotropic stem cells in the bone marrow has
obvious practical implications for th e future of stem cell therap y thatshould no t be missed.
Reconstruction versus correctionDelivery of factors that wou ld stimu late stem cells in situ to initiate a
process leading to regeneration rath er than scar form ation has long
been pursued. But success has been limited owing to problems ofdosage, lack of full activity of recombinant factors, and inability to
sustain a factors presence for an ap pro pr iate length of time. To over-com e these pro blems, gene-activated m atrices are being investigated
that com pr ise plasmid s cod ing for factors in a variety of delivery vehi-cles. These would t ran sduce cells in vivo to bring about appropriate
regeneration, and trials aimed at osteoporotic fractures are beingplanned33. In th ese attem pts, the trad itional principles governing th e
use of carriers merge imaginatively with the frontier of genetic
engineering. No dou bt, if reconstru ction was the initial front ier oftissue engineering, genetic correction is the next. As stem cells are
the critical ingredient in tissue regenerat ion, they are also the criticaltargets of any strategy aimed at correctin g a genetic defect.
Advances in our ability to genetically manipulate cells ex vivo
using viral and no n-viral tran sducing agents has circum vented m anyof the potential hazards of direct gene transfer in hum ans34. Success-
ful stable tran sduction o f holoclone-generating epiderm al cells withretroviral vectors h as paved t he way to th e first trial of gene therapy
for a devastating skin disease, junction al epiderm olysis bullosa, a
recessive disease caused by a misfunctioning laminin molecule35.However, in dominant-negative diseases, a mutant gene must be
silenced, and the techniques for doing this are in their infancy.Homologous recombination and site-directed mutagenesis of stem
cells ex vivo would be the ultimate goal36,37, but antisense RNA, RNAinterference and ham m erhead and h airpin RNAses offer interm edi-
ate strategies to at least prevent expression of a m utan t pro tein38.
With th e prospect of stem cell-mediated gene ther apy, the very def-inition of tissue engineering evolves into engineering of tissue func-
tion . Today, stem cell-based app roach es to tissue reconstru ction op enunpredicted applicative (and market) opportunities. Although this
discussion has been lim ited to systems where extensive preclinical and
clinical studies have already been conducted, more exciting avenuesare in sight in m any areas. But en thusiasm over what un questionably
represents a markedly innovative technique with huge therapeuticpotential m ust be balanced against stringent standards of scientific
and clinical investigation. In addition, we m ust rem ain aware of the
wide range of basic and applied issues associated with each system,with the targeted prob lem s, and with the p redicted solutions. s
1. Stock, U. A. & Vacanti, J. P. Tissue engineering: current state and prospects.An nu . Rev. M ed. 52 ,
443451 (2001).
2. Lagasse, E., Shizuru, J. A., Uchida, N., Tsukamoto, A. & Weissman, I. L. Toward regenerative
medicine.Im m un ity 14 , 425436 (2001).
3. Barrandon, Y. & Green, H. Three clonal types of keratinocyte with different capacities for
multiplication. Proc. Natl Acad. Sci. USA 84 , 23022306 (1987).
4. Pellegrini, G. et al. p63 identifies keratinocyte stem cells. Proc. Nat l Acad. Sci. USA 98 , 31563161 (2001).
5. Ruszczak, Z. & Schwartz, R. A. Modern aspects of wound h ealing: an update.De rm atol. Su rg. 26 ,
219229 (2000).
6. Pellegrini, G. et al. The control of epidermal stem cells (holoclones) in the treatment of massive full-
thickness burns with autologous keratinocytes cultured on fibrin. Transplantation 68 , 868879
(1999).
7. Pellegrini, G. et al. Long-term restoration of dam aged corneal surfaces with autologous cultivated
corneal epithelium.Lan cet349, 990993 (1997).
8. Tsai, R. J., Li, L. M. & Chen, J. K. Reconstruction of dam aged corneas by transplantation of
autologous limbal epithelial cells.N . Engl. J. Med . 343, 8693 (2000).
9. Friedenstein, A. J., Piatetzky, S. II & Petrakova, K. V. Osteogenesis in transplants of b one m arrow cells.
J. Emb ryol. Ex p. M orph ol. 16 , 381390 (1966).
10.Bianco, P. & Gehron Rob ey, P. Marro w strom al stem cells.J. Clin. I nv est. 105, 16631668 (2000).
11.Bianco, P., Riminucci, M., Gronthos, S. & Robey, P. G. Bone marrow stromal stem cells: nature,
biology, and potential applications. Stem Cells 19 , 180192 (2001).
12.Lan gstaff, S. et al. Resorbable bioceramics based on stabilized calcium phosphates. Part I: r ational
design, sample preparation and m aterial characterization.Biom ater ials 20 , 17271741. (1999).
13.Hutm acher, D. W. Scaffolds in tissue engineering bone an d cartilage.Biom ater ials 21 , 25292543
(2000).
14.Bru der, S. P., Kraus, K. H., Gold berg, V. M. & Kadiyala, S. The effect of implants load ed with
autologous mesenchymal stem cells on the h ealing of canine segmental bo ne defects.J. Bone Joint
Surg. Am. 80 , 985996 (1998).
15.Krebsbach, P. H., Mankani, M. H., Satomura, K., Kuznetsov, S. A. & Robey, P. G. Repair of craniotomy
defects using bone m arrow stromal cells. Transplantation 66 , 12721278 (1998).
16.Petite, H. et al. Tissue-engineered bone regeneration.N atu re Biot echn ol. 18 , 959963 (2000).
17.Kon, E. et al. Autologous bone marrow strom al cells loaded on to porous hydroxyapatite ceramic
accelerate bone repair in critical-size defects of sheep long bones.J. Biom ed. M ate r. Res. 49 ,
328337 (2000).
18.Quarto, R. et al. Repair of large bone defects with the use of autologous bone marrow strom al cells.N .
Engl. J. Med. 344, 385386 (2001).
19.Mankani, M. H. et al. Pedicled bone flap formation u sing transplanted bone m arrow stromal cells.
Arch . Sur g. 136, 263270 (2001).
20.Hou, Z. et al. Osteoblast-specific gene expression after transplantation of m arrow cells: implications
for skeletal gene therapy. Proc. Natl Acad. Sci. USA 96 , 72947299 (1999).
21.Horwitz, E. M. et al. Transplantability and therap eutic effects of bone m arrow-derived mesenchymal
cells in children with osteogenesis imperfecta.N atu re Me d. 5, 309313 (1999).
22.Liechty, K. W. et al. Hum an m esenchymal stem cells engraft and demon strate site-specific
differentiation after in utero transplantation in sheep.N atu re Me d. 6, 12821286 (2000).
23.Kocher, A. A. et al. Neovascularization of ischemic myocardium by human bone-m arrow-derived
angioblasts prevents cardiomyocyte apoptosis, reduces remodeling and improves cardiac function.
N atu re M ed. 7, 430436 (2001).
24.Ferrari, G. et al. Muscle regeneration by bone m arrow-derived myogenic progenitors.Science 279,
15281530 (1998).
25.Orlic, D. et al. Bone marrow cells regenerate infarcted m yocardium.N atu re 410, 701705 (2001).
26.Wakitani, S., Saito, T. & Caplan, A. I. Myogenic cells derived from rat bone marrow mesenchymal
stem cells exposed to 5-azacytidine.Mu scle Ner ve 18 , 14171426 (1995).
27.Gussoni, E. et al. Dystrophin expression in the m dx mou se restored by stem cell transplantation.
N atu re 401, 390394 (1999).
28.Makino, S. et al. Cardiomyocytes can be generated from m arrow stromal cells in vitro.J. Clin . Inv est.
103, 697705 (1999).
29.Jackson , K. A.et al. Regeneration of ischemic cardiac mu scle and vascular endothelium by adu lt stem
cells.J. Clin. I nve st. 107, 13951402 (2001).
30.Azizi, S. A., Stokes, D., Augelli, B. J., DiGirolamo, C. & Prockop , D. J. Engraftm ent an d m igration o f
hum an bon e marrow strom al cells implanted in the brains of albino ratssimilarities to astrocyte
grafts. Proc. Natl A cad. Sci. USA 95 , 39083913 (1998).
31.Lagasse, E. et al. Purified hematopo ietic stem cells can differentiate into hepatocytes in vivo.N atu re
M ed. 6, 12291234 (2000).
32.Kuzn etsov, S. A. et al. Circulatin g skeletal stem cells.J. Cell Biol. 153, 11331140 (2001).
33.Bonadio, J. Tissue engineering via local gene delivery: update and future prospects for en hancing the
technology.Ad v. Dr ug De liv. Rev. 44 , 185194 (2000).
34.Asahara, T., Kalka, C. & Isner, J. M. Stem cell therapy and gene transfer for regeneration. Gene Ther. 7,
451457 (2000).
35.Dellambra, E. et al. Toward epiderm al stem cell-mediated ex vivo gene therapy of Junctional
Epidermolysis Bullosa.Hu m . Gen e Th er. 11 , 22832287 (2000).
36.Lanzov, V. A. Gene targeting for gene therapy: prospects. M ol. Gen et. M etab. 68 , 276282 (1999).
37.Li, J. & Baker, M. D. Mechanisms involved in targeted gene replacement in mammalian cells. Genetics
156, 809821 (2000).
38.Jen, K. Y. & Gewirtz, A. M. Suppr ession of gene expression by targeted disru ption o f messenger RNA:
available options and current strategies. Stem Cells 18 , 307319 (2000).
39.John stone, B. & Yoo, J. U. Autologous me senchym al progenitor cells in articular ca rtilage repair. Clin.
Orthop. S156S162 (1999).
40.Gronthos, S., Mankani, M., Brahim, J., Robey, P. G. & Shi, S. Postnatal hum an d ental pulp stem cells
(DPSCs) in vitro and in vivo. Proc. Natl A cad. Sci. USA 97 , 1362513630 (2000).
41.Ram iya, V. K. et al. Reversal of insulin-dependent diabetes using islets generated in vitro from
pancreatic stem cells.N atu re M ed. 6, 278282 (2000).
42.Bjorklund, A. Cell replacement strategies for neurodegenerative disorders.N ovar tis Foun d. Sy m p.
231, 715 (2000).
AcknowledgementsThe supp ort of Telethon Fond azione Onlu s Grant ( to P.B.) is gratefully acknowledged.
insight progress
NATURE | VOL 414 | 1 NOVEMBER 2001 | www.nature.com 12 12001 Macmillan Magazines Ltd







![STEM CELLS EMBRYONIC STEM CELLS/INDUCED PLURIPOTENT STEM CELLS Stem Cells.pdf · germ cell production [2]. Human embryonic stem cells (hESCs) offer the means to further understand](https://static.fdocuments.net/doc/165x107/6014b11f8ab8967916363675/stem-cells-embryonic-stem-cellsinduced-pluripotent-stem-cells-stem-cellspdf.jpg)










