Sinus Histiocytosis Massive Lymphadenopathy · PDF fileSinus Histiocytosis Massive...
Transcript of Sinus Histiocytosis Massive Lymphadenopathy · PDF fileSinus Histiocytosis Massive...

ANNALS OF CLINICAL AND LABORATORY SCIENCE, Vol. 17, No. 3Copyright © 1987, Institute for Clinical Science, Inc.
Sinus Histiocytosis M assive Lym phadenopathy Syndrome:
H istogenesis o f the Hepatic Lesion*
R. E. BROW N, M .D. and CYRIL A. D ’CRUZ, M .D.
Department o f Pathology, Cook-Fort Worth Childrens Medical Center,
Fort Worth, TX 76104
ABSTRACT
Sinus histiocytosis massive lym phadenopathy (SHML) syndrome with hepa tic involvem ent, occurring in a seven-year-old black fem ale, is reported . Morphologic characterization of the hepatic lesion is accomplished utilizing conventional light, fluorescent and electron microscopy, and histochemical techniques and by comparing and contrasting the findings with those in cases of familial erythrophagocytic lymphohistiocytosis (FEL) and virus-associated hemophagocytic syndrome (VAHS). The histiocytic proliferation in the liver in SHM L differs by showing: (a) an in tralobular distribution with portal sparing; (b) m arked steatosis; and (c) lipofuscinosis. The aforesaid intralobular distribution and the accompanying hypertrophy and hyperplasia of Kupffer cells, as well as commonalities of steatosis and lipofuscinosis, and, to a lesser extent, erythrophagocytosis and siderosis, suggest a histogenesis from Kupffer cells. The histochemical finding of fatty acid peroxides and both fluorescent microscopic and histochemical evidence of lipofuscin inclusions, a by-product of lipid peroxidation, in Kupffer cells provide at least a theoretical basis for both erythrophagocytosis and proliferation eventuating in intralobular histiocytosis.
In troduction
S in u s h is t io c y to s is w ith m ass iv e ly m p h a d e n o p a th y (SH M L) was firs t described as a benign clinicopathological entity by Rosai and Dorfman in 1969.18 The majority of cases (some 80 percent)
* Send reprint requests and correspondence to: R. E. Brown, M .D ., D epartm ent o f Pathology, Cook-Fort Worth Children’s Medical Center, 1400 Cooper, Fort Worth, TX 76104.
occur within the first two decades of life a n d a re c h a ra c te r iz e d c lin ic a lly by lym phadenopathy, fever, leukocytosis, hypergam maglobulinemia, and an accele r a t e d e r y th r o c y te s e d im e n ta t io n ra te .18,19,20 Extranodal involvem ent has b een rep o rted in up to 28 p e rc e n t of cases.9,10 Although the liver is a reported site of such involvem ent, inform ation concerning the m orphologic characterization and histogenesis of the hepatic les io n is S parse .6,8 In a tte m p tin g to
1620091-7370/87/0500-0162 $01.50 © Institute for Clinical Science, Inc.

SHM L SYNDROME: TH E HEPATIC LESION 1 6 3
expand the latter, the light, fluorescent and electron microscopic and histochem- ical features of the histiocytic proliferations in the liver of a patient with SHM L syndrom e are reported; the findings are contrasted with those in cases of familial erythrophagocytic lym phohistiocytosis (FEL)1 and virus-associated hemophago- cytic syndrom e (VAHS)3,15; and a histogenesis from Kupffer cells is proposed.
Case Report
A seven-year-old black female presented with a three w eek history of recurrent fevers, wheezing, episodes of vomiting and diarrhea, headaches and co n g estio n , and, finally , righ t up per quadrant (abdominal) pain. Her past medical history included treatment for reactive airway disease. Out-patient laboratory find in gs ob ta in ed tw o w eek s prior, revealed both a normal white blood cell count and hemoglobin concentration and 2 + ketonuria. Therap eu tic agents ad m in istered during th is period included Accurbron® (a theophylline preparation) and Alupent® (a beta-adrenergic stimulator).
Physical examination at the time of admission to C o ok -F ort W orth C h ild re n ’s M ed ica l C en ter revealed a somewhat dehydrated child with a tem perature o f 38.0°C . P ertinent negative findings included absence of lymphadenopathy and organomegaly. Laboratory data revealed: anemia (hemoglobin 7.6 g per dl with expected range for age 11.4 to15.4 g per dl),4 thrombocytopenia (125 x 103 per mm3 with expected range for age 250 to 470 X 103 per mm3); hyperaspartate aminotransferasemia (142 U per L with expected range for age 20 to 45 U per L) and hyperalanine aminotransferasemia (57 U per L with expected range for age of 2 to 15 U per L) associated with eubilirubinemia (total 1.2 mg per dl with expected range for age up to 1.5 mg per dl). An erythrocyte sedim entation rate perform ed on the second day o f admission with the patient’s hematocrit having been raised to 30.6 percent following a transfusion o f packed red blood cells was accelerated (62 mm per hour with expected range for age 0 to 13 mm per hour).
Seronegativ ity for antibodies to M ycoplasm a pneumoniae, hepatitis A and B viruses, Epstein-Barr virus and antinuclear antibodies was documented. Similarly, viral and bacterial cultures collectively of urine, blood, stool, throat and bone marrow failed to dem onstrate infectious agents. A bone marrow biopsy revealed plasmacytosis and erythrophagocy- tosis by histiocytes consistent with a hemophagocytic syndrom e. During this first hospital course, she developed overt congestive heart failure which was even tually controlled w ith Lasix® (furosem ide), packed red blood cells, dopamine, fluid control and oxygen.
A second admission within a two week period was occasioned by a history of continuous fever and “two
pillow” orthopnea. Physical examination revealed: a chronically ill appearing child with a temperature of 38.0°C; tender hepatomegaly and nontender splenomegaly; and palpable submandibular, axillary and inguinal lymph nodes. Laboratory data at this time revealed: anem ia (hem oglobin 5.2 g per dl); mild thrombocytopenia (195 X 103 per mm3); and leukocytosis (15.6 X 103 per mm3) with a predominance of neutrophils; a polyclonal gammopathy as evidenced by increased IgG (1,690 m g per dl with expected range for age 633 to 1,280 mg per dl) and IgE (377 U per ml with expected range for age 0 to 211 U per ml) immunoglobulins in the face of normal concentrations for age of IgA and IgM immunoglobulins and the absence of an M-band in the concomitant serum protein electrophoregram; and eufibrinogenem ia (380 mg per dl with expected range 200 to 400 mg per dl).
Subsequently, definitive bone marrow, liver, and lymph node biopsies were obtained under general anesthesia. A diagnosis o f reactive plasmacytosis and mild erythrophagocytosis was rendered on the bone marrow biopsy. The excisional lymph node biopsies from both the cervical (neck) region and omentum revealed marked sinus histiocytosis with lymphocy- tophagocytosis and plasmacytosis consistent with SHM L syndrom e.18 The patient was treated conservatively with hyperalimentation and transfusions and discharged tw enty days postadm ission in a much improved state.
Approximately two w eeks after discharge, she developed cutaneous lesions, and a punch biopsy of the skin revealed a histiocytic proliferation consistent with extranodal involvem ent by SHM L syndrome.23 At the time of the writing of this manuscript (approxim ately 14 months post discharge), the patient is asymptomatic and in a relatively good state o f health.
Materials and Methods
SHML Syndrome
Excisional lymph node biopsies of the cervical (neck) region and om entum as well as an open liver biopsy provided fresh (unfixed) tissues for the histopathologic studies in this case. Portions of the cervical lymph node w ere subm itted for culture and cryostat sectioning, respectively. Touch im prints w ere made of the cut-surfaces of bo th lym ph nodes and portions of each w ere placed in Carson’s (formalin) fixative for routine light and electron microscopy. The wedge-shaped piece of liver showed m ultiple bu t pinpoint-sized, yellowish foci in the fresh state. Touch preparations were made and a portion was subjected to cryostat sec

164 BROWN AND D'CRUZ
tio n in g . T he re m a in d e r o f th e liv e r biopsy was placed in Carson’s fixative.
The aforesaid cryostat sections of fresh tissue w ere sta ined w ith oil red 0 for lipid; the W inkler-Schultze technique for fatty acid peroxides13 and periodic acid-Schiff hematoxylin (PASH). Cryostat sections of liver fixed in Carson’s w ere treated with 1.0 percent osmium tetrox- ide to dem onstrate lipid. Another portion of the Carson’s-fixed liver tissue was post-fixed in 1.0 percent osmium tetrox- ide and processed for electron m icroscopy. Thin sections w ere stained in ura- n y l a c e t a te a n d le a d c i t r a t e a n d examined in a JEO L transmission electron microscope. Representative depar- affinized sections of lym ph node and liver w ere e ither stained with hematoxy- lin-eosin (H and E), Mallory’s procedure for iron, and Fontana-M asson for lipofus- cin or m ounted in phosphate-buffered saline for detection of possible autofluorescen ce . T he la t te r was c a rr ie d out using an ep i-illum ination flu o rescen t microscope employing a RG12 + KV418 exciter filter and an OG515 barrier filter. A d d itio n a l s ta in in g te c h n iq u e s p e r fo rm ed on deparaffin ized sections of l iv e r in c lu d e d : p e r io d ic a c id -S c h iff hem atoxylin (PASH) with and w ithout diastase pretreatm ent; m ethod of Armed Forces Institu te of Pathology (AFIP) for lipofuscin ; d iam ino silver hydrox ide m ethod for reticu lin fibers; aldehyde- th ionin m ethod for hepatitis B surface antigen; Brow n-H opps Gram stain for b ac te ria ; Z ieh l-N ee lsen for acid fast organisisms and silver-m ethenam ine for fungi.14
E r y t h r o p h a g o c y t ic
Ly m p h o h i s t io c y t o s e s
Biopsy m aterials of liver specim ens from th ree cases of familial erythrophagocytic lym phohistiocytosis (FEL) and one case of Epstein-Barr virus-associated hemophagocytic syndrome (VAHS) were
available in our files. The histopathologic and histochemical findings in these were com pared and contrasted w ith those in SH M L syndrome.
Results
As noted previously, excisional biopsies of cervical and om ental lymph nodes revealed m arked expansion of sinuses by a population of reactive histiocytes conta in ing ab u n d an t cytoplasm and associated, on occasion, with intracytoplas- m ic collections of small lym phocytes. Focal plasm acytosis was also p resen t. The perinodal tissues showed striking m ultilocular change in the adipocytes.
A pro liferation of sim ilar appearing histiocytes was ev ident in the liver as m icronodular foci showing both an intralobu lar d istrib u tio n and contiguity at their periphery with sinusoidal cells (figures 1 and 2). O ther distinguishing histopathologic features of such proliferations included focal hyperem ia and associated congestion and dilatation of sinusoidal sp a ce s . F u r th e r m o r e , in th e la t te r regions, erythrophagocytosis by histiocy tes was m ore read ily ap p rec ia ted . F in a lly , no m ic ro o rg a n is m s w e re detected in these lesions using the aforem entioned staining techniques.
Histochem ical and fluorescent microscopic studies on histiocytic cells within these foci revealed the following intracy- toplasm ic findings: occasional Schiff’s p o s itiv e /d ia s ta se -re s is ta n t aggregates (figure 3); lipofuscin inclusions as evidenced by the combination of Fontana- M asson and (Kinyoun’s) carbol fuchsin positivity and appropriate autofluores- cen ce14,21,22 (figure 4); and num erous lipid inclusions that w ere oil red 0 positive (figure 5) and osmiophilic and frequently exhibited W inkler-Schultze positivity at their cytosolic interface (figure 6). U ltrastructural counterparts of several of these histochemical and fluoresc e n t m icro scop ic fin d in g s w e re also

SHML SYNDROME: THE HEPATIC LESION 165
m ■« V;
\ î • ; i . .*y ;■ • : *»v.. ' V . \ *< • * A. •
k
V* *
* * 4
fV*£*3*
V ,
»> <?m
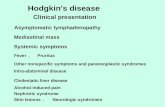
* ' 6FIGURE 1. Low power view of portion of liver lobule (H&E X200) showing a micronodular focus of
relatively pale cells surrounded by trabeculae o f hepatocytes.F ig u r e 2 . H ig h p o w e r v ie w o f su c h m icro n o d u la r fo c i in th e liv e r (H & E x 1000) r ev e a ls a p r e p o n d er a n c e
o f h is t io c y tic c e l ls , s o m e w ith in d e n te d n u c le i an d a b u n d a n t foam y to vacu o lar cy to p la sm .F ig u r e 3. Periodic acid SchifFs (PAS) positive (red) intracytoplasmic aggregates in several histiocytes
within the micronodular foci in the liver (PAS with diastase pretreatment X 1000).F ig u r e 4 . Yellowish-orange autofluorescent inclusions consistent with lipofuscin within histiocytic foci in
the liver. Note bright green autofluorescent erythrocytes within adjacent, congested vascular spaces (depar- affinized, unstained section mounted in phosphate-buffered saline X 1000).
F i g u r e 5 . N u m e r o u s a n iso d im en sio n a l (red) lip id in c lu s io n s o c cu p y th e cy to p la sm o f th e in tra lo b u la r h is t io c y te s in th e liv e r (oil red 0 X 1000).
F ig u r e 6. Indophenol blue synthesis consistent with the presence of fatty acid peroxides evident atperiphery of lipid droplets in hepatic foci using W inkler-Schultze technique (X 1000).
e v id e n t in t r a n s m is s io n e le c t r o n m icrographs of represen tative foci (figures 7 and 8). In comparison with other lymphohistiocytic processes and specifi
cally cases of F E L and VAHS, obvious differences were found. Such differences related to the microanatomical location of the histiocytic proliferations and the

166 BROWN AND D'CRUZ
FIGURE 7. U ltrastru ctu ra l o v e r v ie w o f c lu sters o f in tra lob u lar h is t io c y tic c e l ls w ith in th e liv e r sh o w in g n u m ero u s lip id (L) a n d o cca sio n a l lip o fu sc in (arrow Lf) in c lu sio n s. A lso n o te ly m p h o c y te in u p p e r r igh t h an d co rn er ( X 3750).
degree of steatosis and lipofuscinosis associated with same. These are summarized in table I.
In add ition to the a fo rem en tioned contiguity of sinusoidal cells w ith the in tralobular, m icronodular foci, th ere was som etim es striking proliferation of
K upffer ce lls w h ich a p p e a re d to be expanding and filling the sinusoids and thereby presum ably imposing a physical barrier to the blood flow through same. O n rare occasions, plasm acytosis was noted in association with Kupffer cells. Apart from the morphologic similarity of

SHML SYNDROME: TH E HEPATIC LESION 167
F ig u r e 8. Portions of several histiocytes showing characteristic nuclear indentations. Note numerous, variably sized lipid (L) and occasional lipofuscin (arrow Lf) inclusions and cytoplasmic aggregates o f osmio- philic, granular material (arrowhead Oa). The latter may be contiguous with individual lipid inclusions ( X 12841).
the proliferating Kupffer cells to the histiocytes in the micronodules, there were o ther commonalities to include steatosis, lipofuscinosis, and, to a lesser extent, s id e ro s is an d e ry th ro p h a g o c y to s is .
Finally, a positive reaction for fatty acid peroxides using the W inkler-Schultze technique13 was evident in some sinusoidal, presum ably Kupffer cells in association with lipid inclusions.

1 6 8 B RO W N A N D D ’C RU Z
TABLE I
Comparative Findings in the Liver in Erythrophagocytic Syndromes
Sinus Histiocytosis Familial Erythrophagocytic Virus-AssociatedMassive Lymphadenopathy Lymphohistiocytosis Hemophagocytic Syndrome
(SHML) (FEL) (VAHS)
Infiltrate
Erythrophagocytosis
Steatosis
Lipofuscinosis
Intralobular
Kupffer cells Intralobular infiltrates (occasionally)
Intralobular infiltrates (marked)Kupffer cells (moderate) Hepatocytes (occasionally)
Intralobular infiltrates
Portal with periportal extension
Kupffer cells Portal infiltrates (occasionally)
Absent to minimal in portal infiltratesHepatocytes (mild to marked)
Absent in portal infiltrates
Portal with periportal extension
Kupffer cells Portal infiltrates (occasionally)
Absent to minimal in portal infiltrates Hepatocytes (marked)
Absent in portal infiltrates
Discussion
The clinical and laboratory findings of fever, leukocytosis, polyclonal gammopa- thy, and an accelerated erythrocyte sedim entation ra te w hen coupled w ith the d e v e lo p m e n t o f a ly m p h a d e n o p a th y show ing charac te ris tic histopathologic fea tu re s e s ta b lish e d th e diagnosis of S H M L synd rom e in th is p a tie n t. In ad d itio n , ex tranodal in v o lv em en t by similar appearing histiocytes was evident in biopsies of h e r skin and liver.
A lth o u g h S H M L sy n d ro m e in th e liver m ust be distinguished from other lymphohistiocytic processes such as F E L and VAHS th a t also show p ro m in e n t erythrophagocytosis, the histopathologi- cal differences, based on the finding in our study, are obvious, and, therefore, m ake this task relatively easy. Specifically, th e h istiocytes in SH M L differ from those in F E L and VAHS by showing: (1) an intralobular distribution with portal sparing; (2) m arked steatosis; and (3) lipofuscinosis.
The histogenesis of the hepatic histiocytic proliferation in SHM L appears to be from Kupffer cells. This conclusion is based on the following: (a) the intralobular distribution of the m icronodular foci; (b) the contiguity of said foci with sinu
soidal (Kupffer) cells; (c) an accompanying h y p e r tro p h y and h y p e rp la s ia of Kupffer cells; and (d) commonalities of stea to sis and lipofuscinosis and , to a lesser extent, of erythrophagocytosis and siderosis.
A lthough it is realized tha t th e etio- pathogenesis of the Kupffer cell proliferation in SHM L may involve some inheren t hyper-responsiveness on the part of the reticuloendothelial system to normal s t im u l i , t h e p r e s e n t a u th o r s a re in trig u ed by th e possib ility th a t lip id peroxidation may be initiating the process. The collective evidence for lipid perox idation ’s having occu rred in the proliferating Kupffer cells and/or micronodular histiocytic foci includes histo- chem ical, a u to flu o re sce n t and u ltra - s tru c tu ra l foo tp rin ts o f sam e. T hese com prise : th e p re se n c e o f lipofuscin (which is considered to be a by-product of lipid peroxidation, probably 1-amino- 3 -im inopropene derivatives o f m alon- dialdehyde);21,22,23 the finding of SchifFs positive and granular, osmiophilic aggregates in the cytoplasm of histiocytes by routine histochem istry and transmission e lectron microscopy, respectively;2,5,21 and the dem onstration of fatty acid p e roxides in such cells w ith the W inkler- Schultze technique.13 The elem ents nec

SHM L SYNDROME: TH E HEPATIC LESION 1 6 9
essary to effect lip id peroxidation are u n sa tu ra te d fatty acids and m olecular oxygen w ith “iro n ” serv ing as a catalyst. 17,22,24 In this regard, the presence of siderosis7,24 and of steatosis w ith both g ran u la r, o sm io p h ilic d e n s itie s , and W inkler-Schultze positivity at the cytosolic interface of individual lipid inclusions is noteworthy. Moreover, the activation o f “ scavenger re c e p to rs” 16 in Kupffer cells by products of lipid peroxidation m ight possibly also stim ulate their hypertrophy and proliferation.
The resultant narrowing of sinusoidal spaces w ou ld fo rce in tim a te co n tac t b e tw een K upffer cells and circu lating erythrocytes, perhaps leading to peroxi- dative dam age of red cell m em branes and erythrophagocytosis.12
Finally, the relative rarity of extrano- dal hepatic involvem ent in SHM L synd rom e suggests th a t a com bination of circumstances m ust be operative for this to becom e manifest in any given individual. In this patient, it is clear that m ultiple factors prom oting lipid peroxidation w ere p resen t. For example, free fatty acids for lip id peroxidation appear to have been mobilized from adipose tissue stores as evidenced by the previously described multilocular change in adipocytes in biopsy material. Circumstances prom oting this over the course of her illness include a poor caloric intake consequen t to episodic vomiting and diarrhea and the administration of potential adi- pokinetic agents including theophylline, dopam ine, and a beta-adrenergic stim ula to r .11 A d d itio n a lly , fa c ili ta tio n o r potentiation of lipid peroxidation might have occurred as a result of an increased iron load in the form of transfused red blood cells; the use of the diuretic, furo- sem id e ;25 and th e conversion o f 1,3- dim ethylxanthine (theophylline) to 1,3- d im ethylurate.11 The mechanism of the latter is complex and could involve not only the generation of H2Oa and superox
ide (Oa —) b u t also the reductive release of iron24 from expanded ferritin stores in the Kupffer cells (vide supra).
In summary, it is proposed that lipid peroxidation consequent to an interplay of num erous clinical circumstances and therapeu tic agents may be responsible for stim ulating both erythrophagocytosis and proliferation of Kupffer cells eventuating in intralobular histiocytosis, the hepatic lesion in SH M L syndrome.
Acknowledgm ent
Thanks are extended to Dr. Louis P. Dehner at the University o f Minnesota for reviewing the histopa- thology and concurring in the diagnosis.
References
1. A n s b a c h e r , L . E . , S i n g s e n , B . H . , H o s l e r , M. W., G r im m in g e r , H . , and H e r b e r t , P. N.: Familial erythrophagocytic lymphohistiocytosis: A n association with serum lipid abnormalities. J. Ped. 102:2 7 0 -2 7 3 , 1983.
2 . A r s t il a , A . U . , S m i t h , M. A ., and T r u m p ,B. F.: Microsomal lipid peroxidation: Morphological characterization. Science 275:530- 533, 1972 .
3 . A rya, S . , H o n g , R., and G il b e r t , E . F.: Reactive hem ophagocytic syndrom e. Ped. Pathol. 3:129-141, 1985.
4. B r o w n , R. E . and Ly n c h , S.: L aboratory va lu es-th e pediatric range. Synopsis o f Pediatrics, 6th ed. Hughes, J. G. and Griffith, J. F., eds. St. Louis, The C.V. Mosby Co., 1984, pp. 1002- 1021.
5 . B r o w n , R . E ., C r a v e r , R ., an d D r a k e , R . M .: L ip id p e r o x id a tio n an d p u lm o n a r y h y a lin e m e m b ra n es o f th e n e w b o rn : A h is to c h e m ic a l, f lu o r e s c e n t m ic r o sc o p ic a n d u ltrastru ctu ra l stu d y . A nn . C lin . L ab. Sci. 11:2 5 - 3 0 , 1981 .
6. B u c h in o , J. J., By r d , R. P., and K m e t z , D. R.: Dissem inated sinus histiocytosis with massive lymphadenopathy: Its pathologic aspects. Arch. Pathol. Lab. Med. 206:13-16, 1982.
7. F a ir b a n k s , V F. and B e u t l e r , E.: Iron metabolism . H em atology, 2nd ed. W illiam s, W. J., Beutler, E ., Erslev, A. J., and Rundles, R. W., eds. N ew York, McGraw-Hill Book Co., 1977, pp. 168-177.
8. F o u c a r , E ., R o s a i , J., and D o r f m a n , R. F.: Sinus histiocytosis with massive lymphadenopathy: An analysis o f 14 deaths occurring in a patient registry. Cancer 54:1834-1840, 1984.
9. F o u c a r , E ., R o s a i, J., and D o r f m a n , R. F.: Sinus histiocytosis with massive lymphadenopathy: Ear, nose and throat manifestations. Arch. Otolaryngol. 104:68 7 -6 9 3 , 1978.

1 7 0 BROWN AND D ’CRUZ
10. F o u c a r , E ., R o s a i , J., and DORFMAN, R . F .: The opthalmologic manifestations o f sinus histiocytosis with massive lymphadenopathy. Am. J. Opthalmol. 87:354-367, 1979.
11. G i l m a n , A. G ., G o o d m a n , L. S., and G il m a n , A .: Goodman and Gilman’s The Pharmacological Basis o f Therapeutics, 6th ed. N ew York, Macm illan P ublish ing C o., In c., 1980, pp. 149, 15 4 -1 5 5 , and 592-607 .
12. HEBBEL, R. P. and M i l l e r , W. J.: Phagocytosis o f sickle erythrocytes: Immunologic and oxidative determinants o f hem olytic anemia. Blood 64:733-741, 1984.
13. L i l l i e , R. D . and F u l l m e r , H. M.: Histopathologic Technique and Practical Histochemistry, 4th ed . N ew York, M cG raw -H ill Book C o., 1976, pp. 223-224 .
14. L u n a , L . G .: M anual o f H istologic Staining M eth ods o f th e A rm ed F orces In stitu te o f Pathology, 3rd ed. N ew York, M cG raw -H ill Book C o ., 1968.
15. M c K e n n a , R . W., R is d a l l , R . J., and B r u n n i n g , R . D.: Virus associated hemophagocytic syndrome. Hum. Pathol. 12:39 5 -3 9 8 , 1981.
16. M i l l e r , W. J. and H e b b e l , R. P.: Erythropha- gocytosis as a determinant o f hem olytic rate in sickle disease. The Red Cell: Sixth Ann Arbor Conference. N ew York, Alan R. Liss, Inc., 1984, pp. 8 5 -9 2 .
17. Packer, L., D eamer, D. W. and H eath, R. L.: R egulation and deterioration of structure in m em b ra n es . A d v a n ces in G ero n to lo g ica l Research. Strehler, B. L., ed. N ew York, Academ ic Press, Inc., 1967, vol. 2, pp. 7 7 -120 .
18. R o s a i , J. and D o r f m a n , R . F.: Sinus histiocytosis with massive lymphadenopathy: A newly
recognized benign clinicopathological entity. Arch. Path. 87:63-70 , 1969.
19. R o s a i , J. and D o r f m a n , R . F.: Sinus histiocytosis with massive lymphadenopathy: A pseudo- lymphomatous benign disorder. Analysis of 34 cases. Cancer 30:1174—1188, 1972.
20. S a n c h e z , R ., R o s a i , J., and D o r f m a n , R . F.: Sinus histiocytosis with massive lymphadenopathy: An analysis o f 113 cases with special emphasis on its extranodal manifestations. Lab. Invest. 36:349-350, 1977.
21. S i a k o t o s , A. N. and ARMSTRONG, D .: Age pigm ent, a biochem ical indicator o f intracellular aging. Neurobiology of Aging. Ordy, J. M. and Brizzee, K. R., eds. N ew York, Plenum Press, Inc., 1975, vol. 16, pp. 369-398 .
22. T a p p e l , A. L.: Lipid peroxidation and fluorescent molecular damage to membranes. Pathobi- ology o f C ell M embranes. Trump, B. F. and Arstila, A. U. eds. N ew York, Academic Press, Inc., 1975, pp. 145-170 .
23. T h a w e r a n i , H ., Sa n c h e z , R . L., R o s a i , J., and D o r f m a n , R . F.: The cutaneous manifestations of sinus histiocytosis with massive lymphadenopathy. Arch. Dermatol. 224:191—197, 1978.
24. T h o m a s , C. E ., M o r e h o u s e , L. A ., and A u s t ,S. D .: Ferritin and superoxide-dependent lipid peroxidation. J. Biol. Chem . 260:3 2 7 5 -3 2 8 0 ,1985.
25. W e n d e l , A. and R e it e r , R . : In v itro assessment o f hepatic lipid peroxidation by m alondialde- hyde or ethane determination. Oxygen Radicals in Chemistry and Biology. Bors, W ., Saran, M., and Tait, D ., eds. Berlin, Walter de Gruyter,1984, pp. 345-349 .