Scrotal disorders
-
Upload
airwave12 -
Category
Health & Medicine
-
view
128 -
download
3
Transcript of Scrotal disorders


Congenital disorders
Extra testicular scrotal disorders
Testicular trauma




Ambiguous genitalia
Undescended testes
Patent process vaginalis

Radiologist's role is determination of which internal pelvic structures are present
Associated congenital abnormalities of the urinary tract.
Chromosomal, endocrine and clinical assessment are required
Ultrasound and MRI are the preferred modalities


Majority of prepubertal males
Most commonly lies in the inguinal canal (canalicular).
May lie higher up along the normal line of descent (abdominal testicle)
Most abdominal testicles lie just proximal to the inguinal ring
In a site away from the normal line of descent (ectopic).



Ultrasound first line investigation
Located within inguinal canal
May be normal or atrophic
MRI if not found high signal on T2 and STIR
Testicular phlebography or arteriography





Atrophic with poor spermatogenisis
5 % are not found even at surgical exploration–may be true agenisis
Severely atrophic cannot be located
Increased incidence of malignant neoplasia—x40 timesDevelopment of seminoma
Increased risk in contralateral normal descended testicle
Associated seminal vesicle cysts and agenesis

Failure of closure of the processes vaginalisafter testicular descent
Results in a persistent communication with the abdomen
Incomplete closure of the processes may lead to a developmental cyst,



Hydrocele
Cysts
Varicocele
Epidydmitis
Orcitis
Extratesticular tumors

Formation of fluid between the two layers (visceral and parietal) of the tunica vaginalis.
Mostly idiopathic
May develop as a result of infection (epididymo-orchitis), trauma, malignant testicular tumour or infarction (including torsion).
Sonographically it is seen as an anechoic area partly surrounding the testicle




In infectionclinical and radiological feature of epidydmitis
Chronic infective hydrocele (especially tuberculous) may be associated with considerable calcification of the tunica .
Following trauma a haematocele will exhibit considerable echogenicity.





Common in elderly
The majority are seen in the epididymis.
May be single or multiple.
Classical features on ultrasound
Anechoic, showing distal acoustic enhancement and having no appreciable wall thickness.



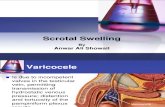
Dilatation of the network of veins draining the testicle
Usually asymptomatic.
Association with subfertility, reported in 21-39% of males
Most frequent between 15 and 25 years of age
Almost always left-sided when symptomatic
Present with scrotal aching and/or soft scrotal mass.
Classically these symptoms worsen during the day while the patient is upright.


Vast majority are primary
Due to developmental abnormalities of the valves and/or the veins themselves.
More likely on the left, where at least 95% are encountered.
Minority occur secondary to a lesion compressing or occluding the testicular vein.

On ultrasound varicoceles are seen as a echo-free serpiginous structures measuring more than 2 mm maximum diameter .
Visible flow may he seen within larger varicoceles.
Their prominence is increased in the upright position and with the Valsalvamanoeuvre.




Inflammation of the epididymis
Mostly seen in young adult males
The clinical presentation varies in severity and acuteness from mild pain, tenderness and scrotal swelling
Severe pyrexal illness with marked scrotal pain and swelling.

On ultrasound the epididymis shows swelling,
Diffuse or patchy reduction in echogenicity,
Doppler ultrasound demonstrates hypervascularity.
A heterogeneous pattern of predominant increase in echogenicity is more frequently associated with chronic epididymitis.
Often an associated hydrocele
Edematous thickening of the overlying skin
There may be coexisting orchitis


Inflammation of the testicle
2/3rd are unilateral.
In the acute phase ultrasound show testicular swelling with patchy or diffuse reduction in echogenicity.
Doppler ultrasound show increased vascularity
Severe orchitis may be associated with ischaemia and infarction with reduced or absent vascularity.

Following resolution the testicle may return to normal.
Severe orchitis heterogeneous areas may develop with a potential for intra testicular abscess formation
May result in atrophy with reduction in size and echogenicity with little or no spermatogenesis.



Twisting of spermatic cord with ischemia of testes
Most frequent in the first year of life or in adolescence, when the testicle is rapidly enlarges
The loose attachment of the testicle and spermatic cord to the scrotum in infants and neonates predisposes to torsion of the entire cord above the level of the scrotum (extravaginaltorsion).
Rotation of the cord within the tunica vaginalis(intravaninal torsion) is the commonest situation in the older age group.





Torsion may be complete or incomplete and spontaneous torsion and detorsion may occur
The degree of torsion determines the severity of the ischemia
In the acute stage ultrasound may be normal or demonstrate a swollen testicle with patchy or diffuse hypoechogenicity .
The epididymis may also become swollen and echo-poor.
There may be a reactive hydrocele and the overlying scrotal skin may be thickened and oedematous.

Doppler ultrasound with sensitivity of 85% in the diagnosis of torsion reduced vascularity (absence or poor colour flow, reduced peak systolic velocities) compared with the unaffected side.
Given the importance of operating within a few hours of the onset of symptoms
Neither the performance nor interpretation of an ultrasound examination should delay surgical treatment.
If there is doubt the urologist should operate on clinical grounds

Is there torsion?

The testicular appendix (hydatid of Morgagni) are vestigial scrotal appendices may undergo torsion
Presents with acute scrotal pain and localized swelling and tenderness.
On ultrasound there is a focal soft-tissue mass adjacent to the upper pole of the epididymis which is often heterogeneous with a central echo-poor area and an associated hydrocele.


Blunt scrotal trauma commonly results in hemorrhage around the testicle (haematocele) and intratesticular hematoma,
May be associated with a tear of the tunica albuginea.
More significant trauma may be associated with demonstrable fragmentation of the testicle.

Ultrasound is the imaging modality.
The commonest finding is a complex haemorrhagic hydrocele (haematocele)
The underlying testicle may show areas of contusion or haematoma, visible as echo-poor areas, often with a relatively linear configuration.

The testicle may be deformed by subcapsularhaemorrhage.
There may be rupture of the capsule (tunica albuginca ) with disruption of the underlying testicle and associated haematoma .
The testicular tear may be linear or complex,
May be fragmentation of the testicle.