Research Article OCH Ameliorates Bone Marrow Failure in...
Transcript of Research Article OCH Ameliorates Bone Marrow Failure in...

Research ArticleOCH Ameliorates Bone Marrow Failure in Mice viaDownregulation of T-Bet Expression
Xiaohong Qiao Xiaotian Xie Wei Shi Jinqing Tang Yuexia Shao and Fuxing Li
Department of Paediatrics Tongji Hospital Tongji University 389 Xincun Road Shanghai 200065 China
Correspondence should be addressed to Xiaotian Xie xiaotianxie4033yeahnet
Received 19 May 2014 Revised 16 July 2014 Accepted 4 August 2014 Published 28 August 2014
Academic Editor David Kaplan
Copyright copy 2014 Xiaohong Qiao et alThis is an open access article distributed under the Creative Commons Attribution Licensewhich permits unrestricted use distribution and reproduction in any medium provided the original work is properly cited
The aim of this study is to evaluate the immunemechanism ofOCH in the treatment of AA (also named bonemarrow failure BMF)induced in mice OCH at a dose of 400 120583gkg was injected intraperitoneally (IP) prior to the induction of BMF Our study showedthat the incidence of BMF was 100 in BMF group and 13 in OCH treatment group Significant higher level of IL-4 and lowerlevel of IFN-120574 were observed in OCH group than that in BMF group (119875 lt 005) as well as untreated group over BMF (119875 lt 005)However there was no significant difference between OCH and untreated group Compared with untreated the expression level ofT-bet in OCH and BMF was all significantly higher However T-bet expression level was lower in OCH than in BMF In additionOCH treatment increased NKT cell fractions of bone marrow and the colonies of CFU-GM In conclusion treatment of OCHprior to the induction of BMF could prevent the incidence of BMF possibly through downregulating T-bet expression leading tothe transition of immune response fromTh1 toTh2 suggesting OCHmight be a new therapeutic approach in the treatment of BMFor AA
1 Introduction
Aplastic anemia (AA) also known as bone marrow fail-ure (BMF) is a blood disorder characterized by impairedhematopoiesis leading to pancytopenia [1]The pathogenesisof AA is very complicated and the impaired hematopoiesisfrom bone marrow was reported to be related with abnor-mal numbers and functions of T lymphocytes as well asdysregulation of cytokine secretion suggesting that AA wasan autoimmune disease characterized by increased Th1 cellsand downstream cytokines [2ndash4] T-bet (T-box expressedin T cell) a member of T-box family discovered in 2000is a Th1-specific transcription factor responsible for Th1cell differentiation [5] Recent studies demonstrated that theexpression level of T-bet was upregulated in AA suggestingits involvement in the pathogenesis of AA [6 7]
OCH is a sphingosine truncated derivative of alpha-gal-actosylceramide (120572-GC) and can stimulate NKT cells toselectively produce Th2 cytokines leading to the transitionof immune response from Th1 to Th2 [8] Previous studiesdemonstrated different cytokines secretion from NKT cellby different stimulus with IFN-120574 predominant by 120572-GC
stimulation and IL-4 by OCH [9] Given the critical rolein the Th2 immune response via NKT activation OCH hasbeen under extensive studies as a therapeutic in the treat-ment of many Th1-related autoimmune diseases such asexperimental encephalomyelitis (EAE) type I diabetes andcollagen-induced arthritis (CIA) [10ndash13]
Abnormal activation of Th1 cells was thought to be themain cause of AA and OCH which was potentially helpful inthe treatment of Th1-related disorders therefore we specu-lated that OCH might be used for AA treatment Our pre-vious studies showed administration of OCH could increasethe overall survival inmicewith BMF [14]However the exactmechanism underlying the effect of OCH on bone marrowremains poorly understood The aim of this study was toinvestigate the effect of OCH on the expression level of T-betthe percentage of NKT cells the colonies of CFU-GM secre-tion of IL-4 and IFN-120574 and the pathology of spleen and bonemarrow in mice with immune-induced BMF Our resultsshowed that single dose OCH prior to the induction of BMFcould ameliorate BMF possibly via downregulating T-betleading to the transition of immune response fromTh1 toTh2
Hindawi Publishing CorporationJournal of Immunology ResearchVolume 2014 Article ID 928743 8 pageshttpdxdoiorg1011552014928743
2 Journal of Immunology Research
2 Materials and Methods
21 Induction of BMF in Mice Inbred male C57BL6 (B6)and female BALBcBy (BALB)mice were purchased from theShanghai Animal Laboratory of Chinese Academy of Scien-ces Hybrid CByB6F1 mice were housed at animal facilities ofthe Animal Laboratory of Tongji Hospital affiliated to TongjiUniversity Animals were provided with standard animalcare free access to diet and water Males and females wereselected from 6 to 16 weeks of age
BMF was induced in mice as previously described [14]Briefly CByB6F1 mice received total body irradiation witha sublethal dose of 55 Gy (137cesium 137cesium source wasprovided by the Department of radiology Fudan UniversityShanghai China) followed by the infusion of lymphocytesisolated from B6 mice to induce bone marrow failure Tailvein blood and bone marrow were collected on day 14 afterlymphocytes infusion and complete blood count and bonemarrow biopsy were performed to evaluate the success ofinduction of bone marrow failure in mice
22 Experimental Groups Design The mice were randomlydivided into five groups as follows untreated group (CByB6F1mice) irradiation group (CByB6F1 mice received 137cesium)BMF group OCH group (OCH was kindly provided by theNational Institutes of Health Tetramer Facility OCH wasdissolved in PBS with 10 dimethyl sulfoxide (DMSO) and400 120583gkg OCH administration prior to the induction ofBMF) control group (PBS with 10 DMSO administration)
23 Complete Blood Count Lateral tail vein blood was drawnon d14 (day 14) and d60 after BMF induction into a tubewith EDTA as anticoagulantThe numbers of white blood cell(WBC) red blood cell (RBC) hemoglobin (HB) and platelet(PLT) were measured by automated blood cell counter
24 Measurement of Level of IFN-120574 and IL-4 in Serum byELISA Orbital sinus blood was drawn on d30 and 60 afterinduction of BMF and was left at room temperature for 24 hfollowed by centrifuging at 3000 rpm for 5minThe superna-tant was isolated to obtain serum The level of IFN-120574 andIL-4 in serum was measured by ELISA kit according tothe manufacturerrsquos instructions (Bender Vienna Austria)Absorbance was read at 450 nm All samples were analyzedin triplicate
25 Assessment of Pathology of Bone Marrow and SpleenPathology of bonemarrow and spleen was evaluated by hem-atoxylin and eosin (HampE) staining as previously described[14] Briefly on d14 and d60 after BMF induction mice weresacrificed Bone marrow and spleen were collected fixedembodied sectioned stained with HampE and examined byusing an Olympus microscope Photographic images of bonemarrow and spleen morphology were captured by using adigital camera
26 CFU Assays Methylcellulose semisolid culture mediumwas obtained as previously described [14] Briefly untreated
mice BMF mice and OCH treated mice were euthanized onday 60 after LN cells infusion BM cells were extracted asepti-cally fromone-side thigh-bone ofmouse BMMNCswere iso-lated through density gradient centrifugation by usingmouselymphocyte separation medium (Haoyang Tianjin China)washed twice with PBS and then resuspended in RPMI-1640(Gibco Rockville MD USA) BMMNCs were planted into24-well plates (Costar CorningUSA) containing the relevantCFU-GM semisolid culture medium For colony forming cellassays colonies gt 50 cells were counted under an invertedmicroscope on day 7
27 Assessment of NKT Cell Percentages by Flow CytometryNKT cell percentages were analyzed in the BMMNCs fromBMF group untreated group and OCH treated group on day60 after LN cells infusion by using flow cytometry accordingto a previous study [14] Briefly 1 times 106 lymphoid cells wereallocated for stainingThe cells were washed with wash buffer(01 sodium azide 01 bovine serum albumin in PBS)and resuspended in the 50120583L of the same buffer One 05 120583Ltest of fluorescently-labeled tetramers was added for stainingand incubated on ice for 30 minutes in the dark and thenwashed with wash buffer Aliquot of optimized FITC-labeledanti-mouse CD3 antibody was added for each staining andthen incubated on ice for 30 minutes in the dark The cellswere washed twice with wash buffer and stored in fixativesolution (1 fetal calf serum 25 formaldehyde in PBS) inthe dark until analysis NKT cells were characterized as theCD3+CD1d120572-GC tetramers + population
28 Measurement of T-Bet Expression Level in Spleen byImmunohistochemical Staining Mice spleen pathology sec-tion was used tomeasure T-bet expression level in spleen by acommercial immunohistochemical staining kit according tomanufacturerrsquos instructions (anti-T-betmonoclonal antibodywas from Santa Cruz Biotechnology lnc USA) The positivecells were defined as tawny granular in cytoplasm andornucleus Five nonrepetitive fields were randomly selectedfrom positive cell region under 10 times 40magnification and thenumbers of positive cells in each field were used to quantifythe expression level of T-bet The percentage of positive cellswas defined as (numbers of positive cellstotal cells) times 100
29 Statistical Analysis All the data were expressed asmean plusmn SD For comparison of blood count mice weightNKT cell percentages T-bet expression level colonies ofCFU and serum level of IL-4 and IFN-120574 among differ-ent groups data was assessed by one-way ANOVA usingSPSS200 software Kaplan-Meier estimator was used for esti-mating the cumulative survival probability after treatmentStatistical significance was defined as the 119875 value less than005 (119875 lt 005)
3 Results
31 BMF Induction On d14 after BMF induction completeblood count including WBC RBC HB and PLT was dra-matically decreased (Table 1) and bonemarrowdysplasiawith
Journal of Immunology Research 3
(a) (b)
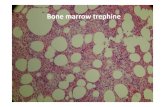
Figure 1 Pathology of bone marrow in mice with untreated (a) or BMF (b) On d14 after BMF induction mice were sacrificed Bone marrowwere collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 1 Complete blood cell count in untreated and BMF group(119899 = 10)
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated 824 plusmn 012 91 plusmn 06 165 plusmn 8 940 plusmn 16
BMF 046 plusmn 013 31 plusmn 07 42 plusmn 8 86 plusmn 15
119865 value 0207 0415 003 0075119905 value 137908 20381 33752 122923119875 value 0000 0000 0000 0000
increased proportion of nonhematopoietic cells (Figure 1)were observed in all the treatedmice indicating the success ofBMF induction Compared to untreated mice bone marrowdysplasia reduced hematopoietic tissue region increasedfatty tissue and decreased numbers of megakaryocytes andhematopoietic cells were seen in BMF mice (Figure 1) Inaddition sinus congestion bleeding and edema were alsofound in bone marrow
32 Mice Weight There was no significant difference in eachgroup before treatment regarding the mice weight Miceweight was increased on d5 in all treatment groups includingthe untreated group (Table 2) compared to day 0 Howeverthe increasing extent was less in all treatment groups thanuntreated as significantly lower weight was observed on d5(119875 lt 001) Compared to BMF group (199plusmn10 g) mice fromirradiation (200 plusmn 10 g) or OCH (200 plusmn 10 g) group hadsignificantly higher weight (119875 lt 001) but lower than that ofuntreated group (218plusmn10 g) Relatively lower weight ofmicefrom irradiation (199plusmn09 g) orOCHgroup (196plusmn09 g) andobviously reduced weight of mice from BMF (149 plusmn 07 g) orcontrol group (150 plusmn 07 g) were found on d10 compared tothat on d5 Mice weight from treatment groups on d10 wasstill significantly lower than that of untreated group (217 plusmn08 g) (119875 lt 001)
33 Mortality Incidence of BMF and Overall Survival Dur-ing 60 days of follow-up no mortality was observed inthe mice from untreated and irradiation groups (Table 3)
10
08
06
04
02
00
000 1000 2000 3000 4000 5000 6000
Cum
ulat
ive s
urvi
val p
roba
bilit
y
Time posttreatment (days)
(1) Untreated(2) Irradiation N = 10
N = 10
(3) BMF N = 15
(4) Control N = 15
(5) OCH N = 15
(1) Censored(2) Censored(3) Censored(4) Censored(5) Censored
Figure 2 Kaplan-Meier analysis of overall survival in mice fromdifferent groups
8 mice died in BMF group and 7 died in control groupBMF occurred in all the remaining mice in BMF and controlgroups (Table 3)However only 2 died inOCHgroupwithoutoccurrence of BMF suggesting the protective effect of OCHin the development of BMF Kaplan-Meier analysis of overallsurvival (Figure 2) showed that there was no significantdifference between untreated and OCH group (119875 gt 005) aswell as between control and BMF group (119875 gt 005) Howevera significant lower overall survival was seen in BMF groupwhen compared to OCH group (119875 lt 005) same to controlgroup compared with untreated (119875 lt 005)
4 Journal of Immunology Research
Table 2 Mice weight in different groups (g)
Group Sample number d0 d5 d10Untreated 10 180 plusmn 04 218 plusmn 10
998771217 plusmn 08
998771
Irradiation 10 180 plusmn 04 200 plusmn 10998771
199 plusmn 09998771
BMF 15 180 plusmn 04 199 plusmn 10
149 plusmn 07
Control 15 180 plusmn 03 199 plusmn 09
150 plusmn 07
OCH 15 180 plusmn 04 200 plusmn 10998771
196 plusmn 09998771
Statistic 119865 = 006 119865 = 7741 119865 = 146234
119875 value 1 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
(a) (b) (c)
Figure 3 Pathology evaluation of bone marrow on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction micewere sacrificed Bone marrow was collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 3 Incidence of mortality and BMF in mice with differenttreatment
Group Sample number Mortality BMFUntreated 10 0 0Irradiation 10 0 0BMF 15 8 7Control 15 7 8OCH 15 2 0
34 Complete Blood Cell Count after Treatment On d14 post-treatment numbers of WBC RBC Hb and PLT (Table 4)in BMF and OCH groups were significantly lower comparedto that in untreated group (119875 lt 001) However significantlower numbers of complete blood cell were observed in BMFcompared to OCH group (119875 lt 001) No statistical differencewas seen between irradiation versus untreated group andcontrol versus BMF group (119875 gt 005) except lower numberof WBC found in irradiation than in untreated group (119875 lt001)
On d60 after treatment complete blood cell count(Table 5) was normalized in OCH and irradiation groups andremained still significantly lower in BMF and control groupscompared to untreated group (119875 lt 005)
35 Serum Level of IFN-120574 and IL-4 Serum was isolated fromorbital sinus blood taken from untreated BMF and OCHgroups of mice on d30 and d60 posttreatment and used tomeasure level of IFN-120574 and IL-4 Compared to untreated and
OCH groups higher level of IFN-120574 and lower level of IL-4were found in BMF group However no significant differencewas observed between untreated and OCH groups (Table 6)
36 Pathology of BoneMarrow and Spleen Bonemarrow andspleen were collected to measure pathology changes on d60posttreatment Compared to untreated mice similar pathol-ogy changes of bone marrow to that observed on d14 afterinduction described in a previous section (BMF induction)were seen in BMF group (Figure 3) More hematopoietic cellsand less nonhematopoietic cells were found in OCH groupRegarding the spleen pathology compared to untreatedmice (Figure 4(a)) the following changes were observedin BMF mice loose structure of spleen tissues indistinctspleen lymph follicle structure reduced acini lienalis obscuregerminal center dilation of splenic sinusoid and thickeningand hyalinization of splenic arteriole wall in some areas(Figure 4(b)) However all the pathological changes occurredin BMF mice were improved in OCH group (Figure 4(c))indicating that OCH treatment could ameliorate BMF asso-ciated with the damage to bone marrow and spleen
37 Increased Numbers of Mononuclear Cells and CFU byOCH On d60 after treatment expanded incubation of CFUcolony in the CFU-GM semisolid culture medium was con-ducted for 7 days for the untreated BMF and OCH groupsof mice Cells with more than 50 colonies were counted Thenumbers of mononuclear cells in BM and CFU in the BMFmice were much lower than that in untreated mice and OCH
Journal of Immunology Research 5
Table 4 Complete blood cell count on d14 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 823 plusmn 011
99877193 plusmn 07
998771163 plusmn 9
998771940 plusmn 8
998771
Irradiation(119899 = 10) 446 plusmn 011
99877191 plusmn 07
998771160 plusmn 8
998771936 plusmn 9
998771
BMF(119899 = 14) 044 plusmn 010
31 plusmn 09
43 plusmn 8
87 plusmn 9
Control(119899 = 14) 045 plusmn 009
32 plusmn 07
42 plusmn 8
89 plusmn 9
OCH(119899 = 15) 425 plusmn 010
99877163 plusmn 08
998771108 plusmn 7
998771560 plusmn 8
998771
Statistic 119865 = 10531525 119865 = 211535 119865 = 670289 119865 = 28505728
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 5 Complete blood cell count on d60 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 843 plusmn 008
99877193 plusmn 06
998771163 plusmn 8
998771880 plusmn 10
998771
Irradiation(119899 = 10) 838 plusmn 007
99877191 plusmn 07
998771160 plusmn 7
998771878 plusmn 8
998771
BMF(119899 = 7) 075 plusmn 010
32 plusmn 06
50 plusmn 9
90 plusmn 8
Control(119899 = 8) 074 plusmn 010
35 plusmn 06
51 plusmn 8
94 plusmn 9
OCH(119899 = 13) 837 plusmn 008
99877192 plusmn 06
998771161 plusmn 8
998771875 plusmn 10
998771
Statistic 119865 = 14553792 119865 = 236290 119865 = 461030 119865 = 20922423
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 6 Serum level of IL-4 and IFN-120574 (pgmL 119899 = 7)
Group IL-4 IFN-120574d30 d60 d30 d60
Untreated 75 plusmn 4998771
73 plusmn 3998771
34 plusmn 3998771
34 plusmn 3998771
BMF 35 plusmn 3
36 plusmn 3
76 plusmn 4
76 plusmn 3
OCH 76 plusmn 4998771
74 plusmn 3998771
33 plusmn 3998771
34 plusmn 3998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 7 The numbers of mononuclear cells and CFU
Group 119873Mononuclear cells CFU(times106 a single thigh bone)
Untreated 7 14 plusmn 06 50 plusmn 6
BMF 7 2 plusmn 01
6 plusmn 1
OCH 7 12 plusmn 06998771
46 plusmn 5998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
mice (119875 lt 001) (Table 7) No difference in mononuclear cellnumbers and CFU was found between untreated mice andthe OCH-treated mice
38 Increased NKT Cell Fraction of BMMNCs by OCH Treat-ment Compared with the untreated mice fewer NKT cellfraction of BMMNCs in BMFmice (024 plusmn 003 versus 184 plusmn005 119875 lt 001 119899 = 7) were found Proportional NKT cellsof BMMNCs were higher in the OCH group mice (328 plusmn
007 119899 = 7) than those in BMF mice (119875 lt 001) (Figure 5)These data revealed that NKT cell population of BMMNCs inBMF mice was decreased whereas OCH increased NKT cellpopulation
39 T-Bet Expression Level in Spleen Immunohistochemi-cal staining was used to determine the protein expressionlevel of T-bet in spleen As seen in Figure 6 significantlyhigher expression level of T-bet was seen in BMF group
6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

2 Journal of Immunology Research
2 Materials and Methods
21 Induction of BMF in Mice Inbred male C57BL6 (B6)and female BALBcBy (BALB)mice were purchased from theShanghai Animal Laboratory of Chinese Academy of Scien-ces Hybrid CByB6F1 mice were housed at animal facilities ofthe Animal Laboratory of Tongji Hospital affiliated to TongjiUniversity Animals were provided with standard animalcare free access to diet and water Males and females wereselected from 6 to 16 weeks of age
BMF was induced in mice as previously described [14]Briefly CByB6F1 mice received total body irradiation witha sublethal dose of 55 Gy (137cesium 137cesium source wasprovided by the Department of radiology Fudan UniversityShanghai China) followed by the infusion of lymphocytesisolated from B6 mice to induce bone marrow failure Tailvein blood and bone marrow were collected on day 14 afterlymphocytes infusion and complete blood count and bonemarrow biopsy were performed to evaluate the success ofinduction of bone marrow failure in mice
22 Experimental Groups Design The mice were randomlydivided into five groups as follows untreated group (CByB6F1mice) irradiation group (CByB6F1 mice received 137cesium)BMF group OCH group (OCH was kindly provided by theNational Institutes of Health Tetramer Facility OCH wasdissolved in PBS with 10 dimethyl sulfoxide (DMSO) and400 120583gkg OCH administration prior to the induction ofBMF) control group (PBS with 10 DMSO administration)
23 Complete Blood Count Lateral tail vein blood was drawnon d14 (day 14) and d60 after BMF induction into a tubewith EDTA as anticoagulantThe numbers of white blood cell(WBC) red blood cell (RBC) hemoglobin (HB) and platelet(PLT) were measured by automated blood cell counter
24 Measurement of Level of IFN-120574 and IL-4 in Serum byELISA Orbital sinus blood was drawn on d30 and 60 afterinduction of BMF and was left at room temperature for 24 hfollowed by centrifuging at 3000 rpm for 5minThe superna-tant was isolated to obtain serum The level of IFN-120574 andIL-4 in serum was measured by ELISA kit according tothe manufacturerrsquos instructions (Bender Vienna Austria)Absorbance was read at 450 nm All samples were analyzedin triplicate
25 Assessment of Pathology of Bone Marrow and SpleenPathology of bonemarrow and spleen was evaluated by hem-atoxylin and eosin (HampE) staining as previously described[14] Briefly on d14 and d60 after BMF induction mice weresacrificed Bone marrow and spleen were collected fixedembodied sectioned stained with HampE and examined byusing an Olympus microscope Photographic images of bonemarrow and spleen morphology were captured by using adigital camera
26 CFU Assays Methylcellulose semisolid culture mediumwas obtained as previously described [14] Briefly untreated
mice BMF mice and OCH treated mice were euthanized onday 60 after LN cells infusion BM cells were extracted asepti-cally fromone-side thigh-bone ofmouse BMMNCswere iso-lated through density gradient centrifugation by usingmouselymphocyte separation medium (Haoyang Tianjin China)washed twice with PBS and then resuspended in RPMI-1640(Gibco Rockville MD USA) BMMNCs were planted into24-well plates (Costar CorningUSA) containing the relevantCFU-GM semisolid culture medium For colony forming cellassays colonies gt 50 cells were counted under an invertedmicroscope on day 7
27 Assessment of NKT Cell Percentages by Flow CytometryNKT cell percentages were analyzed in the BMMNCs fromBMF group untreated group and OCH treated group on day60 after LN cells infusion by using flow cytometry accordingto a previous study [14] Briefly 1 times 106 lymphoid cells wereallocated for stainingThe cells were washed with wash buffer(01 sodium azide 01 bovine serum albumin in PBS)and resuspended in the 50120583L of the same buffer One 05 120583Ltest of fluorescently-labeled tetramers was added for stainingand incubated on ice for 30 minutes in the dark and thenwashed with wash buffer Aliquot of optimized FITC-labeledanti-mouse CD3 antibody was added for each staining andthen incubated on ice for 30 minutes in the dark The cellswere washed twice with wash buffer and stored in fixativesolution (1 fetal calf serum 25 formaldehyde in PBS) inthe dark until analysis NKT cells were characterized as theCD3+CD1d120572-GC tetramers + population
28 Measurement of T-Bet Expression Level in Spleen byImmunohistochemical Staining Mice spleen pathology sec-tion was used tomeasure T-bet expression level in spleen by acommercial immunohistochemical staining kit according tomanufacturerrsquos instructions (anti-T-betmonoclonal antibodywas from Santa Cruz Biotechnology lnc USA) The positivecells were defined as tawny granular in cytoplasm andornucleus Five nonrepetitive fields were randomly selectedfrom positive cell region under 10 times 40magnification and thenumbers of positive cells in each field were used to quantifythe expression level of T-bet The percentage of positive cellswas defined as (numbers of positive cellstotal cells) times 100
29 Statistical Analysis All the data were expressed asmean plusmn SD For comparison of blood count mice weightNKT cell percentages T-bet expression level colonies ofCFU and serum level of IL-4 and IFN-120574 among differ-ent groups data was assessed by one-way ANOVA usingSPSS200 software Kaplan-Meier estimator was used for esti-mating the cumulative survival probability after treatmentStatistical significance was defined as the 119875 value less than005 (119875 lt 005)
3 Results
31 BMF Induction On d14 after BMF induction completeblood count including WBC RBC HB and PLT was dra-matically decreased (Table 1) and bonemarrowdysplasiawith
Journal of Immunology Research 3
(a) (b)
Figure 1 Pathology of bone marrow in mice with untreated (a) or BMF (b) On d14 after BMF induction mice were sacrificed Bone marrowwere collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 1 Complete blood cell count in untreated and BMF group(119899 = 10)
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated 824 plusmn 012 91 plusmn 06 165 plusmn 8 940 plusmn 16
BMF 046 plusmn 013 31 plusmn 07 42 plusmn 8 86 plusmn 15
119865 value 0207 0415 003 0075119905 value 137908 20381 33752 122923119875 value 0000 0000 0000 0000
increased proportion of nonhematopoietic cells (Figure 1)were observed in all the treatedmice indicating the success ofBMF induction Compared to untreated mice bone marrowdysplasia reduced hematopoietic tissue region increasedfatty tissue and decreased numbers of megakaryocytes andhematopoietic cells were seen in BMF mice (Figure 1) Inaddition sinus congestion bleeding and edema were alsofound in bone marrow
32 Mice Weight There was no significant difference in eachgroup before treatment regarding the mice weight Miceweight was increased on d5 in all treatment groups includingthe untreated group (Table 2) compared to day 0 Howeverthe increasing extent was less in all treatment groups thanuntreated as significantly lower weight was observed on d5(119875 lt 001) Compared to BMF group (199plusmn10 g) mice fromirradiation (200 plusmn 10 g) or OCH (200 plusmn 10 g) group hadsignificantly higher weight (119875 lt 001) but lower than that ofuntreated group (218plusmn10 g) Relatively lower weight ofmicefrom irradiation (199plusmn09 g) orOCHgroup (196plusmn09 g) andobviously reduced weight of mice from BMF (149 plusmn 07 g) orcontrol group (150 plusmn 07 g) were found on d10 compared tothat on d5 Mice weight from treatment groups on d10 wasstill significantly lower than that of untreated group (217 plusmn08 g) (119875 lt 001)
33 Mortality Incidence of BMF and Overall Survival Dur-ing 60 days of follow-up no mortality was observed inthe mice from untreated and irradiation groups (Table 3)
10
08
06
04
02
00
000 1000 2000 3000 4000 5000 6000
Cum
ulat
ive s
urvi
val p
roba
bilit
y
Time posttreatment (days)
(1) Untreated(2) Irradiation N = 10
N = 10
(3) BMF N = 15
(4) Control N = 15
(5) OCH N = 15
(1) Censored(2) Censored(3) Censored(4) Censored(5) Censored
Figure 2 Kaplan-Meier analysis of overall survival in mice fromdifferent groups
8 mice died in BMF group and 7 died in control groupBMF occurred in all the remaining mice in BMF and controlgroups (Table 3)However only 2 died inOCHgroupwithoutoccurrence of BMF suggesting the protective effect of OCHin the development of BMF Kaplan-Meier analysis of overallsurvival (Figure 2) showed that there was no significantdifference between untreated and OCH group (119875 gt 005) aswell as between control and BMF group (119875 gt 005) Howevera significant lower overall survival was seen in BMF groupwhen compared to OCH group (119875 lt 005) same to controlgroup compared with untreated (119875 lt 005)
4 Journal of Immunology Research
Table 2 Mice weight in different groups (g)
Group Sample number d0 d5 d10Untreated 10 180 plusmn 04 218 plusmn 10
998771217 plusmn 08
998771
Irradiation 10 180 plusmn 04 200 plusmn 10998771
199 plusmn 09998771
BMF 15 180 plusmn 04 199 plusmn 10
149 plusmn 07
Control 15 180 plusmn 03 199 plusmn 09
150 plusmn 07
OCH 15 180 plusmn 04 200 plusmn 10998771
196 plusmn 09998771
Statistic 119865 = 006 119865 = 7741 119865 = 146234
119875 value 1 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
(a) (b) (c)
Figure 3 Pathology evaluation of bone marrow on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction micewere sacrificed Bone marrow was collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 3 Incidence of mortality and BMF in mice with differenttreatment
Group Sample number Mortality BMFUntreated 10 0 0Irradiation 10 0 0BMF 15 8 7Control 15 7 8OCH 15 2 0
34 Complete Blood Cell Count after Treatment On d14 post-treatment numbers of WBC RBC Hb and PLT (Table 4)in BMF and OCH groups were significantly lower comparedto that in untreated group (119875 lt 001) However significantlower numbers of complete blood cell were observed in BMFcompared to OCH group (119875 lt 001) No statistical differencewas seen between irradiation versus untreated group andcontrol versus BMF group (119875 gt 005) except lower numberof WBC found in irradiation than in untreated group (119875 lt001)
On d60 after treatment complete blood cell count(Table 5) was normalized in OCH and irradiation groups andremained still significantly lower in BMF and control groupscompared to untreated group (119875 lt 005)
35 Serum Level of IFN-120574 and IL-4 Serum was isolated fromorbital sinus blood taken from untreated BMF and OCHgroups of mice on d30 and d60 posttreatment and used tomeasure level of IFN-120574 and IL-4 Compared to untreated and
OCH groups higher level of IFN-120574 and lower level of IL-4were found in BMF group However no significant differencewas observed between untreated and OCH groups (Table 6)
36 Pathology of BoneMarrow and Spleen Bonemarrow andspleen were collected to measure pathology changes on d60posttreatment Compared to untreated mice similar pathol-ogy changes of bone marrow to that observed on d14 afterinduction described in a previous section (BMF induction)were seen in BMF group (Figure 3) More hematopoietic cellsand less nonhematopoietic cells were found in OCH groupRegarding the spleen pathology compared to untreatedmice (Figure 4(a)) the following changes were observedin BMF mice loose structure of spleen tissues indistinctspleen lymph follicle structure reduced acini lienalis obscuregerminal center dilation of splenic sinusoid and thickeningand hyalinization of splenic arteriole wall in some areas(Figure 4(b)) However all the pathological changes occurredin BMF mice were improved in OCH group (Figure 4(c))indicating that OCH treatment could ameliorate BMF asso-ciated with the damage to bone marrow and spleen
37 Increased Numbers of Mononuclear Cells and CFU byOCH On d60 after treatment expanded incubation of CFUcolony in the CFU-GM semisolid culture medium was con-ducted for 7 days for the untreated BMF and OCH groupsof mice Cells with more than 50 colonies were counted Thenumbers of mononuclear cells in BM and CFU in the BMFmice were much lower than that in untreated mice and OCH
Journal of Immunology Research 5
Table 4 Complete blood cell count on d14 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 823 plusmn 011
99877193 plusmn 07
998771163 plusmn 9
998771940 plusmn 8
998771
Irradiation(119899 = 10) 446 plusmn 011
99877191 plusmn 07
998771160 plusmn 8
998771936 plusmn 9
998771
BMF(119899 = 14) 044 plusmn 010
31 plusmn 09
43 plusmn 8
87 plusmn 9
Control(119899 = 14) 045 plusmn 009
32 plusmn 07
42 plusmn 8
89 plusmn 9
OCH(119899 = 15) 425 plusmn 010
99877163 plusmn 08
998771108 plusmn 7
998771560 plusmn 8
998771
Statistic 119865 = 10531525 119865 = 211535 119865 = 670289 119865 = 28505728
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 5 Complete blood cell count on d60 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 843 plusmn 008
99877193 plusmn 06
998771163 plusmn 8
998771880 plusmn 10
998771
Irradiation(119899 = 10) 838 plusmn 007
99877191 plusmn 07
998771160 plusmn 7
998771878 plusmn 8
998771
BMF(119899 = 7) 075 plusmn 010
32 plusmn 06
50 plusmn 9
90 plusmn 8
Control(119899 = 8) 074 plusmn 010
35 plusmn 06
51 plusmn 8
94 plusmn 9
OCH(119899 = 13) 837 plusmn 008
99877192 plusmn 06
998771161 plusmn 8
998771875 plusmn 10
998771
Statistic 119865 = 14553792 119865 = 236290 119865 = 461030 119865 = 20922423
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 6 Serum level of IL-4 and IFN-120574 (pgmL 119899 = 7)
Group IL-4 IFN-120574d30 d60 d30 d60
Untreated 75 plusmn 4998771
73 plusmn 3998771
34 plusmn 3998771
34 plusmn 3998771
BMF 35 plusmn 3
36 plusmn 3
76 plusmn 4
76 plusmn 3
OCH 76 plusmn 4998771
74 plusmn 3998771
33 plusmn 3998771
34 plusmn 3998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 7 The numbers of mononuclear cells and CFU
Group 119873Mononuclear cells CFU(times106 a single thigh bone)
Untreated 7 14 plusmn 06 50 plusmn 6
BMF 7 2 plusmn 01
6 plusmn 1
OCH 7 12 plusmn 06998771
46 plusmn 5998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
mice (119875 lt 001) (Table 7) No difference in mononuclear cellnumbers and CFU was found between untreated mice andthe OCH-treated mice
38 Increased NKT Cell Fraction of BMMNCs by OCH Treat-ment Compared with the untreated mice fewer NKT cellfraction of BMMNCs in BMFmice (024 plusmn 003 versus 184 plusmn005 119875 lt 001 119899 = 7) were found Proportional NKT cellsof BMMNCs were higher in the OCH group mice (328 plusmn
007 119899 = 7) than those in BMF mice (119875 lt 001) (Figure 5)These data revealed that NKT cell population of BMMNCs inBMF mice was decreased whereas OCH increased NKT cellpopulation
39 T-Bet Expression Level in Spleen Immunohistochemi-cal staining was used to determine the protein expressionlevel of T-bet in spleen As seen in Figure 6 significantlyhigher expression level of T-bet was seen in BMF group
6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

Journal of Immunology Research 3
(a) (b)
Figure 1 Pathology of bone marrow in mice with untreated (a) or BMF (b) On d14 after BMF induction mice were sacrificed Bone marrowwere collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 1 Complete blood cell count in untreated and BMF group(119899 = 10)
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated 824 plusmn 012 91 plusmn 06 165 plusmn 8 940 plusmn 16
BMF 046 plusmn 013 31 plusmn 07 42 plusmn 8 86 plusmn 15
119865 value 0207 0415 003 0075119905 value 137908 20381 33752 122923119875 value 0000 0000 0000 0000
increased proportion of nonhematopoietic cells (Figure 1)were observed in all the treatedmice indicating the success ofBMF induction Compared to untreated mice bone marrowdysplasia reduced hematopoietic tissue region increasedfatty tissue and decreased numbers of megakaryocytes andhematopoietic cells were seen in BMF mice (Figure 1) Inaddition sinus congestion bleeding and edema were alsofound in bone marrow
32 Mice Weight There was no significant difference in eachgroup before treatment regarding the mice weight Miceweight was increased on d5 in all treatment groups includingthe untreated group (Table 2) compared to day 0 Howeverthe increasing extent was less in all treatment groups thanuntreated as significantly lower weight was observed on d5(119875 lt 001) Compared to BMF group (199plusmn10 g) mice fromirradiation (200 plusmn 10 g) or OCH (200 plusmn 10 g) group hadsignificantly higher weight (119875 lt 001) but lower than that ofuntreated group (218plusmn10 g) Relatively lower weight ofmicefrom irradiation (199plusmn09 g) orOCHgroup (196plusmn09 g) andobviously reduced weight of mice from BMF (149 plusmn 07 g) orcontrol group (150 plusmn 07 g) were found on d10 compared tothat on d5 Mice weight from treatment groups on d10 wasstill significantly lower than that of untreated group (217 plusmn08 g) (119875 lt 001)
33 Mortality Incidence of BMF and Overall Survival Dur-ing 60 days of follow-up no mortality was observed inthe mice from untreated and irradiation groups (Table 3)
10
08
06
04
02
00
000 1000 2000 3000 4000 5000 6000
Cum
ulat
ive s
urvi
val p
roba
bilit
y
Time posttreatment (days)
(1) Untreated(2) Irradiation N = 10
N = 10
(3) BMF N = 15
(4) Control N = 15
(5) OCH N = 15
(1) Censored(2) Censored(3) Censored(4) Censored(5) Censored
Figure 2 Kaplan-Meier analysis of overall survival in mice fromdifferent groups
8 mice died in BMF group and 7 died in control groupBMF occurred in all the remaining mice in BMF and controlgroups (Table 3)However only 2 died inOCHgroupwithoutoccurrence of BMF suggesting the protective effect of OCHin the development of BMF Kaplan-Meier analysis of overallsurvival (Figure 2) showed that there was no significantdifference between untreated and OCH group (119875 gt 005) aswell as between control and BMF group (119875 gt 005) Howevera significant lower overall survival was seen in BMF groupwhen compared to OCH group (119875 lt 005) same to controlgroup compared with untreated (119875 lt 005)
4 Journal of Immunology Research
Table 2 Mice weight in different groups (g)
Group Sample number d0 d5 d10Untreated 10 180 plusmn 04 218 plusmn 10
998771217 plusmn 08
998771
Irradiation 10 180 plusmn 04 200 plusmn 10998771
199 plusmn 09998771
BMF 15 180 plusmn 04 199 plusmn 10
149 plusmn 07
Control 15 180 plusmn 03 199 plusmn 09
150 plusmn 07
OCH 15 180 plusmn 04 200 plusmn 10998771
196 plusmn 09998771
Statistic 119865 = 006 119865 = 7741 119865 = 146234
119875 value 1 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
(a) (b) (c)
Figure 3 Pathology evaluation of bone marrow on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction micewere sacrificed Bone marrow was collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 3 Incidence of mortality and BMF in mice with differenttreatment
Group Sample number Mortality BMFUntreated 10 0 0Irradiation 10 0 0BMF 15 8 7Control 15 7 8OCH 15 2 0
34 Complete Blood Cell Count after Treatment On d14 post-treatment numbers of WBC RBC Hb and PLT (Table 4)in BMF and OCH groups were significantly lower comparedto that in untreated group (119875 lt 001) However significantlower numbers of complete blood cell were observed in BMFcompared to OCH group (119875 lt 001) No statistical differencewas seen between irradiation versus untreated group andcontrol versus BMF group (119875 gt 005) except lower numberof WBC found in irradiation than in untreated group (119875 lt001)
On d60 after treatment complete blood cell count(Table 5) was normalized in OCH and irradiation groups andremained still significantly lower in BMF and control groupscompared to untreated group (119875 lt 005)
35 Serum Level of IFN-120574 and IL-4 Serum was isolated fromorbital sinus blood taken from untreated BMF and OCHgroups of mice on d30 and d60 posttreatment and used tomeasure level of IFN-120574 and IL-4 Compared to untreated and
OCH groups higher level of IFN-120574 and lower level of IL-4were found in BMF group However no significant differencewas observed between untreated and OCH groups (Table 6)
36 Pathology of BoneMarrow and Spleen Bonemarrow andspleen were collected to measure pathology changes on d60posttreatment Compared to untreated mice similar pathol-ogy changes of bone marrow to that observed on d14 afterinduction described in a previous section (BMF induction)were seen in BMF group (Figure 3) More hematopoietic cellsand less nonhematopoietic cells were found in OCH groupRegarding the spleen pathology compared to untreatedmice (Figure 4(a)) the following changes were observedin BMF mice loose structure of spleen tissues indistinctspleen lymph follicle structure reduced acini lienalis obscuregerminal center dilation of splenic sinusoid and thickeningand hyalinization of splenic arteriole wall in some areas(Figure 4(b)) However all the pathological changes occurredin BMF mice were improved in OCH group (Figure 4(c))indicating that OCH treatment could ameliorate BMF asso-ciated with the damage to bone marrow and spleen
37 Increased Numbers of Mononuclear Cells and CFU byOCH On d60 after treatment expanded incubation of CFUcolony in the CFU-GM semisolid culture medium was con-ducted for 7 days for the untreated BMF and OCH groupsof mice Cells with more than 50 colonies were counted Thenumbers of mononuclear cells in BM and CFU in the BMFmice were much lower than that in untreated mice and OCH
Journal of Immunology Research 5
Table 4 Complete blood cell count on d14 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 823 plusmn 011
99877193 plusmn 07
998771163 plusmn 9
998771940 plusmn 8
998771
Irradiation(119899 = 10) 446 plusmn 011
99877191 plusmn 07
998771160 plusmn 8
998771936 plusmn 9
998771
BMF(119899 = 14) 044 plusmn 010
31 plusmn 09
43 plusmn 8
87 plusmn 9
Control(119899 = 14) 045 plusmn 009
32 plusmn 07
42 plusmn 8
89 plusmn 9
OCH(119899 = 15) 425 plusmn 010
99877163 plusmn 08
998771108 plusmn 7
998771560 plusmn 8
998771
Statistic 119865 = 10531525 119865 = 211535 119865 = 670289 119865 = 28505728
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 5 Complete blood cell count on d60 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 843 plusmn 008
99877193 plusmn 06
998771163 plusmn 8
998771880 plusmn 10
998771
Irradiation(119899 = 10) 838 plusmn 007
99877191 plusmn 07
998771160 plusmn 7
998771878 plusmn 8
998771
BMF(119899 = 7) 075 plusmn 010
32 plusmn 06
50 plusmn 9
90 plusmn 8
Control(119899 = 8) 074 plusmn 010
35 plusmn 06
51 plusmn 8
94 plusmn 9
OCH(119899 = 13) 837 plusmn 008
99877192 plusmn 06
998771161 plusmn 8
998771875 plusmn 10
998771
Statistic 119865 = 14553792 119865 = 236290 119865 = 461030 119865 = 20922423
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 6 Serum level of IL-4 and IFN-120574 (pgmL 119899 = 7)
Group IL-4 IFN-120574d30 d60 d30 d60
Untreated 75 plusmn 4998771
73 plusmn 3998771
34 plusmn 3998771
34 plusmn 3998771
BMF 35 plusmn 3
36 plusmn 3
76 plusmn 4
76 plusmn 3
OCH 76 plusmn 4998771
74 plusmn 3998771
33 plusmn 3998771
34 plusmn 3998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 7 The numbers of mononuclear cells and CFU
Group 119873Mononuclear cells CFU(times106 a single thigh bone)
Untreated 7 14 plusmn 06 50 plusmn 6
BMF 7 2 plusmn 01
6 plusmn 1
OCH 7 12 plusmn 06998771
46 plusmn 5998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
mice (119875 lt 001) (Table 7) No difference in mononuclear cellnumbers and CFU was found between untreated mice andthe OCH-treated mice
38 Increased NKT Cell Fraction of BMMNCs by OCH Treat-ment Compared with the untreated mice fewer NKT cellfraction of BMMNCs in BMFmice (024 plusmn 003 versus 184 plusmn005 119875 lt 001 119899 = 7) were found Proportional NKT cellsof BMMNCs were higher in the OCH group mice (328 plusmn
007 119899 = 7) than those in BMF mice (119875 lt 001) (Figure 5)These data revealed that NKT cell population of BMMNCs inBMF mice was decreased whereas OCH increased NKT cellpopulation
39 T-Bet Expression Level in Spleen Immunohistochemi-cal staining was used to determine the protein expressionlevel of T-bet in spleen As seen in Figure 6 significantlyhigher expression level of T-bet was seen in BMF group
6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

4 Journal of Immunology Research
Table 2 Mice weight in different groups (g)
Group Sample number d0 d5 d10Untreated 10 180 plusmn 04 218 plusmn 10
998771217 plusmn 08
998771
Irradiation 10 180 plusmn 04 200 plusmn 10998771
199 plusmn 09998771
BMF 15 180 plusmn 04 199 plusmn 10
149 plusmn 07
Control 15 180 plusmn 03 199 plusmn 09
150 plusmn 07
OCH 15 180 plusmn 04 200 plusmn 10998771
196 plusmn 09998771
Statistic 119865 = 006 119865 = 7741 119865 = 146234
119875 value 1 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
(a) (b) (c)
Figure 3 Pathology evaluation of bone marrow on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction micewere sacrificed Bone marrow was collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
Table 3 Incidence of mortality and BMF in mice with differenttreatment
Group Sample number Mortality BMFUntreated 10 0 0Irradiation 10 0 0BMF 15 8 7Control 15 7 8OCH 15 2 0
34 Complete Blood Cell Count after Treatment On d14 post-treatment numbers of WBC RBC Hb and PLT (Table 4)in BMF and OCH groups were significantly lower comparedto that in untreated group (119875 lt 001) However significantlower numbers of complete blood cell were observed in BMFcompared to OCH group (119875 lt 001) No statistical differencewas seen between irradiation versus untreated group andcontrol versus BMF group (119875 gt 005) except lower numberof WBC found in irradiation than in untreated group (119875 lt001)
On d60 after treatment complete blood cell count(Table 5) was normalized in OCH and irradiation groups andremained still significantly lower in BMF and control groupscompared to untreated group (119875 lt 005)
35 Serum Level of IFN-120574 and IL-4 Serum was isolated fromorbital sinus blood taken from untreated BMF and OCHgroups of mice on d30 and d60 posttreatment and used tomeasure level of IFN-120574 and IL-4 Compared to untreated and
OCH groups higher level of IFN-120574 and lower level of IL-4were found in BMF group However no significant differencewas observed between untreated and OCH groups (Table 6)
36 Pathology of BoneMarrow and Spleen Bonemarrow andspleen were collected to measure pathology changes on d60posttreatment Compared to untreated mice similar pathol-ogy changes of bone marrow to that observed on d14 afterinduction described in a previous section (BMF induction)were seen in BMF group (Figure 3) More hematopoietic cellsand less nonhematopoietic cells were found in OCH groupRegarding the spleen pathology compared to untreatedmice (Figure 4(a)) the following changes were observedin BMF mice loose structure of spleen tissues indistinctspleen lymph follicle structure reduced acini lienalis obscuregerminal center dilation of splenic sinusoid and thickeningand hyalinization of splenic arteriole wall in some areas(Figure 4(b)) However all the pathological changes occurredin BMF mice were improved in OCH group (Figure 4(c))indicating that OCH treatment could ameliorate BMF asso-ciated with the damage to bone marrow and spleen
37 Increased Numbers of Mononuclear Cells and CFU byOCH On d60 after treatment expanded incubation of CFUcolony in the CFU-GM semisolid culture medium was con-ducted for 7 days for the untreated BMF and OCH groupsof mice Cells with more than 50 colonies were counted Thenumbers of mononuclear cells in BM and CFU in the BMFmice were much lower than that in untreated mice and OCH
Journal of Immunology Research 5
Table 4 Complete blood cell count on d14 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 823 plusmn 011
99877193 plusmn 07
998771163 plusmn 9
998771940 plusmn 8
998771
Irradiation(119899 = 10) 446 plusmn 011
99877191 plusmn 07
998771160 plusmn 8
998771936 plusmn 9
998771
BMF(119899 = 14) 044 plusmn 010
31 plusmn 09
43 plusmn 8
87 plusmn 9
Control(119899 = 14) 045 plusmn 009
32 plusmn 07
42 plusmn 8
89 plusmn 9
OCH(119899 = 15) 425 plusmn 010
99877163 plusmn 08
998771108 plusmn 7
998771560 plusmn 8
998771
Statistic 119865 = 10531525 119865 = 211535 119865 = 670289 119865 = 28505728
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 5 Complete blood cell count on d60 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 843 plusmn 008
99877193 plusmn 06
998771163 plusmn 8
998771880 plusmn 10
998771
Irradiation(119899 = 10) 838 plusmn 007
99877191 plusmn 07
998771160 plusmn 7
998771878 plusmn 8
998771
BMF(119899 = 7) 075 plusmn 010
32 plusmn 06
50 plusmn 9
90 plusmn 8
Control(119899 = 8) 074 plusmn 010
35 plusmn 06
51 plusmn 8
94 plusmn 9
OCH(119899 = 13) 837 plusmn 008
99877192 plusmn 06
998771161 plusmn 8
998771875 plusmn 10
998771
Statistic 119865 = 14553792 119865 = 236290 119865 = 461030 119865 = 20922423
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 6 Serum level of IL-4 and IFN-120574 (pgmL 119899 = 7)
Group IL-4 IFN-120574d30 d60 d30 d60
Untreated 75 plusmn 4998771
73 plusmn 3998771
34 plusmn 3998771
34 plusmn 3998771
BMF 35 plusmn 3
36 plusmn 3
76 plusmn 4
76 plusmn 3
OCH 76 plusmn 4998771
74 plusmn 3998771
33 plusmn 3998771
34 plusmn 3998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 7 The numbers of mononuclear cells and CFU
Group 119873Mononuclear cells CFU(times106 a single thigh bone)
Untreated 7 14 plusmn 06 50 plusmn 6
BMF 7 2 plusmn 01
6 plusmn 1
OCH 7 12 plusmn 06998771
46 plusmn 5998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
mice (119875 lt 001) (Table 7) No difference in mononuclear cellnumbers and CFU was found between untreated mice andthe OCH-treated mice
38 Increased NKT Cell Fraction of BMMNCs by OCH Treat-ment Compared with the untreated mice fewer NKT cellfraction of BMMNCs in BMFmice (024 plusmn 003 versus 184 plusmn005 119875 lt 001 119899 = 7) were found Proportional NKT cellsof BMMNCs were higher in the OCH group mice (328 plusmn
007 119899 = 7) than those in BMF mice (119875 lt 001) (Figure 5)These data revealed that NKT cell population of BMMNCs inBMF mice was decreased whereas OCH increased NKT cellpopulation
39 T-Bet Expression Level in Spleen Immunohistochemi-cal staining was used to determine the protein expressionlevel of T-bet in spleen As seen in Figure 6 significantlyhigher expression level of T-bet was seen in BMF group
6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

Journal of Immunology Research 5
Table 4 Complete blood cell count on d14 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 823 plusmn 011
99877193 plusmn 07
998771163 plusmn 9
998771940 plusmn 8
998771
Irradiation(119899 = 10) 446 plusmn 011
99877191 plusmn 07
998771160 plusmn 8
998771936 plusmn 9
998771
BMF(119899 = 14) 044 plusmn 010
31 plusmn 09
43 plusmn 8
87 plusmn 9
Control(119899 = 14) 045 plusmn 009
32 plusmn 07
42 plusmn 8
89 plusmn 9
OCH(119899 = 15) 425 plusmn 010
99877163 plusmn 08
998771108 plusmn 7
998771560 plusmn 8
998771
Statistic 119865 = 10531525 119865 = 211535 119865 = 670289 119865 = 28505728
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 5 Complete blood cell count on d60 after treatment
Group WBC (times109L) RBC (times1012L) HB (gL) PLT (times109L)Untreated(119899 = 10) 843 plusmn 008
99877193 plusmn 06
998771163 plusmn 8
998771880 plusmn 10
998771
Irradiation(119899 = 10) 838 plusmn 007
99877191 plusmn 07
998771160 plusmn 7
998771878 plusmn 8
998771
BMF(119899 = 7) 075 plusmn 010
32 plusmn 06
50 plusmn 9
90 plusmn 8
Control(119899 = 8) 074 plusmn 010
35 plusmn 06
51 plusmn 8
94 plusmn 9
OCH(119899 = 13) 837 plusmn 008
99877192 plusmn 06
998771161 plusmn 8
998771875 plusmn 10
998771
Statistic 119865 = 14553792 119865 = 236290 119865 = 461030 119865 = 20922423
119875 value 0000 0000 0000 0000Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 6 Serum level of IL-4 and IFN-120574 (pgmL 119899 = 7)
Group IL-4 IFN-120574d30 d60 d30 d60
Untreated 75 plusmn 4998771
73 plusmn 3998771
34 plusmn 3998771
34 plusmn 3998771
BMF 35 plusmn 3
36 plusmn 3
76 plusmn 4
76 plusmn 3
OCH 76 plusmn 4998771
74 plusmn 3998771
33 plusmn 3998771
34 plusmn 3998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
Table 7 The numbers of mononuclear cells and CFU
Group 119873Mononuclear cells CFU(times106 a single thigh bone)
Untreated 7 14 plusmn 06 50 plusmn 6
BMF 7 2 plusmn 01
6 plusmn 1
OCH 7 12 plusmn 06998771
46 plusmn 5998771
Compared with untreated 119875 lt 001 Compared with BMF 998771119875 lt 001
mice (119875 lt 001) (Table 7) No difference in mononuclear cellnumbers and CFU was found between untreated mice andthe OCH-treated mice
38 Increased NKT Cell Fraction of BMMNCs by OCH Treat-ment Compared with the untreated mice fewer NKT cellfraction of BMMNCs in BMFmice (024 plusmn 003 versus 184 plusmn005 119875 lt 001 119899 = 7) were found Proportional NKT cellsof BMMNCs were higher in the OCH group mice (328 plusmn
007 119899 = 7) than those in BMF mice (119875 lt 001) (Figure 5)These data revealed that NKT cell population of BMMNCs inBMF mice was decreased whereas OCH increased NKT cellpopulation
39 T-Bet Expression Level in Spleen Immunohistochemi-cal staining was used to determine the protein expressionlevel of T-bet in spleen As seen in Figure 6 significantlyhigher expression level of T-bet was seen in BMF group
6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

6 Journal of Immunology Research
(a) (b) (c)
Figure 4 Pathology evaluation of spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) On d60 after BMF induction mice weresacrificed Spleens were collected fixed embodied sectioned stained with HampE and examined by using an Olympus microscope
00400
00300
00200
00100
0000
BMF Untreated OCH treatedGroup
The N
KT ce
ll fr
actio
n (
)
Figure 5 A fraction of NKT cells in BMMNCs On d60 after BMFinduction NKT cell percentages of BMMNCs fromBMF untreatedand OCH groups were analyzed Compared with the untreatedgroup there were fewer NKT cells of BMMNCs in BMF group(119875 lt 001 by ANOVA 119899 = 7) NKT cell population was increasedin OCH group The NKT cell percentage of BMMNCs was foundwith statistical differences between the OCH group and BMF group(119875 lt 001 by ANOVA 119899 = 7)
(825 plusmn 005) than that in either untreated (078plusmn005119875 lt001) or OCH group (325 plusmn 006 119875 lt 001) suggesting therole of T-bet in the development of BMF as well as the down-regulation of T-bet expression by OCH However T-bet levelin OCH group was still higher than in untreated group (119875 lt001)
4 Discussion
AA is a blood disease characterized by reduced hematopoie-sis resulting in a deficiency of all three blood cell typesred blood cells white blood cells and platelets [15] AA hasbeen known as an autoimmune disease characterized byTh-1-mediated abnormal immune response There are a grow-ing numbers of studies demonstrating the association ofabnormal numbers and function of NKT cells with manyautoimmune diseases such as diabetes multiple sclerosis
and rheumatoid arthritis [8 16] CD1d is known to activateNKT cells as an antigen presenting molecule [17] and CD1d-deficient mice displayed more frequent and severe skin dis-ease as well as increased local inflammation with infiltrationof lymphocytes and dendritic cells in MRL-lprlpr mice [18]Previous studies demonstrated that activatedNKT cells couldinhibit autoimmune diabetes [19] or EAE [10] in micesuggesting the negative immune-regulatory role of NKT cellsas further supported by previous studies showing reducednumbers of NKT cells in patients with AA [20 21] Howeverthe exact role of NKT cells in AA remains poorly understoodIn this study we showed reduced numbers of NKT cells inmice with BMF and increased after administration of OCHsuggesting the involvement of NKT cells in the pathogenesisof AA as an immunoregulatory factor of Th1Th2
Single administration of OCH could prevent EAE char-acterized byTh1-mediated autoimmune disease via inducingTh2 bias of NKT cells to produce IL-4 [10] Our studiesrevealed that single administration of OCH could preventBMF in mice possibly through activation of NKT cells asprevious studies reported that no preventative effect of OCHwas observed in NKT cell deficient mice CIA [22] Giventhe important role in the autoimmune regulation stimulatingNKT cell activation by OCH could be beneficial in thetreatment of many autoimmune diseases including AA
The pathogenesis of AA is very complicated with lots offactors involved leading to the damage to bone marrow andsubsequent impaired hematopoiesis Recent studies on it aremainly focused on the abnormal regulation of autoimmunityespecially subsets and dysfunction of T lymphocytes [23ndash25] Based on the secreted cytokines and functions there aretwo mainly subsets of T cells Th1 and Th2 which produceIFN-120574 IL-2 TNF-120572 and IL-4 IL-5 IL-6 IL-10 and IL-13 respectively [26] Consistent with AA as a Th1-mediatedautoimmune disease mice with BMF displayed higher levelof IFN-120574 and lower level of IL-4 T-bet is a recently identifiedtranscription factor belonging to T-box family [5] As aTh1-specific transcription factor its expression determinesthe differentiation of resting CD4+T cells to Th1 cells viastimulating IFN-120574 expression [27] In addition T-bet couldinduce and maintain the expression level of IL-12R1205732 andreverseTh2 cells intoTh1with the production of IFN-120574which
Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

Journal of Immunology Research 7
(a) (b) (c)
Figure 6 T-bet expression in spleen on d60 in mice with untreated (a) BMF (b) or OCH (c) Mice spleen pathology section was used tomeasure T-bet expression level in spleen by immunohistochemical staining The positive cells were defined as tawny granular in cytoplasmandor nucleus
inhibits secretion ofTh2 cytokines such as IL-4 IL-5 and IL-13 [28] Our studies demonstrated higher expression level ofT-bet in spleen in mice with BMF compared to untreated aswell as the subsequent higher level of IFN-120574 suggesting theinvolvement of T-bet in the development of AA HoweverT-bet and IFN-120574 level were lower in OCH group than inBMF implying the protective role ofOCH in the developmentof BMF possibly through downregulating T-bet expressionMeanwhile less severe damage to bone marrow and spleenwas observed in OCH group than in BMF indicating theprotective effect of OCH on bonemarrow and spleen in BMFmice
In conclusion our studies showed that OCH as a gly-colipid ligand for NKT cells could protect BMF in micethrough downregulating T-bet expression leading to reducedcytokine secretion of IFN-120574 increased secretion of IL-4 andnumbers of CFU-GM as well as NKT fractions ultimatelyresulting in the transition of immune response from Th1 toTh2 Therefore OCH might be as a new therapeutic strategyin the prophylaxis and treatment of AA
Highlights
(i) OCH ameliorates immune-induced bone marrowfailure in mice
(ii) Increased T-bet expression in mice model of bonemarrow failure
(iii) Downregulation of T-bet expression by OCH
Conflict of Interests
All authors have no conflict of interests to declare
Acknowledgments
This research was supported by The Shanghai MunicipalScience and Technology Commission Key Basic ResearchProject and the Project number is 11JC1411900
References
[1] O J Dolberg andY Levy ldquoIdiopathic aplastic anemia diagnosisand classificationrdquo Autoimmunity Reviews vol 13 pp 569ndash5732014
[2] A M Risitano ldquoImmunosuppressive therapies in the manage-ment of acquired immune-mediated marrow failuresrdquo CurrentOpinion in Hematology vol 19 no 1 pp 3ndash13 2012
[3] P Scheinberg and N S Young ldquoHow I treat acquired aplasticanemiardquo Blood vol 120 no 6 pp 1185ndash1196 2012
[4] S Samarasinghe and D K H Webb ldquoHow I manage aplasticanaemia in childrenrdquo British Journal of Haematology vol 157no 1 pp 26ndash40 2012
[5] V Lazarevic L H Glimcher and G M Lord ldquoT-bet a bridgebetween innate and adaptive immunityrdquoNature Reviews Immu-nology vol 13 pp 777ndash789 2013
[6] E E Solomou K Keyvanfar and N S Young ldquoT-bet a Th1transcription factor is up-regulated in T cells frompatients withaplastic anemiardquo Blood vol 107 no 10 pp 3983ndash3991 2006
[7] N N Shan Y Hu X Liu X Wang D Yuan and Y Li ldquoImbal-anced expression of T-bet and T cell immunoglobulin mucin-3in patients with aplastic anaemiardquo Journal of Clinical Immunol-ogy vol 33 no 4 pp 809ndash816 2013
[8] S Rhost S Sedimbi N Kadri and S L Cardell ldquoImmunomod-ulatory type II natural killer T lymphocytes in health anddiseaserdquo The Scandinavian Journal of Immunology vol 76 no3 pp 246ndash255 2012
[9] S Oki C Tomi T Yamamura and S Miyake ldquoPreferential Th2
polarization by OCH is supported by incompetent NKT cellinduction of CD40L and following production of inflammatorycytokines by bystander cells in vivordquo International Immunologyvol 17 no 12 pp 1619ndash1629 2005
[10] K Miyamoto S Miyake and T Yamamura ldquoA synthetic gly-colipid prevents autoimmune encephalomyelitis by inducingTH2 bias of natural killer T cellsrdquoNature vol 413 no 6855 pp531ndash534 2001
[11] S Miyake and T Yamamura ldquoNKT cells and autoimmunediseases unraveling the complexityrdquo Current Topics in Micro-biology and Immunology vol 314 pp 251ndash267 2007
[12] T Yamamura K Sakuishi Z Illes and S Miyake ldquoUnder-standing the behavior of invariant NKT cells in autoimmunediseasesrdquo Journal of Neuroimmunology vol 191 no 1-2 pp 8ndash15 2007
8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

8 Journal of Immunology Research
[13] K M Walker M Rytelewski D M Mazzuca et al ldquoPrevent-ing and curing citrulline-induced autoimmune arthritis in ahumanized mouse model using a Th2-polarizing iNKT cellagonistrdquo Immunology and Cell Biology vol 90 no 6 pp 630ndash639 2012
[14] X Qiao X Xie S Jiang W Shi J Tang and N Zhou ldquoExper-imental bone marrow failure in mice ameliorated by OCH viatippling the balance of released cytokines from Th1 to Th2rdquoImmunopharmacology and Immunotoxicology vol 34 no 3 pp491ndash498 2012
[15] P Scheinberg and J Chen ldquoAplastic anemia what have welearned from animal models and from the clinicrdquo Seminars inHematology vol 50 no 2 pp 156ndash164 2013
[16] S C Hofmann A Bosma L Bruckner-Tuderman et al ldquoInva-riant natural killer T cells are enriched at the site of cutaneousinflammation in lupus erythematosusrdquo Journal of Dermatologi-cal Science vol 71 no 1 pp 22ndash28 2013
[17] J Rossjohn D G Pellicci O Patel L Gapin and D I GodfreyldquoRecognition of CD1d-restricted antigens by natural killer Tcellsrdquo Nature Reviews Immunology vol 12 no 12 pp 845ndash8572012
[18] J-Q Yang T Chun H Liu et al ldquoCD1d deficiency exacerbatesinflammatory dermatitis in MRL-lprlpr micerdquo European Jour-nal of Immunology vol 34 no 6 pp 1723ndash1732 2004
[19] LGhazarian Y Simoni K Pingris L Beaudoin andA LehuenldquoRegulatory role of NKT cells in the prevention of type 1diabetesrdquoMedecine Sciences vol 29 pp 722ndash728 2013
[20] W Zeng J P Maciejewski G Chen et al ldquoSelective reductionof natural killer T cells in the bonemarrow of aplastic anaemiardquoThe British Journal of Haematology vol 119 no 3 pp 803ndash8092002
[21] Y Wang X Hu C Guo et al ldquoPolarization of natural killer Tcells towards an NKT2 subpopulation occurs after stimulationwith 120572-galactosylceramide and rhG-CSF in aplastic anemiardquoActa Haematologica vol 119 no 3 pp 178ndash186 2008
[22] A Chiba S Oki K Miyamoto H Hashimoto T Yamamuraand S Miyake ldquoSuppression of collagen-induced arthritis bynatural killer T cell activation with OCH a sphingosine-trun-cated analog of 120572-galactosylceramiderdquo Arthritis and Rheuma-tism vol 50 no 1 pp 305ndash313 2004
[23] S Kordasti J Marsh S Al-Khan et al ldquoFunctional characteri-zation of CD4+ T cells in aplastic anemiardquo Blood vol 119 no 9pp 2033ndash2043 2012
[24] L C Platanias ldquoAbnormalities in Th17 T cells in aplastic ane-miardquo Blood vol 116 no 20 pp 4039ndash4040 2010
[25] J Shi M Ge S Lu et al ldquoIntrinsic impairment of CD4+25+regulatory T cells in acquired aplastic anemiardquo Blood vol 120no 8 pp 1624ndash1632 2012
[26] S Romagnani ldquoT-cell subsets (Th1 versus Th2)rdquo Annals ofAllergy Asthma and Immunology vol 85 no 1 pp 9ndash21 2000
[27] S J Szabo B M Sullivan C Sternmann A R Satoskar B PSleckman and L H Glimcher ldquoDistinct effects of T-bet in T
1198671
lineage commitment and IFN-120574 production in CD4 and CD8 Tcellsrdquo Science vol 295 no 5553 pp 338ndash342 2002
[28] E G Schulz LMariani A Radbruch and T Hofer ldquoSequentialpolarization and imprinting of type 1 T helper lymphocytes byinterferon-gamma and interleukin-12rdquo Immunity vol 30 no 5pp 673ndash683 2009
Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom

Submit your manuscripts athttpwwwhindawicom
Stem CellsInternational
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
MEDIATORSINFLAMMATION
of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Behavioural Neurology
EndocrinologyInternational Journal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Disease Markers
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
BioMed Research International
OncologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Oxidative Medicine and Cellular Longevity
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
PPAR Research
The Scientific World JournalHindawi Publishing Corporation httpwwwhindawicom Volume 2014
Immunology ResearchHindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Journal of
ObesityJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Computational and Mathematical Methods in Medicine
OphthalmologyJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Diabetes ResearchJournal of
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Research and TreatmentAIDS
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Gastroenterology Research and Practice
Hindawi Publishing Corporationhttpwwwhindawicom Volume 2014
Parkinsonrsquos Disease
Evidence-Based Complementary and Alternative Medicine
Volume 2014Hindawi Publishing Corporationhttpwwwhindawicom