Pressure sore management
-
Upload
shamim-khan -
Category
Healthcare
-
view
441 -
download
4
description
Transcript of Pressure sore management

SURGICAL INTERVERNTIONS IN
PRESSURE SORE MANAGEMENT AT CRP
Presented by : Dr. Shamim Khan RMO, Medical Care
Services CRP, SAVAR

PRESSURE SORE
Pressure sores are localized areas of tissue breakdown in skin and/or underlying tissues that develop when persistent pressure between a bony site and underlying surface obstructs healthy capillary flow.
Constant external pressure over 70 mm Hg for 2 hours produces irreversible ischemic changes.
Synonyms : Pressure ulcer, Decubitus ulcer,
Bed sore.

Patient Populations at High Risk
Paraplegic or tetraplegic patients Patients with decreased sensation due to
neurologic disorders, e.g. stroke. Patients with impaired mental capacity. Seriously ill patients in an intensive care unit.
Additional Risk Factors Malnutrition Incontinence Tobacco use.

Areas Prone to the Development of Pressure Sores
More common• Scrum• Trochanter• Ischial
tuberosity
Less common• Calcaneum• Malleolus• Scapula• Elbow• Knee

Patients Admitted with Pressure Sore at CRP on
2007 Total patients : 415 Total patients with pressure sore : 173
(30% of total) Male patients with pressure sore : 157
(27%) Female patients with pressure sore : 16
(3%)
Sex distribution among pressure sore patients on 2007
Female3%
Male27%
Total70%

Pressure Sore Staging System
Stage I : Redness of intact skin that does not blanch.
Stage II : Partial-thickness skin loss involving the epidermis and dermis.
Stage III : Full-thickness skin loss involving the underlying subcutaneous fat but not the muscle.
Stage IV : Full-thickness skin loss with extensive destruction, tissue necrosis, or damage in muscle, bone, or supporting structures.

Treatment of STAGE I and II Pressure Sore
Keep the affected tissue clean and the surrounding area dry by regular daily dressing.
Apply antibiotic ointment (e.g., Bacitracin, silver sulfadiazine) daily to areas that have blistered.

Treatment of STAGE III and IV Pressure Sore
If the wound has a red, granulating base : Apply saline dressing daily.
If the wound contains necrotic tissue : - Surgical debridement is necessary. - Follow with daily dressings, using saline or EUSOL solution.
If the wound is infected : - Treat the patient with a course of
antibiotics. - Twice daily dressing with Betadine solution.

Dressing Materials
Normal Saline Betadine solution EUSOL solution Spirit Betadine ointment

Out come of Regular Wound Dressing
On Admission Two months later

Surgical Intervention
Wound Debridement
Skin Grafting
Plastic surgery

Wound Debridement When a wound is covered with black,
dead tissue or thick gray/green exudates, surgical removal of necrotic tissue is needed.
Dead bone or tendon in the wound must be removed.
Bleeding tissue is a good sign healthy tissue. Dead tissue does not bleed.
Once the necrotic tissue has been removed, regular Wet-to-dry dressing should be started.

Out Come of Debridement and Dressing
Before After

Skin Grafting
Cross-section of human skin showing the epidermis, dermis and subcutaneous tissue.
The relative thickness of skin grafts is shown.

Split-thickness Skin Graft Indications :
• Large wound (> 5–6 cm in diameter) that would take many weeks to heal secondarily.
• Wounds that cannot be closed primarily.• Wounds that require more stable
coverage than scar.
Contraindications :• Malnourished patient.• Necrotic tissue or signs of infection at
the wound• A wound that has exposed tendon or
bone.

Skin-graft (Humby) knife
Harvesting a split-thickness graft with the Humby knife.
Wound covered with a split-thickness skin graft.

Skin Grafting at Sacral Pressure Sore
Preoperative Postoperative
Two months before surgery

Plastic Surgery End to end closure Flaps
Pre requisites of plastic surgery : Excellent nutritional status.
Albumin > 3.5 gm/dl, Prealbumin > 20mg/dl, Transferrin > 250 mg/dl (2.5 gm/L).
The patient must not smoke. Patients should be motivated enough to
change positions regularly.

End to End Closure
Preoperative Postoperative

End to End Closure
PreoperativePostoperative

FLAP A flap is a piece of tissue with a blood
supply that can be used to cover an open wound.
A flap can be created from skin with its underlying subcutaneous tissue, fascia, or muscle.

Random Flaps Circulation to a
random flap is provided in a diffuse fashion through tiny vascular connections from the pedicle into the flap.
The pedicle must be bulky to increase the number of vascular connections.
The flap should not be longer than 3 times its width.
Random skin flap. The blood supply comes diffusely from the remaining skinattachment, which serves as the pedicle.

Different Types of Random Flaps
Rhomboid flap Rotation flap Tensor fascia lata (TFL) flap V-Y advancement flap. Rectangular advancement flap.

Rhomboid Flaps Rhomboid
flaps are useful for wounds up to 6 to 8cm in diameter on the trunk or extremity.
Useful in pressure sores with less surrounding tissue laxity.

Rhomboid Flaps
Preoperative
5th Postoperative day 15th Postoperative day

Rhomboid Flaps
Pre-operative Pre-operative
10th Post-operative day15th Post-operative day

Rhomboid Flaps
Pre-operative
7th Post-operative day One month later

Rhomboid Flaps
Per-operative pictures

Buttocks Rotation Flap Most
commonly used for sacral pressure sore.
Useful for sacral wounds about 10 to 12cm in diameter.

Bilateral Rotation Flap
Pre-operative
Per-operative

Bilateral Rotation Flap
Per-operative pictures

Tensor Fascia Lata (TFL) Flap
TFL flap is the most commonly used for closure of trochanteric pressure sore.
The flap is composed of the skin and fascial extension from the TFL muscle.

Tensor Fascia Lata (TFL) Flap
Pre-operative
Post-operative

Tensor Fascia Lata (TFL) Flap
Pre-operative
Per-operative

Tensor Fascia Lata (TFL) Flap
Per-operative pictures

General Post Operative Care
Cleanse and apply antibiotic ointment to the suture lines daily.
If a suction drain was used, it should stay in place at least 1 week.
The patient should apply no pressure to the surgical site until the suture line has healed (usually 2–3 weeks).
Leave the skin sutures in place for at least 14 days unless there are signs of irritation from the sutures.

Failure of Flap surgery
Ischemic flap necrosis.
Infection.
Haematoma.
Recurrence of pressure sore at surgical site.

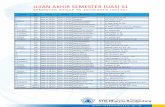
Graphical Presentation of Pressure Sore surgeries from Jan’07 to Apr’08
Skin Grafting
Plastic Surgery
1
9
5
13
5 5
8
20
0
2
4
6
8
10
12
14
16
18
20
Jan'07 - Apr'07 May'07 - Aug'07 Sep'07- Dec'07 Jan'08- Apr'08