Physiology of Coronary Blood Flow
description
Transcript of Physiology of Coronary Blood Flow
Slide 1
Physiology of Coronary Blood FlowDr Sandeep Mohanan,Department of Cardiology,Medical College, Calicut.1OUTLINEIntroductionCoronary microcirculation, resistance beds & autoregulationEndothelium dependent vasodilationCBF during exercisePhysiology of CBF across a stenosisMeasurement of CBFPhysiologic assessment of CAD- noninvasively and invasivelyCoronary collateral circulationCBF abnormalities with normal coronary vessels
INTRODUCTIONThe resting coronary blood flow ~250ml/min (0.8ml/min/g myocardium=5% of COP)
Myocardial oxygen consumption --- balance between supply and demand
According to Ficks principle, oxygen consumption in an organ is equal to the product of regional blood flow and oxygen extraction capacity.
The heart is unique in having a maximal resting O2 extraction (~70-80%)
So, MVO2 = CBF * CaO2
Thus, when systemic oxygenation is stable, the oxygen supply is determined by the coronary blood flow
Adolf Eugene Fick German physician and phsiologist
GREGG effect : Where an increase in coronary blood flow can independently increase the MVO2 (by increasing end-diastolic diameter)
3The coronary blood flow is unique:Helps generate the systole (cardiac output) & simultaneously gets impeded by the systole it generates.
At systole Arterial flow is minimum: directed from the subendocardium to the subepicardium; and the coronary venous outflow is maximumDiastole The coronary inflow is maximum
BASIC PHYSICS OF FLOWBernoullis principleDaniel Bernoulli (Swiss scientist) studied fluid dynamicsand postulated in his book, Hydrodynamica, that for aninviscid flow an increase in the speed of the fluid occurs simultaneously with a decrease inpressureor a decrease in thefluid'spotential energy.
LAW OF CONSERVATION OF ENERGY{Total energy = Kinetic energy + Potential(Pressure) energy}
- May explain in part the increase in flow during diastole
17385Hagen-Poisseuilles equation:-Gives the pressure drop for a viscous liquid( in laminar flow) as it flows through a long cylindrical pipe
-Corresponds to the Ohms law for electrical circuits (V=IR)-Thus halving the radius of the tube increases the resistance by 16 times
Principles were also extended to turbulent flow and helped derived the Darcy-Weisbach equation and the Reynolds number
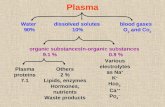
DETERMINANTS OF CORONARY RESISTANCEFlow is determined by the segmental resistance and therefore an understanding of the resistance beds is necessary:3 resistance beds
R1
R2
R3
R2( Microcirculatory resistance) 20- 200mSmall arteries and arteriolesCapillaries: ~ 20% of R2( even if capillary density doubles, perfusion increases by only 10%)
R3( Compressive resistance)- time varying - Increased in heart failure
In the subendocardium R3increases but R2 decreases.So, transmural flow is normally uniform.Broadly 2 compartments of coronary resistance:
1) Epicardial conduit vessels no pressure loss2) Resistance vessels -- < 300m -- gradually dissipating pressure till 20-30 mmHg
Coronary driving pressure = Aortic root pressure LVEDP
The interactions of coronary driving pressure and the coronary resistance are coordinated so as to maintain a constant flow for a given workload.---- CORONARY AUTOREGULATION
CORONARY AUTOREGULATIONMaintenance of a constant regional coronary blood flow over a wide range of coronary arterial pressures when determinants of myocardial oxygen consumption are kept constant.
Below the lower limit: flow becomes pressure dependentUnder optimal circumstances this lower threshold is a mean pressure of 40mmHg.
Sub-endocardial flow compromise: >16Transmural penetrating arteries:
Not influenced by metabolic stimuli.Blood flow driven by coronary driving pressure, flow mediated vasodilation and myogenic regulation.Significantly influences the subendocardial blood flow
MEDIATORS OF CORONARY RESISTANCEPHYSICAL FORCES
METABOLIC MEDIATORS
NEURALCONTROL
PARACRINE FACTORS
Physical forcesThese are intraluminal forces:
Myogenic regulation: Ability of the vascular smooth muscle to oppose changes in coronary arteriolar diameterProbably due to stretch activated L-type Ca channelsPrimarily in > R1
In CAD : R1 > R3 > R2
R1 increases with stenosis severity and impairs flow
Ideal stenosis P-Q relationshipAccording to Bernoullis principle and law of conservation of energy.The total energy = KE + PE; i.e E V2+ PEThe flow across a stenosis (Flow= A * mean velocity)Thus V 1/D2. -Therefore in 50% stenosis, V- 4 times and KE- 16times.- The PE proportionately decreases and is lost as (P) DISTAL PRESSURE LOSSPost stenosis: V comes back to normal Therefore KE decreases to pre-stenosis valuesPE thus becomes (prestenotic PE)- P i.e =Pd
P= Viscous losses + Separation losses + Turbulence
Viscous losses = f1 Q , f1 (Viscous coefficient = 8L/ As2 ) (Hagen-Poiseuille equation)
Separation losses= f2 Q2, f2 (Separation coefficient= /2[1/As-1/An]2 ) - viscosity of blood - density of blood L - length of stenosisAs - CSA of stenotic segmentAn - CSA of normal segment
Flow to distal territory = Pd- venous pressure
Thus the pressure drop across a stenosis varies directly with the length of the stenosis and inversely with fourth power of the diameter.
Therefore overall resistance and thus distal pressure is determined mainly by cross sectional area of the stenosis increases exponentially
Resistance is also flow dependent ( square of flow)Abluminal outward remodelling : No effect on P-Q characteristicsInward remodelling : Significant longitudinal pressure drop
Instantaneous resistance increases during vasodilation43
MEASUREMENT OF CORONARY BLOOD FLOWEarlier microsphere radionuclide techniques were considered gold standard.Presently, regional myocardial blood flow can be quantitated non-invasively equally accurately using MRI, CT and PET.Resting CBF 0.7-1ml/min/gHowever a resting CBF gives little information This may be normal in HCM, CAD, DCMP etc due to inherent adjusting mechanisms.It is the CBF in a stressed heart that brings out the true quality of the coronary vasculature.
STRESS Pharmacological / Physiological
Noninvasive flow measurementsMRI, Doppler echo and Dynamic PET (Nuclear Perfusion studies)Require measurements of the myocardial tissue tracer concentrations and its kinetics.
Vasodilator stress:- Adenosine 140g/kg/min for 4 min( Dypiridamole 560g/kg/min)Induces hyperemia and makes CBF dependent on driving pressure and the residual resistance3 to 5 times flow (2-4ml/min/g)Exposes the minimum coronary vascular resistance of the system
Noninvasive methods may measure either the relative flow (compared to normal regions)or the absolute flow
The concept of Coronary flow reserve pioneered by Lance Gould is central to the functional assessment of CBF across a stenosis.
FUNCTIONAL ASSESSMENT OF CAD - NoninvasiveLance Gould-relationship b/w the anatomic severity of a stenosis and flow resistance47Coronary reserve : Ability to increase CBF above resting value by maximum pharmacologic vasodilation (4 to 5 fold)
Parameters that may affect CFR:
- HR- preload - afterload- contractility- systemic oxygen supply
Flow in the maximally vasodilated heart is pressure dependent.Thus CFR indirectly shows the consistency of the driving coronary pressure uptill the distal territory
Relative Flow Reserve = Regional perfusion of a segment/ Perfusion in normal segment during maximal pharmacological vasodilation/exercise
Compares under same hemodynamic conditionsIndependent of HR and MAPMore lesion specific than the AFR --- correlates with FFR
Limitations:- Requires a normal reference segment--- ? Diffuse CADLow sensitivity requires relatively large differences in regional flowThe uptake of nuclear tracers may not be proportionate in both regionsNot much prognostic data available
Absolute Flow Reserve = Maximal vasodilated flow in a region of interest/ Resting flow of same region. - Normal AFR ~ 4-5Clinically significant impairment if 0.8 best outcomes were attained with OMT alone. IVUS vs FFR comparisonIVUS- best anatomical information of a lesionFFR- best physiological information of a lesionOne cannot be a substitute for the other for in-depth assessment of complex lesionsTakagi et al demonstrated that an IVUS minimal lumen area 0.25 have a better prognosis
-Collateral resistance is tonically regulated by NO and prostaglandins
ABNORMAL CBF WITH NORMAL CORONARY ARTERIESMICROCIRCULATORY IMPAIRMENT As discussed earlier the CFR decreases with 1)Tachycardia (decreased diastolic time),2) Increased preload ( compressive determinants)3) Increased afterload4) Increased contractility5) Decreased Oxygen supply ( anaemia, hypoxia)6) Abnormal endothelium (DM, HTN, DLP, CTDs)
CONDUIT VESSEL DYSFUNCTION: - A longitudinal perfusion gradient develops from base to apex ( Base flows ~ 20% more than apex)
- Endothelial dysfunction, Vessel stiffness, Outward vascular remodelling and diffuse luminal narrowing
ANGINA with NORMAL CORONARIES
Risk factor reduction has been found to significantly improve the CFR in several studies
Thank you
1) The oxygen extraction ratio of the myocardium is :100%90%80-90%70-80%60-70%Multiple Choice Questions2) A 75% simple stenosis in a coronary blood vessel would increase the flow resistance by:a) 24 timesb) 48 timesc) 64 timesd) 128 timese) 256 times3) Subepicardial coronary flow becomes compromised at coronary pressures less than:20mmHg25mmHg30mmHg35mmHg40mmHg
4)Microcirculatory vasodilation in response to increased flow requirements chiefly occur at vessels:a)400micme) Similar contributions at all levels 5) One of the following mediator has a significant endothelium independent vasodilatory effect on normal coronary vasculature:a)Bradykininb) Cholinergic innervationc) ADPd) Adenosinee) Thrombin6) The Hagen-Poiseuille equation focuses on the effect of:
Pressure conservation as total energy is conservedTotal pressure lost as potential energyPressure drop due to viscous losses Pressure drop due to separation lossesPressure drop due to turbulence losses7) Flow to the distal territory of a stenosis is determined by:Pa-PdPa-PvPd-PvPa onlyPv only8)Main advantage of FFR over AFR in physiological assessment of CAD is:It gives anatomical data as well as physiological dataIt correlates better with the severity of CADIt has a better prognostic valueIt is lesion specificIt provides information on microcirculation also9) FAME 2 strategy (conclusion) in managing a epicardial lesion in CSA patients is
a) PTCA to patients with >70% stenosis improves mortality
b) PTCA based on FFR values has a mortality benefit compared to that based on angiographic criteria alone.
c) PTCA based on FFR values decreases urgent revascularisation compared to based on angio criteria alone
d) PTCA by FFR guided vs angio-criteria alone showed no significant differences10) Based on available data, the best results following POBA and PTCA based on FFR criteria are when they are respectively greater than:o.75 and 0.900.90 and 0.940.94 and 0.900.90 and 0.750.75 each