Parkinson’s Disease as ... - Wellness Pharmacy · posthumous, the key features being neuron death...
Transcript of Parkinson’s Disease as ... - Wellness Pharmacy · posthumous, the key features being neuron death...

Page 502 Alternative Medicine Review ◆ Volume 5 Number 6 ◆ 2000
Parris Kidd, PhD (Cell biology, University of California at Berkeley) – Contributing Editor, Alternative Medicine Review;Health educator and biomedical consultant to the supplement industry. Correspondence address: 847 Elm St, El Cerrito,CA 94530
Parkinson’s Disease as MultifactorialOxidative Neurodegeneration: Implications
for Integrative ManagementParris M. Kidd, PhD
IntroductionParkinson’s disease (PD) is the most common disease of motor system degeneration and,
after Alzheimer’s disease, the second most common neurodegenerative disease.1 Parkinson’s dis-ease takes a heavy toll in mental anguish, lost productivity, and health care expenditures. PD promi-nently features dopamine transmitter insufficiency, and current management is almost exclusivelyreliant on dopamine replacement drugs. But, while these drugs are initially effective in most pa-tients, they do not slow the underlying degeneration in the area of the brain most affected, thesubstantia nigra (SN). Their effectiveness declines over time and their adverse effects become in-creasingly more troublesome. Broader options for long-term management are urgently needed.
AbstractParkinson’s disease (PD) is the most common movement pathology, severely afflictingdopaminergic neurons within the substantia nigra (SN) along with non-dopaminergic,extra-nigral projection bundles that control circuits for sensory, associative, premotor,and motor pathways. Clinical, experimental, microanatomic, and biochemical evidencesuggests PD involves multifactorial, oxidative neurodegeneration, and that levodopatherapy adds to the oxidative burden. The SN is uniquely vulnerable to oxidative damage,having a high content of oxidizable dopamine, neuromelanin, polyunsaturated fattyacids, and iron, and relatively low antioxidant complement with high metabolic rate.Oxidative phosphorylation abnormalities impair energetics in the SN mitochondria, alsointensifying oxygen free radical generation. These pro-oxidative factors combine withinthe SN dopaminergic neurons to create extreme vulnerability to oxidative challenge.Epidemiologic studies and long-term tracking of victims of MPTP (1-methyl-4-phenyl-1,2,3,6,-tetrahydropyridine) poisoning, suggest oxidative stress compounded byexogenous toxins may trigger the neurodegenerative progression of PD. Rational,integrative management of PD requires: (1) dietary revision, especially to lower calories;(2) rebalancing of essential fatty acid intake away from pro-inflammatory and towardanti-inflammatory prostaglandins; (3) aggressive repletion of glutathione and othernutrient antioxidants and cofactors; (4) energy nutrients acetyl L-carnitine, coenzymeQ10, NADH, and the membrane phospholipid phosphatidylserine (PS); (5) chelationas necessary for heavy metals; and (6) liver P450 detoxification support.(Altern Med Rev 2000;5(6):502-545)
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 503
Many different lines of evidence haveconverged to suggest PD is primarily an oxi-dative disease, fueled by endogenous suscep-tibility and driven by the cumulative contribu-tions of endogenous and exogenous (environ-mental) oxidant stressors. In this review theevidence for the various oxidative contribu-tions to PD is critiqued, from the perspectiveof developing a more effective and necessar-ily more integrative strategy for its medicalmanagement.
A Disease of ProgressiveNeurodegeneration
Parkinson’s disease was first describedin 1817 by the physician James Parkinson.2
Prior to this, accounts of the symptoms wereremarkably scarce, which led many research-ers to theorize whether this disease may havebeen a product of the beginning of the early19th century and the Industrial Revolution in
England.1 Some speculated that, because cer-tain environmental neurotoxins causeParkinson’s-like (“parkinsonian”) symptoms,some contaminant in the new industrial envi-ronment may have increased its prevalence.This debate has continued to the present, withthe evidence steadily accumulating in favor ofoxidative causation linked to environmentaltoxins.
Parkinson’s disease is widespread inWesternized countries. In the United States,for example, as many as one million peoplehave PD with more than 50,000 new casesbeing diagnosed each year.1 The disease ishighly age-dependent: it can manifest as earlyas the mid-30s, but becomes more commonpast the age of 50, with 57 being the averageage of diagnosis in the United States. Its preva-lence in the over-50s U.S. population is aboveone percent, and in the over-80 populationlikely exceeds five percent.3 PD is becoming
endocrinesystem
diffuseprojections
visual
auditory
somatosensoryInput
vicerosensoryinput
visceromotoroutput
somatomotoroutput
primary sens.fields
secondarysensory fields
sensoryassociation areas
prefrontalassociation areas
premotorfields
primarymotor field
thalamus limbic loop centers striatal loop centers cereb. loop centers
hypothalamus
periaqued grayparabrach. nucl. diff. project
non-thal. nucl.
bulbar and spinalautonomic nuclei
s. nigra
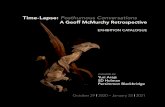
Figure 1: The Pervasive Brain Circuit Involvement of Parkinson’s Disease.Darkened areas are those damaged by the disease. From Braak and Braak.4
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 504 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
more common with the overall aging of popu-lations.
Parkinson’s disease often first becomesnoticeable as tremor in a limb, and as itprogresses three other unmistakable symptomsarise:1-3 bradykinesia (slowness of movement);rigidity (both “cogwheel”/jerkiness and “lead-pipe”/stiffness); and posture instability withimpaired gait, associated with the stoopedstance characteristic of the disease. Bradyki-nesia may cause the patient to feel glued tothe ground or to the chair in which they sit,and progressively erases body language andfacial expressiveness. The disease is not re-stricted to motor degeneration — as many as35 percent of PD cases also develop demen-tia.5
Parkinson’s disease is now recognizedto be a widespread degenerative illness thataffects not just the central nervous system, butalso the peripheral and enteric systems.4 For-merly the disease was typecast as motor sys-tem degeneration, yet sensory fields, associa-tion areas, and premotor fields become dam-aged throughout the brain (Figure 1). The lim-bic, autonomic, and neurosecretory controlfields (hypothalamus) all show micro-ana-tomic damage. At the cellular level, neurondeath in PD is more systemic than previouslyassumed: non-invasive imaging recently dem-onstrated that the nerve supply to the heartdegenerates in PD subjects.6 Biochemically,abnormalities of liver detoxification and mi-tochondrial oxidative phosphorylation alsooccur.7,8
The pathological process that under-lies PD typically is slow-paced but relentlesslyprogressive, the clinical symptoms tending tomanifest relatively late in the pathological pro-gression. Classically, the hallmark of PD hasbeen degeneration of dopamine-producingneurons in the relatively small SN, most in-tensely localized in the zona compacta. Thedefinitive Parkinson’s disease diagnosis is stillposthumous, the key features being neurondeath in the SN accompanied by the presence
of Lewy bodies and Lewy neurites.9
Normally, dopamine produced in theSN is moved to the caudate nucleus and theputamen, where it is involved in stimulatingand coordinating the body’s motor movements.In PD, neurons producing dopamine in the SNdie, reducing the overall supply of dopamineand compromising the brain’s capacity to ef-fectuate movement. Curiously, dopamine-pro-ducing neurons outside of the SN tend not tobe affected, though many other neuronal types— glutamatergic, cholinergic, tryptaminergic,GABAergic, noradrenergic, adrenergic —show “grievous cytoskeletal damage,” accord-ing to Braak and Braak.4
The characteristic pattern of nerve celldestruction in SN neurons appears to be linkedto abnormalities that develop in the cytoskel-eton. The pathognostic Lewy bodies and Lewyneurites are composed mainly of abnormalcytoskeletal neurofilament proteins.3,4 Neuronsafflicted with Lewy formations remain viablefor a relatively long period, but are function-ally compromised and die prematurely. As arule, projection neurons with long axons aremore vulnerable than local circuit and projec-tion neurons with short axons, which tend tobe spared.4
Current Management ofParkinson’s Disease
Parkinsonism is a term broadly appliedto the subject presenting with movement im-paired by rigidity, tremor, or extreme slowness(bradykinesia).1 Parkinsonism can have vari-ous causes (Table 1): occupational exposureto manganese;1 trauma to the brain;9 viral in-flammation of the brain, as with Encephalitislethargica which struck five million victimsduring the years 1916-1926;11 and exposuresto toxins still unknown, such as that which hasafflicted citizens of Guam.12 The diagnosis ofParkinson’s disease is reserved for cases con-firmed by selective cell death in the SN.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 505
Currently, PD is managed mainlythrough dopamine replacement therapy —pharmaceutical agents aimed at replacingdopamine in the brain or mimicking its actionsat dopamine receptors.9 Most commonly usedis the dopamine precursor levodopa in combi-nation with carbidopa (Sinemet® and SinemetCR). The vast majority of patients experiencebenefits initially, but rarely do the benefitspersist. Typically, after 2-5 years on levodopadrugs the patient’s responses become erratic.Nausea is a constant threat, and dyskinesiasdevelop that feature excessive and uncontrol-lable movements. Other adverse effects de-velop: mental confusion, “freezing” and inabil-ity to move, dystonia, low blood pressure epi-sodes, sleep disturbances, and hallucinations.1,9
Adverse side effects usually pose amajor ongoing challenge to the PD patient.10
For example, the combined effects of the dis-ease and the drugs used to treat it produce sleepproblems in an estimated 70 percent of patientsand daytime hallucinations in about 30 per-cent. Levodopa is usually effective for motorsymptoms at the beginning, but over time tendsto cause motor fluctuations, dyskinesias, andother adverse side effects. These can becomeso disabling that surgical treatment becomesthe only apparent option for restoring any qual-ity of life.13
Other drugs used for PD symptommanagement include amantadine(Symmetrel®), selegiline (Eldepryl®,deprenyl), dopamine agonists (bromocriptine,pergolide, pramipexole, ropinirole), and sev-eral anticholinergic drugs. All these have ma-jor adverse effects and generally are less ef-fective than Sinemet® in suppressing symp-toms. Tolcapone, an inhibitor of COMT (cat-echol-O-methyltransferase, the enzyme whichnormally inactivates dopamine), became avail-able in 1998. It caused several deaths from liverfailure.1 Another COMT inhibitor —entacapone — was released in 1999 which wasnot liver-toxic but still caused dyskinesias,nausea, diarrhea, abdominal pain, and urinediscoloration.1
As PD progresses, in addition to theadverse effects accruing from levodopatherapy the ever-worsening loss of dopamineneurons causes progressively crippling dam-age to motor control circuits throughout thebrain.4 The control may shift, so the pathwaysthat normally inhibit movement come to domi-nate those that activate movement. The increas-ing desperation of the patient can become therationale for risky surgical intervention; forexample, whether to remove inhibitory zonesor to implant electrodes aimed at restoring ahealthy balance of circuits.13-15
Antihypertensive, diuretic: Diupres, Enduronyl, Hydropres, Regroton,Demi-Regroton, Salutensin, Ser-Ap-Es
Antihypertensive, non-diuretic: Aldomet
Antidepressant: Asendin, Aventyl/Pamelor, Desyrel, Elavil, Limbitrol,Ludiomil, Luvox, Norpramin, Paxil, Prozac, Sinequan, Tofranil,Triavil, Wellbutrin, Zoloft
Antipsychotic: Compazine, Haldol, Mellaril, Navane, Prolixin,Risperdal, Stelazine, Thorazine, Triavil, Zyprexa
Other: Reglan, Zyban
Table 1: Classes of Prescription Drugs that can PrecipitateParkinsonian Symptoms. From Worst Pills, Best Pills.10
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 506 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
Surgical destruction of brain tissue wastried prior to the advent of levodopa therapy,but produced inconsistent results. More re-cently, microelectrodes are being used to de-tect signals from individual brain cells, usingthese signals as “signposts” to arrive at moreprecise locations in the brain.13 Pallidal andsubthalamic nuclear surgery can improve mo-tor symptoms and levodopa-induceddyskinesias, but only unilateral pallidotomy isacceptable since the bilateral procedure car-ries unacceptably high risk. The unilateral pro-cedure, however, probably the most commonsurgery for advanced PD, unfortunately doesnot allow for postoperative reduction inlevodopa doses. Postsurgical mortality is 1-1.8percent, risk of permanent neurological defi-cit is about five percent, and benefits tend todissipate within 1-4 years.
Deep-brain electrical stimulation(DBS) by way of surgically implanted elec-trodes has the advantages over ablation of be-ing regulatable and reversible. DBS also hasbeen bilaterally performed in many patientswith marked benefit and little permanent mor-bidity.14,15 DBS post-operative morbidity andmortality is less than for ablation, and thestimulation side effects are relatively mild.15
On the negative side, infection may ensue,mechanical failure occurs in 3-4 percent ofcases, batteries must be replaced at regularintervals, and the device is expensive. On thepositive side, successful bilateral stimulationcan allow medication dosing to be reduced,providing the patients a better quality of life.Although results from randomized studies arenot yet available, surgeons who have done bothablation and DBS agree that DBS is better forthe patient.
Obviously, the need to broaden theoptions for therapy in Parkinson’s disease isurgent. This urgency compels renewed focuson the etiology and pathogenesis of the disease.Deeper scientific understanding of PD wouldlead to better preclinical detection andprophylaxis, validation of biomarkers,
confirmation of genetic and environmental riskfactors, and more prolonged symptom controlwith fewer adverse effects.
A Broad Spectrum of PotentialEtiologic Factors
As with almost all disease states, abroad spectrum of both genetic and environ-mental factors have been suggested as contrib-uting to the initiation and progression of PD.Aging is also implicated, with advanced agebeing the single most important risk factor forthe disease.
Role of AgingParkinson’s disease is clearly age-de-
pendent. Several of the neurodegenerative syn-dromes documented in the elderly— gait slow-ing, for example — resemble those seen in PDand may be prodromal for the disease.3 Whilethe inexorable downhill slide of Parkinson’sdisease is unmistakably a disease process, ag-ing undoubtedly contributes to PD progres-sion, perhaps because of its accumulative oxi-dative damage and steady decrease of antioxi-dant capacity.
Heritability and GeneticSusceptibilities
There appears to be an inherited com-ponent to PD, and a number of family pedi-grees with multiple cases of PD have beenextensively studied.16,17 To date, seven loci onfour chromosomes are reliably linked to PDand/or to neurodegeneration of the parkinso-nian type, not always with the presence of theLewy structures. The protein products fromtwo of these loci are linked to nerve cell dam-age in other neurodegenerative conditions.Alpha-synuclein, localized to chromosome 4,is a major component of the Lewy bodies, notjust in PD but also in dementia with Lewy bod-ies and in the Lewy body variant ofAlzheimer’s disease.16 Non-familial PD sub-jects carrying a specific alpha-synuclein allele
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 507
and ApoE4, a high-risk allele for Alzheimer’s,have a 13-fold increased risk of developing PD.Parkin, localized to chromosome 6, causesearly-onset parkinsonism without the Lewybodies that define PD.16 Most PD cases, how-ever, do not have other affected family mem-bers and have no apparent familial contribu-tion.
One particularly good test system withwhich to quantify disease heritability is a twinstudy, in which disease frequency is comparedbetween cohorts of identical twins and frater-nal twins. If genetic factors are important, con-cordance in monozygous (MZ) twins, who are100-percent genetically identical, will begreater than in dizygous twins, who are only50-percent genetically identical. Tanner and ateam of associates did such a twin study.18
Drawing from the U.S. World War IIVeteran Twins Registry, Tanner’s group com-piled a pool of 19,842 white male twins. Afterexhaustive screenings and a series of in-depthdiagnostic examinations, they confirmed 193twins with PD among 172 twin pairs. Theyconfirmed mono- vs. di-zygosity using poly-merase chain reaction analysis of DNA. Forthe entire sample as a whole, with average ageof onset of 64.5 years, there was no signifi-cantly greater concordance of the disease be-tween identical twins than between fraternaltwins, indicating no genetic linkage to PD. Incontrast, for those who developed the diseaseearlier than age 50, further data analysis dis-closed there was greater genetic concordancein the MZ twins. For this group, which repre-sents 10-15 percent of the total PD cases, ge-netic linkage was not ruled out.18
With the key studies now done, thepreponderance of the evidence indicates thegeneral PD population has no more than a mildgenetic contribution. Still, overall absence ofdefined heritability does not necessarily ruleout subpopulations with higher heritability, orsubtle genetically-conditioned vulnerabilities.Rohan de Silva et al16 and Reiss et al17 discusshow various specific gene mutations and
deletions might potentially contribute to PD.The genes involved could act with varyingdegrees of penetrance, or polygenicallycontribute to disease vulnerability with nosingle gene being wholly responsible. Thoughbetter designed and more definitive than thosethat preceded it, the outcome of the Tannerstudy still leaves open possibilities in theseareas. For early-onset PD, the cumulativeevidence is consistent with a strong heritabilitycomponent (at least in white males, the onlygroup studied to date).7,16,17
Some individuals with PD have im-paired liver detoxification. The P450 IID6 en-zyme, which was characterized based on itscapacity to metabolize debrisoquine, wasfound to be dysfunctional more frequently inPD subjects than in non-PD controls.7 Of thePD subjects, those with very early onset (<age 40) were most likely to have this prob-lem. The gene for P450 IID6 was localized tochromosome 22, and efforts are underway todevelop it into a biomarker for early-onset PD,but this may not prove practical. Conductingsuch assays in vivo is expensive and labori-ous, and in the studies some of the medica-tions being taken for PD may have compli-cated the outcomes.
Interestingly, P450 IID6 is present inthe nigrostriatal system and the notorious par-kinsonian toxin, 1-methyl, 4-phenyl, 1,2,3,6-tetrahydropyridine (MPTP) is a substrate forthis complex.7 MPTP came to the forefront ofPD research in 1982, when drug addicts innorthern California began to develop severeparkinsonism after intravenous injection of asynthetic heroin that was contaminated withMPTP as a byproduct of its synthesis.19
Environmental Contributors,Especially Toxins
The MPTP poisonings led to a seren-dipitous finding: that the symptoms resultingfrom exposure to MPTP very closely matchedthe many features of PD.19-21 This shifted the
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 508 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
focus toward environmental factors as poten-tial PD initiators or contributors. As the searchprogresses, a single toxic cause remains elu-sive but a role for environmental factors seemsalmost certain.
Whatever the exact degree ofcontribution from environmental toxins,currently the cumulative evidence suggests PDis a multifactorial oxidative disease. The maincausal, oxidative contributors indicted to dateare: (1) measurable amplification of theendogenous oxidative load by constitutiveimpairments of mitochondrial energytransformations; (2) innate vulnerability of thebrain’s substantia nigra region to oxidativechallenge; and (3) initiation or promotion bytoxic exposure(s) that further depleteantioxidants. These factors combine to initiatea downhill course for the neurons of the SNand elsewhere in the brain, the end result ofwhich appears to be a slow-acting yet long-term progressing, inflammatory process. Thiseventually results in the micro-anatomicdegeneration and clinical symptomatologies ofParkinson’s disease.
Mitochondrial Energetics GenerateEndogenous Oxidative Burden
All the body’s cells, like oxygen-utilizing cells anywhere, generate life energyand simultaneously generate oxygen freeradicals (oxyradicals). The resultant oxidativeburden is an obligatory, unavoidable byproductof oxygen-based (aerobic) respiration. Veryearly in the progression of life, the adoptionof oxygen to drive energetics produced ahigher energy yield from food molecules, butwith a “downside.” This downside was theproduction of oxyradicals, so highly reactivethey have the potential to destroy the livingsystem.22 Antioxidant defenses developed,which curb the toxic threat from oxyradicalsand help keep them integrated with the myriadpathways of healthy metabolism.23 The majorcellular “hot spots,” where the bulk ofoxyradicals are produced and antioxidant
defenses are normally most challenged, are thesemi-independent organelles calledmitochondria.
Present in all human cells, the mito-chondria are the cells’ energy powerhousessince they generate the vast bulk of the ATPthat drives life processes.23 The mitochondriahave their own DNA and manage the oxida-tive phosphorylation process (“oxphos”). Inthis process carbon-carbon double bonds aresplit to create pairs of energized electrons,whose electronic energy is then converted intothe chemical bond energy of ATP. As the mi-tochondria utilize 90 percent or more of thecells’ available oxygen to make ATP, they alsogenerate 90 percent or more of the oxyradicalsthat make up the endogenous oxidative bur-den.24
The mitochondrial electron transfercomplexes use highly electrophilic molecularoxygen to create an electronic potential gradi-ent which “pulls” electrons through a seriesof five cytochrome-protein complexes. Thecomplexes sequentially extract the electrons’energy, converting it to ATP (Figure 2); at theend the electrons are combined with hydro-gen and oxygen to make water. However, dur-ing the transfers single electrons escape enzy-matic control; these combine with oxygen tocreate oxygen free radicals, at a rate of aroundtwo percent of all oxygen consumed. To pro-tect against destruction by this flux ofoxyradicals, the mitochondria have sophisti-cated antioxidant defenses; but inevitably a fewoxyradicals slip through to attackbiomolecules. In PD this electron leakage isabnormally accentuated.25
Flawed Energetics CharacterizesParkinson’s Disease
Parkinson’s disease subjects have beenfound to have abnormalities of oxidative phos-phorylation that impair their mitochondrialenergy generation and almost surely increasetheir endogenous oxidative burden. Researchinto mitochondrial energetics in PD was
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 509
sparked by the observation that the notoriousMPTP targets the mitochondria and inhibitstheir energetic function.25 It is now clear thatPD patients have mitochondrial energetic im-pairment which closely resembles that attrib-utable to MPTP but is apparently constitutivein origin.26-29
The oxidative phosphorylationcomplexes are aggregates of enzymes,functionally linked and distributed in groupsthroughout the inner membranes of themitochondria (Figure 2). The complexes I, II,III, IV, and V occur in spatial sequences thatoptimize electron transfer efficiency whileminimizing the possibilities for single-electron“leakage” to oxygen that would generateoxyradicals.25 The system is finely balanced:damage to any one complex both reduces ATPyield and worsens the inevitable leakage ofoxyradicals from the system.
Schapira and coworkers8 were the firstto report that mitochondrial complex I activ-ity was selectively reduced in the SN of pa-tients with PD, and subsequently this was con-firmed by others.26-29 Haas et al26 found thisabnormality was not confined to the brain:using platelets purified from early-stage pa-tients not on medication for PD, they docu-mented abnormalities of complex I and possi-bly also complexes II and III in their mitochon-dria. The complex I impairment ranged from16-54 percent, and was worse in more ad-vanced cases of the disease. Complex I abnor-malities were also described from non-nigralbrain areas, muscle, and fibroblasts of PD sub-jects, but whether these really exist is still be-ing debated.25,27
In metabolically extreme situations, asfrom exposure to hypoxia, hyperoxia, or meta-bolic poisons, the mitochondrial complexes
Figure 2: The Mitochondrial Electron Transport Complexes. Note CoQshuttling within the inner membrane between complexes I and III. FromReichmann and Janetsky.25
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 510 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
can be shut down and the cell soon dies.25
Complex I is especially sensitive to MPTP,21
and, as mentioned above, is the same complexfound to be hypofunctional in PD patients.8,26,27
Complex I (NADH:ubiquinone oxidoreduc-tase) serves as the principal entry point forelectrons into the enzymatic transport chain.Like most other mitochondrial proteins, com-plex I is genetically coded for by the ring-shaped DNA of the mitochondrion. To helpdetermine whether complex I is geneticallyabnormal, Swerdlow and colleagues27 devisedan experiment using “cybrids.”
Swerdlow’s group first produced acultured line of human neuroblastoma cellsthat contained no mitochondrial DNA. Thenthey repopulated these cells with mitochondriaprepared from the platelets of PD patients orhealthy control subjects. This created matchedpopulations of cybrids in which the cytoplasmwas commonly shared, but the mitochondrialDNA came either from PD mitochondria orfrom non-PD (control) mitochondria. Usingthis elegant means for comparison, they couldconfirm that the PD mitochondria were at least20-percent less efficient in complex I activity,produced higher levels of oxygen free radicals,and rendered their host cells more susceptibleto MPTP-induced cell death. They suggestedthe complex I defect was based in themitochondrial DNA of the PD patient. Suchgene damage could come from parentalinheritance or from oxidative attack upon themitochondria. Whatever the primary source ofthe mitochondrial genic damage, enhancedcomplex I vulnerability (and perhaps damageto other complexes28) helps explain why someindividuals develop PD following toxinexposure, while others do not.
Following on MPTP’s emergence in1982, intensive study of its action mechanismsrendered it an experimental model for exog-enous oxidant toxins and yielded valuable in-sights on PD.19-21,25,28,29 Technically, MPTP isa “protoxin.” It is not toxic by itself but onceit enters the brain becomes biotransformed to
the toxic product MPP+ (1-methyl-4-phenyl-pyridinium) by the enzyme monoamine oxi-dase B (MAO-B).19,20 MPP+ is a highly reac-tive free radical oxidant that is selectively takenup by the dopamine neurons of the substantianigra, then once inside the neurons is selec-tively taken up by their mitochondria.21 Withinthe mitochondrion MPP+ readily inhibits com-plex I of the oxphos apparatus;25 also inhib-ited may be the enzyme alpha-ketoglutaratedehydrogenase, which is located near complexI and also involved in energetics.28,29
MPP+ infiltration of the cells’mitochondria, consequent to MPTP exposure,creates an alarming cellular scenario: extremeimpairment of mitochondrial energyproduction for the cell, accompanied byamplification of oxygen radical production.Most likely a vicious cycle develops, whereinlowered energy production by themitochondria heightens oxyradical formation,which causes oxidative damage, furtherlowering energy production until the cell dies.In an afflicted human progressing towardclinical expression of Parkinson’s disease, thisprocess takes years; MPTP producesparkinsonian symptoms within just days.
Substantia Nigra Vulnerable toOxidative Stress
Oxidative stress exists when the oxi-dative burden on a living system is so greatthat effective antioxidant defenses cannot bemaintained.22,23 Intensified oxidative burden —arising from increased endogenous productionof oxyradicals and/or from excessive exposureto exogenous oxidative agents — threatens toshift the finely balanced oxidation-reductionstate away from reduction and towards oxida-tion. If sufficiently sustained, oxidative stresscan impose lasting oxidative imbalance on theliving system, hastening its demise.30
The brain carries a high endogenousoxidative burden. First, by having myelinsheaths the neurons are particularly enriched
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 511
in polyunsaturated lipids. Due to their highdensity of carbon-carbon double bonds, theselipids are prime targets for oxidative attack.22
Second, the brain consumes a disproportion-ately high share of the body’s oxygen intake,creating a correspondingly high flux of endog-enous oxyradical formation. Third, the activi-ties of the antioxidant enzymes catalase andperoxidase are abnormally low in the brain.The superoxide dismutase enzymes are active,acquiring superoxide oxyradical as it leaks outof the mitochondrial complexes and convert-ing it to hydrogen peroxide (H
2O
2). But in the
virtual absence of catalase and peroxidase,which normally would detoxify these perox-ide products, the burden for detoxifying H
2O
2is shunted onto the glutathione peroxidaseenzyme. This enzyme uses glutathione (GSH)as its essential cofactor, and when it isadaptively induced the brain’s GSH reservesare likely rendered more prone to depletionfrom oxidative attack.30 Multiple studies con-firm that the brain’s substantia nigra region isabnormally depleted of GSH in PD patients.31-34
The substantia nigra’s unique bio-chemistry renders it even more vulnerable tooxidative stress than the brain as a whole. Itsunique biochemical features are:
(1) A high content of dopamine, con-sequent to the high density of dopaminergicneurons in the SN. Dopamine has a strong ten-dency to spontaneously break down into oxi-dant metabolites by “auto-oxidation;” mostreactive among these auto-metabolites are 6-hydroxydopamine quinone and dopamineaminochrome.35 Dopamine’s oxidative break-down also can be accelerated by free (ionized)iron or by other redox-active elements such ascopper, zinc, or manganese.37
(2) An extremely high content of iron,higher even than in the liver,34,36,37 and mostconcentrated in the SN’s zona compacta whichbecomes most damaged in PD.36 It has beensuggested that when iron reaches such highconcentrations in cells it can escape buffer con-trol by ferritin and the other iron-binding pro-teins.37 It could then (via the Fenton reaction)catalytically convert hydrogen peroxide to
• Mitochondrial abnormalities, linked to heightened oxyradical production25
• Substantial (40%) to marked (90%-plus) depletion of GSH (glutathione, glutathione reduced)32,33,37
• Degree of GSH depletion correlates with severity of neuron loss and with disease severity33,34
• Elevated lipid peroxides, hydroperoxides, and malondialdehyde, and decreased polyunsaturated fatty acids40,42
• Increased SOD (superoxide dismutase) activity, generating elevated hydrogen peroxide in absence of elevated peroxidases to detoxify it43
• Increased oxidative damage to DNA and proteins40,41,44
Table 2: Indications of Oxidative Stress in the Substantia Nigra ofParkinson’s Disease Patients.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 512 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
generate the highly reactive hydroxyl radical,which can damage DNA and all other classesof biomolecules.22,35,36 Substantia nigra ironlevels measure even higher in patients withadvanced disease.36
The protein alpha-synuclein, normallya presynaptic constituent, in its aggregatedform is a prominent component of the Lewyaggregates that develop in the SN ofParkinson’s patients.4 Experimentally, ionizediron, in addition to copper and zinc, will cata-lyze its transformation into aggregates.38 Cop-per is sometimes elevated in the cerebrospinalfluid of advanced PD patients, but its in vivorelationship (if any) with alpha-synuclein ag-gregation is not yet apparent.
(3) High activities of the two mono-amine oxidase enzymes (MAO-A and B),which normally function to degrade dopam-ine to products that include hydrogen perox-ide. MAO-B activity increases with aging.39
(4) High content of melanin (dopam-ine-melanin).37,39 This complex macromolecu-lar material can be formed from the auto-oxi-dation of dopamine. Its normal function ap-pears to be the scavenging of free radicals. Butwhen infiltrated with high levels of ionizediron, it can drive the Fenton reaction and ex-acerbate the conversion of endogenous hydro-gen peroxide to the potent hydroxyl radical.37
The population of melanin-enriched, dopa-minergic neurons found in the SN’s zona com-pacta are the worst affected in PD. Melaninwithin the SN could act as a support matrixupon which ionized iron would catalyzeoxyradical generation from available hydro-gen peroxide or from neuromelanin itself.39
(5) Low GSH content relative to otherbrain areas.32-34,37 In animal and cell-level ex-periments, depletion of nigrostriatal GSH en-hanced sensitivity to oxidants and to complexI impairment. GSH depletion seemingly oc-curs early in the disease pathogenesis, so itmay be a central factor in the process.37,40
Techniques are available to detect andquantify oxidative stress in vivo. Table 2 shows
that many of the universally accepted oxida-tive stress indicators are significantly abnor-mal in the SN of the Parkinson’s patient.
The substantia nigra, and particularlyits zona compacta, carries so many pro-oxi-dant biochemical risk factors it could well bean oxidative “accident waiting to happen.” Onesuch accident could be Parkinson’s disease,provoked by oxidant insult from outside theSN.40
Glutathione Depletion Pivotal inParkinson’s Disease
Environmental agents implicated in theetiology of PD include pesticides, oxidant tran-sition and heavy metals (iron, copper, zinc,manganese, mercury, lead, aluminum), andcertain food-borne toxic agents, all of whichcan readily be categorized as oxidative stres-sor agents. What all these diverse agents havein common is their capacity to challenge thefragile antioxidant status of the SN and de-plete its GSH content. The evidence stronglysuggests glutathione depletion is the pivotalevent in Parkinson’s etiology.
Glutathione is a potent molecular anti-oxidant, a conjugation cofactor for the liverP450 system, and an essential cofactor for theglutathione peroxidase family of antioxidantenzymes.23,33,37 GSH also plays higher-levelroles in metabolism: anti-inflammatory, anti-toxin, and metabolic regulator.31 Its levels arehomeostatically maintained inside the livingcell, where the self-adjusting mechanisms formaintaining GSH are numerous. GSH levelsmay well be a life gauge: that is, for as long asits levels are maintained the living cell ishealthy and functional, and once it is severelydepleted the cell is destined to die.31,45
Evidence is growing that GSH deple-tion contributes to neurodegenerative diseases.In numerous animal models of GSH depletion,the blockage at birth of the animal’s capacityfor GSH synthesis distorts brain development.In young or adult animals, GSH blockage re-sults in neuronal pathology. Specific clinical
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 513
evidence in Parkinson’s disease also points toGSH depletion as the common thread. Bainsand Shaw45 gathered together the variousthreads and assembled them into the modelsummarized in Figure 3.
The features of this model most rel-evant to PD are GSH degradation in the SN,and its overlap with the presence of oxidativestressors. A source of oxidative stress need notbe just a toxin — it can be insufficiency ofdietary antioxidants or mineral enzyme cofac-tors, impairment of antioxidant enzyme syn-thesis, or the overall decline of antioxidantdefense capacity with advancing age. Further-
more, the negative synergy between GSHdepletion and oxidative stress certainly neednot result only in PD. This GSH-depletionmodel predicts the clustering ofneurodegenerative disease symptoms some-times clinically observed in the same indi-vidual, including Alzheimer’s disease, amyo-trophic lateral sclerosis (ALS), and PD.
The Bains and Shaw model of patho-logic GSH depletion also predicts that popu-lations most at risk for developing diseasessuch as PD, Alzheimer’s, and ALS are thoseat the low end of the overall range for GSH.45
They propose that “low-glutathione” indi-viduals exist in the population, “primed” forinitiation of PD or other neurodegenerativeprogression. Glutathione depletion could arisein various ways, including genetic propen-sity, poor diet, pharmaceutical treatment (aswith acetaminophen use), or as a function ofage. An Italian clinical team reported that in-travenous administration of GSH to newly-diagnosed PD patients resulted in marked im-provement in motor ability in nine patients.46
These findings were substantiated byPerlmutter in the United States.2
Potential Exogenous Triggers forParkinson’s
In its most healthy state the substantianigra is more vulnerable to oxidative attackthan probably any other brain region. Its
unique co-enrichments with dopamine,monoamine oxidases, iron, and melanin allcontribute to this excessive degree of vulner-ability. The SN also carries the mitochondrialcomplex I defect, which lowers energy produc-tion and intensifies endogenous oxygen freeradical production. Then there is the aging fac-tor: as the decades pass, antioxidant defensestend to become less competent. Conceivablythe SN decompensates only from endogenousoxidative stress, but the evidence argues for anadditional exogenous event or insult. What,then, is the trigger that finally sets in motionthe SN’s degenerative breakdown?
Oxidative stress(mitochondrial activity,
diminished level of otherantioxidants, e.g., SOD,
Vit. C, Vit. E, etc)
GSH synthesis,GSH status
Otherstressors
(environmental toxins, transition metals)
NecrosisExcitotoxicity
Apoptosis
∆GSH
∆Redoxmodulation
of ionotropicreceptors
∆Antioxidant,Free radicalscavengerfunction
∆Neurotransmitteraction
Alterations in ioniccurrents, increase
in [Ca+2], activation ofproteases, etc.
Lack of neuralstimulation, disuse,
failure to releasetrophic factors
Free radicaldamage tomembranes
and mitochondria
Neuron death
Neurodegenerative disorders/Aging
Figure 3: Proposed GSH-depletionModel for Neurodegenerative Disorders,including Parkinson’s Disease. FromBains and Shaw.45
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 514 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
This question cannot be satisfactorilyanswered, but clues do exist. One clue comesfrom a mixed ALS-parkinsonism dementiacomplex specific to the island of Guam.12,47 Anexogenous toxic influence is known to be in-volved, but no single agent has been confirmedbeyond doubt. Prime candidates are the DNApoison cycasin from the false sago palm(Cycas circinalis),47 or two excitotoxins thatalso come from this palm. In addition, there isthe high aluminum content of the soil, and zinccontamination of food prepared from thispalm.12 Some experts speculate that combina-tions of these factors could be acting in syn-ergy.
Another food-borne category of poten-tial neurotoxins is the ß-carbolines (harman,norharman, TaClo)48 and thetetrahydroisoquinolines (TIQ), which arestructurally similar to MPP+.40 Some of thesehave been isolated from the brain, cerebrospi-nal fluid, and plasma of PD patients. They alsoare consumed in foods such as cheese, cocoa,bananas, milk, eggs, and beef, and they crossthe blood-brain barrier.29 The ß-carbolineTaClo can be endogenously formed fromtryptamine, following exposure to chloral ortrichloroethylene, and the TIQs can be formedin the brain from catecholamine condensationwith aldehydes.40 Although they are describedas “weak neurotoxins,” the long-term effectsof chronic exposure have not been well ex-plored.
Heavy metals and transition metals thataccumulate at or near the SN are potential trig-gers for PD. Occupational exposure to iron,aluminum, or manganese for more than 30years greatly increases the risk of acquiringPD (odds ratio 13.64, p < 0.05);49,50 manga-nese overexposures often manifest as parkin-sonism. Iron, though essential for life, is highlyredox-active and chronically high levels couldescape protein buffering and promoteoxyradical generation.35
Acting to some degree like iron, whichis highly oxidative, mercury, lead, zinc, and
copper all have oxidant activity. All are capableof intensifying oxyradical generation in vivoand depleting tissue antioxidant stores. Mer-cury crosses the blood-brain barrier, and acase-control study conducted in Singapore haslinked body burden of this element to the di-agnosis of PD.51
Pesticides have now become highlysuspect as potential Parkinson’s disease trig-gers.52,53 A connection was long suspected be-tween PD and rural living, including the drink-ing of contaminated well water or exposuresto pesticides or herbicides, as well as indus-trial exposures to chemicals and heavy met-als.54 Cases have been reported of workers withexposure to multiple pesticides and early-on-set PD.50 Earlier, epidemiological studies sug-gested an etiological relationship between PDand pesticide exposure; dieldrin which is amitochondrial poison was specifically impli-cated.53 A more recently completed studyadded further likelihood to the possibility thatpesticides trigger PD.55
Dr. Lorene Nelson, a neuro-epidemiologist at Stanford University Schoolof Medicine in Palo Alto, California, andcolleagues did a study of 496 personsdiagnosed with PD and compared them with541 matched controls.55 Using structuredinterviews, they determined that homeexposure to insecticides and herbicides wasassociated with increased risk of PD.Fungicide exposure did not emerge asstatistically significant. Upon further analysis,in-home insecticide exposure for non-gardeners was found to pose higher risk (twicenormal) than outside gardening with herbicides(1.7x) or insecticides (1.5x).
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 515
Parkinson’s Initiation May NotRequire Extended Exposure
Parkinson’s disease is deceptivelycomplex, but as a result of the MPTP experi-ence real progress has been made toward un-derstanding the mechanisms operative in thedisease. A few high-dose exposures to MPTPby the intravenous route can trigger parkinso-nian symptoms that very closely resemblePD.19,20 MPTP’s startling toxicity is an exag-gerated though faithful model for PD wherein,due to molecular abnormalities, the mitochon-dria become targeted by an exogenous oxidanttoxin. This compromises energy supply, mag-nifies oxidative load thus depleting antioxidantresources, and destroys the vulnerable substan-tia nigra.
Following their initial report on MPTPtoxicity,19 Langston and collaborators followedthe fates of a small number of more severelyaffected MPTP victims.20 After seven years,they used positron emission tomography(PET) imaging with labeled fluorodopa to as-sess striatal dopamine function in 10 subjectsoriginally exposed to MPTP for very shortperiods.56 The PET findings closely matchedthe clinical records and indicated nigrostriatalfunction in these subjects was declining morerapidly than in normal aging.
As the years went by, Langston’s groupcontinued long-term patient tracking, and ob-tained samples from the brains of three indi-viduals not long after death.20 They found con-vincing evidence that, following an initial briefperiod of MPTP exposure years previous,some of the victims had progressed to bonafide Parkinson’s disease. All three had origi-nally injected MPTP for no more than a weekin 1982, and they died 3, 12, and 16 years af-ter the initial exposure. At death all had activeneuronal degeneration and a type of reactivehistopathology in the SN that strikingly re-sembled the pattern established for PD, thoughthey had not used MPTP since their initial ex-posure.
These findings from Langston can betaken to suggest that a transient toxic expo-sure — even a relatively short, one-weekperiod of exposure to MPTP — initiated aslowly progressive brain pathology that con-tinued to worsen for as long as 16 years untilthe death of the patient. They reported theirfindings were indicative of “active, ongoingnerve cell loss,” suggesting that, “a time-lim-ited insult to the nigrostriatal system can setin motion a self-perpetuating process ofneurodegeneration.”20 They suggested threepossible mechanisms to explain these dramaticfindings: (1) oxidative stress; (2) treatment ofthe subjects’ initial parkinsonian symptomswith levodopa, which could enhance dopa-mine production in overworked andhypofunctional SN neurons and further pro-mote dopamine oxidation; and (3) a self-per-petuating inflammatory process. None of thesemechanisms excludes the others; on the con-trary, the available findings suggest all threeare simultaneously active in the Parkinson’sbrain. Parkinson’s disease appears to be amultifactorial disease, initiated and probablydriven by oxidative factors.
This multifactorial, oxidative stressmodel for Parkinson’s disease is consistentwith the considerable body of clinical data onPD. It carries a sobering implication: the thou-sands of oxidant chemicals that contaminatethe air, water, soil, and food could act singlyor in combination to trigger disease progres-sion. Foods depleted of antioxidants, oxidantpharmaceuticals, or lifestyle factors that raiseoxidative load (smoking, drinking, chronicvirus load) could all contribute. If the toxicexposure is at relatively low concentration butsustained over time, the process can be set intomotion but take years or decades to clinicallymanifest. The aging process also may comeinto play: a younger individual may be com-paratively resistant to toxic triggers unlessgenetically susceptible, whereas an older per-son might be rendered comparatively defense-less against oxidant attack.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 516 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
The pattern of cell breakdown and in-flammation evident in the PD brain is uniqueto PD. It exhibits some of the predictable fea-tures of nerve tissue reaction to damage, in-cluding microglial activation57,58 and increasesin cytokines such as transforming growth fac-tor-beta (TGF-ß-1) and tumor necrosis factor-alpha (TNF-α).59 Atypical features include aconspicuous absence of astrocytic activation60
and no evidence of apoptotic cell death.58 Justhow this unique mix of processes combine tocreate the inexorable progression of brain de-generation still remains to be deciphered. Un-til more definitive evidence emerges, the strat-egy for attempted prophylaxis of PD, and forits long-term medical management, must befully integrative and take into account all pos-sible contributory factors.
L-Dopa Likely Contributes toDisease Progression
The standard medical therapy for PDcontinues to be levodopa, usually withcarbidopa added to prolong its retention(Sinemet, Sinemet CR). Levodopa is the mostimmediate biochemical precursor to dopa-mine, the neurotransmitter depleted due tobreakdown of the substantia nigra. Thistherapy does not ameliorate the underlyingprogressive loss of dopamine-producing neu-rons and over the long term may contribute toPD progression.
Parkinson’s patients treated withlevodopa sometimes develop elevated plasmahomocysteine (HCy).61 Hyperhomo-cysteinemia is a major risk factor for vasculardisease.62 SAMe (s-adenosyl methionine, amethyl-activated metabolite of methionine) isa key metabolic contributor to the recyclingof HCy.60 Levodopa was found to depleteSAMe from the central nervous system of hu-man subjects, and perhaps poses a threat tothe homeostatic regulation of homocysteine.63
Muller and colleagues64 measuredplasma HCy in Parkinson’s patients treatedwith levodopa, and compared them with
Parkinson’s subjects not previously treated,and healthy controls. HCy levels were almosttwice as high in the levodopa-treated PD pa-tients as compared with the non-treated groupand the healthy group (p < 0.001 and p < 0.002,respectively); plasma HCy of the non-treatedParkinson’s patients did not significantly dif-fer from the healthy participants. Dangerouslyelevated plasma HCy may provide a key tothe increased mortality attributed to vasculardisease in patients with PD.65 These findingsalso suggest PD patients taking levodopa mightbenefit from concomitant supplementationwith folate and vitamin B12, both of whichhelp recycle HCy.
Nutrient Deficiencies in Parkinson’sDisease
The brain uses the same nutrients thatother organs use; therefore, all nutrient classescan be useful to Parkinson’s patients. Manynutrients have been found deficient in PD, andothers are likely to be deficient at some pointduring disease progression.66
Certain individual amino acids are pre-cursors to brain neurotransmitters and signifi-cantly ameliorate symptoms when given asdietary supplements. Tyrosine, phenylalanine,and tryptophan can all be blocked from ab-sorption by levodopa, thereby becoming defi-cient. L-tyrosine is a direct precursor tolevodopa, which is then converted to dopa-mine. Deficiency may develop due to reducedintake from meat, dairy and eggs, or to dimin-ished enzymatic conversion from phenylala-nine. PD patients also may have impaired ca-pacity to utilize L-tyrosine,67 even though itmay be normally absorbed.68 In 1989, Lemoineand collaborators reported L-tyrosine gavebetter clinical results and had many fewer sideeffects than levodopa when tested in a smallgroup of patients.66 L-tyrosine should not betaken at the same time of day as levodopa,since it competes for absorption.
D-phenylalanine is another amino acidthat should not be taken with levodopa.66 The
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 517
D-form (DPA specifically; not the L-form) wasreported to improve rigidity, walking, speechdifficulties, and psychic depression, but nottremor.69 L-tryptophan also competes withlevodopa for absorption.66 Parkinson’s diseasepatients treated with levodopa can manifestlow serum tryptophan,70 and L-tryptophantherapy often helps them break through theirdepression.71 In a placebo-controlled study, L-tryptophan produced improvements in func-tional ability beyond those afforded bylevodopa, and also significantly improvedmood and drive.72 Given with niacin and pyri-doxine, L-tryptophan was useful in ameliorat-ing the motor complications from long-termlevodopa therapy.66
L-methionine is an essential aminoacid, and its supplementation may benefit PD.In one study, 15 patients who had maximalimprovement from standard medications wereincreased gradually from 1 g/day to 5 g/day.73
Ten of the 15 improved on all measures ex-cept tremor and drooling.
A number of B vitamins may be defi-cient in PD patients. In one reported case, de-ficiency of folic acid due to an inborn error offolate metabolism generated parkinsoniansymptoms which included progressive hypoki-nesia, tremor, rigidity, and “pill-rolling,” withdeficiency of dopamine though SN degenera-tion was not found at autopsy.74 Niacin canbecome deficient in patients treated withlevodopa, especially if it is given withcarbidopa or other decarboxylase inhibitors.75
Supplementation with niacin may prolong el-evated brain levodopa levels.76
In the case of vitamin B6, treatmentwith levodopa alone often raises the levels ofthis vitamin, so co-supplementation is con-traindicated.77 By contrast, treatment with thecommonly prescribed levodopa-carbidopacombination may provoke a marginal B6 de-ficiency, and supplementation with B6 canbenefit at least some of these patients.78,79 Vi-tamin B6 can be injected intraspinally withthiamine, for partial symptomatic relief.66
Vitamin C (ascorbic acid) is sometimesfound decreased in Parkinson’s brains.34 Onedouble-blind trial in PD found supplementa-tion produced a modest improvement in func-tional performance.66 In 1975, Sacks andSimpson reported 4 g/day ascorbic acid less-ened nausea and other levodopa side effectsin the case of a 62-year-old man.80 When al-ternated between ascorbic acid and placebo(citric acid) under double-blind conditions, hispatterns of improvement correlated with theperiods of receiving ascorbic acid.
Vitamin E supplementation may beimportant for PD patients. A 1988 survey ofthe dietary habits of PD patients prior to theage of 40 revealed that intakes of nuts, oils,and plums relatively high in vitamin E wereassociated with lowered risk of PD.66 Previ-ous clinical studies using high doses of encap-sulated vitamin E suggested this vitamin hasan important role in slowing disease progres-sion.81,82
Disagreement exists as to whether cop-per is elevated or deficient in PD. It was re-ported elevated in the cerebrospinal fluid ofParkinson’s patients, the degree of elevationbeing significantly correlated with both dis-ease severity and rate of progression.83 Theresearcher suggested copper chelation be usedtherapeutically in these cases. However, oth-ers reported copper in the SN region was ab-normally low.84,85
Glutathione becomes more depletedfrom the SN as the disease progresses (Figure4).34 N-acetyl cysteine86 and alpha-lipoic acidcontribute to GSH repletion and are also po-tent antioxidants. Building on the highly posi-tive findings from Italy — that intravenousGSH benefited all nine patients with early PD46
— the pioneering Perlmutter Center offers in-travenous GSH as the most direct means forGSH repletion.2
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 518 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
Integrative Management ofParkinson’s Disease
With the evidence steadily accumulat-ing that Parkinson’s disease is a multifactorialoxidative disease, there is an urgent need forintegrative management. The allopathic modelthat currently dominates Parkinson’s manage-ment is obsolete. The major adverse side ef-fects of the various drugs currently in use forthe disease, combined with the limitations ofthe dopamine replacement strategy, dictate theneed for alternatives.
The classic Parkinson’s progression —depletion of dopamine-producing neuronsfrom the substantia nigra, the accumulation ofLewy bodies — no longer represents thepathobiology of this disease. A systemic pat-tern for PD is evident from the findings ofmultiple control circuit damage throughout thebrain; damage along the variousnondopaminergic pathways; peripheral nervedegeneration; changes in the heart; mitochon-drial insufficiency in brain and probably inmuscle and platelets; and defective P450detoxification. This broadened understandingof the disease dictates that its medical man-agement strategy also be broadened.
Dietary RevisionDecreasing protein intake is useful in
PD. For patients being maintained onlevodopa, high protein intake typical of West-ern lifestyle may interfere with levodopa avail-ability and contribute to episodic loss of symp-tomatic control by the drug (the “off-on” phe-nomenon). Mena and Cotzias87 assessed sev-eral levels of protein intakes, and found lowintake (0.5 g/kg/day) improved symptomaticcontrol throughout the day, while high intake(10 g/kg/day) exaggerated the off-on pattern.Seven patients were maintained for up to a yearon low protein intake; six of them maintainedstability with five achieving reductions oflevodopa doses. These early results were con-firmed in subsequent clinical studies.88-90
In a double-blind study that comparedlow protein intake (50 g/day for men and 40g/day for women) to high protein intake (80g/day for men and 70 g/day for women), totalperformance scores were significantly im-proved, along with tremor, hand agility, andmobility in the low protein groups.88 In anotherstudy, modifying meal patterns to eat the ma-jority of protein in the evening also improvedsymptoms.89 These effects were unrelated tolevodopa absorption or blood levels; perhapsthey are due to some central action of highdietary protein88 or variation in the plasmacontent of large amino acids.89
Reducing caloric and fat intakes is alsoimportant. Logroscino and his collaboratorsfrom Columbia University91 surveyed the di-etary intakes of 110 PD and 287 non-PD sub-jects in New York City. They found PD pa-tients consumed significantly more calories (p< 0.0001), their energy-adjusted fat intake wassignificantly higher (p < 0.007), and an increas-ing intake of animal fats was strongly relatedto PD (p < 0.001, odds ratio 5.3, 95% confi-dence interval 1.8-15.5). Intakes of antioxi-dants were not significantly different betweenthe groups. These findings are worthy of fur-ther investigation; they are consistent with areport from England that cardiovascular dis-ease, also linked to high fat, high calorie di-ets, is a more predominant cause of deathamong PD patients than the general popula-tion.65
Caloric reduction has been under scru-tiny for some time as a means to better healthand extended longevity. Considerable personaldiscipline is required to adhere to the regimen,but the scientific findings are very clear: lesscalories consumed translates into decreasedfree radical production. This is an importantmeans of lowering endogenous oxidative load,which is linked to aging progression.92 Reduc-tion of lipid calories is also integral to this strat-egy, because lipids are the foremost substratesfor peroxidative attack coming from endog-enous oxidative overload. In addition, high
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 519
animal fat consumption generally results in apro-inflammatory shift in the tissues due to thepreponderance of long-chain omega-6 con-tent.93 Parkinson’s patients may be well advisedto rebalance their dietary fatty acid sources byminimizing saturated fats and increasing long-chain omega-3 intakes while reducing theirtotal caloric intake.
Metal DetoxificationIron occurs at very high concentrations
in the SN, wherein it normally is bound to fer-ritin. Free unbuffered iron likely worsens theoxidative degenerative process in PD, so peri-odic monitoring of iron saturation status isstrongly indicated. Mercury can access thebrain by volatilizing from dental fillings, orby crossing the blood-brain barrier after be-coming absorbed from foods.
A landmark Singapore study assessedmercury body burden and linked this to riskof PD.51 Fifty-four cases of confirmed PD werecompared to 95 hospital-based controls. PDwas accurately diagnosed, then mercury bodyburden indirectly assessed via blood and urinelevels. The relative risk for PD was 8.5x forblood Hg > 5.9 ng/mL (95% confidence inter-val 2.2-33.2), and 14.8x for urine Hg > 6.8 ng/mL (95% confidence interval 3.5-63.7). Den-tists occupationally exposed to mercury inSingapore averaged above this range, and un-exposed office workers averaged below it. A“zero load” approach to mercury detoxifica-tion should be the norm, wherein all sourcesof mercury exposure are eliminated. Wheremercury contamination is identified, chelationshould be used to eliminate it from the body.94
Systemic Glutathione ReplacementWith the evidence so overwhelming
that GSH depletion is a central event inPD,32,33,37 and that the degree of GSH deple-tion is worse in advanced disease (Figure 4,lower), effective repletion of GSH must be atherapeutic priority. Combined intravenousand oral GSH replacement is safe and well
tolerated, providing ongoing benefit. As oralGSH precursors both N-acetylcysteine95 andalpha-lipoic acid are appropriate. GSH is alsoa systemic antioxidant, and its ongoing reple-tion may help ameliorate Parkinson’s-relateddamage in the heart, liver, muscles, and otherorgans.31
Systemic GSH status is also conservedby bolstering other antioxidant defenses. Es-pecially noteworthy is high-dose vitamin C,which provides antioxidant reducing equiva-lents known to conserve GSH. Intravenousascorbate is a long-established and proven pro-tocol.96 Taken together with vitamin C, vita-min E probably also helps delay PD progres-sion.
In 1979, believing oxidative stresscould be a major factor causing neuronal deathin PD, Dr. Stanley Fahn, a neurologist at Co-lumbia University, began prescribing relativelyhigh doses of vitamins C (3 g/day) and E(3,200 IU/day) for his PD patients.81 As con-trols he used data on patients from anotherphysician, who managed her cases almostidentically to his practice but did not adminis-ter antioxidants. After tracking 21 patients fora number of years, Fahn’s group found early-onset patients (onset <54 years) maintained onhigh doses of vitamins C and E were able todelay levodopa or deprenyl therapy by about25 months when compared with matched con-trols. The later-onset patients (54+ years) wereable to delay the transition to drugs by about35 months.
Subsequently, a large, multicenter,double-blind trial was organized. In thisDATATOP study (Deprenyl and TocopherolAntioxidant Therapy of Parkinson’s)82 theParkinson’s Study Group evaluated 2,000 IUof tocopherol and 10 mg of deprenyl per dayin 800 subjects with early PD. Primaryendpoint for the study was disability sufficientto prompt the decision to begin takinglevodopa. The outcome was that deprenyltreatment delayed disability for almost ninemonths, whereas tocopherol treatment (at 2000
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 520 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
IU/day, lower than Fahn’s study) was not foundto extend delay. This finding should not be
unexpected since nutrient antioxidants oftenwork together in coordinated biochemicaldefense rather than acting singly.23,42
Comprehensive GSH conservationrequires additional oral supplementationwith the entire range of nutrient antioxidantsand antioxidant enzyme mineral co-factors.However, since PD causes considerable ner-vous system damage prior to becomingsymptomatic, antioxidant intervention mayslow further progression but is unlikely tocompletely restore function unless imple-mented prior to clinical emergence of thedisease. Bains and Shaw suggest a prophy-lactic strategy for PD, including screeningat early middle-age to detect individuals withlow-glutathione status.45
Essential fatty acids may have ben-efits for PD symptoms. Evening primroseoil, enriched in the anti-inflammatory,omega-6 gamma-linolenic acid, was re-ported to relieve tremor.98 The omega-3 fattyacids, especially DHA and EPA in fish oils,tend to reduce pro-inflammatory cytokineproduction in vivo.99,100 Due to their high pro-pensity for oxidation they should be admin-istered in conjunction with high intakes ofantioxidants. Octacosanol, a long-chain al-cohol found in wheat germ oil, was reportedto be helpful in PD. In a double-blind cross-over trial, 3 of 10 patients significantly im-proved and none worsened, with no adverseside effects experienced.101 The means bywhich this nutrient is benefiting PD is notimmediately evident.
Revitalizing the Parkinson’s BrainGiven the confirmed presence of mi-
tochondrial energetic abnormalities in thesubstantia nigra and elsewhere in the af-flicted brain,26,27,29 nutrients that safely boostmitochondrial function deserve further ex-ploration for clinical benefit in PD. Coen-
zyme Q10 (ubiquinone; CoQ10) is an electronacceptor and antioxidant that is a key compo-nent of mitochondrial electron transfer.24 Two
*
*250
200
150
100
50
0
Coe
nzym
e Q
10
PD SPOUSE CONTROL
100
50
0C C+PD 0-1 2 3-4
PD Stages
Glu
tath
ione
(µg
/g)
Above: platelet coenzyme Q10, compared between PD patients, spouses, and controls. * = significantly different (p<0.01).97
Below: glutathione levels in substantia nigra of PD patients and controls.34
Grade of degeneration and glutathione concentration correlated at r=96%, p<0.05
Figure 4: Deficiency of Coenzyme Q10and Progressive Depletion of Glutathione inParkinson’s Disease.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 521
separate groups reported CoQ10 was signifi-cantly reduced in mitochondria taken from thebrain97 and platelets102 of PD patients (Figure4, upper). Lowered complex I activity wasstrongly correlated with reduced mitochondrialcontent of CoQ10.
Shults and collaborators gave threedifferent oral doses of CoQ10 with vitamin Edaily to 15 PD patients and, after one month,found complex I activity was increased.103 At600 mg/day of CoQ10, complex I activitydoubled to well within the range for healthysubjects, but small sample sizes precluded at-tainment of statistical significance. Since themitochondrial CoQ10 balance may be shiftedfrom the reduced form to the oxidized form inPD,102 the oxidative drain placed on CoQ10may be extreme. Additional supplementationwith other mitochondrial support nutrients —nicotinamide adenine dinucleotide (NADH),acetyl-L-carnitine, and phosphatidylserine(PS) — could diversify energy input to themitochondria and further help compensate forthe energetic impairment of PD.
NADH is an electron energy carrieralso indispensable to mitochondrial oxidativephosphorylation. Birkmayer and collaboratorspioneered its application in PD.104,105
Reasoning that exogenous levodopa down-regulates its own endogenous biosynthesis,they sought to boost endogenous dopamineproduction via the intrinsic pathways.104 Afterfinding that NADH did boost dopamineproduction in cultured nerve cells, theyconducted an open-label trial on PD patients.105
They treated 415 patients intravenously and470 by the oral route. Using patients as theirown controls, they found similar benefitsbetween intravenous and oral NADH. For oralNADH the mean improvement of disabilitywas 19.8 percent, for intravenous 20.6 percent;maximum improvement was 55 and 60percent, respectively, and 36 percent of patientsexperienced better than 10-percent benefit.Subsequently, Kuhn and collaboratorsconfirmed the benefit of intravenous NADH.106
Acetyl-L-carnitine is another mito-chondrial energy carrier, activating transportinto the mitochondria of fatty acids to be usedfor energy. This nutrient has energizing, pro-tective, and trophic effects.107 In animal experi-ments it partially protected the SN againstMPP+ attack, enhanced dopaminergic trans-mission, and boosted intrinsic growth factorproduction.107,108
• Glutathione (reduced, GSH), intravenous, 600-1,000 mg 3 times per week
• Cellular Energizers: Coenzyme Q10 120 mg, NADH 5 mg (twice daily), PhosphatidylSerine 100 mg daily
• Antioxidants: Vitamin C (ascorbic acid) 800 mg, Vitamin E (d-alpha-tocopherol) 1200 IU, alpha- Lipoic acid 80 mg, N-AcetylCysteine (NAC) 400 mg, Ginkgo biloba extract (standardized 24/6) 60mg, Acetyl-L-Carnitine 400 mg, Vitamin D 400 IU, daily.
* Other nutrients: Vitamin B3 (as niacinamide) 100 mg, Vitamin B6 (as pyridoxine) 100 mg, Vitamin B12 (as cyanocobalamin) 200 mcg, Folic acid 800 mcg, Magnesium (as citrate) 420 mg, Zinc (as an "amino acid chelate") 20 mg, daily.
• In PD patients less than 65 years of age, check liver detoxification capacity and treat with milk thistle extract and other liver support nutrients as necessary.
Table 3: The Perlmutter Protocol— Integrative Parkinson’s Disease Management.2
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 522 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
Phosphatidylserine is a fundamentalcomponent of the mitochondrial membranesystems on which are assembled the electrontransfer complexes. It is also a membranebuilding block for the synaptic and other neu-ronal membranes, and plays a key role inelectro-chemical transmission between theneurons. Whole-brain imaging with PETshowed PS can markedly enhance energeticsthroughout the brain.107 In an open-label trialconducted on Parkinson’s patients in Germany,PS provided greater than 10-percent benefitto 7 of 12 subjects.109
For the busy integrative physician toconsolidate all these approaches into a cohe-sive protocol the patient can manage is not aneasy task. One example where this has beenaccomplished, and a paramount resource forintegrative management of PD, is thePerlmutter Health Center in Naples, Florida.The center’s director, David Perlmutter, MD,developed the protocol summarized in Table 3.
Upcoming Advances in IntegrativeManagement
The inexorable downhill slide that cur-rently characterizes Parkinson’s disease can beameliorated through early and aggressive in-tervention based on an integrative protocol asexemplified in Table 3. Over the longer term,medical mastery over this disease awaits ad-vances in presymptomatic detection and riskassessment, and in effective brain restoration.
Relevant to these goals, several promisingtechnological breakthroughs are on the hori-zon.
Functional Whole-Brain ImagingTomographic imaging, both by PET
and SPECT (single photon emission tomog-raphy), offers exciting possibilities for im-proved preclinical detection and for assess-ment of severity and progression. At the cel-lular level in the brain abnormalities are dis-cernible years before the disease becomesclinically manifest, but these can only be vi-sualized microscopically following biopsy.Functional whole-brain imaging is superiorbecause it is non-invasive, is becoming increas-ingly more available, and can now detect andquantify dopamine activity in the living brain.As shown in Figure 5, PET examination usingperfusion with 18F-6-fluorodopa label can ef-fectively probe decreased dopaminergic func-tion in the brain (putamen) prior to the appear-ance of clinical symptoms.110,111
Following its intravenous administra-tion, 18F-6-fluorodopa is taken up by thenigrostriatal dopaminergic projections anddecarboxylated to labeled dopamine anddopamine metabolites. This conversion is im-aged at high resolution using PET. Parkinson’spatients imaged with PET revealed an aver-age 50-percent loss of dopamine uptake by theputamen.111 These data could be compared tothe average 60-80 percent loss of SN zona
Figure 5: PET Imaging of Striatal 18F-dopa Uptake in NormalSubject and Co-twin (monozygotic) of Affected PD Patient. FromPiccini, in Brooks.111
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 523
compacta cells as quantified from postmortemsampling. As putamen dopamine levels be-come reduced by 90 percent in end-stage PD,PET shows the nigrostriatal projections aremaking virtually no dopamine.
Patients with newly emergent, one-sided PD show by PET a 30-percent dopam-ine loss, which matches the 30-percent nigralcell loss threshold (counted at autopsy) forsymptom emergence. In one case, the tech-nique detected impaired dopamine metabolismfive years prior to symptom emergence.111 Thiscould be extremely valuable for risk assess-ment in asymptomatic, at-risk individuals, in-cluding relatives with known PD pedigrees.
Using a new 3-dimensional signal in-tegration approach, 18F-dopa PET and othersophisticated whole-brain labeling technologycan now detect reduced dopamine uptake inall patients with emergent PD, and demonstrateprogressive reductions in the striatal, nigral,and cingulate levels of dopamine storage asthe disease progresses.112 PD can now be dis-criminated from atypical parkinsonian condi-tions with 80-percent accuracy, and non-PDconditions that feature reduced dopamine me-tabolism (striatonigral degeneration, multiplesystem atrophy) can also be quantified anddiscriminated from PD.
Clinical rating scales are notoriouslyimprecise for estimating PD progression. 18F-dopa PET and related imaging provide a moreobjective approach to staging, especially sincedisease duration correlates with dopaminergicdecline. The preclinical “window” of dopam-inergic decline prior to symptom emergenceis estimated at 6 ± 3 years using imaging,113
whereas estimates from nigral cell counts setthis period at an average 4.5 years.111
NeuroprotectionThe allopathic approach to PD man-
agement continues to generate new pharma-ceuticals, with the hope of eventually replac-ing levodopa with a comparably effective andless toxic monotherapy. Potential
neuroprotective monotherapies are receivinghigh priority. Among the drugs already utilizedfor PD management, selegiline and amanta-dine appear to have neuroprotective proper-ties.114 Epidemiologic and clinical evidencesuggests estrogens can be protective in PD,115
and PET-controlled comparisons suggestropinirole may be protective at early stages.114
In a baboon model of PD, nitric oxide syn-thase inhibitors blocked the biochemical andclinical manifestations of MPTP toxicity.116 Ina rat model of PD, infusions of the opiate re-ceptor antagonist naloxone partially protectedagainst SN damage.117 In cultures of dopamin-ergic neurons, the cytokines IL-1ß and IL-6protected against MPP+ toxicity.118 Other pos-sible neuroprotectors for PD are MAO-B in-hibitors, NMDA-receptor antagonists, anddopamine receptor agonists.114 A few expertshave suggested a “multi-neuroprotective” strat-egy be explored, which hopefully is a preludeto an eventual “meeting of the minds” on inte-grative management of PD.
Neural TransplantationAttempts to replace dopamine-secret-
ing neurons within the disease-ravaged sub-stantia nigra, using transplanted adrenal med-ullary or fetal tissue, successfully demon-strated that such tissue can partially survivethe transplantation process, become estab-lished, and produce dopamine in the new tis-sue environment.119 To date, a few patients havebenefited from this landmark procedure, andno doubt relative success will improve as thetechnique is improved. However, transplanteddopamine neurons have not been able to fullyreplace the needed amounts of dopamine. Fu-ture transplant methodology is likely to placegreater priority on stem cells and/or culturedcell lines as the tissue source, probably incloser conjunction with growth factors andother cell-activating substances.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 524 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
Stem Cells, Growth Factors, andGene Therapy
Recent unequivocal demonstration thatstem cells are present in the human brain hascreated a new dimension of possibilities forregeneration of the central nervous system.120
This advance is particularly timely for PD,wherein the earlier limited successes with tis-sue transplantation have prepared the groundfor stem cell transplants which should havebetter implantation potential. Now growth-pro-moting trophic substances, or growth factorsare being employed to improve the possibili-ties for survival of the transplant. One factoralready being utilized for this purpose is glialcell line-derived neurotrophic factor.121 Vaso-active intestinal peptide helps nerve cells inculture to conserve their GSH stores122 Still,from the integrative perspective the challengeis to induce the Parkinson’s brain to endog-enously produce the needed variety and com-binations of growth factors (probably in syn-ergy with stem cells) that would accomplishbrain revitalization.
In the more distant future, gene therapyusing transplantation of genetically engineeredcells, or direct insertion of genes into apatient’s brain cells, may prove clinically fea-sible.123 Skin and muscle cells genetically al-tered to overproduce tyrosine hydroxylasehave been successfully transplanted intoMPTP-parkinsonian monkeys, where they sur-vived, integrated well into the brain, and pro-duced dopamine for several months. A greatdeal of basic research remains, in order to de-velop effective biological vectors for gene in-sertion, to ensure inserted genes will continueto function, and to identify other gene prod-ucts than dopamine-synthesizing enzymeslikely to benefit the disease.
Until that time when such heroic, high-tech medicine has become effective, safe, andfinancially affordable, the available clinicalexperience suggests that PD management canbe markedly improved by following an
integrative medical model. This more rationaland more resourceful medical approach wouldembrace non-invasive early detection,rendering dopamine replacement the last resortrather than the first; pursue nerve tissuerestoration before surgical intervention; andwin for the Parkinson’s disease patient yearsof productive well-being.
References1. Saunders CD. Parkinson’s Disease: A New
Hope. Boston, MA: Harvard Health Publica-tions; 2000.
2. Perlmutter D. BrainRecovery.com:PowerfulTherapy for Challenging Brain Disorders.Naples, FL: The Perlmutter Health Center(www.brainrecovery.com); 2000.
3. Waite LM, Broe GA, Creasey H, et al. Neuro-logical signs, aging, and the neurodegenerativesyndromes. Archs Neurol 1996;53:498-502.
4. Braak H, Braak E. Pathoanatomy ofParkinson’s disease. J Neurol 2000;247 Suppl.2:3-10.
5. Brown RG, Marsden CD. How common isdementia in Parkinson’s disease? Lancet 1984;2:1262-1265.
6. Goldstein DS, Holmes C, Li ST, et al. Cardiacsympathetic denervation in Parkinson disease.Ann Intern Med 2000;133:338-347.
7. Tanner CM. Liver enzyme abnormalities inParkinson’s disease. Geriatrics 1991;46:S60-S63.
8. Schapira AHV, Mann VM, Cooper JM, et al.Anatomic and disease specificity of NADHCoQ1 reductase (complex I) deficiency inParkinson’s disease. J Neurochem1990;55:2142-2145.
9. Olanow CW, Jenner P, Youdim M.Neurodegeneration and Neuroprotection inParkinson’s Disease. New York, NY: Aca-demic Press;1996.
10. Wolfe SM, Sasich LD, Hope RE, et al. WorstPills, Best Pills. New York: Pocket Books;1999.
11. Casals J, Elizan TS, Yahr MD. Postencephaliticparkinsonism - a review. J Neural Transm1998;105:645-676.
12. Stone R. Guam: deadly disease dying out.Science 1993;261:424-426.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 525
13. Krack P, Poepping M, Weinert D, et al.Thalamic, pallidal, or subthalamic surgery forParkinson’s disease? J Neurol 2000;247 Suppl.2:122-134.
14. Bejjani BP, Dormont D, Pidoux B, et al.Bilateral subthalamic stimulation forParkinson’s disease by using three-dimensionalstereotactic magnetic resonance imaging andelectrophysiological guidance. J Neurosurg2000;92:615-625.
15. Jahanshahi M, Ardouin A, Brown RG, et al.The impact of deep brain stimulation onexecutive function in Parkinson’s disease.Brain 2000;123:1142-1154.
16. Rohan de Silva HA, Khan NL, Wood NW. Thegenetics of Parkinson’s disease. Curr OpinGen Dev 2000;10:292-298.
17. Reiss O, Kuhn W, Krueger R. Genetic influ-ence on the development of Parkinson’sdisease. J Neurol 2000;247 Suppl 2:69-74.
18. Tanner CM, Ottman R, Goldman SM, et al.Parkinson disease in twins. JAMA1999;281:341-346.
19. Langston JW, Ballard P, Tetrud JW, Irwin I.Chronic parkinsonism in humans due to aproduct of meperidine-analog synthesis.Science 1983;219:979-980.
20. Langston JW, Forno LS, Tetrud J, et al.Evidence of active nerve cell degeneration inthe substantia nigra of humans years after 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridineexposure. Ann Neurol 1999;46:598-605.
21. Sayre LM. Biochemical mechanism of actionof the dopaminergic neurotoxin MPTP. ToxicolLett 1989;48:121-149.
22. Kidd PM, Levine SA. The biochemistry of freeradicals. In: Levine SA, Kidd PM ed. Antioxi-dant Adaptation: Its Role in Free RadicalPathology. El Cerrito, CA: PMK; 1985.
23. Kidd PM. Natural antioxidants, first-linedefense (Chapter 6). In: Kidd PM, Huber Wed. Living With the AIDS Virus: A Strategy forLong-Term Survival. El Cerrito, CA: PMK;1991.
24. Kidd PM, Huber W, Summerfield F, et al.Coenzyme Q10: Essential Energy Carrier andAntioxidant. El Cerrito, CA: PMK Biomedi-cal;1988.
25. Reichmann H, Janetsky B. Mitochondrialdysfunction — a pathogenetic factor inParkinson’s disease. J Neurol 2000;247 Suppl.2:63-68.
26. Haas RH, Nasirian F, Nakano K, et al. Lowplatelet mitochondrial complex I and complexII/III activity in early untreated Parkinson’sdisease. Ann Neurol 1995;37:714-722.
27. Swerdlow RH, Parks JK, Miller SW, et al.Origin and functional consequences of thecomplex I defect in Parkinson’s disease. AnnNeurol 1996;40:663-671.
28. Mizuno Y, Saitoh H, Sone N. Inhibition ofmitochondrial alpha-ketoglutarate dehydroge-nase by 1-methyl-4-phenylpyridinium ion.Biochem Biophys Res Comm 1987;143:971-976.
29. Mizuno Y, Ikebe S, Hattori N, et al. Role ofmitochondria in the etiology and pathogenesisof Parkinson’s disease. Biochim Biophys Acta1995;1271:265-274.
30. Levine SA, Kidd PM. Antioxidant Adaptation:Its Role in Free Radical Pathology. SanLeandro, CA: Biocurrents/Allergy ResearchGroup; 1985.
31. Kidd PM. Glutathione: systemic protectantagainst oxidative and free radical damage.Altern Med Rev 1997;2(3):155-176.
32. Perry TL, Godin DV, Hansen S. Parkinson’sdisease: a disorder due to nigral glutathionedeficiency? Neurosci Lett 1982;33:305-310.
33. Jenner P. Oxidative mechanisms in nigral celldeath in Parkinson’s disease. Mov Disord1998;13:S24-S34.
34. Riederer P, Sofic E, Rausch W, et al. Transitionmetals, ferritin, glutathione, and ascorbic acidin parkinsonian brains. J Neurochem1989;52:515-520.
35. Pezzella A, d’Ischia M, Napolitano A, et al.Iron-mediated generation of the neurotoxin 6-hydroxydopamine quinone by reaction of fattyacid hydroperoxides with dopamine: a possiblecontributory mechanism for neuronal degen-eration in Parkinson’s disease. J Med Chem1997;40:2211-2216.
36. Jellinger K, Paulus W, Grundke-Iqbal I, et al.Brain iron and ferritin in Parkinson’s andAlzheimer’s diseases. J Neural Transm ParkDis Dement Sect 1990;2:327-340.
37. Youdim MBH, Ben-Schachar D, Riederer P. IsParkinson’s disease a progressive siderosis ofsubstantia nigra resulting in iron and melanininduced neurodegeneration? Acta NeurolScand 1989;126:47-54.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 526 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
38. Paik SR, Shin HJ, Lee JH. Metal-catalyzedoxidation of alpha-synuclein in the presence ofcopper(II) and hydrogen peroxide. ArchBiochem Biophys 2000;378:269-277.
39. Youdim MBH, Ben-Schachar D, Riederer P.The role of monoamine oxidase, iron-melanininteraction, and intracellular calcium inParkinson’s disease. J Neural Transm1990;32:S239-S248.
40. Foley P, Riederer P. Influence of neurotoxinsand oxidative stress on the onset and progres-sion of Parkinson’s disease. J Neurol 2000;247Suppl. 2:82-94.
41. Jellinger KA. Cell death mechanisms inParkinson’s disease. J Neural Transm2000;107:1-29.
42. Dexter DT, Carter CJ, Wells FR, et al. Basallipid peroxidation in substantia nigra isincreased in Parkinson’s disease. J Neurochem1989;52:381-389.
43. Martilla RJ, Lorentz H, Rinne UK. Oxygenprotecting enzymes in Parkinson’s disease:increase of superoxide dismutase-like activity.J Neurol Sci 1988;86:321-331.
44. Kanda S, Bishop JF, Eglitis MA, et al. En-hanced vulnerability to oxidative stress byalpha-synuclein mutations and C-terminaltruncation. Neuroscience 2000;97:279-284.
45. Bains JS, Shaw CA. Neurodegenerativedisorders in humans: the role of glutathione inoxidative stress-mediated neuronal death.Brain Res Rev 1997;25:335-358.
46. Sechi G, Deledda MG, Bua G, et al. Reducedintravenous glutathione in the treatment ofearly Parkinson’s disease. ProgrNeuropsychopharmacol Biol Psychiatry1996;20:1159-1170.
47. Zhang ZX, Anderson DW, Mantel N, RomanGC. Motor neuron disease on Guam: geo-graphic and familial occurrence, 1956-85. ActaNeurol Scand 1996;94:51-59.
48. Kuhn W, Mueller T, Rommelspacher H.Elevated levels of harman and norharman incerebrospinal fluid of parkinsonian patients. JNeural Transm 1996;103:1435-1440.
49. Zayed J. Environmental factors in the etiologyof Parkinson’s disease. Can J Neurol Sci1990;17:286-291.
50. Hirsch EC, Brandel JP, Galle P, et al. Iron andaluminum increase in the substantia nigra ofpatients with Parkinson’s disease: an x-raymicroanalysis. J Neurochem 1991;56:446-451.
51. Ngim CH, Devathasan G. Epidemiologicalstudy on the association between body burdenmercury level and idiopathic Parkinson’sdisease. Neuroepidemiol 1989;8:128-141.
52. Bocchetta A, Corsini GU. Parkinson’s diseaseand pesticides. Lancet 1986;2:1163.
53. Fleming L, Mann JB, Bean J, et al. Parkinson’sdisease and brain levels of organochlorinepesticides. Ann Neurol 1994;36:100-103.
54. Tanner CM, Langston JW. Do environmentaltoxins cause Parkinson’s disease? A criticalreview. Neurology 1990;40 Suppl.3:17-31.
55. Stephenson J. Exposure to home pesticideslinked to Parkinson’s disease. JAMA2000;283:3055-3056.
56. Vingerhoets FJG, Snow BJ, Tetrud JW, et al.Positron emission tomographic evidence forprogression of human MPTP-induced dopam-inergic lesions. Ann Neurol 1994;36:765-770.
57. McGeer PL, Itagaki S, Boyes BE, McGeer EG.Reactive microglia are positive for HLA-DR inthe substantia nigra of Parkinson’s andAlzheimer’s disease brains. Neurology1988;38:1285-1291.
58. Banati RB, Daniel SE, Blunt SB. Glialpathology but absence of apoptotic nigralneurons in long-standing Parkinson’s disease.Mov Disord 1998;13:221-227.
59. Vawter MP, Dillon-Carter O, Tourtellote WW,et al. TGFbeta1 and TGFbeta2 concentrationsare elevated in Parkinson’s disease in ventricu-lar cerebrospinal fluid. Exp Neurol1996;142:313-322.
60. Mirza B, Hadberg H, Thomsen P, Moos T. Theabsence of reactive astrocytosis is indicative ofa unique inflammatory process in Parkinson’sdisease. Neuroscience 2000;95:425-432.
61. Kuhn W, Roebroek R, Blom H, et al. Elevatedplasma levels of homocysteine in Parkinson’sdisease. Eur Neurol 1998;40:225-227.
62. Chambers JC, McGregor A, Jean-Marie J,Kooner JS. Acute hyperhomocysteinaemia andendothelial dysfunction. Lancet 1998;351:36-37.
63. Surtees R, Hyland K. L-3,4-dihydroxyphenylalanine (levodopa) lowerscentral nervous system S-adenosylmethionineconcentrations in humans. J Neurol NeurosurgPsychiatr 1990;53:569-572.
64. Muller T, Werne B, Fowler B, Kuhn W. Nigralendothelial dysfunction, homocysteine, andParkinson’s disease. Lancet 1999;354:126-127.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 527
65. Ben-Shlomo Y, Marmot MG. Survival andcause of death in a cohort of patients withparkinsonism: possible clues to etiology. JNeurol Neurosurg Psychiatr 1995;58:293-299.
66. Werbach MR. Nutritional Influences onIllness. Tarzana, CA: Third Line Press; 1993.
67. Yamaguchi T, Nagatsu T. Effects of tyrosineadministration on serum biopterin in normalcontrols and patients with Parkinson’s disease.Science 1983;219:75-77.
68. Growdon JH, Melamed E, Logue M, et al.Effects of oral L-tyrosine administration onCSF tyrosine and homovanillic acid levels inpatients with Parkinson’s disease. Life Sci1982;30:827-832.
69. Heller B, Fischer E, Martin R. Therapeuticaction of D-phenylalanine in Parkinson’sdisease. Arzneim Forsch 1976;26:577-579.
70. Lehmann J. Tryptophan malabsorption inlevodopa-treated parkinsonian patients. ActaMed Scand 1973;194:181-189.
71. Lehmann J. Levodopa and depression inParkinsonism. Lancet 1971;1:140.
72. Coppen A, Metcalfe M, Carroll JD, Morris JG.Levodopa and L-tryptophan therapy inParkinsonism. Lancet 1972;1:654-658.
73. Smythies JR, Halsey JH. Treatment ofParkinson’s disease with L-methionine.Southern Med J 1984;77:1577.
74. Clayton PT, Smith I, Harding B, et al. Sub-acute combined degeneration of the cord,dementia and parkinsonism due to an inbornerror of folate metabolism. J NeurosurgPsychiatry 1986;49:920-927.
75. Bender DA, Earl CJ, Lees AJ. Niacin depletionin parkinsonian patients treated with L-dopa,benserazide and carbidopa. Clin Sci1979;56:89-93.
76. Black MJ, Brandt RB. Nicotinic acid or N-methyl nicotinamide prolongs elevated braindopa and dopamine in L-dopa treatment.Biochem Med Metab Biol 1986;36:244-251.
77. Mars H. Effect of chronic levodopa treatmenton pyridoxine metabolism. Neurology1975;25:263-266.
78. Baker AB. Treatment of paralysis agitans withvitamin B6 (pyridoxine hydrochloride). JAMA1941;May 31:2484-2488.
79. Zeligs MA. Use of pyridoxine hydrochloride(vitamin B6) in parkinsonism. JAMA1941;May 10:2148-2149.
80. Sacks W, Simpson GM. Ascorbic acid inlevodopa therapy. Lancet 1975;1:527.
81. Fahn S. A pilot trial of high-dose alpha-tocopherol and ascorbate in early Parkinson’sdisease. Ann Neurol 1992;32:S128-S132.
82. Parkinson’s Study Group. Effects of toco-pherol and deprenyl on the progression ofdisability in early Parkinson’s disease. NewEngl J Med 1993;328:176-183.
83. Pall HS, Williams AC, Blake DR, et al. Raisedcerebrospinal-fluid copper concentration inParkinson’s disease. Lancet 1987;2:238-241.
84. Dexter DT, Wells FR, Lees AJ, et al. Increasednigral iron content and alterations in othermetal ions occurring in brain in Parkinson’sdisease. J Neurochem 1989;52:1830-1836.
85. Uitti RJ, Rajput AH, Rozdilsky B, et al.Regional metal concentrations in Parkinson’sdisease, other chronic neurological diseases,and control brains. Can J Neurol Sci1989;16:310-314.
86. Martinez M, Martinez N, Hernandez AI,Ferrandiz ML. Hypothesis: can N-acetylcysteine be beneficial in Parkinson’sdisease? Life Sci 1999;64:1253-1257.
87. Mena I, Cotzias GC. Protein intake andtreatment of Parkinson’s disease withlevodopa. New Engl J Med 1975;292:181-184.
88. Tsui JK, Ross S, Poulin K, et al. The effect ofdietary protein on the efficacy of L-dopa: adouble-blind study. Neurology 1989;39:549-552.
89. Carter JH, Nutt JG, Woodward WR, et al.Amount and distribution of dietary proteinaffects clinical response to levodopa inParkinson’s disease. Neurology 1989;39:552-556.
90. Pare S, Barr SI, Ross SE.. Effect of daytimeprotein restriction on nutrient intakes of free-living Parkinson’s disease patients. Am J ClinNutr 1992;55:701-707.
91. Logroscino G, Marder K, Cote L, et al. Dietarylipids and antioxidants in Parkinson’s disease:a population-based, case-control study. AnnNeurol 1996;39:89-94.
92. Walford RL, Walford L. The Anti-Aging Plan.New York: Four Walls Eight Windows; 1995.
93. Kidd PM. Cell membranes, endothelia, andatherosclerosis - the importance of dietary fattyacid balance. Altern Med Rev 1996;1:148-167.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Page 528 Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000
94. Frackelton JP, Christensen RL. Mercurypoisoning and its potential impact on hormoneregulation and aging: preliminary observationusing a new therapeutic approach. J Adv Med1998:11:9-25
95. van Zandwijk N. N-Acetylcysteine (NAC) andglutathione (GSH): antioxidant andchemopreventive properties, with specialreference to lung cancer. J Cell Biochem1995;Suppl 22:24-32.
96. Cathcart RF. Vitamin C (Ascorbate): Compre-hensive History and Protocols. Los Altos,California, USA: www.orthomed.com; 2000.
97. Shults CW, Haas RH, Passov D, Beal MF.Coenzyme Q10 levels correlate with theactivities of complexes I and II/III in mito-chondria from parkinsonian andnonparkinsonian subjects. Ann Neurol1997;42:261-264.
98. Critchley EMR. Evening primrose oil (Efamol)in parkinsonian and other tremors. In: ClinicalUses of Essential Fatty Acids, Horrobin DF ed.Montreal: Eden Press; 1982.
99. Caughey GE. Effect on tumor necrosis factoralpha and interleukin 1-beta production ofdiets enriched in n-3 fatty acids from vegetableoil or fish oil. Am J Clin Nutr 1996;63:116-122.
100. Youdim KA, Martin A, Joseph JA. Essentialfatty acids and the brain: possible healthimplications. Intl J Dev Neurosci 2000;18:383-399.
101. Snider SR. Octacosanol in Parkinsonism. AnnNeurol 1984;16:723.
102. Gotz ME, Gerstner A, Harth R, et al. Alteredredox state of platelet coenzyme Q10 inParkinson’s disease. J Neural Transm2000;107:41-48.
103. Shults CW, Beal MF, Fontaine D, et al.Absorption, tolerability, and effects onmitochondrial activity of oral coenzyme Q10in parkinsonian patients. Neurology1998;50:793-795.
104. Birkmayer GJD, Birkmayer W. Stimulation ofendogenous L-dopa biosynthesis - a newprinciple for the therapy of Parkinson’sdisease. Acta Neurol Scand Suppl1989;126:183-187.
105. Birkmayer JGD, Vrecko C, Volc D, BirkmayerW. Nicotinamide adenine dinucleotide(NADH) - a new therapeutic approach toParkinson’s disease. Acta Neurol Scand Suppl1993;146:32-35.
106. Kuhn W, Muller T, Winkel R, et al. Parenteralapplication of NADH in Parkinson’s disease:clinical improvement partially due to stimula-tion of endogenous levodopa biosynthesis. JNeural Transm 1996;103:1187-1193.
107. Kidd PM. A review of nutrients and botanicalsin the integrative management of cognitivedysfunction. Altern Med Rev 1999;4:144-161.
108. Steffen V, Santiago M, de la Cruz CP, et al.Effect of intraventricular injection of 1-methyl-4-phenylpyridinium: protection by acetyl-L-carnitine. Hum Exp Toxicol 1995;14:865-871.
109. Fünfgeld EW, Nedwidek P. Neurohomologousphosphatidylserine in Parkinsonian patientswith associated disorders of cerebral metabo-lism. Clin Trials J 1987;24:42-61.
110. Laihinen A, Ruottinen H, Rinne JO, et al. Riskfor Parkinson’s: twin studies for the detectionof asymptomatic subjects using (18F)6-fluorodopa PET. J Neurol 2000;247 Suppl.2:II110-113.
111. Brooks DJ. Morphological and functionalimaging studies on the diagnosis and progres-sion of Parkinson’s disease. J Neurol 2000;247Suppl. 2:11-18.
112. Piccini P, Burn DJ, Ceravalo R, et al. The roleof inheritance in sporadic Parkinson’s disease:evidence from a longitudinal study of dopam-inergic function in twins. Ann Neurol1999;45:577-582.
113. Morrish PK, Rakshi JS, Bailey DL, et al.Measuring the rate of progression and estimat-ing the preclinical period of Parkinson’sdisease with (18F)dopa-PET. J NeurolNeurosurg Psychiatry 1998;64:314-319.
114. Riederer P, Sian J, Gerlach M. Is thereneuroprotection in Parkinson’s syndrome? JNeurol 2000;247 Suppl 4:8-11.
115. Green PS, Simpkins JW. Neuroprotectiveeffects of estrogens: potential mechanisms ofaction. Intl J Dev Neurosci 2000;18:347-358.
116. Snyder SH. No NO prevents parkinsonism.Nat Med 1996;2:965-966.
117. Lu X, Bing G, Hagg T. Naloxone preventsmicroglia-induced degeneration of dopaminer-gic substantia nigra neurons in adult rats.Neuroscience 2000;97:285-291.
118. Akaneya Y, Takahashi M, Hatanaka H.Interleukin-1ß enhances survival andinterleukin-6 protects against MPP+ neurotox-icity in cultures of fetal rat dopaminergicneurons. Exp Neurol 1995;136:44-52.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission

Parkinson’s Disease
Alternative Medicine Review ◆ Volume 5, Number 6 ◆ 2000 Page 529
119. Diederich NJ, Goetz CG. Neuropsychologicaland behavioral aspects of transplants inParkinson’s disease and Huntington’s disease.Brain Cognit 2000;42:294-306.
120. Eriksson PS, Perfilieva E, Bjork-Eriksson T, etal. Neurogenesis in the adult human hippocam-pus. Nat Med 1998;4:1313-1317.
121. Nakao N, Yokote H, Nakai K, Itakura T.Promotion of survival and regeneration ofnigral dopamine neurons in a rat model ofParkinson’s disease after implantation ofembryonal carcinoma-derived neuronsgenetically engineered to produce glial cellline-derived neurotrophic factor. J Neurosurg2000;92:659-670.
122. Offen D, Sherki Y, Melamed E, et al. Vasoac-tive intestinal peptide (VIP) prevents neurotox-icity in neuronal cultures: relevance toneuroprotection in Parkinson’s disease. BrainRes 2000;854:257-262.
123. NINDS (National Institute of NeurologicalDiseases and Stroke), USA. Parkinson’sDisease: A Research Planning Workshop.Bethesda, MD, USA: Office of Scientific andHealth Reports (tel.301-496-5751), NINDS,National Institutes of Health; 1999.
Correction
Alternative Medicine Review vol 5(4);Peripheral Metabolism of ThyroidHormones: A Review, by Greg Kelly, ND.Page 319, left column, third paragraphshould read: Ketones generated fromcalorie deprivation appear to have asuppressive effect on T3 generation andhepatic type I 5’-deiodinase activity.
Copyright©2001 Thorne Research, Inc. All Rights Reserved. No Reprints Without Written Permission


![[ 150 ] THE GROWTH OF EMBRYONIC NEURITES](https://static.fdocuments.net/doc/165x107/5899a4701a28ab05468b817f/-150-the-growth-of-embryonic-neurites.jpg)