Ocular toxoplasmosis
-
Upload
pragyarai53 -
Category
Science
-
view
308 -
download
4
description
Transcript of Ocular toxoplasmosis

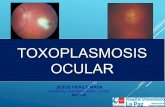
OCULAR TOXOPLASMOSIS
PRAGYA RAI PG-2

• Definition: Ocular toxoplasmosis is a recurrent retinochoroiditis.
• Caused by the organism Toxoplasma gondii, and represents the most common cause infectious posterior uveitis worldwide.

• Toxoplasmosis Represents the main cause of infectious posterior uveitis worldwide and may lead to visual threatening complications including severe retinochoroidal scarring, vitreous opacities, cataracts, glaucoma and choroidal neovascularization.

ORGANISM AND LIFE CYCLE
• Intracellular parasites, capable of infecting virtually any warm-blooded animal and establishing life-long chronic infection.
• Domestic cat represents the archetypical definite host for T. Gondii.
• Three forms• Sporozoites• Trachyzoite• Bradyzoit (tissue cyst)

• Sporozoites contained within an oocyst and result from sexual reproduction of the organisms with the intestinal mucosa of cat.
• Bradyzoites are relatively inactive and are contained within tissue cyst , commonly develop in brain , eye, heart , skeletal muscles and lymph nodes.
• The tachyzoite is the active proliferating form, present in intermediate and definite hosts during acute infection.
• It is able to penetrate any nucleated cell and circulate all over the body, leading to cell lysis, direct tissue
damage.

• Tachyzoites differentiate into bradyzoites, forming tissue cysts.
• The definite host becomes infected by either ingesting meat containing tissue cysts/tachyzoites from intermediated hosts, or by ingesting sporulated oocysts, present in the soil and shed in the feces of another feline host.

• These maturate in the soil into sporulated oocysts, becoming infective after 1–21 days, and persisting in the environment for up to 18 months.
• Transplacental transmission in recently infected hosts, and more rarely laboratory accidents and organ transplantation, are other possible modes of infection.

Transmission
• Beef• Undercooked lamb , pork, chicken• Environment contaminated by feces of
infected cats family• Organ transplantation• Blood transfusion• Water

EPIDEMIOLOGY
• United States antibodies to T. gondii are found in nearly 20% of the human population.
• France, as well as in South America this rate reaches up to 80%
• first trimester of pregnancy, rates of transplacental infection are around 10–25%, and progressively increase to reach 60–80% in the third trimester.

• Congenital toxoplasmosis used to be blamed for most cases of ocular toxoplasmosis.

pathology
• Histopathologically , active ocular toxoplasmosis is manifest as a focal retinochoroiditis with necrotizing granulomatous inflamation of the retina ,choroid viterous and ant. uveal tract.
• Mononuclear inflamatory infiltrates are present.• Disruption / migration of RPE is observed.• Inflammatory process can extend to underlying
sclera.


Pathogenesis• Depend upon a delicate balance b/w
hostimmunity and parasite virulence.• Immunoimmaturity associated with congenital
toxoplasmosis clearly asst. with systemic and ocular lesions .
• Some are related to disruption of embryogenesis and fetogenesis.

• In immunocompetent patients with postnatal infection , a small number of these individuals develop ocular disease soon after seroconversion.
• The local innate immune response driven by a variety of cells including polymorphonuclear leukocytes , macrophages , B/T lymphocytes and NK cells.

• Other such as dendritic cells , also help to trigger the adaptive immune response.
• The adaptive immune response is mainly coordinated by CD4+T lymphocytes and macrophages.
• CD8+t lymphocytes are also cytotoxic to infected cells.

• Parasite virulence is also an important determination of pathogenesis
• Type 1 are highly virulent • Type 2 are the lest virulent• Type 3 are also lest virulent

In Immunosuppressed• Have both tachyzoites and tissue cysts in
areas of retinal necrosis and within retinal pigment epithelial cells.
• Parasites can occasionally be found in the iris, choroid, vitreous, and optic nerve

CLINICAL MANIFESTATIONS• Systemic disease-Immunocompetent individuals with postnatally
acquired toxoplasmosis are frequently asymptomatic.
• Some develop fever, malaise and variable lymphadenopathy.
• Only a small number evolve to severe systemic disease, including pneumonitis, hepatitis, myocarditis and even encephalitis.
• Immunocompromised individuals, especially those with AIDS , are susceptible to life threatening disease .(neurotoxoplasmosis)

• Congenital toxoplasmosis is associated with a large spectrum of systemic manifestations, ranging from intrauterine death/severe malformations to a neonatal infectious syndrome including anemia,thrombocytopenia, cutaneous rash, hepatitis, pneumonitis, myocarditis and even encephalitis.

Ocular presentation
Symptoms • Floaters• Reduced central vision • Metamorphopsia• photophobia
Sign (The hallmarks)• Vitreous inflammation• Anterior uveitis• Retinal vasculitis is also
present (occationally) • These active lesions
associated with more severe vitreous haze can typically display a ‘headlight-in-the-fog’
• Intraocular pressure is elevated in 10–30% of these cases.

necrotizing retinochoroiditisSatellite lesion adjacent to old hyperpigmented scars The typical wagon-wheel scar in the
macula

Lipidic exudates (kyrieles arteriolitis) Herpetic retinitis

• New or Acute lesion– Intensely white– Focal lesion overlying vitreous inflammatory haze
(head light in the fog)– Acute anterior uveitis
• Healed lesion– Border become more defined– Hyperpigmented after several months– Large scar will have atrophic center (devoid of all
choroidal retinal elements)


Investigation
• Serological test-presence of IgG antibodies specific to T. gondii and denoting previous exposure to it. Absence of specific IgG and IgM virtually excludes the possibility of toxoplasmosis.
• Congenital toxoplasmosis, specific IgM and/or IgA antibodies and/or persistently high levels of specific IgG antibodies to T. gondii after 12 months of life seal the diagnosis.

• (PCR) of ocular fluids-The former is possible through calculation of the Goldman-Witmer or Witmer-Desmonts coefficient, based on the correlation between titers of specific antibodies to T. gondii in aqueous humor/serum, versus the globulin titers in the same fluids.
• A high coefficient indicates intraocular synthesis of anti-T. gondii antibodies, and a low coefficient has an opposite interpretation, although this may also occur in the setting of severe disruption of the blood-ocular barrier.

• Sabin-Feldman dye test <1:16 or 1:32 is negative• Western blot analysis (identify membrane and cytoplasmic antigen)• ELISA• Indirect fluorescein antibody test.(IFA)• Hemagglutination test.• Indirect hemagglutination test
• Imaging modalities including echography, fluorescein or indocyanine green angiography, as well as optical coherence tomography are seldom decisive to the diagnosis.
• X-ray skull • CT and MRI

DIFFERENTIAL DIAGNOSIS OF PRIMARY OR RECURRENTTOXOPLASMIC RETINOCHOROIDITIS
• Infectious• Bacterial• Syphilis• Tuberculosis• Bartonellosis (neuroretinitis, focal retinitis, and
angiomatous lesions)• Lyme disease• Endogenous endophthalmitis• Others

• Viral• Acute retinal necrosis/necrotizing herpetic retinopathy• CMV retinitis• Progressive outer retinal necrosis• Others• Fungal• Candidiasis (particularly endogenous endophthamitis)• Aspergillosis• Others• Parasitic• DUSN • Toxocariasis• Others

• Noninfectious• Associated with systemic disease• Behçet’s disease• Sarcoidosis• Others• Primarily not associated with systemic disease• Serpiginous/ampiginous choroiditis and others• Multifocal choroiditis and panuveitis• Punctate inner choroidopathy• Multiple evanescent white dots syndrome• Unilateral acute idiopathic maculopathy• Others• Neoplastic• Primary vitreoretinal lymphoma

ComplicationNearly 25 % of eyes develop visual loss as a result of the following-Common – • Direct involvement of the macula .• Secondary ON head involvement due to a juxtapapillary lesion
Uncommon-Primary ON head involvement Occlusion of a major blood vesselChoroidal neovascularization Serous RDTractional RDMacular oedema.

Treatment and Prevention
• Available drugs do not eliminate tissue cysts and cannot prevent chronic infection
• No treatment has proven to be superior or even more effective than no treatment
• Antitoxoplasmic agents and systemic steroids have never been studied in large clinical trials

Drug and dosage Precautions and observations
Sulfadiazine 1 g QID in adults50-100 mg/kg/day in children
Caution and dose correction for hepatic renalfailure.Contraindicated in G6PDH deficiency.Hydration and alcalinization of urine may preventcrystalluria.Avoid at the end of gestation (risk of kernicterus).Hypersensitivity and allergies demand suspension.Stevens-Johnson syndrome possible but rare.Bone marrow suppression in < 0.1%.
PyrimethamineLoading dose of 100 mg, followedby 25–50 mg/day1 mg/kg/day in children
Caution in hepatic or renal failure.Contraindicated in first trimester (teratogenic).Common gastrointestinal disturbances.Risk of bone marrow depression demandsconcomitant use of folinic acid (5–7.5 mg/dayor 15 mg 3×/week) and periodic CBCmonitoring

Clindamycin300 mg qid10–25 mg/kg/day in children
Caution in hepatic or renal failure.Common gastrointestinal disturbances. Risk ofpseudomembranous colitis (suspend if bloodydiarrhea
Azithromycin250–500 mg/day5 mg/kg/day in children
Food decreases oral absorption.Gastrointestinal disturbances in less than 10%.May be used in pregnancy.

Sulfamethoxazole/ trimethoprim800 mg/160 mg bid40–50 mg/8–10 mg/kg/day inchildren
Better tolerated than classic therapy, but probablyless effective.Caution and dose correction in case of hepatic/renal failure. Contraindicated in G6PDHdeficiency.Avoid during gestation (risk of teratogeny andkernicterus).Risk of sulfa hypersensitivity.Bone marrow suppression uncommon.
Spiramycin1.5 million IU (500 mg) qid
Atovaquone750 mg qid30 mg/kg/day in children
High levels in placenta.Safest antiparasitic drug in pregnancy.Limited intraocular penetration.Gastrointestinal disturbances and hypersensitivity.
Caution with liver failure.Food increases drug absorption.Maculopapular rash in up to 20%.No safety studies concerning gestation / lactation.

MAIN FACTORS INFLUENCING TREATMENTDECISION ON ACTIVE TOXOPLASMIC RETINOCHOROIDITIS
• Immune status of the individual• Location and size of the active lesion• Presence of macular and/or optic disc edema• Degree of vitritis and of decreased vision• Clinical course• Special situations (newborns, pregnant women, drug
allergy)• Adverse effects of antiparasitic drugs and corticosteroids

Primary prophylactic measures are essential in seronegative women right before and during pregnancy and in immunosuppressed patients.
These measures include:
• Avoiding ingestion of raw/undercooked meat (freezing at −20°C/−4°F
• overnight also destroys tissue cysts);• Drinking only well-filtered or boiled water;• Carefully washing vegetables/fruits before consumption;• Using gloves and washing hands/kitchen utensils after
manipulating• meat/soil;• Avoiding contact with felines and their feces (even in soil or litter• boxes).• Monthly serologic screening of susceptible women during
pregnancy is also highly recommended.

COURSE AND PROGNOSIS
• Toxoplasmic retinochoroiditis is a recurrent disease, with up to two thirds of patients developing reactivations later in life. These are more common in congenital than in postnatally acquired toxoplasmosis, and occur especially in the first year after the previous episode.
• Some patients, however, sustain long-lasting disease remission

• Prognosis depends on the immune status and age of the patient, as well as on the size and location of the lesions
• Local complications such as persistent vitreous opacities, macular edema, epiretinal membranes, extensive retinochoroidal scarring, choroidal neovascularization, optic atrophy and even retinal detachment may be associated with significantly decrease.

THANK YOU