Nursing Magazine, For Hartford Hospital Nurses and Alumnae ... Library/Publications/Nursing...
Transcript of Nursing Magazine, For Hartford Hospital Nurses and Alumnae ... Library/Publications/Nursing...

NursingFor Hartford Hospital nurses and alumnae of the Hartford Hospital School of Nursing
Spring 2014
A Framework For Nursing Practice• Transforming Care Systemwide
• Best Practices In Breastfeeding
• New Council Promotes Research
Plus: Nightingale Awards • A Look Back

NursingEditorial StaffAmanda BlaszykHelayne LightstoneRebecca Stewart
WriterNoreen Kirk
DesignerAlan Colavecchio
PhotographyCill Russo
Advisory Board
Cheryl Ficara, RN, MS, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCare
Gail Nelson, RN, MS, NEA-BCDirector of Professional Development and Performance ImprovementHartford Hospital
Betty Ann Fusco, RNPresident, Alumnae Association of the Hartford Hospital School of Nursing, HHSN ’66
Patricia Andreana Ciarcia, RN, MSNExecutive Director of Alumnae Affairs, Alumnae Association of the Hartford HospitalSchool of Nursing, HHSN ’62
Hartford Hospital Nursing is a publicationof the Hartford Hospital Department ofNursing and the Alumnae Association ofthe Hartford Hospital School of Nursing.
Send correspondence to:Hartford Hospital Nursing80 Seymour StreetHartford, CT 06102-5037Attention: Cheryl Ficara, RN, MS, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCaree-mail: [email protected]
Alumnae Association of the Hartford Hospital School of Nursing560 Hudson StreetHartford, CT 06106Attention: Pat Ciarcia, RN, MSNExecutive Director of Alumnae Affairse-mail: [email protected]: 860.563.2005
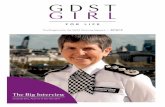
On the cover:
Ryan Reinsch, RN, a nurse in theemergency department’s behavioral healthunit – the “purple pod.”
Photo by Cill Russo
Contents
1 Messages From Executive Leadership
2 A Framework For Nursing Practice
3 The ADVOCACY Of NursingInnovation In Patient Flow
4 The ADVOCACY Of NursingTransforming Care Systemwide
5 The ART Of NursingCollaborating For Better Care
6 The ART Of NursingBest Practices In Breastfeeding
7 The ETHICS Of NursingHonoring The Patient
8 The SCIENCE Of NursingNew Council Promotes Research
9 Nightingale Awards
10 Nursing News & Notes
11 A Message From The President Of The Alumnae Association
12 Alumnae SpotlightInspired By Opportunity
13 A Look BackA Woman Of Many Talents
14 The PILLBOX Alumnae NewsNews and photos from our graduates
17 In Memoriam

1HARTFORD HOSPITAL NURSING / SPRING 2014
Evidence-Based CareIs The Best Care
Why did you decide to become anurse? If you’re like most of us, youwanted to help heal or comfortpeople who were sick or injured. So,if you learned that something couldbenefit your patient, you’d naturallyembrace it wholeheartedly in yourown practice. That is what evidence-
based practice is all about: doing what is best for our patients.And that’s why employing best practices on every unit, everyday, for every patient, must be a top priority for all of us.
Best practices are discovered through research, which isrelated to the science element of our Nursing ProfessionalPractice Model. Yet best practices exist in every aspect ofnursing, including art, advocacy and ethics. Ourresponsibility as nurses is to learn what those best practicesare so we can use them to benefit our patients. The waywe’ve always done something might not be the best way. It’svital that we question the status quo, discover what theevidence says works best for patients, and then put thatknowledge into practice at the bedside.
The new Council for Innovation and Transformation willhelp us do this. The CIT’s mission is to help nurses connectwith research, identify best practices and then incorporatethose practices in their daily care. The council will play akey role in stimulating nursing’s spirit of inquiry—the spiritthat will help ensure that we take our practice to the veryhighest levels.
We know from experience that implementing bestpractices benefits patients. Adopting evidence-basedpractices has helped us dramatically reduce patient fallsand the development of pressure ulcers, for example. As wework together to employ best practices in other respects, I’mconfident we’ll enhance patient outcomes in those areas, aswell.
In nursing, as in life, balance is key. The facts andstatistics drawn from research are important, but so are themore intangible qualities of an excellent nurse. We see thisin nurses who help patients and families decide whether tocontinue high-tech interventions. We see it in the creativecollaboration among nurses and others who recently re-envisioned and redesigned the purple pod to ensure morecompassionate, dignified care for behavioral health patientsin crisis. The examples are endless.
The beauty of our Nursing Professional Practice Model isthat it illustrates the critical integration of all aspects ofnursing—the essential balance that translates into a betterhuman experience for everyone whose life is touched by anurse.
Thank you for all you do.
Cheryl Ficara, RN, MS, NEA-BCVice President, Patient Care ServicesHartford Region, Hartford HealthCare
Nurses And The FutureOf Hartford Hospital
It’s a privilege to share somethoughts with you in thispublication for the first timesince assuming my position lastfall. I’ve seen Hartford Hospital’sNursing magazine many timesover the years, and have found
it to be a great vehicle for spotlighting the invaluablecontributions nurses make to the well-being ofpatients and families and to the organization as awhole.
Those of you I’ve had the chance to work withknow that I have the greatest respect for nurses. Askilled, knowledgeable, caring nurse by the bedside isone of the greatest advantages a patient can have. Itis the bedside nurse who sees the patient most often,gets to know the patient and family, administerstreatments and monitors progress. You are theiradvocate, their voice, the one who listens to theirconcerns and helps them understand the oftenconfusing language and process of medical care.When patients and families reflect on theirexperience at Hartford Hospital, what they tend toremember most clearly is the nurse who gave themcare and comfort at the bedside.
As a physician, I’ve always considered nurses mypartners in clinical care. Close collaboration betweenphysicians and nurses has been one of the mostpositive developments in medicine in recent decades.Together with our colleagues from a variety ofdisciplines, we form a highly effective team—oneable to obtain the best possible outcomes forpatients.
Today, Hartford Hospital, like hospitals nationwide,is facing unprecedented challenges. Nurses play apivotal role in our ability to meet those challengesand remain a solvent, viable organization. Successdepends on you—on your commitment to discoveringand adopting best practices, your willingness to breakdown “silos” and collaborate across disciplines anddepartments, and your eagerness to evolve andchange as circumstances demand.
I look forward to celebrating nursing’scontributions to health care during Nurses Week2014 and to working with you over the months aheadto shape a successful future for Hartford Hospital.
Stuart K. Markowitz, MD, FACRPresident, Hartford HospitalSenior Vice President, Hartford HealthCare
Messages From Executive Leadership

2 HARTFORD HOSPITAL NURSING / SPRING 2014
A Framework For Nursing Practice
Hartford Hospital nurses introduced the hospital’s currentNursing Professional Practice Model in early 2013. Themodel was the result of months of work by nurses frommany areas throughout the hospital. Their goal was todevelop a visual representation that defined the scope ofnursing practice and that would enable consistency ofpractice across all specialties.
Hartford Hospital’s four core values of excellence,
integrity, caring and safety form the foundation of themodel. Enhancing the human health experience is at thecenter, because this is the focus of all nursing practice. Fourinterrelated elements surrounding the center show thevarious aspects of nursing: advocacy, art, ethics andscience. The breadth of these elements underscores thebroad background, knowledge, talent and skill that nursesdraw on in providing care.
The six stories on the following pages show how nursesat Hartford Hospital are putting the model into practiceevery day, whether it’s providing direct care to patients ordeveloping new processes and approaches that will benefitall patients, now and in the future.
Nursing Professional Practice Model
The Nursing Professional Practice Model is a visual symbol of the complex undertakingthat is nursing.

3HARTFORD HOSPITAL NURSING / SPRING 2014
•• The ADVOCACY Of Nursing
How can we expedite the flow of patients through theemergency department while continuing to provideexcellent care? That’s the question that nurses and otherssought to answer when they formed the interdepartmentalEmergency Department-Inpatient Medical Nursing PatientFlow Team last fall. “We wanted to redesign the flow,improve overall response to patients who were waiting,reduce the number of patients leaving without being seenand expedite all patients to the appropriate level of care,”says team co-leader Michael Davis, RN, MBA, NE-BC,director of medical nursing. “By expediting care, we areadvocating for the health and well-being of our patients.”
Mr. Davis and team co-leader Danette Alexander, RN,MSN, NEA-BC, nurse director of emergency services andLIFE STAR, assembled a team that included staff nursesfrom N11, CB5 and the ED; nurse managers; patientsupport staff; a clinical informatics specialist and H3Wfacilitators. The group used “lean” methodologies and afive-day rapid-improvement process known as “kaizen” todiagram patient flow and identify ways of improving it.
The team found that patient flow was often hindered bydelays in transporting ED patients with telemetry monitorsup to inpatient units. Such patients must be monitored by anurse during transport. ED nurses were performing thatrole, but that meant they were out of the ED for 15 to 20hours each day, which contributed to a backup of patientsin the ED. The solution? Change the process so that, when
the patient was ready to go up, the unit nurse would meetthe patient in the ED and accompany him or her to theinpatient unit.
Janet Smith, RN, of CB5, one of the nurses on the team,says she was skeptical about the plan at first, but soonrealized it worked well for all concerned. “Patients are reallyhappy to meet their nurse in the ED,” she says. “It reducesanxiety in patients and families because they’re meetingthe nurse ahead of time.” She adds that “it opens a windowfor you to focus on this admission. Before, you might nothave had a chance to go through their plan of care rightaway. Now, you can dedicate yourself to the patient.”
Jennifer Parkington, RN, of N12, was among the first tolearn about the new process. She soon became a championfor it, explaining it to other nurses on her unit. Severalraised concerns about taking time to leave the floor. “Butit’s not wasted time,” Ms. Parkington says. “You can startyour assessment right in the ED.” She adds, “Quite honestly,I think it helps a floor nurse plan her admission a littlebetter. Before, you could be in the middle of a med pass or afamily crisis and not be prepared to take an admission. Thisway, we have a window of time to plan for the admission.”
After the process was implemented on two inpatientunits, the ED saw reductions in length of stay, number of patients leaving without being seen, time from patientarrival to first ED location, and time between bedassignment and arrival on admitting unit.
The most important effect of the change, JenniferParkington says, is that “Ultimately, it benefits the care ofthat patient.” •
Jennifer Parkington, RN, of N12, prepares to accompany a patient from the emergencydepartment to her unit. Transporting the patient is Royan Johnson, transport aide.
A new system for transferring ED patients toinpatient units proves highly successful.
Innovation In Patient Flow

4 HARTFORD HOSPITAL NURSING / SPRING 2014
Nurses Melissa Hernandez, RN, BSN; and Jamie Houle, RN, BSN;with Julie Michaelson, RN, consulting analyst with the clinicalinformatics department. They’re among scores of nurses involvedin the CareConnect initiative.
•• The ADVOCACY Of Nursing
Transforming Care Systemwide
Hartford HealthCare Senior Vice President and ChiefMedical Officer Rocco Orlando, MD, may have summed upthe importance of the CareConnect project best when hesaid, “CareConnect is the largest and most ambitioussystem-wide effort ever at Hartford HealthCare and it willhave a huge impact on our patients and families.” Thiswide-ranging undertaking seeks to transform patient careby creating an electronic system that will ensure safe,coordinated, evidence-based care that is consistent acrossall HHC entities. It’s a tall order—one that’s drawing on theexpertise of hundreds of people from throughout thesystem. Many of them are nurses at Hartford Hospital.
Susan Marino, RN, CPHIMS, Hartford HealthCare’s chiefnursing informatics officer, says that nurses are crucial tothe success of the initiative. “Nurses coordinate care at thebedside,” Ms. Marino says. “They understand thecomplexities of managing and planning care incollaboration with every discipline. Nurses are keenly awareof and can articulate workflow challenges, safety issuesand transitions of care—elements important to our futuresystems design.”
By taking part in the CareConnect process, Ms. Marinosays, “Nurses are advocating for nursing practice and forpatient care.”
Nurses serve on HHC’s Clinical Informatics Team and theCareConnect Core Team—groups that are spearheading theoverall effort.
A number of Hartford Hospital nurses have been tappedto take part in a series of validation sessions where theywill provide input on the design of the system. They willalso serve as subject matter experts when CareConnect isimplemented, training others and providing support duringthe rollout.
Melissa Hernandez, RN, BSN, clinical leader of themedical ICU, and Jamie Houle, RN, BSN, of thecardiothoracic ICU, are two of these subject matter experts.
Both took part in a recent validation session.“It’s great to have input into how we’ll integrate this into
care, since we are the end users,” Ms. Hernandez says. “Ourgoal is to have the system reflect what we do in nursingcare, how we make decisions and what we do every day forour patients.”
“It’s nice to be able to say, ‘This is what I would like tosee,’ as opposed to having somebody who doesn’t sit at thebedside say, ‘This is what you’re going to do,’” Mr. Houlesays. “It’s really empowering, especially knowing that this isgoing to impact your day-to-day job.”
Commenting on the future implementation ofCareConnect, Mr. Houle says that, while change is oftendifficult, “People should keep in mind that this is a terrificthing for our patients, and we will be there to help them. Ithink it’s a tremendous step in the right direction and willhave a good impact on everybody involved.” •
Nurses and other team members who participated in a CareConnect validation session in March 2014.
Nurses are contributing their clinical expertiseto CareConnect.

Unprecedented collaboration between Hartford Hospital’semergency services and the Institute of Living hastransformed care in the emergency department’sbehavioral health unit, known as the purple pod. Thecollaborative effort, called the Emergency DepartmentBehavioral Health Initiative, was launched in June 2012with the goal of enhancing the quality of care.
“The leadership from both specialties agreed it was timeto create a physically and emotionally safe environment forthese patients and transform the way care is delivered,”says Danette Alexander, RN, MSN, NEA-BC, nurse director of emergency services and LIFE STAR.
An H3W team was formed with executive sponsorshipfrom Cheryl Ficara, RN, MS, NEA-BC, vice president ofpatient care services, and Hank Schwartz, MD, vicepresident of behavioral health and psychiatrist-in-chief ofthe IOL. The group included physicians, nurses andadministrators from both departments, as well asrepresentatives from security and facilities.
“One of the first things we discovered was the need todisrupt the ‘us’ versus ‘them’ mentality,” says Mrs.Alexander. “Inside the purple pod, we have emergencynurses and psychiatric clinicians. The biggest hurdle waskeeping the patient in the center—saying ‘What does thispatient need?’ rather than ‘What do the separatedisciplines need?’”
The initial conversations centered on whether these wereED patients or IOL patients. The group ultimately decidedthat, while these patients have mental health issues, theyare in crisis just like any other patient coming into the EDand therefore should be managed in the ED. Once this wasestablished, participants could begin the work ofdetermining how to integrate best practices into care ofpatients in psychiatric crisis.
Over the course of the initiative, team membersimproved communications and developed strong,collaborative working relationships. Mrs. Alexanderexplains, “We had to learn each other’s realities—to havepsychiatry staff understand what was going on in the EDand ED staff understand what behavioral health patientsneeded.”
To further increase understanding of the behavioralhealth patient in crisis, IOL Nurse Director Ellen Blair,APRN, NEA-BC, arranged for psychiatric educators toprovide regular educational sessions for ED staff.
The team went on to recommended sweeping physicalchanges that would create a state-of-the-art facilitydesigned to enhance patient safety and privacy andpreserve each patient’s dignity. “The overarching impetusfor everything was to maintain dignity of the patient,” saysMrs. Alexander.
The renovated purple pod features 23 treatment areas.Spaces are designed to facilitate quiet, dignity and safety.Many of the rooms have special lighting that helps patientsfeel calmer. The flow of patients from the main ED to thepurple pod is streamlined and promotes safety. Theenclosed nurses’ station allows clinicians to discusspatients or give report without being overheard.
“The difference is night and day,” says Ryan Reinsch, RN, a nurse in the ED purple pod. Psychiatric patients, headds, are typically already suffering from a loss of control.“You want them to be safe, but you want to give them backsome control and try to build trust and a therapeuticrapport. This new environment helps us do that.”
Kathryn Delaney, RN, who also works in the ED purplepod, has noticed a dramatic reduction in the number ofpatients who need to be restrained. In the former, crampedpurple pod, where patients could see and hear one another,one patient’s acting out often escalated to others. “It wouldbe like a domino effect,” she says. “Now restraints are rare.”
The redesigned unit also promotes continuedcollaboration and better patient care, Ms. Delaney says.“Now we and the psychiatry clinicians share the samespace instead of having separate areas. We’re more in theloop, and interventions are made more quickly becauseclinicians are out among the patients.”
The process of transferring patients from the purple podto the appropriate level of care at the IOL has alsoimproved, says Mr. Reinsch. “It takes the cooperation of thepurple pod and psychiatry staff. It’s a team approach. Likeanything else, you can’t be effective without a team.” •
5HARTFORD HOSPITAL NURSING / SPRING 2014
•• The ART Of Nursing
Multidisciplinary collaboration is enhancing carein the emergency psychiatric unit.
Psychiatric Nurse Educator Ruth Reiser, APRN, discusses a patientwith Ryan Reinsch, RN.
Collaborating For Better Care

Hartford Hospital is proud tohave earned the prestigiousBaby-Friendly designation forthe last 14 years. Baby-Friendly status is awarded tohospitals that demonstratethey use best practices toencourage new mothers tobreastfeed their babies. Thedesignation is awarded byBaby-Friendly USA, a nonprofitgroup that advocates for theuse of breastfeeding guidelinesdeveloped by the World HealthOrganization and UNICEF.Those guidelines are aimed atencouraging breastfeedingworldwide to promote child health and reduce infantmortality.
Winning the Baby-Friendly designation is challenging.Through a site visit and comprehensive documentation,hospitals and birthing centers must demonstrate that theyfollow the Ten Steps to Successful Breastfeeding (seesidebar), and the multiple, detailed steps within each one.
Mary Marshall-Crim, FNP/BC, IBCLC, APRN, unit leader ofHartford Hospital’s Lactation Program, says the hospital isconstantly enhancing its efforts to meet and maintainBaby-Friendly’s criteria of 75 percent of mothers choosingto breastfeed exclusively, as well as the Joint Commission’sgoal of 80 percent. Recent innovations include renovationsto the postpartum unit that will allow mothers andnewborns to be together as much as possible—somethingknown to encourage breastfeeding. The hospital alsoprovides a constellation of educational and other servicesto promote breastfeeding. It recently expanded its servicesto include outpatient lactation consultations, available byappointment, and a weekly support group.
But postpartum nurses also bring the art of nursing tobear every day, Ms. Marshall-Crim says, through educationand sensitivity to each new mother’s needs. “It is an art toteach that mother and to support her in what she knows,”Ms. Marshall-Crim says. “It’s a very sensitive, vulnerabletime for her, and we try to make her feel confident and notundermine what she may already know.”
The nurses on the unit, all of whom have extensivetraining in lactation education and breastfeedingmanagement, take special care to understand what eachmother and baby needs and to provide information andsupport tailored to those needs. “We try to give themfactual information, but also support the intuition theymay have,” Ms. Marshall-Crim says. “That’s the challenge
every postpartum nurse struggleswith at some point.”
The nurses also constantlyassess what they can do to helpfeedings go well. Is the mother inpain and therefore not ready tobreastfeed right now? Is the babyfussy and in need of comfortbefore he or she can nurse?Weighing issues such as these alsorequires art, Ms. Marshall-Crimsays.
That art extends to beingsensitive to individual needs.Although “rooming in” is thestandard of care, for example,some mothers may have a medicalor special need to spend timealone.
The use of evidence-basedpractices, combined with the artnurses bring to their roles hasachieved positive results, both in
rates of breastfeeding and in the responses of patients.“Mothers who come to a Baby-Friendly hospital havecertain expectations,” Ms. Marshall-Crim says. “Overwhelm-ingly, we find patients appreciate what we offer in terms ofpostpartum care.” •
6 HARTFORD HOSPITAL NURSING / SPRING 2014
Mary Marshall-Crim, APRN, helps Melissa Mathieubreast-feed her twins.
The Ten Steps to Successful Breastfeeding
1. Have a written breastfeeding policy that is routinelycommunicated to all health care staff.
2. Train all health care staff in the skills necessary toimplement this policy.
3. Inform all pregnant women about the benefits andmanagement of breastfeeding.
4. Help mothers initiate breastfeeding within one hourof birth.
5. Show mothers how to breastfeed and how tomaintain lactation, even if they are separated fromtheir infants.
6. Give infants no food or drink other than breast-milk, unless medically indicated.
7. Practice rooming in – allow mothers and infants toremain together 24 hours a day.
8. Encourage breastfeeding on demand.
9. Give no pacifiers or artificial nipples tobreastfeeding infants.
10. Foster the establishment of breastfeeding supportgroups and refer mothers to them on discharge fromthe hospital or birth center.
Source: www.babyfriendlyusa.org
•• The ART Of Nursing
Best Practices In BreastfeedingEncouraging breastfeedingdraws on the nurse’s art and use of evidence-based practices.

7HARTFORD HOSPITAL NURSING / SPRING 2014
As a certified critical care nurse in Hartford Hospital’sCardiac Intensive Care Unit, Carolyn Tschummi, RN, BSN,BA, CCRN, is well-acquainted with the many technologicalresources available to patients who are extremely ill.“We’ve clearly crossed a threshold in medicine—atechnological threshold—where we’re often capable ofreplacing the function of a damaged organ or system witha machine or a medical intervention,” she says. Thequestion that nurses and their colleagues wrestle with, shesays, is whether providing these advanced therapies is rightfor an individual patient. “Although these therapies areavailable, they’re not always going to improve the quality of life for someone long term. And quality of life is differentfor every person.”
Advanced therapeutics such as VADs (ventricular assistdevices), ECMO (extracorporeal membrane oxygenation),CVVH (continuous veno-venous hemofiltration) andtherapeutic hypothermia are invaluable, often life-saving,resources, but their use must be tailored to each patient’sneeds and goals.
Deciding whether to offer a patient advanced therapiesor to recommend discontinuing them is a complex processinvolving multiple specialties. One example of such asystematic screening process is that of the VAD team. Thisgroup, which meets weekly, includes physicians, advancedpractice nurses, nurses, palliative care specialists, socialworkers, occupational therapists, physical therapists anddieticians.
“Each patient being considered for a VAD is evaluated byeach discipline,” says Michele Kolios, RN, BSN, MS, nursemanager of the Coronary Care Unit and Cardiothoracic ICU.“When you create a situation where the patient isevaluated at all of these levels, you’re better able todetermine the best possible scenario for the patient—onethat’s reflective of their personal goals.”
Nursing plays a unique role in the process, says EvelynDeJesus, RN, BSN, CCRN, nurse manager of the SurgicalTrauma Intensive Care Unit. “The anchor is nursing. We arethe ones there advocating for the patient and being themedium to coordinate all the different specialties. We’rethe one entity that doesn’t change. We stay with thepatient.”
Nurses are in a unique position to understand andconvey the wishes and goals of a critically ill patient. “Weusually have just one or two patients, so our conversationswith them often grow deep,” Carolyn Tschummi says. “Youget to know the person—not just the sick person in thebed, but the person they’ve been their whole life.”
Getting to know the patient, Ms. Tschummi says, builds a foundation of trust and establishes a therapeuticrelationship. “Once you establish that foundation, you havea starting point for helping them with decisions that mightbe difficult,” she says.
Those decisions become especially difficult at the endstages of illness. And, again, the nurse’s role is critical.“Sometimes, when I’m alone in the room with the patient,holding their hand and having that emotional connection,and with their knowing I’m their advocate, they mayexpress that they’re tired and don’t want to carry on. Whensomething like that happens, we definitely become thevoice of our patients.”
Whether it’s through speaking with the patient directlyor learning about the patient from the family, nurses bringthe patient’s perspective to the medical team’sdeliberations. Ms. Tschummmi says, “In theseconversations, whether it’s about using technology orwithdrawing care, the goal always should be: Would thishonor them? Is this what they would want? It isn’t aboutus, the family or the technology. It’s only about the personin the bed.”
Michele Kolios says that advanced therapeutics havecreated a new dimension in terms of the demands on ICUnurses, both in the expertise they must have and their levelof commitment. “It is incredibly hard work,” Ms. Kolios says.“I look at them with such admiration and pride as I seethem manage these patients.” •
•• The ETHICS Of Nursing
Carolyn Tschummi, RN, BSN, BA, CCRN, talks with patient George Petro in the Cardiac Intensive Care Unit.
Critical care nurses balance advancedtherapeutics with patients’ wishes.
Honoring The Patient

8 HARTFORD HOSPITAL NURSING / SPRING 2014
Research is key to learning what constitutes evidence-based care. That’s why Hartford Hospital nurses havecreated a new nursing council, the Council for Innovationand Transformation, or CIT. The CIT’s stated mission is “To promote an evidence-based culture where nurses usescholarly and academic resources to innovate andtransform practice and enhance the human health careexperience.”
The CIT grew out of a desire to more fully develop theresearch component of Hartford Hospital’s NursingProfessional Practice Model (see page 2). Initially, a steeringcommittee was formed that included Deborah Gingras, MS,RN, CNS; Ruth Zafian, MS, RN, CNS; Research Scientist KarylBurns, PhD; Ethics Committee Director Barbara Jacobs, PhD;and Nurse Director Cathy Yavinsky, RN, MS, CNE-BC, whoserved as mentor.
One of the steering committee’s first steps was to surveyHartford Hospital nurses to assess the current state ofnursing research. Results showed that nurses want supportand mentoring resources, direct involvement of bedsidenurses, education about research, dissemination of resultsback to the bedside nurse, and help in identifying researchquestions. With this information in hand, the CIT steeringcommittee invited staff nurses to the council’s first formalmeeting, which was held in October 2013.
Janice Wilson, RN, BSN, CNOR, an operating room nurse,is one of those who joined the CIT. “Andrea Hagstrom and Iare representatives from perioperative services,” Ms. Wilsonsays. “But there are nurses from all the different areas ofthe hospital, and they’re very diverse in terms of roles and
levels of experience. I feel really excited to interact withnurses from so many areas of practice.”
Each monthly meeting of the CIT includes aneducational presentation, followed by a business meeting.At each meeting, guest speakers provide information keyedto helping participants become more familiar with findingand evaluating research and developing their own researchquestions.
Clinical Librarian Lisa Carter, MSLIS, one of the firstpresenters, went on to create a system to help HartfordHealthCare nurses stay abreast of research in theirspecialties through a program called Netvibes. By logging into netvibes.com and entering a password, nurses can viewthe tables of contents of prominent journals in their fieldsthat provide RSS feeds, then obtain full text copies ofselected articles from their medical libraries. A link to thesite is on the Nursing Research page. “Existing electronictable of contents services clog up email boxes,” Ms. Cartersays. “This source is organized so nurses can access theinformation when they’re ready.”
Janice Wilson emphasizes that the CIT has a dual goal.“It aims to enhance our understanding of how to obtainevidence through literature searches, but also to inspireand empower nurses to conduct their own research—tocultivate a desire to learn more.”
Nurses participating in the CIT are advocates forresearch among their peers. Ms. Wilson, in collaborationwith Andrea Hagstrom, has introduced a journal club in herunit to encourage colleagues to read and evaluate researchand apply it in their practice. “You break down the fear andlet people know that research is not beyond their scope,”Ms. Wilson says. “All nurses, no matter what level ofeducation, can participate in the research process.” •
•• The SCIENCE Of Nursing
The Council for Innovation and Transformation helps bring evidence-based care to the bedside.
The CIT concept in action. CIT member Janice Wilson, BSN, RN, CNOR (third from left),started a journal club on her unit. Participants read a published research study, thenmeet to discuss it. Shown at a recent meeting are Linda Motyl, RN; Diana Norman, RN;Ms. Wilson; Nurse Educator Andrea Hagstrom, MSN, RN, CNOR, CNL; Kris McGrath,BSN, RN; Cristin Haines, BSN, RN, CNOR; David Chicoine, RN; and Auria Mercado,CST. Absent from the photo: Mayra Matos, BSN, RN; Carmen Melo, BSN, RN; TheresaChristians, BSN, RN; and Conni Levesque, CST.
New Council Promotes Research

9HARTFORD HOSPITAL NURSING / SPRING 2014
Mary Clare Robinson, RN, BSNPerioperative Services
Christine Rooney, RN, MSNMedicine
Renee Sandone, BS, RNCardiovascular
Marlene Silvis, RN, MPH, OCN, CHPNOncology
Sarah Wheeler, RN, BSN, CENEmergency Department
Eileen Hermann, RN, PhDPerioperative Services
Meghan Link, RN, BSNWomen's Health
Brittany Andrews Odackal, RNC, BSNCardiovascular
Julie Purzycki, RN, BSNNeuro/Trauma
Regina Radikas, APRNTransplant
Keith Bergeron, RN, ASN, ACMCase Coordination
Paul Campbell, RN, BSNInstitute of Living
Mary DelCiampo, BSN, NCCWomen's Ambulatory Health Services
Karen DePasquale, RN, ASNBone & Joint Institute
Neal Galeota, RNSurgery
Nightingale AwardsCongratulations to Hartford Hospital’s 2014 Nightingale Award Recipients!We salute these 15 nurses who were chosen by their colleagues as exemplars of nursing excellence. They and otheraward recipients will be honored at the 12th Annual Hartford Regional Nightingale Awards for Excellence in NursingGala hosted by VNA HealthCare on May 8, 2014, at the Hartford Marriott Downtown.

10 HARTFORD HOSPITAL NURSING / SPRING 2014
Nursing News & NotesWe congratulate these Hartford Hospital nurses on their recent achievements.
Case Coordination
Tara Thompson, RN, earned her Accredited CaseManager certification.
Medicine
Ruth Amador, RN, MSN (C12), was the keynote speakerat a symposium, Disaster Training: Empowering OurElderly, which was held on Feb. 22, 2014. Thesymposium was organized by Hartford Hospitalmembers of the National Association of HispanicNurses-Hartford Chapter and the Hartford HospitalCenter for Emergency Preparedness.
Caroline Kaminski Ferrara, RN (B11I), earned herCertified Critical Care Registered Nurse designation.
Loren Frazao, RN, earned her MSN.
Melissa Hernandez, RN; and Nina Wright, RN (B11I),earned their BSNs.
Neuro-Trauma
Frederick Gluszek, II, BSN, RN, CCRN (C9I), earned hisCertified Critical Care Registered Nurse designation.
Nursing Administration
Amy Albano, RN, MBA, FACHE, presented a poster atthe American College of Healthcare Executives’ March24, 2014, Congress on Healthcare Leadership. The postertitle was “Managing Staffing Expense by MonitoringProductivity.”
Oncology
Lisa Solari, PCA (CB4), will graduate from CentralConnecticut State University in May 2014 with her BSN.
STAR Team
Colette Keise, RN, and Debbie Ann Ellington, RN, passedtheir advanced nursing certification examination fortheir APRN licensure.
Congratulations to those who earnednursing degrees:Lucy Boccacio (OR), Molly Ough (B9E), Lindsey Whalen(N8), Christina Weaver (ED), Maggie Holmes (ED),Elizabeth Onyebuchi (B5), Lisa Mistenti (B5) andElizabeth Gineo (N12).
Nurses were among participants at the CareConnect validation session in March.

I saw my first robin of theseason yesterday, and animmediate feeling of well-being came over me. How sadthat some people with mentalillness cannot feel that joy.Hartford Hospital this year isaddressing mental illness witha campaign called “Stop TheStigma” to help modify thepublic’s reaction to mentalillness and reduce the shameand isolation that one in four
Americans endure. At least 7,000 people have taken thepledge, and I encourage you to join if you have not done soalready. I remember driving by the Institute of Living as achild in the 1950s. As student nurses at Hartford HospitalSchool of Nursing, my classmates and I had to complete a three-month rotation at either the Institute of Living orNorwich State Hospital. It was amazing sharing withclassmates how these two hospitals differed in theirtreatment of mental illness. In retrospect, psychiatric carehas certainly improved, but it is an ongoing process.Perhaps with more acceptance and openness, people willventure out of their isolation and seek treatment. Wecannot do what we have always done and expect differentoutcomes. Hospitals are now being measured andreimbursed by clinical outcomes and patient satisfaction.
We must be creative and efficient as well as caring, yetadhere to budget, time and staffing constraints. What agigantic task!
The Alumnae Association is also striving to encouragewellness within its membership. The Medical Fund hasbeen used more this year than in previous years forassistance with physical and occupational therapy, hearingaids, dental procedures and medications, just to mention afew. We have donated money to the Children’sAdvancement Fund, aiding children with special needs, theInternational Rett Syndrome Foundation, and thePhilippine Disaster Relief Fund. The board is working on adissolution clause to add to our bylaws. Our AnnualBanquet and Meeting with election of board members willbe June 1, 2014, at the Crowne Plaza in Cromwell. Anyoneinterested in running for office should contact KarenMazzarella, nominating chairman.
Looking forward to spring and hoping to see you at ourAnnual Banquet. Your board continues to strive to serve its membership and welcomes your comments andsuggestions.
Betty Ann Vose Fusco, RN (HHSN ’66)President, Alumnae Association of the Hartford Hospital School of Nursing
11HARTFORD HOSPITAL NURSING / SPRING 2014
Join Your AlumnaeAssociationBecome one of the nearly 600HHSN graduates who belong to theAlumnae Association of the HartfordHospital School of Nursing.Membership dues are only $10 per year andinclude membership in the Alumnae MedicalFund. Members are eligible to apply forscholarships.To join, simply mail your $10 non-tax-deductible check (payable to the AlumnaeAssociation of HHSN Inc.) to the addressbelow, along with your full name, class year,mailing address, telephone number and e-mail address. For more information, please contact Betty Ann Fusco, president, [email protected]; Pat Ciarcia, executivedirector of alumnae affairs, [email protected]; or visitwww.HHSNalumnae.org. You can also writeto the Alumnae Association of the Hartford Hospital School of Nursing, 560 Hudson Street, Hartford, CT 06106.
From The Alumnae Association President
PresidentBetty Ann Vose Fusco, RN ’66
Vice PresidentMary Jane Pappalardo Densmore,RNC, BA, MA ’69
Recording SecretaryAlicia Plikaitis Junghans, RN ’66
Program and PublicityGail Pendleton Rapoza, RN ’66
NominatingKaren Stinson Mazzarella, RN, BA ’69
Directors
Jerri Saltus Sicaras, RN, ’63
Lesley Prentice McGrath, RN ’61
Christine Johnson, RN, MS ’61
Barbara Biel Nowak ’73
Executive Director of Alumnae AffairsPatricia Andreana Ciarcia, RN, MSN ’62
Board TreasurerJane Wallace Lasher, RN, BSN, ’74
Vice TreasurerTheresa Gwozdz, APRN, ’76
The Board Of The Alumnae AssociationOf The Hartford Hospital School Of Nursing
STAY CONNECTED! If your email address changes, please notify Pat Ciarcia.

Seeking and seizing opportunity is a themethat runs through the long nursing career ofChristine Johnson, RN, MS (HHSN ’61).
“I was always willing to take opportunities andchallenges,” says Christine Johnson. “I never got sofixated on one area that I didn’t ever want to doanything else. By heeding the counsel ofexceptional mentors, I realized change is alwayshappening, and you need to be prepared for thefuture.”
Ms. Johnson began her career inHartford Hospital’s emergencydepartment. After a brief stint as astaff nurse in San Francisco, shereturned to the ED as a unitmanager. It was the mid-1960s, andone of the emerging innovations inmedicine was the development ofcoronary intensive care units.When Hartford Hospital opened itsfirst CICU in 1968, Ms. Johnson wasits head nurse. The unit providedleading-edge care for heart attackpatients. It also provided nurseswith opportunities they had neverhad before.
For the first time at HartfordHospital, nurses in the CICU weregoing to be able to do their own IVs,perform CPR and initiate therapiessuch as defibrillation without having to wait for aphysician’s order. The goal was to increase patientsurvival rates by taking immediate action.
“We were so excited about it, because it wascutting-edge at the time and offered anopportunity to do something to improve patientcare,” Ms. Johnson says.
Ms. Johnson adds, “It was the type of unit wherenurses were becoming more independent, butworking collaboratively with physicians. It was avery collaborative approach to how we allfunctioned.”
After earning a bachelor’s degree in 1972, Ms.Johnson returned to Hartford Hospital as a clinicalspecialist in cardiology—another brand-new rolefor nurses. She educated new staff about Interpreting arrhythmias and performing CPR, andtaught patient education classes, as well.
Soon, Ms. Johnson was back in school, earningher master’s degree at the University ofConnecticut. A practicum she did as part of herstudies resulted in her being offered a position on a
new community research project called Triage. Theinnovative project focused on enabling the elderlyto stay in their homes by providing services specificto their needs. The project was funded throughMedicare and run by nurses in collaboration withsocial workers. The chance to learn about funding,payment systems and other financial matters, Ms. Johnson says, “was a cutting-edge opportunityfor me.”
Her fiscal experience was helpful when shereturned to Hartford Hospital in an administrative
capacity as director of medicineand rehabilitation. In this role, shewas responsible for millions ofdollars in salaries and supplies.She was also in a position to helpbring about changes that sheknew from her clinical experienceneeded to be made, with much ofthe focus being onnurse/physician collaborativepractice.
In 1987, she became vicepresident of nursing and then ofpatient care services at NewEngland Baptist Hospital inBoston. During her 12 years there,she spearheaded major changes inits nursing school and in nursingpractice, all focused on enhancingthe quality of patient care.
“You always start by focusing on the patient,”Ms. Johnson says. “If you focus your thoughts andreasoning on the best interests of the patient, yoursatisfaction and success will be rewarding.”
In the late 1990s, hospitals were beginning todevelop rehabilitation or “transitional” units. Ms.Johnson was responsible for getting New EnglandBaptist’s unit up and running. In the process, shelearned all about long-term care. So when shesought a new opportunity, it was as director ofnursing at a long-term care facility back inConnecticut. Seven years later, she retired fromthat position, but went on to teach for several yearsin the master’s program of the University ofConnecticut School of Nursing.
Now truly retired, Ms. Johnson says, “I feel as if Ihad three separate careers: clinical, administrativeand academic. There’s no other profession I canthink of where you can have so manyopportunities. And there was no better place tobuild the foundation for my career than theHartford Hospital School of Nursing.” •
HARTFORD HOSPITAL NURSING / SPRING 201412
Alumnae Spotlight
Christine Johnson, RN, MS
Inspired By Opportunity

The 1936 yearbook of the Hartford HospitalTraining School for Nurses has a personality all itsown. Embellishing several of its pages arecharming pen-and-ink drawings by class memberLauretta Slate Schulz. Mrs. Schulz, who died inApril 2013 at the age of 98, was a woman of manytalents, including a gift for art. “I think she couldhave had a good career as an artist,” says Mrs.Schulz’s daughter, Nancy Schulz Winter ofBurlington, Conn. Mrs. Schulz’s interests rangedfrom art and theater to gardening, animals andliterature. Nursing, though, remained her chiefpassion and her life’s work.
After graduating, Mrs. Schulz worked for theVisiting Nurse Association before enlisting in theU.S. Army. During World War II she served as a firstlieutenant in the Pacific Theater of Operations. Shewas stationed in the Philippines, New Guinea andAustralia and on a tramp steamer that had beenconverted into a hospital ship. “On land, she was ina base camp created to help wounded soldiers,”Mrs. Winter says. “But at sea, she was in the line offire. They were surrounded by Japanese submarineson several occasions.” Mrs. Schulz and her fellownurses underwent rigorous training so they’d bebetter prepared in case of enemy occupation orbeing taken prisoner.
Mrs. Schulz’s daughter recalls some stories hermother would tell from her days as a young nursein wartime. Once, when shipments of supplieswere delayed because of the fighting, Mrs. Schulzand her fellow soldiers subsisted for a month onalmost nothing except beet greens and cannedgrapefruit juice, which they referred to as “batteryacid.” While camped on land in tropical NewGuinea, the nurses would hang their uniform topsoutside to dry overnight. One morning, crossing theencampment after breakfast, Mrs. Schulz feltsomething odd and looked down to see a red,
eight-inch-long millipede inside her shirt. Shescreamed and tore off the shirt, drawing cheersfrom nearby soldiers.
After the war, Mrs. Schulz attended college onthe G.I. Bill, earning her Bachelor’s Degree fromSaint Joseph College (now the University of SaintJoseph) and her Master’s Degree from HillyerCollege (now the University of Hartford). Shebecame a school nurse and health educator in theWest Hartford school system, where she developeda health curriculum, led the Future Nurses ofAmerica club and published a health newsletter.The job was an ideal one for a now-single mother,because she and her daughter had similarschedules.
During the summers, Mrs. Schulz worked as thecamp nurse at prestigious summer camps acrossNew England, and her little girl was one of thecampers. The arrangement enabled Mrs. Schulz togive her daughter a foundation in music, art, danceand other fields that would shape her life andcareer.
Mrs. Schulz often returned to Hartford Hospitalpart time throughout the 1970s and ’80s to work asthe head nurse on Center 10 and Center 11. “She’dwork the night shift on holidays so the head nurseon the floor could be with her family,” Mrs. Winterrecalls.
Mrs. Schulz made her home with her daughterand son-in-law in her later years. In 1986, the 50thanniversary of her graduation, the family hosted aparty for Mrs. Schulz’s classmates who hadreturned for the annual banquet. “We figured outthat we had one-sixteenth of the graduating classthere,” Mrs. Winter says. “It was a thrill for her tohave her friends together. She was very proud to bea nurse.” •
13HARTFORD HOSPITAL NURSING / SPRING 2014
A Look Back
Lauretta Slate Schultz (HHTS ’36) celebrating her 82ndbirthday in 1998 with her daughter, Nancy.
A Woman Of Many Talents
Sketches by Lauretta appear in the 1936 yearbook.

June Perret Noble ’54 singing “God Bless America”with Sam Pasco and His Band.
Jefferson House residents enjoying the sing-along.
Alumnae members sing along with the JeffersonHouse residents. Front: Lesley Prentice McGrath ’61,Theresa Gwozdz ’76, June Perret Noble ’54, MaryJane Pappalardo Densmore ’69, Christine Johnson’61. Back: Karen Stinson Mazzarella ’69, Joan GageHaines ’61, Gail Pendleton Rapoza ’66.
CLASS OF 1933
Faith Barnes Salomone’33, one of HartfordHospital School ofNursing’s remainingcentenarians, passedaway in January 2014 atthe age of 102. At theage of 7 Faith haddecided that she wantedto be a nurse, and shefulfilled that dreamwhen she graduated
from Hartford Hospital Training School in 1933. Herfamily describes Faith as one who “nursed thewhole neighborhood” and, as a result, “everyoneloved her.” At the time of her death, her family says,Faith was “sharp as a tack.”
CLASS OF 1950
Irene Sakmar O’Day ’50, a breast cancer survivor,gave a presentation to the Shoreline League ofDemocratic Women on the Dr. Susan Love ResearchFoundation campaign to eradicate breast cancer.This is the largest online research effort to find thecause of and cure for breast cancer.
CLASS OF 1951
Carolyn Bunning Clarke ’51 lives in a retirementcommunity in Canada and is happy to be relievedof all the details of caring for a house. Her childrenand grandchildren are doing well. She still enjoystraveling and would love to hear from herclassmates at: [email protected].
Alumnae The Pillbox
14 HARTFORD HOSPITAL NURSING / SPRING 2014
The Alumnae Association of the Hartford HospitalSchool of Nursing held its final annual meeting on Oct.20, 2013, at Jefferson House. In the future, the annualmeeting will be incorporated into the annual Junebanquet. Because the annual meeting has been held atJefferson House for several years, we wanted to thankthe residents for their hospitality in hosting this event.Sam Pasco and His Band entertained 17 alumnaemembers and 50 Jefferson House residents and staff.The band played songs from Irving Berlin, GeorgeGershwin, and Rogers and Hammerstein. The residentsand alums sang along and all had a wonderful time.The silver tea set that we all used at our school ofnursing was on display and brought back wonderfulmemories!

15HARTFORD HOSPITAL NURSING / SPRING 2014
CLASS OF 1953
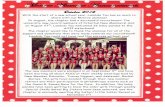
The Class of 1953 celebrated their 60th HHSNreunion at Cugino’s Restaurant, Farmington, Conn.,on Sept 18, 2013.
Front Row: Jean MacDougall Doll ’53, IreneNesteruk ’53, Marilyn Erickson Osborne ’53,Marion Sabonis O’Leary ’53, Jean Miles Scanlon ’53.Back Row: Nancy Rolick Powell, MD, ’53, JeanCanfield Hill ’53, Anna Jablonski Oleasz ’53,Nancy Bowers Lack ’53, Gay Bradbury Mahder ’53,Joyce Gifford McGovern ’53.
Front Row: Cynthia Erickson Griggs ’53, EthelCarlson Lavieri ’53, Edith Kuehn Zimmerman ’53,Evelyn Redlich Russ ’53.Back Row: Elaine Coyne Saunders ’53, NancyChoma Noel ’53, Ann Knibloe Minatti ’53,Rosemary Ross Stewart ’53, Georgia ClarkErickson ’53, Barbara Quilitch Gordon ’53.
CLASS OF 1959
Ardell Schmidt Patterson ’59 and Irene CardinSmith ’59 are making plans for the Class of 1959 asthey celebrate their 55th reunion this year. Theactivities will take place prior to the AlumnaeBanquet on Sunday, June 1, 2014, and anyonewishing more information may contact Ardell at:[email protected] or Irene at:[email protected].
CLASS OF 1960
Patricia Tencza Reig ’60 has created these twopastel paintings and says that nurses do otherthings besides taking care of loved ones andpatients.
CLASS OF 1962
Linda Arle Duval ’62 and her husband Billcelebrated their 50th wedding anniversary thisyear.
CLASS OF 1966
The Class of 1966 is gearing up for its goldenanniversary, which is only two years away. If anyclassmates have ideas about how to celebrate thismilestone, please contact Betty Ann Vose Fusco,Gail Pendleton Rapoza or Alfie Plikaitis Junghans.Betty Ann Vose Fusco ’66, president of theAlumnae Association, cruised Alaska this past Junewith her family and enjoyed the orangeCreamsicles® on Punta Cana for a week withEunice French Ecker ’66. Her next adventure is acruise to the Caribbean.Alicia “Alfie” Plikaitis Junghans ’66 has, in herwords, “kissed the Angel of Death” and is now luckyenough to be participating in a country-wideclinical study of multiple myeloma. The study issponsored by the Mayo Clinic.Patricia “Tisha” Kenny ’66 retired from runningthe nonprofit, Health & Human ResourceEducation, which she started with two other peoplein 1984. She is now a full-time artist, painting andcreating cards from her art. Her website is:www.tishakenny.etsy.com.Sue Hilton Latulipe ’66 has relocated from NewHampshire to Texas to be closer to her family. Dr. Lee Turlis Phares ’66 continues to teach and isvery active in the Rotary Club, frequently travelingfor them.Carolyn “Kitty” Kirtland Phillips ’66 is at herwinter home in Daytona Beach, Fla., enjoying thenot-so-nice weather this season.Gail Pendleton Rapoza ’66 is sunbathing in Cancunand this summer is off on a Rhine River cruise.
Pastel paintings by P. Reig.

16 HARTFORD HOSPITAL NURSING / SPRING 2014
Lillian Rund Tibbles ’66 has just published her firstbook. It is available in bookstores and onAmazon.com. The title is Learn to Video Call withKids: A Beginner’s Guide to Skype, Face Time and VideoCall with Children. Although she has publishedarticles in nursing journals about the use ofcomputers, this is a fun book that she thinks maybe of interest to HHSN grandmothers. It is free, funand easy to use. After a wonderful career innursing, Lillian is finally retired. She lives in Naples,Fla., with her husband of 43 years, Ken. They havea daughter who lives in Wyoming, a son in SouthCarolina, two grandsons and a granddaughter.
Lillian Rund Tibbles’ first book.
The Class of ’66 Lunch Bunch will resume theirfun-filled luncheons once the weather improves. Allare encouraged to attend. Notifications will be sentout once the date is set.
CLASS OF 1969Jean Bajek ’69 continues to work at CVS Pharmacyin Panama City Beach, Fla. She uses her vacationtime to visit her teenage grandchildren inConnecticut and her two grandsons (ages 1 and 4)in Kentucky.
CLASS OF 1972
Dr. Laura Caramanica ’72 is pictured with Dr. Eileen Breslin ’75 at Laura’s inductionceremony into the Academy of Nursing.
Laura Caramanica ’72 was inducted as a Fellow inthe Academy of Nursing on Oct. 19, 2013, at theacademy’s 40th annual meeting. Her sponsors wereDr. Eileen Breslin ’75, dean of the University ofTexas School of Nursing in San Antonio, Texas, andDr. Rhonda Anderson, former chief operating officerat Hartford Hospital and current chief executiveofficer of Banner Children’s Hospital in Arizona.
The academy serves the public and the nursingprofession by advancing health policy and practicethrough generation, synthesis and dissemination ofnursing knowledge.
Laura also completed a certificate in theFundamentals of Magnet, a course certificationprogram.
CLASS OF 1974Deborah Carson ’74 would like to remind herclassmates that this year is their 40th HHSNanniversary. She is asking that they make a specialeffort to attend the Alumnae Banquet on June 1 tocelebrate this event.Betsy Gaudian ’74 is the inpatient diabetes nurseclinician at the Center for Diabetes and MetabolicCare at St. Francis Hospital in Hartford, Conn.Previously, Betsy worked in community health as aregistered dietitian and a certified diabeteseducator.
CLASS OF 1975Gail Bonney Castonguay ’75 lives in Hebron,Maine, with her husband, Leon. She has justcelebrated her 30th year at Androscoggin HomeCare & Hospice, where she is a clinical supervisor.She received her BSN from St. Joseph’s College in2005. She and Leon have five children and sixgrandchildren.
CLASS OF 1976Ann Lambert Minor ’76 is a holistic nurse, atherapeutic touch teacher, and a hospice andpalliative care nurse. She received the 2012selection for excellence in her field by the End ofLife Nursing Education Consortium. Ann is theTranquill Passages director at Southington CareCenter and the holistic care coordinator atSouthington Care Center and Jerome Home in New Britain, Conn.

IN MEMORIAM
Let Us Hear From You!
We would love to receive photos andnews from HHSN alumnae. Pleasemail information to the AlumnaeAssociation of the Hartford HospitalSchool of Nursing, 560 HudsonStreet, Hartford, CT 06106 or e-mail [email protected].
Request For HHSN Nursing Pins
We often receive requests for areplacement HHSN nursing pin.Because they are no longer made,the only way we can get a pin is ifan alum is willing to donate one tothe Alumnae Association. We wouldthen give the pin to the requestingalum. If you are interested indonating your pin for this purpose,please contact Pat Ciarcia at 860.563.2005 or [email protected].
Give A Lasting Gift
Your contribution today will make adifference to our nursing educationprogram. Mail your gift to Hartford Hospital, Fund Development,80 Seymour Street, Hartford, CT06102. You can act now and showyour commitment to nursingeducation forever by includingHartford Hospital and/or theAlumnae Association of HHSN Inc.in your estate plans. For moreinformation, please contact Carol S.Garlick, vice president, philanthropy,at 860.545.2162 [email protected].
17HARTFORD HOSPITAL NURSING / SPRING 2014
Faith Barnes Salomone ’33
Margaret Hammond Lintelmann ’40
Yetta Horowitz Rutchik ’41
Lois Schurmann Barlow Cox Query ’48
Dorothy Peterson Humphrey ’48
Marjorie Shields ’48
Gertrude Petersen Tyrol ’50
Joanne Fletcher ’51
Elaine Schultz Cihocki ’54
Nedra Leach Caccomo ’56
Arline Warner Titus ’57
Ann Ambrose Fryer ’59
Susan Avery Gilmartin ’61
Carol Boyce Goedert ’64
Physician
Dr. Edward Fredericks – Neurology
PHO
TO
BY
LA
NN
Y N
AG
LER

Non ProfitOrganizationU.S. Postage
PAIDHartford, CT
Permit No. 4361
Address Service Requested
“Affiliate” nursing students at the Institute of Living circa 1940. Students from schools across the state regularly joined Hartford Hospital School of Nursing students at the IOL for the
psychiatric portion of their training.
80 Seymour StreetP.O. Box 5037Hartford, CT 06102-5037