November-December 2007, Pages 374-399 doi:10.1016/j.cppeds.2007.09 ...
Transcript of November-December 2007, Pages 374-399 doi:10.1016/j.cppeds.2007.09 ...

Current Problems in Pediatric and Adolescent Health Care Volume 37, Issue 10, November-December 2007, Pages 374-399
doi:10.1016/j.cppeds.2007.09.001 | How to Cite or Link Using DOI Copyright © 2007 Mosby, Inc. All rights reserved.
Permissions & Reprints
Infant Feeding: Initiation, Problems, Approaches
John Nicholas Udall Jr MD, PhDa
aDepartment of Pediatrics; WVUHSC-Charleston, Women and Children’s Hospital, Charleston, WV.
Available online 28 November 2007.
Article Outline
Section I: Developmental Aspects of Swallowing and Feeding in Infants and Young Children (
http://www.nature.com/gimo/contents/pt1/full/gimo17.html) Incidence and Prevalence of Feeding and Swallowing Disorders in Pediatrics
Development of Feeding and Swallowing Skills Prenatal Swallowing and Sucking
Infant Feeding and Swallowing
Transition Feeding
Critical and Sensitive Periods with Implications for Behavioral and Sensory-based Feeding
Problems
Effects When Oral Feeding Is Not Possible in the Newborn Period
Taste and Smell in Oral Feeding of Infants and Young Children
Clinical Assessment of Pediatric Swallowing and Feeding Disorders for Primary Care Physicians Principles of Clinical Feeding Evaluation
Categories of Causes of Swallowing and Feeding Disorders
Caregiver Perceptions of Feeding Problems
Interdisciplinary Team Approach
Instrumental Examination of Swallowing
Management of Feeding and Swallowing Problems in Pediatrics
Section II: Gut Motility and Enteral Feeding Tolerance with an Emphasis on Premature Infants
Gastrointestinal Motility Esophagus
Stomach and Small Intestine
Postprandial Small Intestinal Motility

Interdigestive Small Intestinal Motility
Colon
Developmental Aspects Mouth and Esophagus
Stomach
Small Intestine
Feeding Recommendations for Premature Infants
Section III: Behavioral Treatment of Feeding Disorders Classification
Evaluating Feeding Problems
Treatment Appetite Manipulation
Behavioral Contingency Techniques
Section IV: Feeding Issues in the Disabled Child Magnitude of the Problem
Nutritional Needs Inadequate Intake
Increased Losses
Energy Requirements
Assessment Medical History
Nutritional History
Physical Examination
Anthropometrics
Laboratory Evaluation
Recommendations
Other Considerations
References The impetus for this issue comes from a Topic Symposium entitled, ―Infant Feeding: Initiation, Problems,
Approaches‖ held at the Pediatric Academic Societies meeting in Toronto May 6, 2007. The symposium
focused on four aspects of feeding infants and young children. Each aspect was discussed by an authority in
the field.
One presentation concerned the developmental aspects of swallowing and feeding infants and young
children. Another addressed the development of gut motility in the premature infant and its relationship to
enteral feeding. The third topic concerned the behavioral treatment of feeding disorders in toddlers and
finally, feeding issues related to neurologically impaired children were reviewed.
Feeding premature and full-term infants through the first few years of life has become an area of interest and
study over the past two decades. The realization that some infants and children are not fed easily or may
develop feeding problems resistant to traditional approaches has led to the institution of feeding teams at
larger pediatric centers. Hopefully, information presented at the Topic Symposium and contained within this
issue will be shared with others as we follow emerging research concerning the optimal feeding of normal
infants and children, and those with feeding disorders.

Section I: Developmental Aspects of Swallowing and Feeding in Infants and
Young Children (http://www.nature.com/gimo/contents/pt1/full/gimo17.html)
Adequate respiration and nutrition are essential throughout a lifetime. Breathing usually does not require
active effort by infants except for those with complicating factors, for example, bronchopulmonary dysplasia,
upper airway obstruction as in Pierre Robin sequence, other craniofacial anomalies, and severe
laryngotracheomalacia. Eating, on the other hand, requires active effort by infants who must have exquisite
timing and coordination of simultaneous breathing, sucking, and swallowing. Adequate growth, defined by
weight gain in early infancy and for the first few years of life, is the primary measure of successful feeding.
Breathing, sucking, and swallowing are activities that occur in the upper aerodigestive tract and are
orchestrated by cranial nerves and specific areas in the brain. Successful oral feeding requires that children
have functional oral sensorimotor and swallowing skills, adequate pulmonary and gastrointestinal function,
central nervous system integration, and normal musculoskeletal tone. A breakdown in coordination of
swallowing and breathing can result in aspiration. Aspiration may present with coughing and choking,
usually during feeding, and is indicative of compromised airway protective reflexes. If laryngotracheal
sensation is also affected, aspiration may be silent without overt manifestations.
Normal feeding patterns reflect the early developmental pathways that are the basis for later communication
skills. The interrelationships between feeding (in all living beings) and complex verbal communication
(unique to humans) are multifactorial and in need of continued research. The study of comparative anatomy
and its implications for human communication are well described.1
Professionals who examine and treat infants and children who have feeding and swallowing problems must
have a thorough understanding of embryologic and developmental anatomy of the upper aerodigestive tract
and the physiology of deglutition. Research in the past 30 years has added to the understanding of the
orderly development of feeding and swallowing in utero through infancy.
Incidence and Prevalence of Feeding and Swallowing Disorders in Pediatrics
Feeding and swallowing disorders are relatively common in early infancy and in some instances may be
markers for significant health implications that do not become obvious until later. As many as 35% of infants
exhibit food selectivity and refusal, as revealed by parent interviews in general population surveys. Feeding
problems are relatively common in various infant populations, including, but not limited to, preterm ―at-risk‖
infants, infants with congenital heart disease following open-heart surgery, infants diagnosed with
nonorganic failure to thrive, and children with cerebral palsy (CP). Prevalence rates of dysphagia range from
57 to 92% varying by type of CP.2 Children with CP and dysphagia are found to have a higher incidence of
undernutrition, growth failure, and poor health than those children without swallowing problems. Children
with more severe forms of CP and dysphagia have higher mortality rates than other groups.
This review provides an overview of (1) the development of feeding and swallowing skills, including
critical/sensitive periods with implications for behavioral and sensory based feeding problems; (2) taste and
smell, and their impact on oral feeding; (3) clinical assessment; (4) instrumental examination of pediatric
swallowing disorders; and (5) management of pediatric feeding and swallowing disorders.
Development of Feeding and Swallowing Skills
Prenatal Swallowing and Sucking

In utero studies of fetuses have documented the early development of swallowing and oral-motor function3
(Table 1). In utero swallowing is important for the regulation of amniotic fluid volume and composition,
recirculation of solutes from the fetal environment, and the maturation of the fetal gastrointestinal tract.4 The
pharyngeal swallow, one of the first motor responses in the pharynx, has been observed between 10 and 14
weeks’ gestation.5 Recent studies have demonstrated swallowing in most fetuses by 15 weeks’ gestation
and consistent swallowing by 22 to 24 weeks’ gestation.3
TABLE 1.
Gestational ages for swallowing and sucking
Swallowing function Gestational age (wk)
Pharyngeal swallow 10-14
True suckling 18-24
Tongue cupping 28
Sustained total oral nutrition 34-37 View Within Article
True suckling begins around the 18th to 24th week and is characterized by a distinct backward and forward
movement of the tongue. The frequency of suckling motions can be altered by taste. Taste buds are evident
at 7 weeks’ gestation. By 12 weeks’ gestation, distinctively mature receptors are noted. Self oral-facial
stimulation usually precedes suckling and swallowing. Tongue cupping is seen by 28 weeks’ gestation.
This backward and forward movement of the tongue in suckling is all that can be expected because the
tongue fills the oral cavity at this stage of development. Backward movement appears more pronounced
than forward movement. Tongue protrusion does not extend beyond the border of the lips. Serial ultrasound
images have shown that suckling motions increase in frequency in the later months of fetal life.3 By 34
weeks’ gestation, a healthy preterm infant likely suckles and swallows well enough to sustain nutrition strictly
through oral feedings. Some healthy preterm infants may be ready to begin oral feeding by 32 to 33 weeks’
gestation.
It has been estimated that the near-term human fetus swallows 500 to 1000 mL/d of amniotic fluid.4 Earlier
reports had indicated that the fetus swallows about 450 to 500 mL of amniotic fluid per day (of the total 850
mL) and excretes about the same amount in urine.6 Decreased rates of fetal suckling are associated with
digestive tract obstruction or neurologic damage. Intrauterine growth retardation may be a manifestation of
neurologic damage. Lack of regular swallowing by the fetus should lead one to suspect problems that may
be related primarily to the preterm infant or primarily to the mother. Maternal polyhydramnios characterized
by excessive amniotic fluid in the uterus may result from multiple fetal and maternal etiologies. Severe
polyhydramnios is more strongly associated with congenital malformations than mild or moderate
polyhydramnios.7
Infant Feeding and Swallowing
Oral feeding that requires suckling, swallowing, and breathing coordination is the most complex
sensorimotor process the newborn infant undertakes. Premature infant patterns differ from those of full-term
infants. Lau and coworkers describe five primary developmental stages of sucking that characterize the
maturational process (Table 2).8 Sucking patterns in infants born at less than 30 weeks’ gestation were

monitored from the time they were introduced to oral feeding until they reached full oral feeding. The five-
stage scale demonstrates the relationship between the development of sucking and oral feeding
performance of preterm infants. A high interobserver reliability was observed on 50 bottle-feeding
assessments. The authors suggest that there is no significant in utero maturation of sucking occurring
between 26 and 29 weeks’ gestation, or they had insufficient statistical power to detect a difference over this
developmental period. A significant correlation between the level of maturity of an infant’s sucking and
gestational age was found. Feeding performance correlated with progression of oral feeding. These authors
suggest that developmental scales can be used clinically for the identification and characterization of the
oral sensorimotor skills of preterm infants at any point in their development as they progress in their
individual oral feeding schedule. Objective and quantitative evaluations of infants’ nonnutritive and nutritive
sucking would be helpful in evaluating strength and coordination. One proposal includes a finger pressure
device to allow for quantification of specific measures of nonnutritive sucking in combination with a
nipple/bottle system developed for monitoring nutritive sucking.9 However, there is no standardized
quantifiable procedure available currently.
TABLE 2.
Five primary stages of sucking in preterm infants
Stage
Description
1a No suction; arrhythmic expression
1b Arrhythmic alternation of suction and expression
2a No suction; rhythmic expression
2b Arrhythmic alternation of suction and expression; sucking bursts noted
3a No suction; rhythmic expression
3b Rhythmic suction and expression; suction amplitude increases, wide amplitude range, prolonged sucking bursts
4 Rhythmic suction and expression; well-defined suction, amplitude range decreased
5 Rhythmic, well-defined suction and expression; increasing suction amplitude; sucking pattern similar to term infant
Adapted from Lau et al.8
View Within Article
Term infants typically show food-seeking behavior through rooting for a breast or bottle. Preterm infants
gradually achieve skills for rooting, suckling, and swallowing for functional oral feeding as they mature.
Important early developmental milestones and feeding skills from birth to 36 months are shown in Table 3.

Children older than 36 months typically are eating regular table food and drinking from an open cup. They
continue to refine their skills but do not attain new skills.
TABLE 3.
Developmental milestones and feeding skills birth to 36 months
Age (mo)
Development/posture Feeding/oral sensorimotor
Birth to 4-6
Neck and trunk with balanced flexor and extensor tone
Visual fixation and tracking
Learning to control body against gravity
Sitting with support near 6 months
Rolling over
Brings hands to mouth
Nipple feeding, breast, or bottle
Hand on bottle during feeding (2-4 months)
Maintains semiflexed posture during feeding
Promotion of infant–parent interaction
6-9 (transition feeding)
Sitting independently for a short time
Self-oral stimulation (mouthing hands and toys)
Extended reach with pincer grasp
Visual interest in small objects
Object permanence
Stranger anxiety
Crawling on belly, creeping on all fours
Feeding more in upright position
Spoon feeding thin, pureed foods
Suckle pattern initially suckle →suck
Both hands to hold bottle
Finger feeding introduced
Vertical munching of easily dissolvable solids
Preference for parents to feed
9-12 Pulling to stand Cup drinking

Age (mo)
Development/posture Feeding/oral sensorimotor
Cruising along furniture
First steps by 12 months
Assisting with spoon; some become independent
Refining pincer grasp
Eats lumpy, mashed food
Finger feeding for easily dissolvable solids
Chewing includes rotary jaw action
12-18
Refining all gross and fine motor skills
Walking independently
Climbing stairs
Running
Grasping and releasing with precision
Self-feeding: grasps spoon with whole hand
Holding cup with two hands
Drinking with 4-5 consecutive swallows
Holding and tipping bottle
>18-24
Improving equilibrium with refinement of upper extremity coordination
Increasing attention and persistence in play activities
Parallel or imitative play
Independence from parents
Using tools
Swallowing with lip closure
Self-feeding predominates
Chewing broad range of food
Up–down tongue movements precise
24-36
Refining skills
Jumping in place
Pedaling tricycle
Using scissors
Circulatory jaw rotations
Chewing with lips closed
One-handed cup holding and open cup

Age (mo)
Development/posture Feeding/oral sensorimotor
drinking with no spilling
Using fingers to fill spoon
Eating wide range of solid food
Total self-feeding, using fork
Adapted from Arvedson and Brodsky10
(pp. 62-7).
View Within Article
The development of independent, socially acceptable, feeding processes begins at birth and progresses
throughout the first few years of childhood. Oral sensorimotor skills improve within general
neurodevelopment, acquisition of muscle control that includes posture and tone, cognition, and language,
and psychosocial skills (Table 3).10
Feeding and swallowing skill development parallels psychosocial milestones of homeostasis, attachment,
and separation/individuation (Table 4).11
Infants during the first 2 to 3 months of life strive toward
homeostasis with the environment. Goals include sleep regulation, regular feeding schedules, and awake
states that are developmentally advantageous in the development of emotional attachment to primary
caregivers. Successful pleasurable feeding experiences foster efficient nipple control, reaching, smiling, and
social play. Thus, feeding gradually becomes a social event. Caregivers should not interpret pauses
between sucking bursts as a need for burping or early satiety. Once caregivers interrupt feeding, some
infants do not resume sucking readily. Caregivers then may perceive that an infant is full or too tired to
continue, so they stop the feeding. If this pattern becomes habitual, the infant is likely to gain weight slowly
or not at all, which results in undernutrition or failure to thrive. If the interactions between infant and
caregiver fail to develop appropriately, the infant may indicate lack of pleasure, loss of appetite, and, in
severe forms, vomiting and rumination. Significant feeding problems can evolve out of a mismatch between
infants’ cues and caregivers’ interpretations of the cues.
TABLE 4.
Feeding-related psychosocial milestone: birth to 36 months
Stage Psychosocial milestones
Birth to 3 months (homeostasis)
Cues for feeding: arousal, cry, rooting, sucking
Caregiver responds to cues (leads to

Stage Psychosocial milestones
self-regulation)
Infant quiets to voice
Hunger–satiety pattern develops
Infant smile promotes interaction with primary caregiver
Pleasurable feeding experiences → greater environmental interaction
3-6 months (attachment)
Primary interactions—―falling in love‖
↑Reciprocity of positive infant and caregiver interactions
Consistent cues
Anticipation of feeding
Pauses likely socialization, not necessarily for burping or to indicate satiety
Smiling, laughing, social, alert
Preferred feeders are parents
Calls for attention by 6 months
6-36 months (separation/individuation)
Responds to ―no‖
Imitates movements, and gradually imitation of speech
Play activity to explore environment (7-9 months)
Facial expression used to indicate likes and dislikes
Follows simple directions
Self-feeding emerges

Stage Psychosocial milestones
Mealtimes become more predictable
Speech becomes important
Direction following—gradually 2- to 3-step commands
Mealtimes become part of whole family schedule
Rapid increase in language 24-36 months
Independent feeding by end of period
Adapted from Chatoor et al.11
View Within Article
Transition Feeding
Infants show readiness for the transitional feeding period that usually begins around 4 to 6 months in
typically developing infants, which also is the period of attachment for psychosocial milestones (Table 4).11
Transition feeding describes the readiness for and initiation of spoon feeding, usually with thin cereal mixed
into breast milk or formula for most infants. Infant developmental skills that indicate readiness for spoon
feeding include, but are not limited to, upright sitting with minimal support, midline head position maintained
for several minutes without support, hand-to-mouth motor skills, dissociation of lip and tongue motions, and
anatomic changes resulting in more space for the tongue within the oral cavity that allow for vertical motion
of the tongue in addition to the previously restricted movements of ―in and out‖ suckling. Over the next
several months, infants gain oral sensorimotor skills for accepting thicker and lumpier food by spoon. Then,
they move into a period of greater independence noted by finger feeding of easily dissolvable solid food.
They gradually become more precise in picking up small pieces of food (or other objects), as they attain a
pincer grasp with thumb and forefinger, which is expected by 10 to 12 months.
Critical and Sensitive Periods with Implications for Behavioral and Sensory-based Feeding Problems
The concept of critical and sensitive time periods in overall human development is well documented in some
areas of development and in animal research. Lorenz12
interpreted findings from animal embryologic studies
to imply that there is a period during early development when the organism is primed to receive and perhaps
permanently encode important environmental information. These interpretations do not mean that later
learning cannot occur or that it is not important, but they do emphasize the possible significance of these
early experiences.
Critical and sensitive periods are believed to exist in the development of normal feeding behavior.
Descriptions of these critical periods typically focus on the introduction of chewable textures (Table 3).
Children develop oral side preferences for chewing that relate to hand preferences in many instances.

Chewing skills vary with textures. Children develop mature chewing skills for solid foods earlier than for
viscous and pureed foods. However, it is common for children who have not mastered the timing and
coordination for swallowing purees and other smooth food to be kept on those textures because caregivers
may believe that these children are not ready for introduction of chewable food, which is not necessarily
true. Children need to be introduced to solid foods at the most appropriate times. Children may reject solids
on initial presentation if they are introduced after the critical periods. The longer the delay in the introduction
of solids, the more difficult it is for many children to accept chewable food. Withholding solids at a time when
a child should be able to chew (6 to 7 months developmental level) can result in food refusal and even
vomiting,13
which in turn may have a significant negative effect on nutrition and hydration status.
Studies in mice reveal that those fed a soft-feed (powdered) diet after weaning reduced synaptic formation in
the cerebral cortex and impaired the ability of spatial learning (radial maze) in adulthood when compared
with mice fed a hard-feed (pelleted) diet.14
Similar deficits may result from lack of experience and exposure
to age-appropriate foods in humans, providing a conceptual framework to explain clinical observations of the
challenges encountered in the learning of oral sensorimotor and other skills in children not fed during
critical/sensitive periods for oral skill development. Perhaps when children have not been introduced to solid
foods within the critical sensitive periods, broad aspects of development may be affected negatively. One
may assume that these children missed not only this critical period for chewing, but also the underlying
skills, which include trunk stability, head control, mobility of limbs, and mouthing experiences involving
hands, fingers, and toys. Physiologic processes that are underpinnings for oral sensorimotor and swallowing
skills, such as respiratory control, also have critical periods that can impact the feeding process.
Psychosocial development, personality, and environment are additional factors that must be considered for
children with feeding issues. Some children may respond in aversive ways when presented with certain
textures, tastes, or temperatures of food and liquid. These same children may be hypersensitive to tight
clothes or tags on their clothes. They may not like to wear shoes. They may get upset when their hands get
dirty, so they refuse to do finger painting and will not put their fingers into pudding or other pureed food.
Critical and sensitive periods may apply to the mother, with effects related to the potential for efficient
feeding and global development of an infant.15
Maternal early contact with both preterm and term infants has
been found to have a positive effect on the mother’s attachment behavior and ultimately enhanced
development of the infant.
Effects When Oral Feeding Is Not Possible in the Newborn Period
When infants with major physical and physiologic problems are prevented from initiating oral feeding in the
same timeframes as their more typically developing peers, many demonstrate prolonged delays and
significant difficulty with oral feeding. In addition, significant variations are found in the form and function of
the ingestive systems of age-matched healthy infants and at-risk infants. Ultrasounds revealed that fetal
swallowing occurred most commonly in the presence of oral-facial stimulation. Hands were touching face
and mouth. In some instances, fingers or thumbs were seen in the mouth. Perhaps some infants miss critical
periods while still in the womb. Miller and colleagues3 postulate that prenatal development indices of
emerging aerodigestive skills may guide postnatal decisions for feeding readiness and, ultimately, advance
the care of medically fragile neonates. Clinicians must have knowledge regarding normal development to
appreciate and understand the implications of differences in infants and young children with feeding and
swallowing problems, which are likely to be just one or two pieces of a much larger and more complex

puzzle. All aspects must be delineated to plan management strategies that will permit adequate nutrition
without pulmonary issues and without stress to the child as well as to the caregiver.
Taste and Smell in Oral Feeding of Infants and Young Children
Understanding an infant’s awareness of taste and smell, along with responses to textures and temperature,
is fundamental for clinicians of any discipline to determine the potential for acceptance of new foods.
Physicians, dietitians, nurses, and therapists who guide parents when children are failing to thrive, or have
limited range of foods in the diet, must examine the broad parameters that can impact on a child’s feeding
status. These experiences occur much earlier than many professionals would expect. Initial experiences
with flavors occur before birth, because the flavor of amniotic fluid changes as a function of the dietary
choices of the mother. Flavors from the mother’s diet during pregnancy are transmitted to amniotic fluid,
which are not only perceived by the fetus but also enhance the acceptance and enjoyment of that flavor in a
food during weaning from the breast. The ability to detect additional tastes and flavors develops after birth.
Thus, it is clear the early sensory experiences have an impact on the acceptance of flavors and foods during
infancy and childhood.16
It has long been shown that human infants are born with a preference for sweet. Their sensory apparatus
can detect sweet tastes. Tatzer and colleagues17
found that preterm infants fed exclusively via gastric tubes
exhibited more nonnutritive sucking in response to minute amounts of glucose than to water solutions
presented intraorally. Infants produced more frequent and stronger sucking responses when offered a
sucrose-sweetened nipple compared with a latex nipple.18
Exposure to flavors in breast milk may serve to heighten preferences for these flavors and facilitate the
weaning process. Some breastfed infants are more willing to accept a novel vegetable on first presentation
than are formula-fed infants.19
Children who have been breastfed for at least 6 months are also less likely to
become picky eaters.20
The ability to detect and prefer a salt taste does not appear until infants are about 4 months of age. Animal
model studies demonstrate that this developmental change may reflect postnatal maturation of central and
peripheral mechanisms underlying salt taste perception.21
The preference that emerges at this age appears
to be largely unlearned.
An example of the importance of early exposure to flavors is found in the acceptance of protein hydrolysate
formulas by 7-month-old infants who had readily accepted this kind of formula when compared with their
regular milk- or soy-based formula in the first couple months of life. These formulas are known by a variety
of names depending on the company that produces and distributes them in the United States and in other
countries throughout the world. A sensitive period in early infancy is suggested as at least one important
factor, as shown by the finding that those infants 7 months and older avidly accept these formulas if they
have experienced them during the first months of life. However, in marked contrast, 7- to 8-month-old infants
who had no previous experience with hydrolysate formulas strongly rejected them and displayed extreme
and immediate facial grimaces, similar to those observed in newborns in response to bitter and sour
tastes.22
Professionals who make decisions regarding feeding of infants and young children have to consider multiple
variables. Differences in flavor acceptance that occur from breastfed to bottle-fed infants and that likely
change over time reflect complex interactions of sensory and motor factors.

Clinical Assessment of Pediatric Swallowing and Feeding Disorders for Primary Care
Physicians
There are four key questions that physicians and nurses in primary care can ask parents when an infant or
young child presents at the office or clinic with parental concerns related to feeding. The answers help
determine if a comprehensive clinical feeding and swallowing assessment is needed, even though the
answers do not necessarily define the problem:
• How long do mealtimes typically take? If more than about 30 minutes on any regular basis, there is a problem. Prolonged feeding times are major red flags pointing to the need for further investigation. • Are mealtimes stressful? Regardless of descriptions of factors that underlie the stress, further investigation is needed. It is very common for parents to state that they ―just dread mealtimes.‖ • Does the child show any signs of respiratory stress? Signs may include rapid breathing, gurgly voice quality, nasal congestion that increases as the meal progresses, and panting by an infant with nipple feeding. Recent upper respiratory illness may be a sign of aspiration with oral feeds, although there may be other causes. • Has the child not gained weight in the past 2 to 3 months? Steady appropriate weight gain is particularly important in the first 2 years of life for brain development as well as overall growth. A lack of weight gain in a young child is like weight loss in an older child or adult.
Principles of Clinical Feeding Evaluation
The clinical evaluation of an infant or child with complex issues related to feeding and swallowing includes a
thorough history, physical examination, and feeding observation. Instrumental assessments of swallowing
may be needed following the clinical evaluation when concerns are noted regarding pharyngeal phase
physiology and risks for aspiration with oral feeding. Most children are best served in the context of an
interdisciplinary team. Unfortunately, such teams are available only in a limited number of medical centers in
the United States and in other countries throughout the world. Information is provided that should be useful
for physicians, dietitians/nutritionists, and other professionals who do not have an interdisciplinary team
available. All professionals who work with these infants and children are urged to collaborate with
appropriate colleagues and to develop an interdisciplinary team to whatever extent is possible. Particular
attention is paid to factors that are likely to interfere with adequate nutrition and hydration, because the most
fundamental goals for all children relate to optimal status of nutrition and hydration.
Categories of Causes of Swallowing and Feeding Disorders
A careful reading of the medical, developmental, and feeding history is the first step that is critical to
decision-making. Swallowing and feeding disorders in infants and children are complex and can have
multiple causes in various categories of disorders including, but are not limited to the following:
• Disorders that affect hunger/appetite, food-seeking behavior, and ingestion • Anatomic abnormalities of the oropharynx • Anatomic/congenital abnormalities of the larynx and trachea • Anatomic abnormalities of the esophagus • Disorders affecting suck-swallow-breathing coordination • Disorders affecting neuromuscular coordination of swallowing • Disorders affecting esophageal peristalsis • Mucosal infections and inflammatory disorders causing dysphagia • Other miscellaneous disorders associated with feeding and swallowing difficulties, for example, xerostomia, hypothyroidism, trisomy 18 and 21, Prader–Willi syndrome, allergies, lipid and lipoprotein metabolism disorders, and a variety of craniofacial syndromes. Link and Rudolph
23 have a detailed list of specific causes within each of the above categories.
Caregiver Perceptions of Feeding Problems

Each person involved with feeding and caring for a child is likely to have perceptions of the feeding status
and problems that differ from other caregivers and professionals. Information is needed from more than one
caregiver or professional involved with the child. Questions are formulated to delineate the feeding status as
clearly as possible. The following questions go beyond the screening questions suggested earlier. A
discussion of each of these questions can be found at
http://www.nature.com/gimo/contents/pt1/full/gimo17.html.
How long does it take to feed the child? Is the child independent for feeding or dependent on others to a greater degree than would be expected for age and overall developmental status? Is the child a total oral feeder? Do differences in food textures, temperatures, or tastes change the child’s response at mealtime? Does the feeding problem change throughout the course of the meal? Does the feeding problem vary by time of day or by feeder? Does the child maintain a midline neutral position of the trunk, neck, and head without requiring added support? Are there signs of breathing difficulties during feeding? Does the child have emesis regularly? Does the child refuse food? Does the child get irritable or sleepy and lethargic during mealtimes? How do the child and caregiver interact? Are there signs of forced feeding?
Interdisciplinary Team Approach
An interdisciplinary team approach offers the benefit of coordinated consultation and problem-solving for
multiple interrelated problems. Effective management of these medically complex children depends on the
expertise of many specialists, who may work independently and as a team (Table 5). Case coordination is
often a critical component that is intensive and needed to optimize the child’s health and development along
with the family’s ability to cope with multiple issues and sometimes disparate opinions and
recommendations. An interdisciplinary approach is recommended at institutions where professionals
evaluate and treat children with complex feeding and swallowing problems. Success factors include the
following:
• Collegial interaction among relevant specialists • Shared group philosophy related to diagnostic approaches and management protocols • Team leadership with organization for evaluation and sharing of information • Willingness to engage in creative problem-solving and research • Time commitment for the labor-intensive work that is required TABLE 5.
Feeding/swallowing team members and their functions
Team member Function
Parents Primary caregiver and decision-maker for child
Physician Medical leader
(gastroenterologist, developmental pediatrician, or pediatric physiatrist)
Team co-leader
Pediatric health and neurodevelopmental diagnosis
Medical and health monitoring

Team member Function
within specialty area
Speech-language pathologist
Team co-leader (active in feeding clinic and coordinates programmatic activities)
Clinic and inpatient feeding and swallowing evaluation
Videofluoroscopic swallow study (VFSS) with radiologist
Flexible endoscopic examination of swallowing (FEES) with otolaryngologist
Oral sensorimotor intervention program
Nurse
Leads preclinic planning
Reviews records and parent information
Coordinates patient follow-up
Changes gastrostomy tubes
Dietitian/nutritionist
Assesses past and current diets
Determines nutrition needs
Monitors nutrition status
Psychologist
Identifies and treats psychological and behavioral feeding problems
Guides parents for behavior modification strategies
Directs inpatient behavioral feeding program
Occupational therapist Evaluates and treats children with problems related to posture, tone, and sensory issues
Social worker
Assists families for community resources in a variety of ways
Acts as advocate for the child

Team member Function
Additional specialists
Otolaryngologist
Physical examination of upper aerodigestive tract
Detailed airway assessment
FEES with speech-language pathologist
Medical and surgical treatment of airway problems
Pulmonologist Lower airway disease—evaluation and management
Radiologist
VFSS with speech-language pathologist
Computed tomography (CT) scan of chest
Varied radiographic diagnostic studies
Pediatric surgeon Surgical management of gastrointestinal disease
Cardiovascular surgeon Surgical management of cardiac disease
Neurologist/neurosurgeon Medical and surgical management of neurologic problems
Physical therapist Seating evaluations and modifications to seating systems
Adapted from Arvedson and Brodsky10
(pp. 6-7).
View Within Article
Depending on the expertise and interest in different institutions, team members may be drawn from different
disciplines. The functions should cover those described (Table 5). Not all disciplines will be needed for all
children. It is important to determine which disciplines can best serve the child and family so that patient
care can be both efficient and efficacious. Specific discipline involvement may change over time as the
child’s needs change.
Instrumental Examination of Swallowing
Instrumental examinations may be needed for infants and children particularly when the pharyngeal and
esophageal physiology needs to be delineated objectively to answer specific questions related to the safety
and efficiency for oral feeding. However, a full discussion of this is beyond the scope of this article and the
reader is referred to http://www.nature.com/gimo/contents/pt1/full/gimo17.html.

Management of Feeding and Swallowing Problems in Pediatrics
Management decisions are made in light of the total child with consideration for medical/surgical, nutrition,
oral sensorimotor, behavioral, and psychosocial factors. Intervention strategies are focused on primary
problem areas of deficit. Evidence-based practice guidelines are needed. Airway stability and adequate
nutrition/hydration status are prerequisites for all oral sensorimotor and behavioral approaches to increase
the volume of oral feeding or to improve oral skills to expand food textures and to increase efficiency. Initial
efforts to improve caloric intake may include increasing caloric density of food, as per the dietitian and
physician, along with making adjustments of food textures to improve efficiency and safety or oral feeding.
Adequate fluid intake is critical to meet hydration needs and to minimize potential of constipation, which can
be a major complicating factor in facilitating hunger, appetite, and interest in feeding.
Oral sensorimotor intervention involves strategies related to the function of oral structures for bolus
formation and oral transit that are under voluntary neurologic control, that is, the jaw, lips, cheeks, tongue,
and palate. Techniques vary widely among therapists with little evidence of efficacy, efficiency, and
outcomes. Some children appear to improve oral function when foods vary on the basis of texture, tastes,
and temperature. Other children show significantly improved oral skills and timing of swallowing with posture
and position changes. Frequently used strategies include tapping or stroking the face and using a ―Nuk®‖
brush or other kinds of stimulation. Parents and therapists report that this kind of stimulation will ―wake up
the system‖ and then the child will swallow more quickly and more firmly. However, data are sorely lacking.
Goals of specific exercises usually relate to improved strength and coordination, but without defined
objective measures of outcomes.
Professionals and parents do not disagree about the importance of adequate nutrition/hydration. However,
there is more likely to be disagreement regarding the need for a gastrostomy tube (GT). It is not unusual for
parents to need some time, at least a few weeks or even months, before they agree to a GT. A nasogastric
tube may be used for a few weeks as a test to determine if the child tolerates needed volume of liquid per
feeding without discomfort or emesis. The nasogastric tube feeds also provide an opportunity to monitor
weight gain. If nonoral feeds are likely to be required for longer than several weeks, not necessarily for total
oral feeding but perhaps just to meet fluid requirements or for medications, a GT should be considered. A
feeding GT often relieves stress on the caregivers by allowing freedom from fear of malnutrition. More
efficient caloric delivery also frees time for other more pleasurable interactions with the child. Some oral
therapy should continue at appropriate levels to ensure the continued experience and maximal development
of oral skills over time. Speech-language pathologists can train parents, who can then take advantage of
offering tastes during several brief ―practice‖ sessions each day. Duration of each session should be only
about 5 to 10 minutes in these circumstances. When a child is on bolus feeds, optimal timing for
―pleasurable practice‖ is likely to be shortly before the start of the tube feeding, providing the child does not
show aversive reactions to the tube feedings.
Data on evidence-based research are needed. All therapeutic approaches have a primary goal for each
child to experience healthy, safe, and pleasurable oral feeding, whether the child is a total oral feeder or gets
just limited quantities and types of food for practice and pleasure. Pulmonary stability and nutritional well-
being are always the primary goals for all infants and children.
Section II: Gut Motility and Enteral Feeding Tolerance with an Emphasis on
Premature Infants

The gastrointestinal tract is a complex organ that starts at the mouth and ends at the anus. Its functions
include mastication of food, digestion and absorption of nutrients, elimination of waste, and protection of the
host from infectious organisms and toxins. Normal intestinal motility is important for each of these functions.
When normal motility is absent or impeded a variety of diseases and/or disorders may occur.
Much information now exists concerning gastrointestinal motility in adults. However, we are just beginning to
understand the developmental aspect and the importance of motility in premature and term infants.
Gastrointestinal Motility
When considering motility in adults and children, the intestine may be divided into segments that are
separated by sphincters. Food introduced into the mouth is masticated, mixed with fluid, electrolytes,
immunoglobulins, and enzymes. The mixture is delivered to the esophagus, propelled distally through the
gastroesophageal sphincter and into the stomach where it is churned with additional fluid, electrolytes, acid,
and enzymes. The mixture then transits the pylorus and empties into the small intestine. Long-chain fats and
triglycerides present in the mixture empty slowly from the stomach. Liquids low in fat have a more rapid
transit into the small intestine where digestion continues and where nutrients are absorbed as they move
fairly rapidly through the small intestine. Ingested material not digested and absorbed is delivered to the
colon through the ileocecal valve. Transit slows as the colon reabsorbs water, and the liquid chyme is
propelled by peristalsis into the transverse and descending colon. By the time waste reaches the sigmoid
colon and rectum, much of the water has been reabsorbed. The fecal mass is then compact and ready for
elimination.
Esophagus
Motility in each of the gastrointestinal segments is unique to that part of the intestine. The esophagus can be
divided into three functional regions: upper esophageal sphincter (UES), esophageal body, and lower
esophageal sphincter (LES). The coordinated motor pattern of the esophagus, or primary peristalsis, is
initiated by the act of swallowing. A rapidly progressing pharyngeal contraction transfers the bolus through a
relaxed UES into the esophagus (Fig 1). As a swallow is initiated, there is laryngeal elevation as the
swallow-bolus passes from the pharynx, across the UES, and into the proximal esophagus. As the UES
closes, a progressive circular contraction begins in the upper esophagus and proceeds distally along the
length of the esophageal body to propel the bolus through a relaxed LES. The LES is not an anatomically
discrete sphincter but a high-pressure zone (Fig 1). Secondary peristalsis is a progressive contraction in the
esophageal body that is not induced by a swallow, but rather by stimulation of sensory receptors in the
esophageal body. This type of peristalsis is usually induced in two ways: by luminal distention from refluxed
gastric contents or following incomplete clearing of esophageal contents by primary peristalsis.
Full-size image (345K)

FIG 1. Esophageal motor events in response to a swallow. The UES relaxes when the swallow-bolus moves
from the pharynx into the proximal esophagus. The contraction wave moves down the esophagus and as it
approaches the LES there is relaxation of that high pressure zone. *While every effort has been made to
locate the copyright owner of this work, Academy Professional Information Services, we have been unable
to do so and obtain permission for the reproduction of this figure. Given its scientific value, we have taken
the step of reproducing it here and invite anyone with a claim to the copyright of this work to contact us at
212-633-3957.
View Within Article
Physiologically, the LES in children is a 2- to 3-cm-long segment of tonically contracted smooth muscle at
the distal end of the esophagus. Intraabdominal pressure, gastric distention, peptides, hormones, various
foods, and many drugs modify the LES pressure. When swallowing, LES relaxation is mediated via
preganglionic, cholinergic vagal fibers in addition to postganglionic, noncholinergic, nonadrenergic nerves.
However, the LES can also transiently relax independent of swallowing, and an increased proportion of this
type of inappropriate relaxation has been reported in children with gastroesophageal reflux.[24] and [25]
Stomach and Small Intestine
The stomach mixes the food-bolus with additional fluid, electrolytes, and enzymes and propels the chyme
toward the pylorus. The mixture is emptied into the proximal small intestine. Two distinctive patterns of
motility may occur in the small intestine: postprandial and interdigestive.
Postprandial Small Intestinal Motility
Following a meal, there can be segmentation contractions of the stomach and small intestine that chop, mix,
and roll chyme, and/or peristalsis, which propels the chyme toward the large intestine.
Interdigestive Small Intestinal Motility
This pattern of motility is seen between meals when the stomach and small intestine are devoid to a large
extent of food and chyme. During this period, so-called housekeeping contractions originate in the gastric
pacemaker or proximal small intestine and propagate down the small intestine, sweeping it clean of debris.
This pattern is called the migrating motor complex. The migrating motor complex consists of three distinctive
contraction patterns or phases (Fig 2). Phase 1 is a motor quiescent period, which follows phase 3 and
precedes phase 2. Phase 2 is a period of irregular contractions, varying in amplitude and periodicity. Phase
3 is a distinctive pattern of regular, high-amplitude contractions repeating at a maximal rate for several
minutes. Each phase migrates proximal to distal. The term migrating motor complex best describes the
entire cycle, although it has been occasionally used interchangeably with phase 3.
Full-size image (128K)
FIG 2. Gastrointestinal motility pattern in a healthy adult. Note the cyclic occurrence of each phase of the
migrating motor complex. The most recognizable motor pattern is phase 3 (asterisks), which is distinguished

by a band of repetitive contractions. It is followed by phase 1, motor quiescence, and then phase 2, which is
characterized by periodic irregular contractions. Phase 3 starts either in the stomach or in the proximal small
intestine. *While every effort has been made to locate the copyright owner of this work, Academy
Professional Information Services, we have been unable to do so and obtain permission for the reproduction
of this figure. Given its scientific value, we have taken the step of reproducing it here and invite anyone with
a claim to the copyright of this work to contact us at 212-633-3957.
View Within Article
Motility in the small intestine, as in all parts of the digestive tube, is controlled by excitatory and inhibitory
signals from the enteric nervous system with input from the central nervous system. In addition, a number of
gastrointestinal hormones affect gastrointestinal motility.26
Colon
Three prominent patterns of motility are observed in the colon: (1) segmentated contractions; (2)
antiperistalic contractions which tend to propel fecal debris toward the cecum; and (3) mass movements. In
periods between meals, the colon is generally quiescent. Following a meal, colonic motility increases
significantly due in part to gastrocolic and duodenocolic reflexes. Several times each day mass movements
push feces into the rectum. When rectal volume increases to the appropriate threshold, the internal anal
sphincter relaxes. When this is followed by voluntary relaxation of the external anal sphincter, defecation
occurs. Figure 3 shows the sequence of pressure changes in the normal colon.26
Full-size image (159K)
FIG 3. This colonic motility pattern is characterized by high-amplitude propagated contractions (HAPCs)
starting in the descending colon and migrating both proximally and distally. *While every effort has been
made to locate the copyright owner of this work, Academy Professional Information Services, we have been
unable to do so and obtain permission for the reproduction of this figure. Given its scientific value, we have
taken the step of reproducing it here and invite anyone with a claim to the copyright of this work to contact
us at 212-633-3957.
View Within Article
This complex and coordinated mechanism which moves ingested nutrients and fluid through the
gastrointestinal tract is immature at birth. It is common to see this immaturity manifest as gastroesophageal
reflux, abdominal distention, or sometimes diarrhea and/or constipation. We have recently gained a better
understanding of the development of gastrointestinal motility. Hopefully, as we continue to explore this new
area of research, improved methods for feeding premature and full-term newborns will be developed.
Developmental Aspects

Mouth and Esophagus
The gastrointestinal tract is essentially fully formed by 11 weeks of gestation, when swallowing of amniotic
fluid begins. By 18 to 20 weeks sucking movements appear, and at 37 weeks’ gestation a normal fetus can
swallow and process nearly 500 mL. of amniotic fluid a day.26
As early as 1983, Bernbaum and colleagues
studied nonnutritive sucking during the gavage feedings of 30 premature infants with birth weights less than
1500 g.27
All feedings were performed using oral-gastric feeding tubes. The control group (n = 15) was fed a
standard formula using set amounts of formula. The experimental group of 15 premature infants was fed the
same formula and amount. However, in the experimental group the oral-gastric tube was inserted through a
central aperture in a nipple that the infant sucked while being fed via the oral-gastric tube. This was defined
as nonnutritive sucking (NNS). The investigators found that NNS decreased intestinal transit time (increased
motility) and caused a more rapid weight gain despite comparable caloric intake, resulting in a shortened
hospital stay. They concluded that, although the physiologic mechanisms resulting from the NNS were not
elucidated, NNS may be an important factor to consider when feeding premature infants.27
More recently Pinelli and Symington reviewed the literature and set out to determine whether NNS in
preterm infants influences: (a) weight gain; (b) energy intake; (c) heart rate; (d) oxygen saturation; (e) length
of hospital stay; (f) intestinal transit time; (g) age at full oral feeds; or (h) any other clinically relevant
outcomes.28
Several data bases were searched including The Cochrane Central Register of Controlled
Trials. After a comprehensive search, the authors found that there was a significant decrease in length of
stay of premature infants receiving a NNS intervention. Other positive clinical outcomes of NNS were a more
rapid transition from tube to bottle feeding and better bottle-feeding performance. No negative outcomes
were noted. However, the review did not reveal a consistent benefit of NNS with respect to other major
clinical variables (weight gain, energy intake, heart rate, oxygen saturation, intestinal transit time, age at full
oral feeds, and behavioral state). Based on available evidence, the authors concluded that NNS in preterm
infants appeared to have some clinical benefit and did not have short-term negative effects.28
Primary esophageal peristalsis, induced by swallowing, begins during early fetal life. One aspect of
esophageal motility that has been studied in infants is the laryngeal chemoreflex. This collective response to
stimulation of the pharynx or larynx includes startle, rapid swallowing, apnea, laryngeal constriction,
hypertension, and bradycardia—mechanisms that protect the fetus living in an aqueous environment from
amniotic fluid aspiration. The development of these mechanisms prepare the fetus for postnatal adaptation.
The chemoreflex can be studied in infants by stimulating the pharynx with saline or water.29
In some infants,
laryngeal chemoreflexes may be ineffective, leading to aspiration, or they may be overly effective, resulting
in apnea. However, in infants born extremely premature, or with congenital anomalies or hypoxic/ischemic
encephalopathy, feeding difficulties may precede the diagnosis of delayed neurologic development.
There is not much evidence of esophageal defense mechanisms against gastroesophageal reflux (GER) in
infants, although a wealth of information exists from adult studies. Using new techniques, Jadcherla and
colleagues have characterized esophageal protective phenomena in developing infants.29
Their study
apparatus consists of a water-perfusion manometry system with a specially designed manometric catheter.
The researchers infuse varying volumes of air, water, or apple juice into the mid-esophagus and note
responses of the upper gastrointestinal tract to these stimuli. They have identified three responses to the
stimuli: (a) occurrence of esophageal peristalsis unrelated to a swallow (secondary peristalsis); (b) increase
in UES pressure; and (c) occurrence of primary peristalsis. These protective reflexes were elicited reliably
and safely.29

With this new technology, we may be able to study feeding techniques and nutrient formulations that
minimize recruitment of these protective mechanisms. Perhaps this information will lead to infant formulas
that are better tolerated and associated with less GER.
Stomach
It is common practice to check gastric residuals (GR) before feeding very low birth weight infants. The
gastric residual volume (GRV) is regarded as an objective parameter for feeding intolerance in premature
and term infants. Increased pregavage residuals are regarded as one of the gastrointestinal manifestations
of stage I (suspected) necrotizing enterocolitis. The definition of increased GR, however, and its relation to
feeding intolerance has never been studied in a systematic manner during enteral feeding of extremely low
birth weight infants (ELBW: <1000g). Furthermore, the presence of gastric fluid, which is green, suggests
poor emptying or reflux of bile into the stomach and may prompt the suspension of feedings or the initiation
of diagnostic procedures. However, the significance of green GR and its impact on feeding intolerance has
not been studied in ELBW infants. Mihatsch and coworkers in Germany studied 99 ELBW premature infants
in regards to GR volume and green gastric aspirate.30
Using a standardized protocol, premature infants were
evaluated from day 3 to day 14 of life. At 48 hours of age, milk feedings were started at 12 mL/kg/d, divided
over 12 feeding periods each day. When GR were checked before each feeding, a GRV of 2 mL or less was
tolerated by infants who weighed <750 g at birth and a gastric residual volume up to 3 mL was tolerated by
infants weighing >750 g at birth. When GRV increased markedly, feedings were reduced or withheld. The
color of the GR was also assessed. The investigators found that the median volume of formula tolerated by
infants at 14 days of life was 103 mL/kg/d. The mean GRV for infants in the study did not correlate with the
amount that was taken on the 14th day. Furthermore, green GR did not correlate with the feeding volume,
which could be tolerated on day 14. The authors concluded that GRV below 2 and 3 mL, respectively, for the
two weight groups (<750 and >750 g) and a green color of the residual should not slow down the
advancement of feeding volumes.30
Gastric emptying has also been studied in older infants. Tolia and coworkers designed a prospective study
using gastric scintigraphy to assess gastric emptying and the frequency of GER when three different
formulas were fed infants.31
Twenty-eight infants under 1 year of age with GER were studied. They were
given three different formulas using the same volume per single feeding: a casein-predominant formula, a
soy formula, and a whey-hydrolysate formula were all given in randomized order. A significant difference (P
< 0.05) in GER episodes was noted when comparing the casein-predominant and whey hydrolysate
feedings. Gastric emptying was more rapid with the whey-hydrolysate formula compared with the casein-
based formula. The presumption is that casein-based formulas curdle in the stomach and slow gastric
emptying, whereas whey-based formulas do not curdle and clear the stomach more rapidly. The curdling
predisposes the infant to GER. The authors suggest ―that formula selection may be important in the
treatment of conditions associated with delayed gastric emptying.‖31
Others have noted similar findings when
comparing whey-based and casein-formula feedings in spastic quadriplegic children.32
Small Intestine
As survival of preterm infants has increased, so has morbidity related to immaturity of the gastrointestinal
tract. Although a variety of enteral feeding regimens are used for feeding preterm infants, few studies have
tested the efficacy of these regimens, because no direct measure of intestinal motility has been available.

However, experience suggests that preterm infants may tolerate enteral feedings well using special formulas
designed for premature infants if they are fed in a carefully prescribed regimen. Physical characteristics of
the nutrients, such as caloric content, osmotic load, pH, fat content, and fiber content, may all affect gastric
emptying and gastrointestinal motility in infants as they do in adults.
Jadcherla and others recently developed a technique to record small intestinal motility in preterm and term
infants.[33] and [34]
As in the adult, intestinal motor activity in the neonate changes in response to enteral
feeding. When slow-infusion feedings are given to preterm or term infants, duodenal motor activity
significantly increases postprandially compared with that seen during fasting. This ―fed response‖ may be
altered by the rate of infusion and the concentration of the formula. Using a low-compliance, continuous
perfusion manometry system, motor activity responses to different formulas can be assessed in preterm and
term infants.[33] and [34]
Jadcherla and his group studied two commercially available formulas of different nutrient densities: Similac
20 (20 cal/oz) and Similac Special Care (24 cal/oz).34
Infants in a very controlled fashion received both
formulas at different times. Motor responses during the feeding of the two formulas differed significantly.
When the preterm infants were fed for the first time, their motor activity increased when they were fed the
lower calorie-dense formula, Similac 20. Motor activity decreased when fed the higher calorie-dense
formula. However, these differences in motor responses to the two formulas were not present 10 days later
when the infants were restudied using both formulas. The inhibition of motor responses to the calorically
denser formula early on may underlie the feeding intolerance infants experience when they are first fed
formula. However, this inhibitory response diminishes with age, suggesting that denser formulas can be
introduced later to preterm infants.34
Feeding Recommendations for Premature Infants
Although we are just beginning to appreciate the complexity of gastrointestinal motility in premature and full-
term infants and understand how formulas and feeding may influence gastrointestinal motility,
recommendations based on current evidence is available.35
Optimal nutrition is critical in the management of small, preterm infants. However, no standard has been set
for the precise nutritional needs of infants born prematurely. Present recommendations are designed to
provide nutrients to approximate the rate of growth and composition of weight gain for a normal fetus of the
same postmenstrual age and to maintain normal concentrations of blood and tissue nutrients. Generally,
intrauterine growth rate can eventually be achieved, but it is not obtained until well after the time of birth.
Nearly all ELBW infants experience significant growth retardation during their stay in the neonatal intensive
care unit. This is largely a result of the management of acute neonatal illnesses and gradual advancement of
feeding to minimize the risk of feeding-related complications, such as necrotizing enterocolitis.35
The quality of postnatal growth depends on the type, quantity, and quality of the feedings consumed.
Preterm infants fed standard infant formulas gain a higher percentage of their weight as fat when compared
with a fetus of the same maturity. The use of specially formulated preterm infant formulas and preterm
human milk fortifiers results in a composition of weight gain and bone mineralization closer to that of the
reference fetus.35
Randomized prospective trials of ELBW infants fed specially formulated preterm formulas (Table 6) have
shown significant improvements in growth and cognitive development when compared with feeding of
standard formulas for full-term infants.36

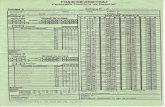
TABLE 6.
Nutrient data/liter for formulas used to feed low-birth-weight and prematurely born infants
Similac Special Care 24
Enfamil Premature Lipil
24
Neosure Advance
22 cal
Enfacare 22 cal
Liquid (Ross
Laboratories
Columbus, OH)
Liquid (Mead
Johnson,
Evansville, IN)
Liquid (Ross
Laboratories,
Columbus, OH)
Liquid (Mead
Johnson,
Evansville, IN)
Energy, kcal 806 810 746 740
Protein, g 22 24 19.4 21
Fat, g 43.8 41 41 39
Polyunsaturated, g
8.3 10.3 — —
Monounsaturated, g
3.5 4.5 — —
Saturated, g 32 26.2 — —
Linoleic acid, g 5.7 8.5 5.6 7.1
Carbohydrate, g
86.1 90 76.9 79
Reproduced from reference35>
with permission.
View Within Article
Recent findings concerning gastrointestinal motility and formula composition underscore the need for the
clinician to carefully plan and monitor the nutritional care of preterm infants during hospitalization and after
discharge. A consensus recommendation of nutrition experts on specific nutrient requirements in preterm
infants summarizes available data and recommendations and should be referred to for more detailed
information.[37], [38] and [39]
Hopefully, with a better understanding of gastrointestinal function, intestinal motility, and formula
composition, we will be able to design more appropriate formulas for premature and term infants.
Section III: Behavioral Treatment of Feeding Disorders
Feeding is an important part of the everyday life of infants and young children, and much parent–child
interaction occurs during feeding. About 25 to 40% of infants and toddlers are reported by their caregivers to
have feeding problems, mainly colic, vomiting, slow feeding, and refusal to eat.40
Severe feeding problems
are prevalent in 40 to 70% of children with developmental disabilities and chronic medical conditions.[40] and

[41] It has been suggested that many feeding disorders develop as a result of an organic condition but are
maintained over time by behavioral factors.41
Because of the prevalence of feeding disorders, busy
pediatricians will have ample opportunity during their careers to come in contact with these challenging
problems. They must be prepared to handle them and have a strategy as to how to approach the simple
uncomplicated problems and know when to refer more complicated patients to a tertiary center that has a
feeding team in place.
Classification
A review of the literature reveals several attempts to classify pediatric feeding disorders. Earlier, physicians
and investigators focused on failure to thrive as a diagnostic label. This diagnosis was made when an
infant’s or child’s weight and height measurements fell below the 5th percentile on growth standards or a
patient’s established growth curve decelerated across two major percentiles over time.42
The most
frequently cited classification of failure to thrive was that of organic or nonorganic. Organic failure to thrive
included problems related to structural or anatomic abnormalities involved with feeding (eg, defects of the
palate, tongue, and esophagus), neuromuscular problems (eg, cerebral palsy, paralysis), or other known
physiological reasons (eg, esophagitis, gastroesophageal reflux). In contrast, nonorganic failure to thrive had
origins based in disruptive social and environmental influences, which adversely influenced or contributed to
the problem.41
It has been suggested that the vast majority of childhood undernutrition in the United States
in the past has been attributable to the so-called nonorganic causes.43
The organic–nonorganic classification
was rigid and failed to account for feeding problems, which may have a combination of physiological,
environmental, and/or behavioral components. In most instances there are several reasons or causes for a
feeding disorder.41
In 1998 Burklow and her colleagues at Cincinnati Children’s Hospital Medical Center suggested an
alternative classification.41
Their Interdisciplinary Feeding Team (IFT) reported a classification system that
allowed them to categorize 103 children (64 males and 39 females) with feeding disorders. The children
were referred to the IFT for concerns related to poor oral intake and problems with sustained growth.
Disciples represented on the team included Pediatric Gastroenterology, Nursing, Nutrition, Occupational
Therapy, Psychology, and Speech Pathology. Intake evaluations were reviewed on each consecutive child
seen from September 1992 to September 1995. The IFT identified five categories that reflected the nature of
the complex feeding disorders in these infants and children: (1) structural abnormalities; (2) neurological
conditions; (3) behavioral issues; (4) cardiorespiratory problems; and (5) metabolic dysfunction.
Developmental delay or mental retardation was reported in 74% (n = 76) of all subjects. Thirty-eight percent
(n = 39) of the subjects were born prematurely (range, 24-36 weeks). There were no significant gender
differences for prematurity, developmental delay, or categorization of feeding problems. The percentage
occurrence of categories and clusters of categories are shown in Figure 4. It is of note that 85% of subjects
were categorized as having a behavioral component to their feeding disorder. Neurological conditions were
identified in 73% of the sample: structural abnormalities in 57% of the sample; cardiorespiratory problems in
7%; and metabolic dysfunction in 5% of the sample.41

Full-size image (10K)
FIG 4. Percent of subjects assigned to each category (alone or in combination). Bar 1: behavioral issues, n =
88 (85%); Bar 2: neurological conditions, n = 75 (73%); Bar 3: structural abnormalities, n = 59 (57%); Bar 4:
cardiorespiratory problems, n = 7 (7%); Bar 5: metabolic dysfunction, n = 5 (5%). *Reproduced from
reference 41
with permission.
View Within Article
The authors note that a majority of the feeding disorder patients had a combination of organic and
nonorganic problems. They therefore suggest that no attempt be made to force a choice between organic
and nonorganic characterization of feeding problems. They conclude that children referred to their team
represent those with the most complex types of feeding disorders, including structural anomalies, who have
been unresponsive to initial treatment efforts in the community by a single discipline such as Occupational
Therapy or Speech Pathology. Their report underscores the point that behavior plays an important role in
children with feeding problems.41
More recently, an alternative classification of feeding disorders has been suggested by Bernard-Bonnin.40
She suggests that early feeding disorders be classified according to the following: (1) structural
abnormalities; (2) neurodevelopmental disabilities; and (3) behavioral-feeding disorders (Table 7). Like
Burklow and her group, she suggests that there is often overlap. The first category, that of structural
abnormalities, includes three anatomic areas: the naso-oropharynx, the larynx and trachea, and the
esophagus. The second category, neurodevelopmental disabilities, is composed of conditions that disrupt
the process of learning to eat and result in oral-hypersensitivity and oral-motor dysfunction. The third
category, behavioral feeding disorders, includes six types of disorders (Table 7). It is not clear if pica should
be considered in this group since it is common for infants and children before 24 months of age to mouth
and occasionally eat nonnutritive substances. Pica should be considered only when the behavior persists for
longer than 1 month and is judged inappropriate for the developmental level of the child.42
TABLE 7.
Classification of feeding disorders
Structural abnormalities
• Abnormalities of the naso-oropharynx: choanal atresia, cleft lip or palate, Pierre Robin sequence, macroglossia, ankyloglossia
• Abnormalities of the larynx and trachea: laryngeal cleft, laryngeal cyst, subglottic stenosis, laryngo-tracheomalacia
• Abnormalities of the esophagus: tracheoesophageal

fistula, congenital esophageal atresia or stenosis, esophageal stricture, vascular ring
Neurodevelopmental disabilities
• Cerebral palsy
• Arnold–Chiari malformation
• Myelomeningocele
• Familial dysautonomia
• Muscular dystrophies and myopathies
• Möbius syndrome
• Congenital myotonic dystrophy
• Myasthenia gravis
• Oculopharyngeal dystrophy
Behavioral feeding disorders
• Feeding disorder of state regulation (0-2 months)
• Feeding disorder of reciprocity (2-6 months)
• Infantile anorexia (6 months-3 years)
• Sensory food aversions
• Feeding disorder associated with concurrent medical condition
• Posttraumatic feeding disorder
Reproduced from reference40
with permission.
View Within Article
Evaluating Feeding Problems
Bernard-Bonnin suggests that there are five key questions to be answered when evaluating feeding
disorders:
1 How is the problem manifested? 2 Is the child suffering from any disease? 3 Has the child’s weight and development been affected? 4 What is the emotional climate during meals? 5 Are there great stress factors present in the family?

She also suggests a thorough history and physical examination be obtained and laboratory investigations be
held to a minimum when infants have normal physical examinations, normal growth curves, and normal
developmental assessments.40
Linscheid notes that assessment of a feeding disorder can be accomplished by a number of standardized
questionnaires, by parent and/or child interaction observation schemes, and by interview.44
Verbal or written
information supplied by the referral source is important and reports from dieticians or language therapists
may help determine adequacy of the child’s current nutritional intake and possible oral-motor problems.
Questionnaires, designed to be completed by parents, yield information in terms of the nature and degree of
the feeding problem. The Childhood Eating Behavior Inventory and the Behavioral Pediatrics Feeding
Assessment Scale are good examples. Although these instruments are very important in research,
Linscheid has not found them to be useful in clinical practice.44
Although it is important to obtain information from the referring health care professional, an interview with the
parent or caregiver should serve as the main assessment strategy. During this interview, an attempt is made
to collect information in several areas. First, information should be gathered concerning the types, textures,
and variety of foods the child is eating. A 3- or 7-day food diary taken by the parents can be helpful.
However, in the absence of this, parents can fairly accurately recall the child’s intake over the past few days.
These data often constitute an adequate sample of overall nutrient intake.44
If the child is currently receiving tube feedings, it is important to get a thorough history of whether the patient
has ever eaten by mouth, when tube feedings were initiated, and the type of formula and the calories,
protein, and nutrient content of the tube feedings. Some children are on infusion pumps that administer
calories slowly into the stomach during the night or over much of the day. Others are fed by bolus feedings
or the deliverance of larger quantities (eg, 4 oz) over a shorter period of time using gravity, syringes, or
pumps. Parents should be asked whether the child shows any indication of hunger at any time throughout
the day. Children who have been on bolus feedings often indicate that they are hungry, either by their
behavior (becoming cranky) or by actually pointing to their feeding tube to indicate to the parent that they are
feeling hunger. Children on slow enteral infusion schedules are less likely to show signs of hunger.
If the child is not receiving tube feedings, it is important to document a typical eating day. Questions about
actual mealtime behaviors should reveal behavior problems. In some cases, the health care worker can
observe directly or by videotape a ―typical‖ feeding. Generally, misperceptions or inaccurate descriptions of
the problem by parents are usually not so great as to alter dramatically treatment decisions or cause a major
revamping of the treatment plan.44
The busy clinician in evaluating the infant or child should not ―rush to judgment.‖ This has been pointed out
in a publication almost 20 years ago.45
Two infants were described whose weight and/or height gradually
came to rank below the fifth percentile during the first 18 months of life. Numerous tests were performed,
and the diagnosis of gastroesophageal reflux led to fundoplication in each infant. The concept that higher
energy intakes result in greater increases in length led eventually to placement of a gastrostomy feeding
tube in each of the infants. Increases in weight during gastrostomy feedings had no effect on growth in
length. The vague concept of failure to thrive proved to be misleading in these two infants and obscured the
fact that constitutionally short children can fall below the 5th percentile in length at any time before the age
of 2 or 3 years.45
The difficulty in classifying and treating children with feeding disorders is underscored from a report by
Tolia.46
She reported seven infants and children who were between the ages of 13 and 30 months at the

time of presentation. They all failed to consume adequate calories and suffered delayed growth. No specific
etiology for the decreased intake was discovered. None had any developmental delay nor were there any
psychiatric conditions present in mothers. Changes in formula and psychologic intervention were
unsuccessful in modifying feeding habits except in two infants. All of the patients were supplemented with
enteral formulas. Three did not consume enough orally and needed nasogastric tube infusions, with
eventual placement of gastrostomy tubes in two. The third infant required continued nasogastric tube
feedings. A significant increase in caloric intake was associated with improvement in growth percentiles.
Weight and height percentiles improved in all and crept into the normal range in five and four patients,
respectively. Attempts at weaning off the supplements resulted in weight loss in all.46
This report
underscores the challenges the clinician faces in assessing and effectively treating infants and children with
feeding disorders.
Treatment
Appetite Manipulation
Motivation to eat can be related to deprivation of calories. Generally, calorie deprivation results in increased
appetite. How to make a child hungry and yet keep him or her safe is a major consideration in treatment
planning. Inducing hunger or stimulating appetite in a child is almost always as important, or in some cases
more important, for success than the specific behavioral contingencies which may be tried. This is especially
true for feeding problems related to an unusual variety of foods or to problems of food texture. The degree to
which hunger can be induced predicts the speed and degree of success.
Linscheid notes that the importance of motivation to eat can be demonstrated by a case with which he was
involved.44
A child was referred because he was taking 1 to 2 hours to eat each meal. The mother was
spending 3 to 6 hours a day attempting to feed the child. On interview, when asked what the child drinks, the
mother and grandmother, who were both at the interview, stated that the child consumed about ¾ of a gallon
of milk each day. Rough calculations suggested that this child was getting about 1800 calories a day from
milk. It was very easy to understand why the patient would have very little motivation to consume baby food
and why meals were taking so long to complete. The successful treatment of the child involved, first,
increasing oral intake of soft textured foods and then moving to normal textures and variety. This goal could
not be accomplished without a dramatic decrease in the calories obtained from the milk. There is no
behavioral contingency program strong enough to induce a child like this to dramatically increase his intake
of food as long as he is getting his daily caloric needs met with milk.44
The most basic form of appetite manipulation for children feeding by mouth is to simply restrict all calories
between meals, while continuing to offer water or other zero-calorie fluids during these periods. However,
some would suggest that an appetite stimulant such as cyproheptadine may be tried.[47] and [48]
This agent is
not without side effects.49
For children who are treated on an outpatient basis, it is very important to arrange daily weight checks and
hydration assessments and to teach parents the clinical signs of low blood sugar or dehydration. Parents
cannot be asked to take chances with their child’s health, and if they are not able to follow through with
appetite manipulation at home, the treatment most likely will be unsuccessful.44
Behavioral Contingency Techniques

Behavioral therapy is more efficacious in feeding disorders associated with tube feeding than nutrition
counseling alone.[50] and [51]
There are a number of straightforward behavioral procedures that have been
shown to be effective in the treatment of childhood feeding problems including those associated with tube
feedings (Table 8). These meal-time rules generally involve positive and negative reinforcement and mild
punishment. Rigid adherence to a specific technique may be counterproductive, and the appropriateness of
various techniques depends on behavioral changes that may occur during treatment. Feeding treatments
should initially be conducted by trained therapists or by parents serving as therapists. These strategies can
be based in the home or in the inpatient setting.52
A supportive therapist/parent should:
• Be engaging but not overwhelming. • Talk in a quiet and encouraging manner. • Be careful not to overwhelm with talking or behavior. • Seat the infant so that he/she is straight up and facing forward. • Sit directly in front of the infant. • Wait for the infant to pay attention and open up before feeding. • Feed when the infant wants to eat, but evolve structure. • Let the infant touch his/her food and feed himself/herself with their fingers. • Let the infant decide how fast he/she wants to eat. • Respect the infant’s food preferences. • Respect the infant’s caution: all children learn to eat eventually. • Let the infant eat as much as desired. • Stop when the infant indicates that he/she is full. TABLE 8.
Food rules applicable to children beyond infancy
Scheduling
• Regular mealtimes; only planned snacks added
• Mealtimes no longer than 30 minutes
• Nothing offered between meals except water
Environment
• Neutral atmosphere (no forcing of food)
• A sheet should be placed under the chair to catch any mess
• No game playing during feeding
• Food never given as reward or present
Procedures
• Small portions are offered
• Solids are given first and fluids last
• Self-feeding encouraged as much as possible
• Food is removed after 10-15 minutes if the child plays

without eating
• Meals are terminated if the child throws food in anger
• Wiping a child’s mouth and cleaning up occurs only after the meal is completed
Reproduced from reference40
with permission.
View Within Article
In the inpatient treatment model, meals are usually time restricted to a maximum of 25 minutes. This time
limitation is used for two reasons: First, it is felt that longer meal times, particularly in the early stages when
meals are distressing, may serve to reinforce the child’s perception that feeding is an unpleasant or stressful
activity. Second, children without feeding problems usually eat within this time period, and the cessation of
the meal after 20 or 25 minutes helps ensure that the child will be hungry for the next meal. Treatment meals
are usually done three times a day, 7 days a week. There are three treatment meals per day with 3½ to 4
hours in between feedings.44
The final step in inpatient treatment is to have the parent feed the child with the therapist nearby (either
observing through a one-way mirror or standing in the hallway) in case there are questions or problems.
Discharge from the hospital can be considered when three criteria are met. The first is that the child is taking
sufficient calories to at least maintain his or her weight. The second is that treatment goals for variety are
achieved. The third requirement is that the parent and the therapist agree that the parent has acquired the
necessary feeding techniques and is capable of implementing them at home.44
In summary, Chatoor suggests that, because feeding disorders are diverse in etiology and frequently involve
unusual or abnormal behavior of the infant and/or the mother in addition to medical issues that may relate to
choking, severe vomiting, reflux, or the intermittent insertion of a nasogastric tube, the behavioral therapy
should be tailored to the etiology of the feeding disorder.42
This requires a multimember team of health care
workers with experience in diagnosing and treating feeding disorders. However, it is up to the primary health
care provider to know when to refer these patients and how to search out resources that are best matched
for each infant and child.
Section IV: Feeding Issues in the Disabled Child
The subject of feeding disabled children has gained the attention of health professionals over the past 15
years. The Nutrition Committee of the Canadian Pediatric Society first addressed this issue in 1994 in the
publication, ―Undernutrition in children with a neurodevelopmental disability‖; a revision of the original
recommendations is currently in progress.53
The American Dietetic Association adopted a position statement
on ―Providing nutrition services for infants, children and adults with developmental disabilities and special
health care needs‖ in 2003.54
Then in 2004, the American Academy of Pediatrics devoted a chapter in their
Pediatric Nutrition Handbook entitled, ―Nutritional support for children who are neurologically impaired.‖55
Finally, a consensus paper published in 2006 addressed this same subject, ―Nutrition support for
neurologically impaired children: a clinical report of the North American Society for Pediatric
Gastroenterology, Hepatology, and Nutrition.‖56
This fourth section draws in part from information presented in these four documents.

Magnitude of the Problem
Infants and children with developmental disabilities have diagnoses and conditions that place them at
nutritional risk. A developmental disability may be the result of identified etiologies (eg, chromosomal
abnormalities, congenital anomalies, inherited metabolic disorders, specific syndromes, neuromuscular
dysfunction) or it may not be associated with any diagnosed condition. Occasionally, persons may have two
or more conditions (eg, cerebral palsy and epilepsy; Down syndrome and congenital heart disease).
Children with special health care needs are those who have or are at an increased risk for impaired physical
developmental, behavioral, and emotional problems which require health and related services of a type or
amount beyond that required by healthy children.57
A survey of children from birth to 3 years of age with
developmental delays in early intervention programs found 79 to 90% had one or more nutrition risk
indicators.54
The Centers for Disease Control and Prevention reported that 17% of children under 18 years
of age have some type of developmental disability.58
Undernutrition, growth failure, overweight, micronutrient deficiencies, and osteopenia are nutritional
comorbidities that affect the neurologically impaired.56
Monitoring neurologically impaired children for
nutritional comorbidities should be an integral part of their care. Early involvement by a multidisciplinary
team of physicians, nurses, dieticians, occupational and speech therapists, psychologists, and social
workers is essential to prevent the adverse outcomes associated with feeding difficulties and poor nutritional
status. Undernutrition and overweight lead to increased health care use, hospitalization, and physician visits,
as well as diminished participation in home and school activities. Careful evaluation and monitoring of
severely disabled children for nutritional problems are warranted because of the increased risk of nutrition-
related morbidity and mortality.59
Undernutrition is a frequent problem in children with severe CP who often have significant impairment of
their eating and swallowing mechanisms.53
CP occurs in 3 to 4 per 1000 live births, and one-third of these
children are severely affected.60
Even without intervention, some children with a severe disability live more
than 30 years; the average death rate in severe cerebral palsy is 5% or less per year. Pseudobulbar palsy,
which occurs in severe CP, affects eating and swallowing. As a result, food intake is decreased and eating
time is increased. Thus oral feeding may meet with little success, despite the efforts of caregivers. GER and
aspiration of food and severe constipation often compound the problem.53
The early alternative to oral feeding has been nasogastric tube feedings; however, the use of such tubes is
associated with unacceptable long-term complications—mainly reflux and vomiting. A new approach to
feeding disabled children is through a percutaneous gastrostomy tube, which bypasses most problems with
nasogastric tube feeding. In the past most children with severe CP lived in institutions. Today they return to
the community to live in group homes or with their families. This makes a systematic approach to the
nutrition support even more important.53
Many of these children have clinically important GER regardless of whether they have been fed through a
nasogastric tube. The cause of reflux in such patients is unclear; it is probably related to intestinal
dysmotility, delayed gastric emptying, and the fact that many of them spend many hours in a recumbent
position.[32] and [53]
If reflux is significant and frequent, it may increase the risk of food aspiration and aspiration
pneumonia. In addition to reflux, aspiration of food or liquids while being fed orally is a risk in children with a
severe disability.53

Body mass index and other anthropometric parameters have been used to better determine if children with
developmental delay were obtaining appropriate nutritional support. Sanchez-Lastres and coworkers
evaluated the nutritional status of 128 developmentally delayed children.61
Historical information and multiple
anthropometric data were obtained for each subject. Analysis of the data suggested that 33% of subjects
showed borderline or definite malnutrition. Children with definite malnutrition had significantly lower IQ
scores than those who were better nourished. The authors concluded that malnutrition as determined by
anthropometric variables occurs with a high prevalence in developmentally delayed children and that the
prevalence of malnutrition increases with age and increasing IQ deficit.61
It is clear that developmental disabilities are common and that children with developmental disabilities are at
risk for malnutrition and it comorbidities.
Nutritional Needs
Campanozzi and coworkers studied body mass index and anthropometric variables in 21 children with CP,
GER, and/or chronic constipation and correlated these parameters with motor function.62
One aim of the
investigators was to evaluate the role of nutrition on gross motor ability using Gross Motor Function Measure
before and after 6 months of nutritional rehabilitation. The authors found that malnutrition and
gastrointestinal disorders were common in children with CP. However, improved nutrition status, particularly
a gain in fat-free mass, appeared to have a positive impact on motor function in children with CP.62
Nutritional factors such as inadequate intake, increased losses, and altered energy requirements clearly
contribute to the poor nutritional status of patients with neurological disabilities.
Inadequate Intake
Inadequate intake seems to be a major factor contributing to malnutrition since aggressive nutritional
supplementation improves growth.55
An increase in weight for length Z-score from −2.71 to −1.18 was seen
23 months after gastrostomy and tube feedings were initiated in a group of disabled children.55
Some note
an increase of 10 to 46% in body weight over 5 weeks with a 50% increase of intake by means of
nasogastric tube feedings.63
Children with CP spontaneously consume fewer calories than age-matched
control children.64
Reasons for inadequate intake are numerous. Oral-motor dysfunction is found in more
than 90% of children with cerebral palsy.65
Sucking and swallowing problems, inadequate lip closure,
drooling, and persistent extrusion reflex make oral feedings difficult. It is a major factor in the pathogenesis
of malnutrition in patients with CP since weight, height, and weight-for-height Z-scores are significantly lower
in patients with oral-motor dysfunction than in other patients.66
Because of their poor oral and fine-motor
skills, these children depend on a caretaker for feedings. Since they are often unable to communicate
hunger and satiety, the caretaker ends up regulating their intake. Often times, the task of feeding such a
child is difficult and time-consuming, and inadequate intake may ensue. It has been shown that the
caretaker often overestimates caloric intake and time spent feeding the child.55
In addition, GER may also
lead to food refusal, especially if reflux esophagitis is present.
Increased Losses
In addition to decreased intake, excessive losses may occur from spillage and frequent emesis.
Energy Requirements

Defining energy requirements is very important because of the patient’s inability to communicate hunger and
satiety and because of abnormal physical activity, body composition, and food intake. Unfortunately, energy
needs are poorly defined in this heterogeneous population. Energy intake in normally growing patients with
spastic quadriplegic CP fed exclusively by gastrostomy has been estimated in some studies at 60 ± 15% of
recommended daily allowance for gender and age, and 103 ± 32% of recommended daily allowance for
weight.55
Resting energy expenditure in well-nourished, nonambulatory, bedridden patients is significantly
less than that of healthy age-matched controls.67
In addition, resting energy expenditure per unit of body cell
mass is significantly reduced, suggesting a role of the central nervous system in energy regulation.
Therefore calculation of total energy needs based on healthy children overestimates the energy
requirements of children with spastic quadriplegic CP.67
Caloric needs of children with developmental disabilities should be individualized, taking into account basal
metabolic rate, muscle tone, activity level, and desired growth. A formula to calculate the energy needs of
children with severe CP has been developed by Krick and coworkers.68
It uses basal metabolic rate and
accounts for muscle tone, activity level, and growth factors (normal growth-for-height age and catch-up
growth). As can be seen from Table 9, increased motor-tone and increased activity result in a higher daily
caloric requirement. However, the best way to evaluate adequacy of nutritional therapy in a given patient is
to monitor response in terms of weight gain. Caloric intake can then be adjusted accordingly.69
TABLE 9.
Calories (kcal/d) = (BMR × muscle tone factor × activity factor) + growth factor. Where: BMR (kcal/d) = Body
surface area (m2) × standard metabolic rate (kcal/m
2/h) × 24 h
Muscle tone factor 0.9 decreased muscle tone
1.0 normal muscle tone
1.1 increased muscle tone
Activity factor 1.15 bedridden
1.2 dependent (wheel chair)
1.25 crawling
1.3 ambulatory
Growth factor 5 kcal/g of desired weight gain
Reproduced by permission from reference.55
View Within Article
Assessment
Medical History
Assessment of health status must include knowledge of the underlying disease to better understand its
natural history (ie, static versus degenerative versus temporary neurological impairment). The type of
intervention will differ depending on whether the underlying disease is a terminal condition, a short-term
reversible condition, or a chronic condition. In addition, the duration and the severity of the neurological
disability may correlate with a greater risk of malnutrition. The presence of other medical problems such as

chronic respiratory symptoms, recurrent pneumonia, GER, constipation, and the use of medication must be
evaluated and considered when planning nutritional intervention.55
Nutritional History
The nutritional history is of the utmost importance and must encompass all aspects of the feeding process. A
good evaluation of oral motor skills must be done since oromotor impairment is a major factor leading to
malnutrition. Swallowing function, including adequacy of lip closure, drooling, spilling, extrusion reflex,
incoordination, gagging, delayed swallowing, and symptoms suggestive of aspiration, such as choking and
coughing, should be evaluated. The amount of time spent feeding the child should be estimated. Feeding
efficiency in patients with severe CP is far below normal, as it may take them 12 to 15 times longer to chew
and swallow than normal children of the same weight. Even longer mealtime does not compensate for the
child’s feeding impairment and, as a consequence, caloric intake is often insufficient. Appetite and ability to
self-feed, as well as feeding schedule, must be taken into account. Sixty percent of patients with CP are
totally dependent on a caretaker for their intake.64
For the caretaker, often the parent, too much time spent
around meals may impair the parent–child relationship and take the caretaker away from other activities and
siblings. It is also important to assess parental perception of mealtime, as it is often perceived as a stressful
and not enjoyable experience.55
A review of a typical day’s food intake or a full 3-day food record will help assess caloric intake but also
adequacy of fiber, vitamin, and mineral intake. Food refusal or a recent change in feeding pattern may be
indicative of an underlying problem.
A careful review of the previous growth pattern is very important and growth charts for height and weight as
well as weight gain or weight loss must be recorded. Infants with CP who had low birth weight are at greater
nutritional risk.55
Physical Examination
Physical examination includes weight, height or length, and head circumference and signs of malnutrition or
specific nutrient deficiency. In addition, muscle tone, activity level, and skeletal deformities such as scoliosis
and contractures should be assessed.
Anthropometrics
Weight and length or height must be obtained at every visit and should be as accurate as possible, always
using the same technique and equipment. Weight should be measured on the same scale every time with
the child wearing little or no clothing. Length should be obtained supine in children under age 2 years or in
older children unable to stand. Linear growth assessment is important to detect chronic malnutrition but may
be difficult to obtain in children with severe contractures or scoliosis.
Laboratory Evaluation
Basic laboratory evaluation includes a complete blood count and iron studies, as iron-deficiency anemia
occurs frequently. Serum albumin and prealbumin will reflect nutritional adequacy in the previous month and
week, respectively. Serum electrolyte and blood urea nitrogen may help in assessing hydration status.55
Recommendations
The following recommendations are based on existing, mainly descriptive, studies and on expert opinion.53

Secondary undernutrition due to an eating problem in children with CP and other neurodevelopmental
disabilities should be treated or, ideally, prevented. The management of undernutrition in children with
neurodevelopmental disability is best performed by a multidisciplinary team. Restoring the nutrition of these
children and reducing the time spent feeding them each day should be regarded as an important part of their
general care. The nutritional status of these children is best determined by techniques that measure body fat
stores, for which there are normative data, such as triceps skinfold measurements.
Treatment should start with high-energy supplementation, given orally. However, in children with a severe
disability, therapy may necessitate tube feeding, either to supplement oral feeding or to replace it. The
advent of percutaneous enterostomy has introduced a welcome alternative for children who require tube
feeding for more than 6 to 8 weeks. Daily energy needs are lower in patients with a neurodevelopmental
disability than in other patients because they are inactive and have reduced muscle mass; energy needs
range from 2900 to 4600 kJ per day. Hence, formulas designed for infants or children less than 6 years of
age should be used because of their higher ratios of nutrients to energy (Table 10).
TABLE 10.
Formulas
Infant Pediatric Adult
Cow milk Cow milk Protein blend
Enfamil Lipil Kindercal Boost
Similac Advance Nutren Jr. Ensure
Pediasure Nutren
Osmolyte
Soy
Enfamil Prosobee Lipil — —
Good Start Supreme Soy — —
Similac Isomil Advance — —
Partially hydrolyzed (whey-based)
Good Start Supreme DHA & ARA
— —
Hydrolysate (casein) Hydrolysate (whey)
Hydrolysate (whey)
Nutramigen Lipil Peptamen Jr. Peptamen
Pregestimil
Alimentum
Amino acids Amino acids Amino acids
Elecare Elecare Vivonex TEN
Neocate Neocate 1+
Vivonex Pediatric
Reproduced by permission from reference56
.

View Within Article
In children with mild disabilities, oral motor skills should be maintained and improved. One effective strategy
is to feed the child through an enterostomy tube only when he or she is asleep, usually at night. The child is
then likely to get thirsty and hungry during the day and want to eat. This gives the caregiver or therapist an
opportunity to promote oral-motor skills.53
Other Considerations
There are issues concerning the feeding of disabled children which require additional study and continued
experience.53
These are noted below.
1 The management of children with a progressive neuromuscular disability must be considered individually, with the fully informed consent of parents and caregivers. For many of these children, enterostomy, gastrostomy, or jejunostomy feedings have helped improve their quality of life. 2 Many and perhaps all children with a neurodevelopmental disability have intestinal dysmotility, evidenced by gastroesophageal reflux, delayed gastric emptying, and constipation. A better understanding of intestinal function and motility and their management is needed. 3 Little is known about the nutrient needs of patients with CP and other neurodevelopmental disabilities. Existing pediatric enteral products have a limited calcium and phosphorus content. Bone mineralization in these children should be evaluated to determine whether present levels of calcium and phosphorus intake are too low. 4 Studies are needed to determine the best behavioral approaches to children whose oromotor skills have advanced to the point that they are capable of eating but who are unable to eat because of behavioral problems. Hopefully, continued research will improve our ability to assess these patients and increase our
understanding of how best to meet their specific nutrient requirements. This will allow us to optimize the
nutritional status, development, and health of each child.
References
1 J. Laitman and J. Reidenberg, Specializations of the human upper respiratory and upper digestive
systems as seen through comparative and developmental anatomy, Dysphagia 8 (1993), pp. 318–325. Full
Text via CrossRef | View Record in Scopus | Cited By in Scopus (31)
2 P.B. Sullivan, B. Lambert, M. Rose, M. Ford-Adams, A. Johnson and S. Griffiths, Prevalence and severity
of feeding and nutritional problems in children with neurological impairment: Oxford feeding study, Dev Med
Child Neurol 42 (2000), pp. 674–680. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus
(99)
3 J.L. Miller, B.C. Sonies and C. Macedonia, Emergence of oropharyngeal, laryngeal and swallowing activity
in the developing fetal upper aerodigestive tract: an ultrasound evaluation, Early Hum Dev 71 (1) (2003), pp.
61–87. Article | PDF (744 K) | View Record in Scopus | Cited By in Scopus (26)
4 M.G. Ross and M.J.M. Nyland, Development of ingestive behavior, Am J Physiol 43 (1998), pp. R879–
R893. View Record in Scopus | Cited By in Scopus (45)

5 J.I. Devries, G.H. Visser and H.F. Prechtl, The emergence of fetal behavior: II: Quantitative aspects, Early
Hum Dev 12 (1985), pp. 99–120. Abstract | PDF (1175 K) | View Record in Scopus | Cited By in Scopus
(99)
6 J.F. Bosma, Development of feeding, Clin Nutr 5 (1986), pp. 210–218. View Record in Scopus | Cited By
in Scopus (32)
7 N. Lazebnik and A. Many, The severity of polyhydramnios, estimated fetal weight and preterm delivery are
independent risk factors for the presence of congenital malformations, Gynecol Obstet Invest 48 (1999), pp.
28–32. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (7)
8 C. Lau, R. Alagugurusamy, R.J. Schanler, E.O. Smith and R.J. Schulman, Characterization of the
developmental stages of sucking in preterm infants during bottle feeding, Acta Paediatr 89 (2000), pp. 846–
852. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (52)
9 C. Lau and I. Kusnierczyk, Quantitative evaluation of infant’s nonnutritive and nutritive sucking, Dysphagia
16 (2001), pp. 58–67. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (23)
10 J.C. Arvedson and L. Brodsky, Pediatric swallowing and feeding: assessment and management (2nd
Edition), Singular–Thomson Learning, Albany, NY (2002).
11 I. Chatoor, S. Schaefer, L. Dickson and J. Egan, Non-organic failure to thrive: a developmental
perspective, Pediatr Ann 13 (1984), pp. 829–843.
12 K. Lorenz, Evolution and modification of behavior, University of Chicago Press, Chicago (IL) (1965).
13 R.S. Illingworth and J. Lister, The critical or sensitive period, with special reference to certain feeding
problems in infants and children, J Pediatr 65 (1964), pp. 840–848.
14 T. Yamamoto and A. Hirayama, Effects of soft-diet feeding on synaptic density in the hippocampus and
parietal cortex of senescence-accelerated mice, Brain Res 902 (2001), pp. 255–263. Article | PDF
(1365 K) | View Record in Scopus | Cited By in Scopus (19)
15 J.H. Kennell, M.A. Trause and M.H. Klaus, Evidence for a sensitive period in the human mother, Ciba
Found Symp 33 (1975), pp. 87–101. View Record in Scopus | Cited By in Scopus (8)
16 J.A. Mennella, C.P. Jagnow and G.K. Beauchamp, Prenatal and postnatal flavor learning by human
infants, Pediatrics 107 (2001), p. e88. Full Text via CrossRef
17 E. Tatzer, M.T. Schubert, W. Timischl and G. Simbruner, Discrimination of taste and preference for sweet
in premature babies, Early Hum Dev 112 (1985), pp. 23–30. Abstract | PDF (667 K) | View Record in
Scopus | Cited By in Scopus (9)

18 T.R. Maone, R.D. Mattes, J.C. Bernbaum and G.K. Beauchamp, A new method for delivering a taste
without fluids to preterm and term infants, Dev Psychobiol 23 (1990), pp. 179–191. Full Text via CrossRef |
View Record in Scopus | Cited By in Scopus (19)
19 S.A. Sullivan and L.L. Birch, Infant dietary experience and acceptance of solid foods, Pediatrics 93
(1994), pp. 271–277. View Record in Scopus | Cited By in Scopus (105)
20 A.T. Galloway, Y. Lee and L.L. Birch, Predictors and consequences of food neophobia and pickiness in
young girls, J Am Diet Assoc 103 (2003), pp. 692–698. Article | PDF (228 K) | View Record in Scopus |
Cited By in Scopus (44)
21 D.L. Hill and C.M. Mistretta, Developmental neurobiology of salt taste sensation, Trends Neurosci 13
(1990), pp. 188–195. Abstract | PDF (1110 K) | View Record in Scopus | Cited By in Scopus (32)
22 J.A. Mennella, Development of the chemical senses and the programming of flavor preference:
Physiologic/immunologic responses to dietary nutrients: role of elemental and hydrolysate formulas in
management of the pediatric patient, Report of the 107th Conference on Pediatric Research 9, Ross
Products Division, Abbott Laboratories, Columbus, OH (1998), pp. 201–208.
23 D.T. Link and C.D. Rudolph, Gastroenterology and nutrition: feeding and swallowing. In: C.D. Rudolph
and A.M. Rudolph, Editors, Rudolph’s Pediatrics (21st Edition), McGraw–Hill, New York (2003), p. 1382.
24 S. Cucchiara, M. Bortolotti, R. Minella and S. Auricchio, Fasting and postprandial mechanisms of
gastroesophageal reflux in children with gastroesophageal reflux disease, Dig Dis Sci 38 (1993), pp. 86–92.
Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (50)
25 S.L. Werlin, W.J. Dodds, W.J. Hogan and R.C. Arndorfer, Mechanisms of gastroesophageal reflux in
children, J Pediatr 97 (1980), pp. 244–249. Abstract | PDF (415 K) | View Record in Scopus | Cited By in
Scopus (53)
26 In: P.E. Hyman and C. Di Lorenzo, Editors, Pediatric gastrointestinal motility disorders, Academy
Professional Information Services, Inc, New York (1994), pp. 1–436.
27 J.C. Bernbaum, G.R. Pereira, J.B. Watkins and G.J. Peckham, Nonnutritive sucking during gavage
feeding enhances growth and maturation in premature infants, Pediatrics 71 (1983), pp. 41–45. View Record
in Scopus | Cited By in Scopus (72)
28 J. Pinelli and A. Symington, Non-nutritive sucking for promoting physiologic stability and nutrition in
preterm infants, Cochrane Database Syst Rev 4 (2005) CD001071.

29 S.R. Jadcherla, R.G. Hoffmann and R. Shaker, Effect of maturation of the magnitude of
mechanosensitive and chemosensitive reflexes in the premature human esophagus, J Pediatr 149 (2006),
pp. 77–82. Article | PDF (284 K) | View Record in Scopus | Cited By in Scopus (14)
30 W.A. Mihatsch, P. von Schoenaich, H. Fahnenstich, N. Dehne, H. Ebbecke and C. Plath et al., The
significance of gastric residuals in the early enteral feeding advancement of extremely low birth weight
infants, Pediatrics 109 (2002), pp. 457–459. Full Text via CrossRef | View Record in Scopus | Cited By in
Scopus (43)
31 V. Tolia, C.H. Lin and L.R. Kuhns, Gastric emptying using three different formulas in infants with
gastroesophageal reflux, J Pediatr Gastroenterol Nutr 15 (1992), pp. 297–301. Full Text via CrossRef |
View Record in Scopus | Cited By in Scopus (49)
32 M.D. Fried, V. Khoshoo, D.J. Secker, D.L. Gilday, J.M. Ash and P.B. Pencharz, Decrease in gastric
emptying time and episodes of regurgitation in children with spastic quadriplegia fed a whey-based formula,
J Pediatr 120 (1992), pp. 569–572. Abstract | PDF (328 K) | View Record in Scopus | Cited By in
Scopus (29)
33 W.J. Koenig, R.P. Amarnath, V. Hench and C.L. Berseth, Manometrics for preterm and term infants: a
new tool for old questions, Pediatrics 95 (1995), pp. 203–206. View Record in Scopus | Cited By in Scopus
(19)
34 S.R. Jadcherla and C.L. Berseth, Acute and chronic intestinal motor activity responses to two infant
formulas, Pediatrics 96 (1995), pp. 331–335. View Record in Scopus | Cited By in Scopus (9)
35 In: R.E. Kleinman, Editor, Nutritional needs of the preterm infant. Pediatric Nutrition Handbook. American
Academy of Pediatrics (5th Edition), American Academy of Pediatrics, Elk Grove Village (IL) (2004), pp. 23–
54.
36 R. Morley and A. Lucas, Influence of early diet on outcome in preterm infants, Acta Paediatr Suppl 405
(1994), pp. 123–126. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (16)
37 In: R.C. Tsang, A. Lucas, R. Uauy and S. Zlotkin, Editors, Nutritional needs of the preterm infant:
scientific basis and practical guidelines, Williams & Wilkins, Baltimore, MD (1993).
38 R.A. Evans and P. Thureen, Early feeding strategies in preterm and critically ill neonates, Neonatal Netw
20 (2001), pp. 7–18. View Record in Scopus | Cited By in Scopus (8)
39 D.J. Raiten, S.C. Kalhan and W.W. Hay, Maternal nutrition and optimal infant feeding practices:
executive summary, Am J Clin Nutr 85 (2007), pp. 577S–583S.

40 A.C. Bernard-Bonnin, Feeding problems of infants and toddlers, Can Fam Physician 52 (2006), pp.
1247–1251. View Record in Scopus | Cited By in Scopus (7)
41 K.A. Burklow, A.N. Phelps, J.R. Schultz, K. McConnell and C. Rudolph, Classifying complex pediatric
feeding disorders, JPGN 27 (1998), pp. 143–147. Full Text via CrossRef | View Record in Scopus | Cited By
in Scopus (63)
42 I. Chatoor, Feeding and eating disorders of infancy and early childhood. In: J.M. Wiener and M.K.
Dulcan, Editors, Textbook of child and adolescent psychiatry (3rd Edition), American Psychiatric Publishing,
Inc, Washington, DC (2004), pp. 639–657.
43 R. Markowitz and C. Duggan, Failure to thrive: malnutrition in the pediatric outpatient setting. In: W.A.
Walker, J.B. Watkins and C. Duggan, Editors (3rd Edition), BC Decker Inc, London (2003), pp. 897–909.
44 T.R. Linscheid, Behavioral treatments for pediatric feeding disorders, Behav Modif 30 (2006), pp. 6–23.
Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (20)
45 G.B. Stickler, Gastrostomy dependence in two constitutionally short children, AJDC 142 (1988), pp. 937–
939. View Record in Scopus | Cited By in Scopus (1)
46 V. Tolia, Very early onset nonorganic failure to thrive in infants, JPGN 20 (1995), pp. 73–80. Full Text via
CrossRef | View Record in Scopus | Cited By in Scopus (22)
47 P.K. Lemons and N.N. Dodge, Persistent failure-to-thrive: a case study, J Pediatr Health Care 12 (1998),
pp. 27–32. Abstract | PDF (1235 K) | View Record in Scopus | Cited By in Scopus (5)
48 D.N. Homnick, J.H. Marks, K.L. Hare and S.K. Bonnema, Long-term trial of cyproheptadine as an
appetite stimulant in cystic fibrosis, Pediatr Pulmonol 40 (2005), pp. 251–256. Full Text via CrossRef | View
Record in Scopus | Cited By in Scopus (11)
49 M. Berger, J. White, L.B. Travis, B.H. Brouhard, R.J. Cunningham and R. Patnode et al., Toxic psychosis
due to cyproheptadine in a child on hemodialysis: a case report, Clin Nephrol 7 (1977), pp. 43–44. View
Record in Scopus | Cited By in Scopus (2)
50 D. Benoit, E.E.L. Wang and S.H. Slotkin, Discontinuation of enterostomy tube feeding by behavioral
treatment in early childhood: a randomized controlled trial, J Pediatr 137 (2000), pp. 498–503. Abstract |
PDF (82 K) | View Record in Scopus | Cited By in Scopus (26)
51 K.C. Byars, K.A. Burklow, K. Ferguson, T. O’Flaherty, K. Santoro and A. Kaul, A multicomponent
behavioral program for oral aversion in children dependent on gastrostomy feedings, JPGN 37 (2003), pp.
473–480. Full Text via CrossRef | View Record in Scopus | Cited By in Scopus (17)

52 E. Satter, The feeding relationship: problems and interventions, J Pediatr 117 (1990), pp. S181–S189.
Abstract | PDF (976 K) | View Record in Scopus | Cited By in Scopus (58)
53 J. Patrick, P.B. Pencharz, M. Belmonte, M. Ste-Marie, I.W. Killam, M.P. Boland, Nutrition Committee and
Canadian Paediatric Society, Undernutrition in children with a neurodevelopmental disability, Can Med
Assoc J 151 (1994), pp. 753–759.
54 American Dietetic Association, Providing nutrition services for infants, children, and adults with
developmental disabilities and special health care needs (2003) Available at:
http://www.eatright.org/cps/rde/xchg/ada/hs.xsl/advocacy..
55 In: R.E. Kleinman, Editor, Nutritional support for children who are neurologically impaired: Pediatric
Nutrition Handbook (5th Edition), American Academy of Pediatrics, Elk Grove Village (IL) (2004), pp. 629–
642.
56 V. Marchand, K.J. Motil and NASPGHAN Committee on Nutrition, Medical Position Paper: Nutrition
support for neurologically impaired children: a clinical report of the North American Society for Pediatric
Gastroenterology, Hepatology and Nutrition, JPGN 43 (2006), pp. 123–135. Full Text via CrossRef | View
Record in Scopus | Cited By in Scopus (10)
57 M. McPherson, P. Arango, H. Fox, C. Lauver, M. McManus and P.W. Newacheck et al., A new definition
of children with special health care needs, Pediatrics 102 (1998), pp. 137–140. View Record in Scopus |
Cited By in Scopus (279)
58 Centers for Disease Control and Prevention, Developmental Disabilities (2003) Atlanta, GA. Available at
http://www.cdc.gov/ncbddd/dd/default.htm..
59 L. Samson-Fang, E. Fung, V.A. Stallings, M. Conaway, G. Worley and P. Rosenbaum et al., Relationship
of nutritional status to health and societal participation in children with cerebral palsy, J Pediatr 141 (2002),
pp. 637–643. Abstract | PDF (79 K) | View Record in Scopus | Cited By in Scopus (42)
60 K.B. Nelson and J.H. Ellenberg, Epidemiology of cerebral palsy, Adv Neurol 19 (1978), pp. 421–435.
View Record in Scopus | Cited By in Scopus (50)
61 J. Sanchez-Lastres, J. Eiris-Punal, J.L. Otero-Cepeda, P. Pavon-Belinchon and M. Castro-Gago,
Nutritional status of mentally retarded children in north-west Spain: I. Anthropometric indicators, Acta
Paediatr 92 (2003), pp. 747–753. View Record in Scopus | Cited By in Scopus (15)
62 A. Campanozzi, G. Capano, E. Miele, A. Romano, G. Scuccimarra and E. Del Giudice et al., Impact of
malnutrition on gastrointestinal disorders and gross motor abilities in children with cerebral palsy, Brain Dev
29 (2007), pp. 25–29. Article | PDF (98 K) | View Record in Scopus | Cited By in Scopus (10)

63 J. Patrick, M. Boland, D. Stoski and G.E. Murry, Rapid correction of wasting in children with cerebral
palsy, Dev Med Child Neurol 28 (1986), pp. 734–739. View Record in Scopus | Cited By in Scopus (53)
64 S. Reilly and D. Skuse, Characteristics and management of feeding problems of children with cerebral
palsy, Dev Med Child Neurol 34 (1992), pp. 379–388. View Record in Scopus | Cited By in Scopus (73)
65 S. Reilly, D. Skuse and X. Poblete, Prevalence of feeding problems and oral motor function in children
with cerebral palsy: a community survey, J Pediatr 129 (1996), pp. 877–882. Article | PDF (593 K) |
View Record in Scopus | Cited By in Scopus (122)
66 J. Krick and M.A. Van Duyn, The relationship between oral-motor involvement and growth: a pilot study in
a pediatric population with cerebral palsy, J Am Diet Assoc 84 (1984), pp. 555–559. View Record in Scopus
| Cited By in Scopus (46)
67 M.P. Azcue, G.A. Zello, L.D. Levy and P.B. Pencharz, Energy expenditure and body composition in
children with spastic quadriplegic cerebral palsy, J Pediatr 129 (1996), pp. 870–876. Article | PDF (682
K) | View Record in Scopus | Cited By in Scopus (40)
68 J. Krick, P.E. Murphy, J.F. Markham and B.K. Shapiro, A proposed formula for calculating energy needs
of children with cerebral palsy, Dev Med Child Neurol 34 (1992), pp. 481–487. View Record in Scopus |
Cited By in Scopus (27)
69 K.J. Motil, Enteral nutrition in the neurologically impaired child. In: S.B. Baker, R.D. Baker and A. Davis,
Editors, Pediatric enteral nutrition, Chapman & Hall, New York (1994), pp. 217–237.
Current Problems in Pediatric and Adolescent Health Care Volume 37, Issue 10, November-December 2007, Pages 374-399