NCC Pediatrics Continuity Clinic Curriculum: Toxic Stress ... · of health, learning, and behavior...
Transcript of NCC Pediatrics Continuity Clinic Curriculum: Toxic Stress ... · of health, learning, and behavior...

NCC Pediatrics Continuity Clinic Curriculum:
Toxic Stress and Adverse Childhood
Experiences Faculty Guide
Goals & Objectives: To understand toxic stress, its adverse effects on children, and how children and their families
can overcome these negative health effects
Define toxic stress.
o How do stress responses differ?
What determines whether an adverse childhood experience (ACE) may be associated
with a toxic stress response?
What is the Adverse Childhood Experiences study?
How does toxic stress affect the developing brain?
What are the potential health consequences of toxic stress?
What is resilience?
Pre-Meeting Preparation: Please review the following enclosures: Watch the TEDTalk on ACEs by Nadine Burke-Harris, MD, MPH, FAAP:
https://youtu.be/95ovIJ3dsNk
Read AAP Technical Report “The Lifelong Effects of Early Childhood Adversity and
Toxic Stress”
Read Military Children and Families: Strengths and Challenges During Peace and War
(begin at “Strengths and Challenges Among Military Children and Families” pg. 66 and
stop at “Strengths-Based Approaches” pg. 68, or continue through for extra credit 😊)
Conference Agenda: Quiz
Cases
Extra Credit: ● ACEs study
© Developed by CPT Saira Ahmed, CPT Christin Folker, Edited by CPT W.
Aaron Adams, 2018. Updates Christin Folker, 2019.

TECHNICAL REPORT
The Lifelong Effects of Early Childhood Adversity andToxic Stress
abstractAdvances in fields of inquiry as diverse as neuroscience, molecularbiology, genomics, developmental psychology, epidemiology, sociology,and economics are catalyzing an important paradigm shift in our un-derstanding of health and disease across the lifespan. This converging,multidisciplinary science of human development has profound impli-cations for our ability to enhance the life prospects of children and tostrengthen the social and economic fabric of society. Drawing on thesemultiple streams of investigation, this report presents an ecobiodeve-lopmental framework that illustrates how early experiences and envi-ronmental influences can leave a lasting signature on the geneticpredispositions that affect emerging brain architecture and long-termhealth. The report also examines extensive evidence of the disruptiveimpacts of toxic stress, offering intriguing insights into causal mech-anisms that link early adversity to later impairments in learning, be-havior, and both physical and mental well-being. The implications ofthis framework for the practice of medicine, in general, and pediatrics,specifically, are potentially transformational. They suggest that manyadult diseases should be viewed as developmental disorders that beginearly in life and that persistent health disparities associated with pov-erty, discrimination, or maltreatment could be reduced by the allevi-ation of toxic stress in childhood. An ecobiodevelopmental frameworkalso underscores the need for new thinking about the focus and bound-aries of pediatric practice. It calls for pediatricians to serve as bothfront-line guardians of healthy child development and strategically po-sitioned, community leaders to inform new science-based strategiesthat build strong foundations for educational achievement, economicproductivity, responsible citizenship, and lifelong health. Pediatrics2012;129:e232–e246
INTRODUCTIONOf a good beginning cometh a good end.
John Heywood, Proverbs (1546)
The United States, like all nations of the world, is facing a numberof social and economic challenges that must be met to securea promising future. Central to this task is the need to produce a well-educated and healthy adult population that is sufficiently skilled toparticipate effectively in a global economy and to become responsiblestakeholders in a productive society. As concerns continue to growabout the quality of public education and its capacity to prepare thenation’s future workforce, increasing investments are being made in
Jack P. Shonkoff, MD, Andrew S. Garner, MD, PhD, and THECOMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD ANDFAMILY HEALTH, COMMITTEE ON EARLY CHILDHOOD,ADOPTION, AND DEPENDENT CARE, AND SECTION ONDEVELOPMENTAL AND BEHAVIORAL PEDIATRICS
KEY WORDSecobiodevelopmental framework, new morbidity, toxic stress,social inequalities, health disparities, health promotion, diseaseprevention, advocacy, brain development, human capitaldevelopment, pediatric basic science
ABBREVIATIONSACE—adverse childhood experiencesCRH—corticotropin-releasing hormoneEBD—ecobiodevelopmentalPFC—prefrontal cortex
This document is copyrighted and is property of the AmericanAcademy of Pediatrics and its Board of Directors. All authorshave filed conflict of interest statements with the AmericanAcademy of Pediatrics. Any conflicts have been resolved througha process approved by the Board of Directors. The AmericanAcademy of Pediatrics has neither solicited nor accepted anycommercial involvement in the development of the content ofthis publication.
The guidance in this report does not indicate an exclusivecourse of treatment or serve as a standard of medical care.Variations, taking into account individual circumstances, may beappropriate.
All technical reports from the American Academy of Pediatricsautomatically expire 5 years after publication unless reaffirmed,revised, or retired at or before that time.
www.pediatrics.org/cgi/doi/10.1542/peds.2011-2663
doi:10.1542/peds.2011-2663
PEDIATRICS (ISSN Numbers: Print, 0031-4005; Online, 1098-4275).
Copyright © 2012 by the American Academy of Pediatrics
e232 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

the preschool years to promote thefoundations of learning. Althoughdebates about early childhood policyfocus almost entirely on educationalobjectives, science indicates thatsound investments in interventionsthat reduce adversity are also likely tostrengthen the foundations of physicaland mental health, which would gen-erate even larger returns to all ofsociety.1,2 This growing scientific un-derstanding about the common rootsof health, learning, and behavior inthe early years of life presents a po-tentially transformational opportunityfor the future of pediatrics.
Identifying the origins of adult diseaseand addressing them early in life arecritical steps toward changing ourcurrent health care system from a“sick-care” to a “well-care” model.3–5
Although new discoveries in basicscience, clinical subspecialties, andhigh-technology medical interventionscontinue to advance our capacity totreat patients who are ill, there isgrowing appreciation that a success-ful well-care system must expand itsscope beyond the traditional realm ofindividualized, clinical practice to ad-dress the complex social, economic,cultural, environmental, and devel-opmental influences that lead topopulation-based health disparitiesand unsustainable medical care ex-penditures.2,6,7 The science of earlychildhood development has much tooffer in the realization of this vision,and the well-being of young childrenand their families is emerging as apromising focus for creative invest-ment.
The history of pediatrics conveys a richnarrative of empirical investigationand pragmatic problem solving. Itsemergence as a specialized domainof clinical medicine in the late 19thcentury was dominated by concernsabout nutrition, infectious disease, andpremature death. In the middle of
the 20th century, as effective vaccines,antibiotics, hygiene, and other publichealth measures confronted the in-fectious etiologies of childhood illness,a variety of developmental, behavioral,and family difficulties became knownas the “new morbidities.”8 By the endof the century, mood disorders, pa-rental substance abuse, and exposureto violence, among other conditions,began to receive increasing attentionin the pediatric clinical setting andbecame known as the “newer mor-bidities.”9 Most recently, increasinglycomplex mental health concerns; theadverse effects of television viewing;the influence of new technologies; ep-idemic increases in obesity; and per-sistent economic, racial, and ethnicdisparities in health status have beencalled the “millennial morbidities.”10
Advances in the biological, develop-mental, and social sciences now offertools to write the next importantchapter. The overlapping and syner-gistic characteristics of the mostprevalent conditions and threats tochild well-being—combined with theremarkable pace of new discoveriesin developmental neuroscience, ge-nomics, and the behavioral and socialsciences—present an opportunity toconfront a number of important ques-tions with fresh information and anew perspective. What are the bi-ological mechanisms that explain thewell-documented association betweenchildhood adversity and adult healthimpairment? As these causal mecha-nisms are better elucidated, what canthe medical field, specifically, and so-ciety, more generally, do to reduce ormitigate the effects of disruptiveearly-life influences on the origins oflifelong disease? When is the optimaltime for those interventions to beimplemented?
This technical report addresses theseimportant questions in 3 ways. First,it presents a scientifically grounded,
ecobiodevelopmental (EBD) frameworkto stimulate fresh thinking about thepromotion of health and prevention ofdisease across the lifespan. Second, itapplies this EBD framework to betterunderstand the complex relationshipsamong adverse childhood circum-stances, toxic stress, brain architec-ture, and poor physical and mentalhealth well into adulthood. Third, itproposes a new role for pediatriciansto promote the development and im-plementation of science-based strate-gies to reduce toxic stress in earlychildhood as a means of preventingor reducing many of society’s mostcomplex and enduring problems,which are frequently associated withdisparities in learning, behavior, andhealth. The magnitude of this latterchallenge cannot be overstated. A re-cent technical report from the Amer-ican Academy of Pediatrics reviewed58 years of published studies andcharacterized racial and ethnic dis-parities in children’s health to be ex-tensive, pervasive, persistent, and, insome cases, worsening.11 Moreover,the report found only 2 studies thatevaluated interventions designed toreduce disparities in children’s healthstatus and health care that also com-pared the minority group to a whitegroup, and none used a randomizedcontrolled trial design.
The causal sequences of risk thatcontribute to demographic differencesin educational achievement and physi-cal well-being threaten our country’sdemocratic ideals by undermining thenational credo of equal opportunity.Unhealthy communities with too manyfast food franchises and liquor stores,yet far too few fresh food outletsand opportunities for physical activity,contribute to an unhealthy population.Unemployment and forced mobilitydisrupt the social networks that sta-bilize communities and families and,thereby, lead to higher rates of violence
PEDIATRICS Volume 129, Number 1, January 2012 e233
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

and school dropout. The purpose ofthis technical report is to leverage newknowledge from the biological andsocial sciences to help achieve thepositive life outcomes that could beaccrued to all of society if more effec-tive strategies were developed to re-duce the exposure of young childrento significant adversity.
A NEW FRAMEWORK FORPROMOTING HEALTHYDEVELOPMENT
Advances in our understanding ofthe factors that either promote orundermine early human developmenthave set the stage for a significantparadigm shift.12 In simple terms, theprocess of development is now un-derstood as a function of “naturedancing with nurture over time,” incontrast to the longstanding but nowoutdated debate about the influenceof “nature versus nurture.”13 That isto say, beginning prenatally, continu-ing through infancy, and extendinginto childhood and beyond, develop-ment is driven by an ongoing, in-extricable interaction between biology(as defined by genetic predisposi-tions) and ecology (as defined by thesocial and physical environment)12,14,15
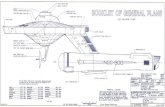
(see Fig 1).
Building on an ecological model thatexplains multiple levels of influenceon psychological development,16 and arecently proposed biodevelopmentalframework that offers an integrated,science-based approach to coordinated,early childhood policy making andpractice across sectors,17 this techni-cal report presents an EBD frameworkthat draws on a recent report fromthe Center on the Developing Child atHarvard University to help physiciansand policy makers think about howearly childhood adversity can lead tolifelong impairments in learning, be-havior, and both physical and mentalhealth.1,6
Some of the most compelling newevidence for this proposed frameworkcomes from the rapidly moving fieldof epigenetics, which investigates themolecular biological mechanisms (suchas DNA methylation and histone acet-ylation) that affect gene expressionwithout altering DNA sequence. Forexample, studies of maternal care inrats indicate that differences in thequality of nurturing affect neuralfunction in pups and negatively affectcognition and the expression of psy-chopathology later in life. Moreover,rats whose mothers showed increasedlevels of licking and grooming duringtheir first week of life also showed lessexaggerated stress responses as adultscompared with rats who were rearedby mothers with a low level of lickingand grooming, and the expression ofmother-pup interactions in the pups
has been demonstrated to be passedon to the next generation.18–22 Thisburgeoning area of research is chal-lenging us to look beyond geneticpredispositions to examine how envi-ronmental influences and early expe-riences affect when, how, and to whatdegree different genes are actuallyactivated, thereby elucidating themechanistic linkages through whichgene-environment interaction can af-fect lifelong behavior, development,and health (see Fig 1).
Additional evidence for the proposedframework comes from insights ac-crued during the “Decade of theBrain” in the 1990s, when the NationalInstitutes of Health invested signifi-cant resources into understandingboth normal and pathologic neuronaldevelopment and function. Subse-quent advances in developmentalneuroscience have begun to describefurther, in some cases at the molec-ular and cellular levels, how an in-tegrated, functioning network withbillions of neurons and trillions ofconnections is assembled. Becausethis network serves as the biologicalplatform for a child’s emerging social-emotional, linguistic, and cognitiveskills, developmental neuroscience isalso beginning to clarify the under-lying causal mechanisms that explainthe normative process of child de-velopment. In a parallel fashion, lon-gitudinal studies that document thelong-term consequences of childhoodadversity indicate that alterations ina child’s ecology can have measurableeffects on his or her developmentaltrajectory, with lifelong consequencesfor educational achievement, economicproductivity, health status, and lon-gevity.23–27
The EBD framework described in thisarticle presents a new way to thinkabout the underlying biological mech-anisms that explain this robust linkbetween early life adversities (ie, the
FIGURE 1The basic science of pediatrics. An emerging,multidisciplinary science of development sup-ports an EBD framework for understanding theevolution of human health and disease acrossthe life span. In recent decades, epidemiology,developmental psychology, and longitudinalstudies of early childhood interventions havedemonstrated significant associations (hashedred arrow) between the ecology of childhoodand a wide range of developmental outcomesand life course trajectories. Concurrently, ad-vances in the biological sciences, particularly indevelopmental neuroscience and epigenetics,have made parallel progress in beginning toelucidate the biological mechanisms (solidarrows) underlying these important associa-tions. The convergence of these diverse dis-ciplines defines a promising new basic scienceof pediatrics.
e234 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

new morbidities of childhood) and im-portant adult outcomes. The innovationof this approach lies in its mobilizationof dramatic scientific advances in theservice of rethinking basic notions ofhealth promotion and disease pre-vention within a fully integrated, lifespan perspective from conception toold age.6 In this context, significantstress in the lives of young children isviewed as a risk factor for the genesisof health-threatening behaviors as wellas a catalyst for physiologic respon-ses that can lay the groundwork forchronic, stress-related diseases laterin life.
Understanding the Biology ofStress
Although genetic variability clearlyplays a role in stress reactivity, earlyexperiences and environmental influ-ences can have considerable impact.Beginning as early as the prenatal pe-riod, both animal28–30 and human31,32
studies suggest that fetal exposure tomaternal stress can influence laterstress responsiveness. In animals, thiseffect has been demonstrated notonly in the offspring of the studiedpregnancy but also in subsequentgenerations. The precise biologicalmechanisms that explain these find-ings remain to be elucidated, butepigenetic modifications of DNA ap-pear likely to play a role.31,33,34 Earlypostnatal experiences with adversityare also thought to affect future re-activity to stress, perhaps by alteringthe developing neural circuits con-trolling these neuroendocrine respon-ses.34,35 Although much researchremains to be performed in this area,there is a strong scientific consensusthat the ecological context modulatesthe expression of one’s genotype. Itis as if experiences confer a “sig-nature” on the genome to authorizecertain characteristics and behaviorsand to prohibit others. This concept
underscores the need for greater un-derstanding of how stress “gets underthe skin,” as well as the importanceof determining what external and in-ternal factors can be mobilized toprevent that embedding process orprotect against the consequences ofits activation.
Physiologic responses to stress arewell defined.36–38 The most exten-sively studied involve activation of thehypothalamic-pituitary-adrenocorticalaxis and the sympathetic-adrenomedullarysystem, which results in increasedlevels of stress hormones, such ascorticotropin-releasing hormone (CRH),cortisol, norepinephrine, and adrena-line. These changes co-occur witha network of other mediators thatinclude elevated inflammatory cyto-kines and the response of the para-sympathetic nervous system, whichcounterbalances both sympatheticactivation and inflammatory respon-ses. Whereas transient increases inthese stress hormones are protectiveand even essential for survival, ex-cessively high levels or prolongedexposures can be quite harmful orfrankly toxic,39–41 and the dysregulationof this network of physiologicmediators (eg, too much or too littlecortisol; too much or too little in-flammatory response) can lead toa chronic “wear and tear” effecton multiple organ systems, includingthe brain.39–41 This cumulative, stress-induced burden on overall body func-tioning and the aggregated costs, bothphysiologic and psychological, re-quired for coping and returning tohomeostatic balance, have been re-ferred to as “allostatic load.”38,42–44
The dynamics of these stress-mediatingsystems are such that their over-activation in the context of repeated orchronic adversity leads to alterationsin their regulation.
The National Scientific Council onthe Developing Child has proposed
a conceptual taxonomy comprising 3distinct types of stress responses (incontrast to the actual stressors them-selves) in young children—positive,tolerable, and toxic—on the basis ofpostulated differences in their po-tential to cause enduring physiologicdisruptions as a result of the intensityand duration of the response.17,45 Apositive stress response refers toa physiologic state that is brief andmild to moderate in magnitude. Cen-tral to the notion of positive stress isthe availability of a caring and re-sponsive adult who helps the childcope with the stressor, thereby pro-viding a protective effect that facili-tates the return of the stress responsesystems back to baseline status. Ex-amples of precipitants of a positivestress response in young children in-clude dealing with frustration, gettingan immunization, and the anxiety as-sociated with the first day at a childcare center. When buffered by an en-vironment of stable and supportiverelationships, positive stress respon-ses are a growth-promoting elementof normal development. As such, theyprovide important opportunities toobserve, learn, and practice healthy,adaptive responses to adverse expe-riences.
A tolerable stress response, in con-trast to positive stress, is associatedwith exposure to nonnormative expe-riences that present a greater magni-tude of adversity or threat. Precipitantsmay include the death of a familymember, a serious illness or injury,a contentious divorce, a natural di-saster, or an act of terrorism. Whenexperienced in the context of buffer-ing protection provided by suppor-tive adults, the risk that suchcircumstances will produce excessiveactivation of the stress responsesystems that leads to physiologicharm and long-term consequencesfor health and learning is greatly
PEDIATRICS Volume 129, Number 1, January 2012 e235
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

reduced. Thus, the essential char-acteristic that makes this form ofstress response tolerable is theextent to which protective adultrelationships facilitate the child’s adap-tive coping and a sense of control,thereby reducing the physiologic stressresponse and promoting a return tobaseline status.
The third and most dangerous form ofstress response, toxic stress, can re-sult from strong, frequent, or pro-longed activation of the body’s stressresponse systems in the absence ofthe buffering protection of a supportive,adult relationship. The risk factorsstudied in the Adverse ChildhoodExperiences Study23 include examplesof multiple stressors (eg, child abuseor neglect, parental substance abuse,and maternal depression) that arecapable of inducing a toxic stress re-sponse. The essential characteristic ofthis phenomenon is the postulateddisruption of brain circuitry and otherorgan and metabolic systems dur-ing sensitive developmental periods.Such disruption may result in ana-tomic changes and/or physiologicdysregulations that are the precursorsof later impairments in learning andbehavior as well as the roots of chronic,stress-related physical and mental ill-ness. The potential role of toxic stressand early life adversity in the patho-genesis of health disparities under-scores the importance of effectivesurveillance for significant risk factorsin the primary health care setting. Moreimportant, however, is the need forclinical pediatrics to move beyond thelevel of risk factor identification and toleverage advances in the biology of ad-versity to contribute to the critical taskof developing, testing, and refining newand more effective strategies for re-ducing toxic stress and mitigating itseffects as early as possible, beforeirrevocable damage is done. Statedsimply, the next chapter of innovation
in pediatrics remains to be written,but the outline and plot are clear.
Toxic Stress and the DevelopingBrain
In addition to short-term changes inobservable behavior, toxic stress inyoung children can lead to less out-wardly visible yet permanent changesin brain structure and function.39,46
The plasticity of the fetal, infant, andearly childhood brain makes it par-ticularly sensitive to chemical influ-ences, and there is growing evidencefrom both animal and human studiesthat persistently elevated levels ofstress hormones can disrupt its de-veloping architecture.45 For example,abundant glucocorticoid receptors arefound in the amygdala, hippocampus,and prefrontal cortex (PFC), and ex-posure to stressful experiences hasbeen shown to alter the size andneuronal architecture of these areasas well as lead to functional differ-ences in learning, memory, and as-pects of executive functioning. Morespecifically, chronic stress is associ-ated with hypertrophy and overactivityin the amygdala and orbitofrontalcortex, whereas comparable levels ofadversity can lead to loss of neuronsand neural connections in the hippo-campus and medial PFC. The functionalconsequences of these structuralchanges include more anxiety relatedto both hyperactivation of the amyg-dala and less top-down control as aresult of PFC atrophy as well as im-paired memory and mood control asa consequence of hippocampal re-duction.47 Thus, the developing archi-tecture of the brain can be impairedin numerous ways that create a weakfoundation for later learning, behav-ior, and health.
Along with its role in mediating fearand anxiety, the amygdala is also anactivator of the physiologic stressresponse. Its stimulation activates
sympathetic activity and causes neu-rons in the hypothalamus to releaseCRH. CRH, in turn, signals the pituitaryto release adrenocorticotropic hor-mone, which then stimulates theadrenal glands to increase serumcortisol concentrations. The amygdalacontains large numbers of both CRHand glucocorticoid receptors, begin-ning early in life, which facilitate theestablishment of a positive feedbackloop. Significant stress in early child-hood can trigger amygdala hypertro-phy and result in a hyperresponsiveor chronically activated physiologicstress response, along with increasedpotential for fear and anxiety.48,49 It isin this way that a child’s environmentand early experiences get under theskin.
Although the hippocampus can turnoff elevated cortisol, chronic stressdiminishes its capacity to do so andcan lead to impairments in memoryand mood-related functions that arelocated in this brain region. Exposureto chronic stress and high levels ofcortisol also inhibit neurogenesis inthe hippocampus, which is believed toplay an important role in the encodingof memory and other functions. Fur-thermore, toxic stress limits the abilityof the hippocampus to promote con-textual learning, making it more dif-ficult to discriminate conditions forwhich there may be danger versussafety, as is common in posttraumaticstress disorder. Hence, altered brainarchitecture in response to toxic stressin early childhood could explain, atleast in part, the strong associationbetween early adverse experiencesand subsequent problems in the de-velopment of linguistic, cognitive, andsocial-emotional skills, all of which areinextricably intertwined in the wiringof the developing brain.45
The PFC also participates in turningoff the cortisol response and hasan important role in the top-down
e236 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

regulation of autonomic balance (ie,sympathetic versus parasympatheticeffects), as well as in the develop-ment of executive functions, such asdecision-making, working memory,behavioral self-regulation, and moodand impulse control. The PFC is alsoknown to suppress amygdala activity,allowing for more adaptive responsesto potentially threatening or stress-ful experiences; however, exposure tostress and elevated cortisol results indramatic changes in the connectivitywithin the PFC, which may limit itsability to inhibit amygdala activity and,thereby, impair adaptive responses tostress. Because the hippocampus andPFC both play a significant role inmodulating the amygdala’s initiationof the stress response, toxic stress–induced changes in architecture andconnectivity within and between theseimportant areas might accountfor the variability seen in stress-responsiveness.50 This can then resultin some children appearing to be bothmore reactive to even mildly adverseexperiences and less capable of effec-tively coping with future stress.36,37,45,51
Toxic Stress and the EarlyChildhood Roots of LifelongImpairments in Physical andMental Health
As described in the previous section,stress-induced changes in the archi-tecture of different regions of thedeveloping brain (eg, amygdala, hip-pocampus, and PFC) can have poten-tially permanent effects on a range ofimportant functions, such as regulat-ing stress physiology, learning newskills, and developing the capacityto make healthy adaptations to futureadversity.52,53 As the scientific evi-dence for these associations has be-come better known and has beendisseminated more widely, its impli-cations for early childhood policy andprograms have become increasingly
appreciated by decision makersacross the political spectrum. Not-withstanding this growing awareness,however, discussions about earlybrain development in policy-makingcircles have focused almost entirelyon issues concerned with schoolreadiness as a prerequisite for lateracademic achievement and the de-velopment of a skilled adult work-force. Within this same context, thehealth dimension of early childhoodpolicy has focused largely on the tra-ditional components of primary pedi-atric care, such as immunizations,early identification of sensory im-pairments and developmental delays,and the prompt diagnosis and treat-ment of medical problems. That said,as advances in the biomedical scienceshave generated growing evidencelinking biological disruptions associ-ated with adverse childhood experi-ences (ACE) to greater risk for a varietyof chronic diseases well into the adultyears, the need to reconceptualizethe health dimension of early child-hood policy has become increasinglyclear.1,6 Stated simply, the time hascome to expand the public’s un-derstanding of brain developmentand shine a bright light on its re-lation to the early childhood rootsof adult disease and to examine thecompelling implications of this grow-ing knowledge base for the future ofpediatric practice.
The potential consequences of toxicstress in early childhood for thepathogenesis of adult disease areconsiderable. At the behavioral level,there is extensive evidence of a stronglink between early adversity and awide range of health-threatening be-haviors. At the biological level, there isgrowing documentation of the extentto which both the cumulative burdenof stress over time (eg, from chronicmaltreatment) and the timing ofspecific environmental insults during
sensitive developmental periods (eg,from first trimester rubella or pre-natal alcohol exposure) can createstructural and functional disruptionsthat lead to a wide range of physicaland mental illnesses later in adult life.1,6
A selective overview of this extensivescientific literature is provided below.
The association between ACE and un-healthy adult lifestyles has been welldocumented. Adolescents with a his-tory of multiple risk factors are morelikely to initiate drinking alcohol ata younger age and are more likely touse alcohol as a means of coping withstress than for social reasons.54 Theadoption of unhealthy lifestyles as acoping mechanism might also explainwhy higher ACE exposures are asso-ciated with tobacco use, illicit drugabuse, obesity, and promiscuity,55,56 aswell as why the risk of pathologicgambling is increased in adults whowere maltreated as children.57 Ado-lescents and adults who manifesthigher rates of risk-taking behaviorsare also more likely to have troublemaintaining supportive social net-works and are at higher risk of schoolfailure, gang membership, unemploy-ment, poverty, homelessness, violentcrime, incarceration, and becomingsingle parents. Furthermore, adultsin this high-risk group who becomeparents themselves are less likely tobe able to provide the kind of stableand supportive relationships that areneeded to protect their children fromthe damages of toxic stress. This in-tergenerational cycle of significantadversity, with its predictable repeti-tion of limited educational achieve-ment and poor health, is mediated, atleast in part, by the social inequalitiesand disrupted social networks thatcontribute to fragile families andparenting difficulties.7,58,59
The adoption of unhealthy lifestylesand associated exacerbation of so-cioeconomic inequalities are potent
PEDIATRICS Volume 129, Number 1, January 2012 e237
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

risk factors for poor health. Up to 40%of early deaths have been estimatedto be the result of behavioral or life-style patterns,3 and 1 interpretation ofthe ACE study data is that toxic stressin childhood is associated with theadoption of unhealthy lifestyles as acoping mechanism.60 An additional 25%to 30% of early deaths are thought tobe attributable to either inadequaciesin medical care3 or socioeconomic cir-cumstances, many of which are knownto contribute to health care–relateddisparities.61–67
Beyond its strong association withlater risk-taking and generally un-healthy lifestyles, it is critically im-portant to underscore the extent towhich toxic stress in early childhoodhas also been shown to cause physi-ologic disruptions that persist intoadulthood and lead to frank disease,even in the absence of later health-threatening behaviors. For example,the biological manifestations of toxicstress can include alterations in im-mune function68 and measurable in-creases in inflammatory markers,69–72
which are known to be associatedwith poor health outcomes as diverseas cardiovascular disease,69,70,73 viralhepatitis,74 liver cancer,75 asthma,76
chronic obstructive pulmonary dis-ease,77 autoimmune diseases,78 poordental health,72 and depression.79–81
Thus, toxic stress in early childhoodnot only is a risk factor for later riskybehavior but also can be a directsource of biological injury or disrup-tion that may have lifelong conse-quences independent of whatevercircumstances might follow later inlife. In such cases, toxic stress can beviewed as the precipitant of a physio-logic memory or biological signaturethat confers lifelong risk well beyondits time of origin.38,42–44
Over and above its toll on individuals,it is also important to address theenormous social and economic costs
of toxic stress and its consequencesfor all of society. The multiple dimen-sions of these costs extend from dif-ferential levels of civic participationand their impacts on the quality ofcommunity life to the health and skillsof the nation’s workforce and itsability to participate successfully ina global economy. In the realm oflearning and behavior, economistsargue for early and sustained invest-ments in early care and educationprograms, particularly for childrenwhose parents have limited educationand low income, on the basis of per-suasive evidence from cost-benefitanalyses that reveal the costs of in-carceration and diminished economicproductivity associated with educa-tional failure.82–86 In view of the rela-tively scarce attention to healthoutcomes in these long-term follow-upstudies, the full return on investmentsthat reduce toxic stress in earlychildhood is likely to be much higher.Health care expenditures that arepaying for the consequences of un-healthy lifestyles (eg, obesity, tobacco,alcohol, and substance abuse) areenormous, and the costs of chronicdiseases that may have their originsearly in life include many conditionsthat consume a substantial percent-age of current state and federalbudgets. The potential savings inhealth care costs from even small,marginal reductions in the prevalenceof cardiovascular disease, hyperten-sion, diabetes, and depression are,therefore, likely to dwarf the consid-erable economic productivity andcriminal justice benefits that havebeen well documented for effectiveearly childhood interventions.
In summary, the EBD approach tochildhood adversity discussed in thisreport has 2 compelling implicationsfor a full, life span perspective onhealth promotion and disease pre-vention. First, it postulates that toxic
stress in early childhood plays animportant causal role in the inter-generational transmission of dispa-rities in educational achievement andhealth outcomes. Second, it under-scores the need for the entire medicalcommunity to focus more attention onthe roots of adult diseases that orig-inate during the prenatal and earlychildhood periods and to rethinkthe concept of preventive health carewithin a system that currently perpetu-ates a scientifically untenable wall be-tween pediatrics and internal medicine.
THE NEED FOR A NEW PEDIATRICPARADIGM TO PROMOTE HEALTHAND PREVENT DISEASE
In his 1966 Aldrich Award address,Dr Julius Richmond identified childdevelopment as the basic science ofpediatrics.87 It is now time to expandthe boundaries of that science by in-corporating more than 4 decades oftransformational research in neurosci-ence, molecular biology, and genomics,along with parallel advances in the be-havioral and social sciences (see Fig 1).This newly augmented, interdisciplinary,basic science of pediatrics offers apromising framework for a deeperunderstanding of the biology andecology of the developmental process.More importantly, it presents a com-pelling opportunity to leverage theserapidly advancing frontiers of knowl-edge to formulate more effective strat-egies to enhance lifelong outcomes inlearning, behavior, and health.
The time has come for a coordinatedeffort among basic scientists, pediat-ric subspecialists, and primary careclinicians to develop more effectivestrategies for addressing the origins ofsocial class, racial, and ethnic dis-parities in health and development.To this end, a unified, science-basedapproach to early childhood policyand practice across multiple sectors(including primary health care, early
e238 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

care and education, and child welfare,among many others) could providea compelling framework for a new erain community-based investment inwhich coordinated efforts are drivenby a shared knowledge base ratherthan distracted by a diversity of tradi-tions, approaches, and funding streams.
Recognizing both the critical value andclear limitations of what can be ac-complished within the constraints ofan office visit, 21st century pediatricsis well positioned to serve as the pri-mary engine for a broader approachto health promotion and disease pre-vention that is guided by cutting-edgescience and expanded in scope be-yond individualized health care.88,89
The pediatric medical home of thefuture could offer more than the earlyidentification of concerns and timelyreferral to available programs, asenhanced collaboration between pedia-tricians and community-based agen-cies could be viewed as a vehiclefor testing promising new interven-tion strategies rather than simply
improving coordination among exist-ing services. With this goal in mind,science tells us that interventions thatstrengthen the capacities of familiesand communities to protect youngchildren from the disruptive effectsof toxic stress are likely to promotehealthier brain development and en-hanced physical and mental well-being. The EBD approach proposed inthis article is adapted from a science-based framework created by theCenter on the Developing Child atHarvard University to advance earlychildhood policies and programs thatsupport this vision (see Fig 2).1 Itsrationale, essential elements, and im-plications for pediatric practice aresummarized below.
Broadening the Framework forEarly Childhood Policy andPractice
Advances across the biological, be-havioral, and social sciences support2 clear and powerful messages forleaders who are searching for more
effective ways to improve the health ofthe nation.6 First, current health pro-motion and disease prevention poli-cies focused largely on adults wouldbe more effective if evidence-basedinvestments were also made tostrengthen the foundations of healthin the prenatal and early childhoodperiods. Second, significant reductionsin chronic disease could be achievedacross the life course by decreasingthe number and severity of adverseexperiences that threaten the well-being of young children and bystrengthening the protective relation-ships that help mitigate the harmfuleffects of toxic stress. The multipledomains that affect the biology ofhealth and development—includingthe foundations of healthy devel-opment, caregiver and communitycapacities, and public and private sec-tor policies and programs—providea rich array of targeted opportunitiesfor the introduction of innovativeinterventions, beginning in the earli-est years of life.1
FIGURE 2An ecobiodevelopmental framework for early childhood policies and programs. This was adapted from ref 1. See text for details.
PEDIATRICS Volume 129, Number 1, January 2012 e239
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

The biology of health and develop-ment explains how experiences andenvironmental influences get underthe skin and interact with geneticpredispositions, which then result invarious combinations of physiologicadaptation and disruption that affectlifelong outcomes in learning, behavior,and both physical and mental well-being. These findings call for us toaugment adult-focused approaches tohealth promotion and disease preven-tion by addressing the early childhoodorigins of lifelong illness and disability.
The foundations of healthy devel-opment refers to 3 domains that es-tablish a context within which theearly roots of physical and mentalwell-being are nourished. These in-clude (1) a stable and responsiveenvironment of relationships, whichprovides young children with consis-tent, nurturing, and protective inter-actions with adults to enhance theirlearning and help them developadaptive capacities that promote well-regulated stress-response systems;(2) safe and supportive physical,chemical, and built environments,which provide physical and emotionalspaces that are free from toxins andfear, allow active exploration withoutsignificant risk of harm, and offersupport for families raising youngchildren; and (3) sound and appropri-ate nutrition, which includes health-promoting food intake and eatinghabits, beginning with the future moth-er’s preconception nutritional status.
Caregiver and community capaci-ties to promote health and preventdisease and disability refers to theability of family members, early child-hood program staff, and the social cap-ital provided through neighborhoods,voluntary associations, and the parents’workplaces to play a major supportiverole in strengthening the foundationsof child health. These capacities canbe grouped into 3 categories: (1) time
and commitment; (2) financial, psycho-logical, social, and institutional resour-ces; and (3) skills and knowledge.
Public and private sector policiesand programs can strengthen thefoundations of health through theirability to enhance the capacities ofcaregivers and communities in themultiple settings in which childrengrow up. Relevant policies includeboth legislative and administrativeactions that affect systems respon-sible for primary health care, publichealth, child care and early education,child welfare, early intervention, familyeconomic stability (including employ-ment support for parents and cashassistance), community development(including zoning regulations that in-fluence the availability of open spacesand sources of nutritious food), hous-ing, and environmental protection,among others. It is also important tounderscore the role that the privatesector can play in strengthening thecapacities of families to raise healthyand competent children, particularlythrough supportive workplace policies(such as paid parental leave, supportfor breastfeeding, and flexible workhours to attend school activities andmedical visits).
Defining a Distinctive Niche forPediatrics Among Multiple EarlyChildhood Disciplinesand Services
Notwithstanding the important goalof ensuring a medical home for allchildren, extensive evidence on thesocial determinants of health indicatesthat the reduction of disparities inphysical and mental well-being willdepend on more than access to high-quality medical care alone. Moreover,as noted previously, experience tellsus that continuing calls for enhancedcoordination of effort across servicesystems are unlikely to be sufficient ifthe systems are guided by different
values and bodies of knowledge andthe effects of their services are mod-est. With these caveats in mind,pediatricians are strategically situatedto mobilize the science of early child-hood development and its underly-ing neurobiology to stimulate freshthinking about both the scope of pri-mary health care and its relation toother programs serving young chil-dren and their families. Indeed, everysystem that touches the lives of chil-dren—as well as mothers before andduring pregnancy—offers an oppor-tunity to leverage this rapidly growingknowledge base to strengthen thefoundations and capacities that makelifelong healthy development possible.Toward this end, explicit investmentsin the early reduction of significantadversity are particularly likely togenerate positive returns.
The possibilities and limitations ofwell-child care within a multidimen-sional health system have been thefocus of a spirited and enduring dis-cussion within the pediatric com-munity.88,90,91 Over more than halfa century, this dialogue has focusedon the need for family-centered,community-based, culturally compe-tent care for children with develop-mental disabilities, behavior problems,and chronic health impairments, aswell as the need for a broader con-textual approach to the challenges ofproviding more effective interventionsfor children living under conditions ofpoverty, with or without the additionalcomplications of parental mental ill-ness, substance abuse, and exposureto violence.10 As the debate has con-tinued, the gap between the call forcomprehensive services and the re-alities of day-to-day practice has re-mained exceedingly difficult to reduce.Basic recommendations for routinedevelopmental screening and refer-rals to appropriate community-basedservices have been particularly difficult
e240 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

to implement.92 The obstacles to prog-ress in this area have been formidableat both ends of the process—beginningwith the logistical and financial chal-lenges of conducting routine develop-mental screening in a busy officesetting and extending to significantlimitations in access to evidence-based services for children andfamilies who are identified as havingproblems that require intervention.
Despite long-standing calls for an ex-plicit, community-focused approach toprimary care, a recent national studyof pediatric practices identified per-sistent difficulties in achieving effec-tive linkages with community-basedresources as a major challenge.92 Aparallel survey of parents also notedthe limited communication that ex-ists between pediatric practices andcommunity-based services, such asSupplemental Nutrition Program forWomen, Infants, and Children; childcare providers; and schools.93 Per-haps most important, both groupsagreed that pediatricians cannot beexpected to meet all of a child’s needs.This challenge is further complicatedby the marked variability in qualityamong community-based services thatare available—ranging from evidence-based interventions that clearly im-prove child outcomes to programs thatappear to have only marginal effectsor no measurable impacts. Thus, al-though chronic difficulty in securingaccess to indicated services is animportant problem facing most prac-ticing pediatricians, the limited evi-dence of effectiveness for many of theoptions that are available (particu-larly in rural areas and many statesin which public investment in suchservices is more limited) presents aserious problem that must be acknowl-edged and afforded greater attention.
At this point in time, the design andsuccessful implementation of moreeffective models of health promotion
and disease prevention for childrenexperiencing significant adversity willrequire more than advocacy for in-creased funding. It will require a deepinvestment in the development, test-ing, continuous improvement, andbroad replication of innovative modelsof cross-disciplinary policy and pro-grammatic interventions that are guidedby scientific knowledge and led bypractitioners in the medical, educa-tional, and social services worlds whoare truly ready to work together (andto train the next generation of prac-titioners) in new ways.88,89 The sheernumber and complexity of under-addressed threats to child health thatare associated with toxic stressdemands bold, creative leadershipand the selection of strategic priori-ties for focused attention. To this end,science suggests that 2 areas areparticularly ripe for fresh thinking:the child welfare system and thetreatment of maternal depression.
For more than a century, child welfareservices have focused on physicalsafety, reduction of repeated injury,and child custody. Within this context,the role of the pediatrician is focusedlargely on the identification of sus-pected maltreatment and the docu-mentation and treatment of physicalinjuries. Advances in our understand-ing of the impact of toxic stress onlifelong health now underscore theneed for a broader pediatric approachto meet the needs of children who havebeen abused or neglected. In somecases, this could be provided withina medical home by skilled clinicianswith expertise in early childhoodmental health. In reality, however, themagnitude of needs in this area gen-erally exceeds the capacity of mostprimary care practice settings. A re-port from the Institute of Medicine andNational Research Council15 statedthat these needs could be addressedthrough regularized referrals from
the child welfare system to the earlyintervention system for children withdevelopmental delays or disabilities;subsequent federal reauthorizationsof the Keeping Children and FamiliesSafe Act and the Individuals with Dis-abilities Education Act (Part C) bothincluded requirements for establish-ing such linkages. The implementationof these federal requirements, how-ever, has moved slowly.
The growing availability of evidence-based interventions that have beenshown to improve outcomes for chil-dren in the child welfare system94
underscores the compelling need totransform “child protection” from itstraditional concern with physicalsafety and custody to a broader focuson the emotional, social, and cognitivecosts of maltreatment. The Centers forDisease Control and Prevention hastaken an important step forward bypromoting the prevention of childmaltreatment as a public health con-cern.95,96 The pediatric communitycould play a powerful role in leadingthe call for implementation of thenew requirement for linking childwelfare to early intervention programs,as well as bringing a strong, science-based perspective to the collaborativedevelopment and implementation ofmore effective intervention models.
The widespread absence of attentionto the mother-child relationship inthe treatment of depression in womenwith young children is another strikingexample of the gap between scienceand practice that could be reduced bytargeted pediatric advocacy.97 Exten-sive research has demonstrated theextent to which maternal depressioncompromises the contingent reciproc-ity between a mother and her youngchild that is essential for healthy cog-nitive, linguistic, social, and emotionaldevelopment.98 Despite that well-documented observation, the treat-ment of depression in women with
PEDIATRICS Volume 129, Number 1, January 2012 e241
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

young children is typically viewed asan adult mental health service andrarely includes an explicit focus onthe mother-child relationship. This se-rious omission illustrates a lack ofunderstanding of the consequencesfor the developing brain of a youngchild when the required “serve andreturn” reciprocity of the mother-childrelationship is disrupted or incon-sistent. Consequently, and not sur-prisingly, abundant clinical researchindicates that the successful treat-ment of a mother’s depression doesnot generally translate into compara-ble recovery in her young child unlessthere is an explicit therapeutic focuson their dyadic relationship.98 Pedia-tricians are the natural authorities toshed light on this current deficiency inmental health service delivery. Advo-cating for payment mechanisms thatrequire (or provide incentives for) thecoordination of child and parent med-ical services (eg, through automaticcoverage for the parent-child dyadlinked to reimbursement for the treat-ment of maternal depression) offers 1promising strategy that AmericanAcademy of Pediatrics state chapterscould pursue. As noted previously,although some medical homes mayhave the expertise to provide thiskind of integrative treatment, mostpediatricians rely on the availabilityof other professionals with special-ized skills who are often difficult tofind. Whether such services are pro-vided within or connected to themedical home, it is clear that stan-dard pediatric practice must movebeyond screening for maternal de-pression and invest greater energy insecuring the provision of appropriateand effective treatment that meetsthe needs of both mothers and theiryoung children.
The targeted messages conveyed inthese 2 examples are illustrative ofthe kinds of specific actions that offer
promising new directions for the pe-diatric community beyond general callsfor comprehensive, family-centered,community-based services. Althoughthe practical constraints of office-basedpractice make it unlikely that manyprimary care clinicians will ever playa lead role in the treatment of childrenaffected by maltreatment or maternaldepression, pediatricians are still thebest positioned among all the pro-fessionals who care for young childrento provide the public voice and scientificleadership needed to catalyze the de-velopment and implementation of moreeffective strategies to reduce adver-sities that can lead to lifelong disparitiesin learning, behavior, and health.
A great deal has been said about howthe universality of pediatric primarycare makes it an ideal platform forcoordinating the services needed byvulnerable, young children and theirfamilies. In this respect, the medicalhome is strategically positioned toplay 2 important roles. The first is toensure that needs are identified, state-of-the-art management is provided asindicated, and credible evaluation isconducted to assess the effects of theservices that are being delivered. Thesecond and, ultimately, more trans-formational role is to mobilize the en-tire pediatric community (includingboth clinical specialists and basicscientists) to drive the design andtesting of much-needed, new, science-based interventions to reduce thesources and consequences of signifi-cant adversity in the lives of youngchildren.99 To this end, a powerful newrole awaits a new breed of pedia-tricians who are prepared to build onthe best of existing community-basedservices and to work closely withcreative leaders from a range of dis-ciplines and sectors to inform inno-vative approaches to health promotionand disease prevention that generategreater effects than existing efforts.
No other profession brings a compara-ble level of scientific expertise, profes-sional stature, and public trust—andnothing short of transformationalthinking beyond the hospital and of-fice settings is likely to create themagnitude of breakthroughs in healthpromotion that are needed to matchthe dramatic advances that are cur-rently emerging in the treatment ofdisease. This new direction must bepart of the new frontier in pediatrics—a frontier that brings cutting-edgescientific thinking to the multidimen-sional world of early childhood policyand practice for children who facesignificant adversity. Moving that fron-tier forward will benefit considerablyfrom pediatric leadership that pro-vides an intellectual and operationalbridge connecting the basic sciencesof neurobiology, molecular genetics,and developmental psychology to thebroad and diverse landscape of health,education, and human services.
SUMMARY
A vital and productive society with aprosperous and sustainable future isbuilt on a foundation of healthy childdevelopment. Health in the earliestyears—beginning with the futuremother’s well-being before she be-comes pregnant—lays the ground-work for a lifetime of the physical andmental vitality that is necessary fora strong workforce and responsibleparticipation in community life. Whendeveloping biological systems arestrengthened by positive early expe-riences, children are more likely tothrive and grow up to be healthy,contributing adults. Sound health inearly childhood provides a foundationfor the construction of sturdy brainarchitecture and the achievement ofa broad range of skills and learningcapacities. Together these constitutethe building blocks for a vital andsustainable society that invests in its
e242 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

human capital and values the lives ofits children.
Advances in neuroscience, molecularbiology, and genomics have convergedon 3 compelling conclusions: (1) earlyexperiences are built into our bodies;(2) significant adversity can producephysiologic disruptions or biologicalmemories that undermine the devel-opment of the body’s stress responsesystems and affect the developingbrain, cardiovascular system, immunesystem, and metabolic regulatory con-trols; and (3) these physiologic dis-ruptions can persist far into adulthoodand lead to lifelong impairments inboth physical and mental health. Thistechnical report presents a frame-work for integrating recent advancesin our understanding of human de-velopment with a rich and growingbody of evidence regarding the dis-ruptive effects of childhood adversityand toxic stress. The EBD frameworkthat guides this report suggests thatmany adult diseases are, in fact, de-velopmental disorders that begin earlyin life. This framework indicates thatthe future of pediatrics lies in itsunique leadership position as a credi-ble and respected voice on behalf ofchildren, which provides a powerfulplatform for translating scientific ad-vances into more effective strategiesand creative interventions to reducethe early childhood adversities thatlead to lifelong impairments in learn-ing, behavior, and health.
CONCLUSIONS
1. Advances in a broad range ofinterdisciplinary fields, includingdevelopmental neuroscience, molec-ular biology, genomics, epigenetics,developmental psychology, epidemi-ology, and economics, are converg-ing on an integrated, basic scienceof pediatrics (see Fig 1).
2. Rooted in a deepening understand-ing of how brain architecture is
shaped by the interactive effectsof both genetic predisposition andenvironmental influence, and howits developing circuitry affects alifetime of learning, behavior, andhealth, advances in the biologicalsciences underscore the founda-tional importance of the earlyyears and support an EBD frame-work for understanding the evolu-tion of human health and diseaseacross the life span.
3. The biology of early childhood ad-versity reveals the important roleof toxic stress in disrupting devel-oping brain architecture and ad-versely affecting the concurrentdevelopment of other organ sys-tems and regulatory functions.
4. Toxic stress can lead to potentiallypermanent changes in learning(linguistic, cognitive, and social-emotional skills), behavior (adap-tive versus maladaptive responsesto future adversity), and physiology(a hyperresponsive or chronicallyactivated stress response) and cancause physiologic disruptions thatresult in higher levels of stress-related chronic diseases and in-crease the prevalence of unhealthylifestyles that lead to wideninghealth disparities.
5. The lifelong costs of childhoodtoxic stress are enormous, as man-ifested in adverse impacts on learn-ing, behavior, and health, andeffective early childhood interven-tions provide critical opportunitiesto prevent these undesirable out-comes and generate large eco-nomic returns for all of society.
6. The consequences of significant ad-versity early in life prompt an ur-gent call for innovative strategiesto reduce toxic stress within thecontext of a coordinated system ofpolicies and services guided by anintegrated science of early child-hood and early brain development.
7. An EBD framework, grounded in anintegrated basic science, providesa clear theory of change to helpleaders in policy and practice craftnew solutions to the challenges ofsocietal disparities in health, learn-ing, and behavior (see Fig 2).
8. Pediatrics provides a powerful yetunderused platform for translatingscientific advances into innovativeearly childhood policies, and prac-ticing pediatricians are ideally po-sitioned to participate “on theground” in the design, testing,and refinement of new models ofdisease prevention, health promo-tion, and developmental enhance-ment beginning in the earliestyears of life.
LEAD AUTHORSJack P. Shonkoff, MDAndrew S. Garner, MD, PhD
COMMITTEE ON PSYCHOSOCIALASPECTS OF CHILD AND FAMILYHEALTH, 2010–2011Benjamin S. Siegel, MD, ChairpersonMary I. Dobbins, MDMarian F. Earls, MDAndrew S. Garner, MD, PhDLaura McGuinn, MDJohn Pascoe, MD, MPHDavid L. Wood, MD
LIAISONSRobert T. Brown, PhD – Society of PediatricPsychologyTerry Carmichael, MSW – National Associationof Social WorkersMary Jo Kupst, PhD – Society of PediatricPsychologyD. Richard Martini, MD – American Academy ofChild and Adolescent PsychiatryMary Sheppard, MS, RN, PNP, BC – NationalAssociation of Pediatric Nurse Practitioners
CONSULTANTGeorge J. Cohen, MD
CONSULTANT AND LEAD AUTHORJack P. Shonkoff, MD
STAFFKaren S. Smith
PEDIATRICS Volume 129, Number 1, January 2012 e243
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

COMMITTEE ON EARLY CHILDHOOD,ADOPTION, AND DEPENDENT CARE,2010–2011Pamela C. High, MD, ChairpersonElaine Donoghue, MDJill J. Fussell, MDMary Margaret Gleason, MDPaula K. Jaudes, MDVeronnie F. Jones, MDDavid M. Rubin, MDElaine E. Schulte, MD, MPH
STAFFMary Crane, PhD, LSW
SECTION ON DEVELOPMENTAL ANDBEHAVIORAL PEDIATRICS EXECUTIVECOMMITTEE, 2010–2011Michelle M. Macias, MD, Chairperson
Carolyn Bridgemohan, MDJill Fussell, MDEdward Goldson, MDLaura J. McGuinn, MDCarol Weitzman, MDLynn Mowbray Wegner, MD, Immediate PastChairperson
STAFFLinda B. Paul, MPH
REFERENCES
1. Center on the Developing Child at HarvardUniversity. The foundations of lifelonghealth are built in early childhood. Avail-able at: www.developingchild.harvard.edu.Accessed March 8, 2011
2. Knudsen EI, Heckman JJ, Cameron JL,Shonkoff JP. Economic, neurobiological,and behavioral perspectives on buildingAmerica’s future workforce. Proc Natl AcadSci U S A. 2006;103(27):10155–10162
3. McGinnis JM, Williams-Russo P, KnickmanJR. The case for more active policy atten-tion to health promotion. Health Aff (Mill-wood). 2002;21(2):78–93
4. Schor EL, Abrams M, Shea K. Medicaid:health promotion and disease preventionfor school readiness. Health Aff (Millwood).2007;26(2):420–429
5. Wen CP, Tsai SP, Chung WS. A 10-year ex-perience with universal health insurancein Taiwan: measuring changes in healthand health disparity. Ann Intern Med. 2008;148(4):258–267
6. Shonkoff JP, Boyce WT, McEwen BS. Neuro-science, molecular biology, and the child-hood roots of health disparities: buildinga new framework for health promotion anddisease prevention. JAMA. 2009;301(21):2252–2259
7. Braveman P, Barclay C. Health disparities be-ginning in childhood: a life-course perspec-tive. Pediatrics. 2009;124(suppl 3):S163–S175
8. Haggerty RJRK, Pless IB. Child Health andthe Community. New York, NY: John Wileyand Sons; 1975
9. Committee on Psychosocial Aspects ofChild and Family Health; American Acad-emy of Pediatrics. The new morbidityrevisited: a renewed commitment to thepsychosocial aspects of pediatric care.Pediatrics. 2001;108(5):1227–1230
10. Palfrey JS, Tonniges TF, Green M, RichmondJ. Introduction: addressing the millennialmorbidity—the context of community pe-diatrics. Pediatrics. 2005;115(suppl 4):1121–1123
11. Flores G, ; Committee On Pediatric Re-search. Technical report—racial and eth-nic disparities in the health and healthcare of children. Pediatrics. 2010;125(4).Available at: www.pediatrics.org/cgi/con-tent/full/125/4/e979
12. Bronfenbrenner U. The Ecology of HumanDevelopment: Experiments by Nature andDesign. Cambridge, MA: Harvard UniversityPress; 1979
13. Sameroff A. A unified theory of de-velopment: a dialectic integration of natureand nurture. Child Dev. 2010;81(1):6–22
14. Sameroff AJ, Chandler MJ. Reproductiverisk and the continuum of caretaking cau-sality. In: Horowitz FD, Hetherington M,Scarr-Salapatek S, Siegel G, eds. Review ofChild Development Research. Chicago, IL:University of Chicago; 1975:187–244
15. National Research Council, Institute ofMedicine, Committee on Integrating theScience of Early Childhood Development;Shonkoff JP, Phillips D, eds. From Neuronsto Neighborhoods: The Science of EarlyChildhood Development. Washington, DC:National Academies Press; 2000
16. Bronfenbrenner U. Making Human BeingsHuman: Bioecological Perspectives on Hu-man Development. Thousand Oaks, CA:Sage Publications; 2005
17. Shonkoff JP. Building a new bio-developmental framework to guide the fu-ture of early childhood policy. Child Dev.2010;81(1):357–367
18. Bagot RC, Meaney MJ. Epigenetics and thebiological basis of gene × environmentinteractions. J Am Acad Child Adolesc Psy-chiatry. 2010;49(8):752–771
19. National Scientific Council on the DevelopingChild. Early experiences can alter gene ex-pression and affect long-term development:working paper #10. Available at: www.developingchild.net. Accessed March 8, 2011
20. Meaney MJ. Epigenetics and the biologicaldefinition of gene × environment inter-actions. Child Dev. 2010;81(1):41–79
21. Meaney MJ, Szyf M. Environmental pro-gramming of stress responses through DNAmethylation: life at the interface betweena dynamic environment and a fixed genome.Dialogues Clin Neurosci. 2005;7(2):103–123
22. Szyf M, McGowan P, Meaney MJ. The socialenvironment and the epigenome. EnvironMol Mutagen. 2008;49(1):46–60
23. Felitti VJ, Anda RF, Nordenberg D, et al.Relationship of childhood abuse andhousehold dysfunction to many of theleading causes of death in adults. The Ad-verse Childhood Experiences (ACE) Study.Am J Prev Med. 1998;14(4):245–258
24. Schweinhart LJ. Lifetime Effects: The High/Scope Perry Preschool Study Through Age40. Ypsilanti, MI: High/Scope Press; 2005
25. Flaherty EG, Thompson R, Litrownik AJ,et al. Effect of early childhood adversity onchild health. Arch Pediatr Adolesc Med.2006;160(12):1232–1238
26. Koenen KC, Moffitt TE, Poulton R, Martin J,Caspi A. Early childhood factors associatedwith the development of post-traumaticstress disorder: results from a longitudinalbirth cohort. Psychol Med. 2007;37(2):181–192
27. Flaherty EG, Thompson R, Litrownik AJ,et al. Adverse childhood exposures andreported child health at age 12. AcadPediatr. 2009;9(3):150–156
28. Cottrell EC, Seckl JR. Prenatal stress, glu-cocorticoids and the programming of adultdisease. Front Behav Neurosci. 2009;3:19
29. Darnaudéry M, Maccari S. Epigenetic pro-gramming of the stress response in maleand female rats by prenatal restraint stress.Brain Res Brain Res Rev. 2008;57(2):571–585
30. Seckl JR, Meaney MJ. Glucocorticoid “pro-gramming” and PTSD risk. Ann N Y AcadSci. 2006;1071:351–378
31. Oberlander TF, Weinberg J, Papsdorf M,Grunau R, Misri S, Devlin AM. Prenatal ex-posure to maternal depression, neonatalmethylation of human glucocorticoid re-ceptor gene (NR3C1) and infant cortisol
e244 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

stress responses. Epigenetics. 2008;3(2):97–106
32. Brand SR, Engel SM, Canfield RL, Yehuda R.The effect of maternal PTSD following inutero trauma exposure on behavior andtemperament in the 9-month-old infant. AnnN Y Acad Sci. 2006;1071:454–458
33. Murgatroyd C, Patchev AV, Wu Y, et al. Dy-namic DNA methylation programs persis-tent adverse effects of early-life stress. NatNeurosci. 2009;12(12):1559–1566
34. Roth TL, Lubin FD, Funk AJ, Sweatt JD.Lasting epigenetic influence of early-lifeadversity on the BDNF gene. Biol Psychiatry.2009;65(9):760–769
35. Szyf M. The early life environment and theepigenome. Biochim Biophys Acta. 2009;1790(9):878–885
36. Compas BE. Psychobiological processes ofstress and coping: implications for resil-ience in children and adolescents—com-ments on the papers of Romeo & McEwenand Fisher et al. Ann N Y Acad Sci. 2006;1094:226–234
37. Gunnar M, Quevedo K. The neurobiology ofstress and development. Annu Rev Psychol.2007;58:145–173
38. McEwen BS. Physiology and neurobiology ofstress and adaptation: central role of thebrain. Physiol Rev. 2007;87(3):873–904
39. McEwen BS. Stressed or stressed out: whatis the difference? J Psychiatry Neurosci.2005;30(5):315–318
40. McEwen BS, Seeman T. Protective anddamaging effects of mediators of stress.Elaborating and testing the concepts ofallostasis and allostatic load. Ann N Y AcadSci. 1999;896:30–47
41. McEwen BS. Protective and damagingeffects of stress mediators. N Engl J Med.1998;338(3):171–179
42. Korte SM, Koolhaas JM, Wingfield JC, McE-wen BS. The Darwinian concept of stress:benefits of allostasis and costs of allostaticload and the trade-offs in health anddisease. Neurosci Biobehav Rev. 2005;29(1):3–38
43. McEwen BS. Mood disorders and allostaticload. Biol Psychiatry. 2003;54(3):200–207
44. McEwen BS. Stress, adaptation, and dis-ease. Allostasis and allostatic load. Ann N YAcad Sci. 1998;840:33–44
45. National Scientific Council on the Devel-oping Child. Excessive Stress Disrupts theArchitecture of the Developing Brain:Working Paper #3. Available at: developing-child.harvard.edu/resources/reports_and_working_papers/. Accessed March 8, 2011
46. McEwen BS. Protective and damagingeffects of stress mediators: central role of
the brain. Dialogues Clin Neurosci. 2006;8(4):367–381
47. McEwen BS, Gianaros PJ. Stress- andallostasis-induced brain plasticity. AnnuRev Med. 2011;62:431–445
48. National Scientific Council on the De-veloping Child. Persistent fear and anxietycan affect young children’s learning anddevelopment: working paper #9. Availableat: www.developingchild.net. AccessedMarch 8, 2011
49. Tottenham N, Hare TA, Quinn BT, et al. Pro-longed institutional rearing is associatedwith atypically large amygdala volume anddifficulties in emotion regulation. Dev Sci.2010;13(1):46–61
50. Boyce WT, Ellis BJ. Biological sensitivity tocontext: I. An evolutionary-developmentaltheory of the origins and functions ofstress reactivity. Dev Psychopathol. 2005;17(2):271–301
51. Francis DD. Conceptualizing child healthdisparities: a role for developmental neu-rogenomics. Pediatrics. 2009;124(suppl 3):S196–S202
52. Juster RP, McEwen BS, Lupien SJ. Allostaticload biomarkers of chronic stress andimpact on health and cognition. NeurosciBiobehav Rev. 2010;35(1):2–16
53. McEwen BS, Gianaros PJ. Central role of thebrain in stress and adaptation: links tosocioeconomic status, health, and disease.Ann N Y Acad Sci. 2010;1186:190–222
54. Rothman EF, Edwards EM, Heeren T, HingsonRW. Adverse childhood experiences predictearlier age of drinking onset: results froma representative US sample of current orformer drinkers. Pediatrics. 2008;122(2).Available at: www.pediatrics.org/cgi/content/full/122/2/e298
55. Anda RF, Croft JB, Felitti VJ, et al. Adversechildhood experiences and smoking duringadolescence and adulthood. JAMA. 1999;282(17):1652–1658
56. Anda RF, Felitti VJ, Bremner JD, et al. Theenduring effects of abuse and related ad-verse experiences in childhood. A conver-gence of evidence from neurobiology andepidemiology. Eur Arch Psychiatry ClinNeurosci. 2006;256(3):174–186
57. Scherrer JF, Xian H, Kapp JM, et al. Asso-ciation between exposure to childhood andlifetime traumatic events and lifetimepathological gambling in a twin cohort.J Nerv Ment Dis. 2007;195(1):72–78
58. Wickrama KA, Conger RD, Lorenz FO, Jung T.Family antecedents and consequences oftrajectories of depressive symptoms fromadolescence to young adulthood: a lifecourse investigation. J Health Soc Behav.2008;49(4):468–483
59. Kahn RS, Brandt D, Whitaker RC. Combinedeffect of mothers’ and fathers’ mentalhealth symptoms on children’s behavioraland emotional well-being. Arch PediatrAdolesc Med. 2004;158(8):721–729
60. Felitti VJ. Adverse childhood experiencesand adult health. Acad Pediatr. 2009;9(3):131–132
61. Althoff KN, Karpati A, Hero J, Matte TD.Secular changes in mortality disparities inNew York City: a reexamination. J UrbanHealth. 2009;86(5):729–744
62. Cheng TL, Jenkins RR. Health disparitiesacross the lifespan: where are the chil-dren? JAMA. 2009;301(23):2491–2492
63. DeVoe JE, Tillotson C, Wallace LS. Uninsuredchildren and adolescents with insuredparents. JAMA. 2008;300(16):1904–1913
64. Due P, Merlo J, Harel-Fisch Y, et al. Socio-economic inequality in exposure to bullyingduring adolescence: a comparative, cross-sectional, multilevel study in 35 countries.Am J Public Health. 2009;99(5):907–914
65. Reid KW, Vittinghoff E, Kushel MB. Associa-tion between the level of housing in-stability, economic standing and healthcare access: a meta-regression. J HealthCare Poor Underserved. 2008;19(4):1212–1228
66. Stevens GD, Pickering TA, Seid M, Tsai KY.Disparities in the national prevalence ofa quality medical home for children withasthma. Acad Pediatr. 2009;9(4):234–241
67. Williams DR, Sternthal M, Wright RJ. So-cial determinants: taking the social contextof asthma seriously. Pediatrics. 2009;123(suppl 3):S174–S184
68. Bierhaus A, Wolf J, Andrassy M, et al. Amechanism converting psychosocial stressinto mononuclear cell activation. Proc NatlAcad Sci U S A. 2003;100(4):1920–1925
69. Araújo JP, Lourenço P, Azevedo A, et al.Prognostic value of high-sensitivity C-reactive protein in heart failure: a system-atic review. J Card Fail. 2009;15(3):256–266
70. Galkina E, Ley K. Immune and inflammatorymechanisms of atherosclerosis (*). AnnuRev Immunol. 2009;27:165–197
71. Miller GE, Chen E. Harsh family climate inearly life presages the emergence of aproinflammatory phenotype in adolescence.Psychol Sci. 2010;21(6):848–856
72. Poulton R, Caspi A, Milne BJ, et al. Associ-ation between children’s experience of so-cioeconomic disadvantage and adulthealth: a life-course study. Lancet. 2002;360(9346):1640–1645
73. Ward JR, Wilson HL, Francis SE, CrossmanDC, Sabroe I. Translational mini-reviewseries on immunology of vascular dis-ease: inflammation, infections and Toll-like
PEDIATRICS Volume 129, Number 1, January 2012 e245
FROM THE AMERICAN ACADEMY OF PEDIATRICS
by 1394751 on April 27, 2017Downloaded from

receptors in cardiovascular disease. ClinExp Immunol. 2009;156(3):386–394
74. Heydtmann M, Adams DH. Chemokines inthe immunopathogenesis of hepatitis C in-fection. Hepatology. 2009;49(2):676–688
75. Berasain C, Castillo J, Perugorria MJ,Latasa MU, Prieto J, Avila MA. Inflammationand liver cancer: new molecular links. AnnN Y Acad Sci. 2009;1155:206–221
76. Chen E, Miller GE. Stress and inflammationin exacerbations of asthma. Brain BehavImmun. 2007;21(8):993–999
77. Yao H, Rahman I. Current concepts on therole of inflammation in COPD and lungcancer. Curr Opin Pharmacol. 2009;9(4):375–383
78. Li M, Zhou Y, Feng G, Su SB. The critical roleof Toll-like receptor signaling pathways inthe induction and progression of autoim-mune diseases. Curr Mol Med. 2009;9(3):365–374
79. Danese A, Moffitt TE, Pariante CM, Ambler A,Poulton R, Caspi A. Elevated inflammationlevels in depressed adults with a history ofchildhood maltreatment. Arch Gen Psychi-atry. 2008;65(4):409–415
80. Danese A, Pariante CM, Caspi A, Taylor A,Poulton R. Childhood maltreatment pre-dicts adult inflammation in a life-coursestudy. Proc Natl Acad Sci U S A. 2007;104(4):1319–1324
81. Howren MB, Lamkin DM, Suls J. Associa-tions of depression with C-reactive protein,IL-1, and IL-6: a meta-analysis. PsychosomMed. 2009;71(2):171–186
82. Cuhna F, Heckman JJ, Lochner LJ, MasterovDV. Interpreting the evidence on life cycleskill formation. In: Hanushek EA, Welch F, eds.Handbook of the Economics of Education.
Amsterdam, Netherlands: North-Holland; 2006:697–812
83. Heckman JJ, Stixrud J, Urzua S. The effectsof cognitive and non-cognitive abilities onlabor market outcomes and social behav-ior. J Labor Econ. 2006;24:411–482
84. Heckman JJ. Role of income and familyinfluence on child outcomes. Ann N Y AcadSci. 2008;1136:307–323
85. Heckman JJ. The case for investing in dis-advantaged young children. Available at:www.firstfocus.net/sites/default/files/r.2008-9.15.ff_.pdf. Accessed March 8, 2011
86. Heckman JJ, Masterov DV. The productivityargument for investing in young children.Available at: http://jenni.uchicago.edu/human-inequality/papers/Heckman_final_all_wp_2007-03-22c_jsb.pdf. Accessed March 8, 2011
87. Richmond JB. Child development: a basicscience for pediatrics. Pediatrics. 1967;39(5):649–658
88. Leslie LK, Slaw KM, Edwards A, Starmer AJ,Duby JC, ; Members of Vision of Pediatrics2020 Task Force. Peering into the future:pediatrics in a changing world. Pediatrics.2010;126(5):982–988
89. Starmer AJ, Duby JC, Slaw KM, Edwards A,Leslie LK, ; Members of Vision of Pediat-rics 2020 Task Force. Pediatrics in theyear 2020 and beyond: preparing forplausible futures. Pediatrics. 2010;126(5):971–981
90. Halfon N, DuPlessis H, Inkelas M. Trans-forming the U.S. child health system. HealthAff (Millwood). 2007;26(2):315–330
91. Schor EL. The future pediatrician: pro-moting children’s health and development.J Pediatr. 2007;151(suppl 5):S11–S16
92. Tanner JL, Stein MT, Olson LM, Frintner MP,Radecki L. Reflections on well-child carepractice: a national study of pediatricclinicians. Pediatrics. 2009;124(3):849–857
93. Radecki L, Olson LM, Frintner MP, Tanner JL,Stein MT. What do families want from well-child care? Including parents in the re-thinking discussion. Pediatrics. 2009;124(3):858–865
94. Fisher PA, Gunnar MR, Dozier M, Bruce J,Pears KC. Effects of therapeutic inter-ventions for foster children on behavioralproblems, caregiver attachment, and stressregulatory neural systems. Ann N Y Acad Sci.2006;1094:215–225
95. Mercy JA, Saul J. Creating a healthier fu-ture through early interventions for chil-dren. JAMA. 2009;301(21):2262–2264
96. Middlebrooks JS, Audage NC. The effects ofchildhood stress on health across the life-span. Available at: www.cdc.gov/ncipc/pub-res/pdf/Childhood_Stress.pdf. Accessed July20, 2009
97. Earls MF, ; Committee on PsychosocialAspects of Child and Family Health; Ameri-can Academy of Pediatrics. Incorporatingrecognition and management of perinataland postpartum depression into pediatricpractice. Pediatrics. 2010;126(5):1032–1039
98. Center on the Developing Child at HarvardUniversity. Maternal depression can un-dermine the development of young chil-dren: working paper #8. Available at: www.developingchild.harvard.edu. Accessed March8, 2011
99. Shonkoff J. Protecting brains, not simplystimulating minds. Science. 2011;333(6045):982–983
e246 FROM THE AMERICAN ACADEMY OF PEDIATRICSby 1394751 on April 27, 2017Downloaded from

DOI: 10.1542/peds.2011-2663; originally published online December 26, 2011; 2012;129;e232Pediatrics
and David L. WoodMary I. Dobbins, Marian F. Earls, Andrew S. Garner, Laura McGuinn, John Pascoe
DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS, Benjamin S. Siegel, CHILDHOOD, ADOPTION, AND DEPENDENT CARE, AND SECTION ONASPECTS OF CHILD AND FAMILY HEALTH, COMMITTEE ON EARLY
Jack P. Shonkoff, Andrew S. Garner, THE COMMITTEE ON PSYCHOSOCIALThe Lifelong Effects of Early Childhood Adversity and Toxic Stress
ServicesUpdated Information &
/content/129/1/e232.full.htmlincluding high resolution figures, can be found at:
References
/content/129/1/e232.full.html#ref-list-1at:This article cites 84 articles, 22 of which can be accessed free
Citations /content/129/1/e232.full.html#related-urls
This article has been cited by 100 HighWire-hosted articles:
Subspecialty Collections
/cgi/collection/development:behavioral_issues_subDevelopmental/Behavioral Pediatrics
_and_family_health/cgi/collection/committee_on_psychosocial_aspects_of_childHealthCommittee on Psychosocial Aspects of Child and Familythe following collection(s):This article, along with others on similar topics, appears in
Permissions & Licensing
/site/misc/Permissions.xhtmltables) or in its entirety can be found online at: Information about reproducing this article in parts (figures,
Reprints /site/misc/reprints.xhtml
Information about ordering reprints can be found online:
rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.Grove Village, Illinois, 60007. Copyright © 2012 by the American Academy of Pediatrics. All and trademarked by the American Academy of Pediatrics, 141 Northwest Point Boulevard, Elkpublication, it has been published continuously since 1948. PEDIATRICS is owned, published, PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
by 1394751 on April 27, 2017Downloaded from

DOI: 10.1542/peds.2011-2663; originally published online December 26, 2011; 2012;129;e232Pediatrics
and David L. WoodMary I. Dobbins, Marian F. Earls, Andrew S. Garner, Laura McGuinn, John Pascoe
DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS, Benjamin S. Siegel, CHILDHOOD, ADOPTION, AND DEPENDENT CARE, AND SECTION ONASPECTS OF CHILD AND FAMILY HEALTH, COMMITTEE ON EARLY
Jack P. Shonkoff, Andrew S. Garner, THE COMMITTEE ON PSYCHOSOCIALThe Lifelong Effects of Early Childhood Adversity and Toxic Stress
/content/129/1/e232.full.htmllocated on the World Wide Web at:
The online version of this article, along with updated information and services, is
of Pediatrics. All rights reserved. Print ISSN: 0031-4005. Online ISSN: 1098-4275.Boulevard, Elk Grove Village, Illinois, 60007. Copyright © 2012 by the American Academy published, and trademarked by the American Academy of Pediatrics, 141 Northwest Pointpublication, it has been published continuously since 1948. PEDIATRICS is owned, PEDIATRICS is the official journal of the American Academy of Pediatrics. A monthly
by 1394751 on April 27, 2017Downloaded from

Military Children and FamiliesStrengths and Challenges During Peace and War
Nansook Park University of Michigan
Throughout history, military children and families haveshown great capacity for adaptation and resilience. How-ever, in recent years, unprecedented lengthy and multiplecombat deployments of service members have posed mul-tiple challenges for U.S. military children and families.Despite needs to better understand the impact of deploy-ment on military children and families and to provideproper support for them, rigorous research is lacking.Programs exist that are intended to help, but their effec-tiveness is largely unknown. They need to be better coor-dinated and delivered at the level of individuals, families,and communities. Research and programs need to take acomprehensive approach that is strengths based and prob-lem focused. Programs for military children and familiesoften focus on the prevention or reduction of problems. It isjust as important to recognize their assets and to promotethem. This article reviews existing research on militarychildren and families, with attention to their strengths aswell as their challenges. Issues in need of further researchare identified, especially research into programs that assistmilitary children and families. Military children and fam-ilies deserve greater attention from psychology.
Keywords: military children, military families, strengths,challenges, strengths-based approaches
The gathering of military men should be thanking their children,their fine and resourceful children, who were strangers in everyschool they entered, thanking them for their extraordinary serviceto their country, for the sacrifices they made over and over again. . . Military brats . . . [spend] their entire youth in service to thiscountry and no one even [knows]. (Conroy, 1991, p. xxv)
A common saying in the military is that when oneperson joins, the whole family serves. Militaryfamilies may often be in the background of public
discourse on the military, but they are critical to its success.Although aspects of military life can be difficult for fami-lies, positive family functioning boosts a service member’smorale, retention, and ability to carry out missions (Shin-seki, 2003). According to a recent report, service membersreported positive family relationships as a source of resil-ience and problems at home as a source of stress andinterference (Mental Health Advisory Team 6, 2009). Anyefforts to build a strong, effective, and sustainable militaryforce must also consider military families, improving therelationships of the soldier with his or her family membersand strengthening the family itself (cf. Gottman, Gottman,& Atkins, 2011).
Since the start of the Global War on Terror, militarychildren and families have faced multiple tests associatedwith unprecedented lengthy and multiple deployments;shorter stays at home between deployments; and greaterrisks of death, injury, and psychological problems amongservice members. Although many military children andfamilies rise to the occasion and do well (Wiens & Boss,2006), these challenges can take a toll on their health andwell-being (Chandra, Burns, Tanielian, Jaycox, & Scott,2008; Flake, Davis, Johnson, & Middleton, 2009). Despiteurgent needs to better understand the impact of deploymenton military children and families and to provide appropriatesupport for them, there is a dearth of research. Programsand interventions exist, but definitive conclusions aboutwhat really works are by and large lacking.
Programs that try to assist military children and fam-ilies often focus only on the prevention or reduction ofproblems. As important as it is to address problems, it isjust as important to recognize the strengths and assets ofmilitary children and families and to promote and bolsterthem. A full and accurate picture of military children andfamilies is needed upon which to base interventions. One ofthe best ways to prevent or solve problems is to identifywhat goes well and to use this as the basis of intervention(Park, 2004, 2009; Park & Peterson, 2008; Park, Peterson,& Brunwasser, 2009; Peterson & Park, 2003).
Over the years, studies of military children and fam-ilies by psychologists have been isolated from and ne-glected by mainstream psychology. Most studies are doneby researchers who are present or former members of themilitary or immediate members of military families. Stud-ies are too rarely published in the mainstream psychologyjournals. This state of affairs needs to change to meet thesurging needs of military children and families.
This article describes what is known about militarychildren and families: their demographics, their challenges,and their strengths, during both peace and war times. Also
I would like to acknowledge Daniel Fifis, retired school psychologist atFort Jackson Schools, Columbia, South Carolina, whose generosity anddedication to military children and families have touched so many, in-cluding me. I thank Christopher Peterson, Albert Cain, Mary Keller,Jennifer Kirkpatrick, and Joyce Hodson for their help during preparationof this article. Special thanks go to Patricia K. Shinseki, who sharedvaluable insights and resources about military children and families andprovided inspiration through her deep concerns and caring for them.
Correspondence concerning this article should be addressed to Nan-sook Park, Department of Psychology, University of Michigan, 530Church Street, Ann Arbor, MI 48109-1043. E-mail: [email protected]
65January 2011 ● American Psychologist© 2011 American Psychological Association 0003-066X/11/$12.00Vol. 66, No. 1, 65–72 DOI: 10.1037/a0021249

addressed are issues and gaps in the existing research andpractice. The thesis is that greater attention to the strengthsand assets of military children and families is needed inorder to design and implement effective programs to sup-port them. This approach echoes the premise of the U.S.Army Comprehensive Soldier Fitness (CSF) program de-scribed elsewhere in this special issue (Cornum, Matthews,& Seligman, 2011). The fitness of soldiers extends beyondmere physical prowess to include psychosocial well-being,a key component of which is the well-being of their fam-ilies (Peterson, Park, & Castro, 2011; Rohall, Segal, &Segal, 1999). Currently, collaborative efforts between psy-chologists and the U.S. Army are extending the CSF pro-gram to family members.
The Changing Demographics of theModern U.S. Military FamilyIn the United States today, there are several million menand women wearing the uniform of the country’s military.In broad terms, this is a young (50% below age 25) andmale (85%) population, with individuals from rural, lessaffluent, and ethnic minority (African American andLatino/a) backgrounds overrepresented (U.S. Departmentof Defense, Defense Manpower Data Center, 2008). Al-most all have a high school degree or equivalent, and 70%have at least some college credits. About half of them aremarried, with about 10% of the armed forces in dual-careermarriages (i.e., married to another member of the military).
In contrast to the U.S. population as a whole, membersof the military tend to marry earlier, a fact that researchersneed to take into account in comparing military and civilianfamilies because marriage at a younger age can be associ-ated with more problems than marriage at an older age(Amato, Booth, Johnson, & Rogers, 2007). Among married
individuals in the armed forces, more than 70% have one ormore children, and there are at least 1.85 million childrenwith one or both parents in the military (65% active dutyand 35% Reserves or National Guard; Chandra et al., 2008;Segal & Segal, 2004).
Research on military families as well as formal pro-grams to support them often uses a narrow definition ofwhat a family entails: mother and father—one of whomwears a uniform—and their biological children. The so-called nuclear family is not the only type that exists,especially in the contemporary United States. Single-parentfamilies have increased in recent decades, as well asblended families and intergenerational families. With theincrease of women in the military, dual-career militaryfamilies have increased (Segal & Segal, 2004). Each typeof family has unique difficulties and assets.
In this article, the phrase military children and fami-lies is used to refer broadly to all individuals who areconnected to a military family—traditional and nontradi-tional families, extended and binuclear families, spousesand significant others, sons and daughters, stepsons andstepdaughters, brothers and sisters, parents and grandpar-ents, and so on. The focus is on military-connected chil-dren, but the functioning of all family members bears onthe well-being of these children.
Strengths and Challenges AmongMilitary Children and FamiliesMilitary life presents both challenges and opportunities togrow for children and families (Hall, 2008). To provideeffective services for military children and families, weneed a better understanding of these challenges andstrengths framed in terms of the culture and function of themilitary during peace and during war.
During Peace
Even during peaceful times, military children and familiesface recurrent separations, frequent and often suddenmoves, difficult reunions, long and often unpredictableduty hours, and the threat of injury or death of the militaryservice member during routine training and peaceful mis-sions (Black, 1993). On average, active duty military fam-ilies move every two to three years within the United Statesor overseas (Croan, Levine, & Blankinship, 1992). Second-ary school-age students move three times more often thantheir civilian counterparts do (Shinseki, 2003). These fre-quent relocations disrupt children’s schoolwork, activities,and social networks, requiring ongoing adjustment to newschools and cultures. Children can grow up feeling rootlessand may have difficulties building deeper relationships ormaintaining long-term commitments (Wertsch, 1991). Es-pecially during adolescence, interruption of peer relation-ships can be detrimental to a child’s psychosocial devel-opment (Shaw, 1979). Also, separation from a parentbecause of military assignments can have negative impactson a child’s school performance and mental health (Jensen,Grogan, Xenakis, & Bain, 1989). Due to different schooland state requirements for course credits and course mate-
NansookPark
66 January 2011 ● American Psychologist

rials, frequent moves pose additional challenges for aca-demic achievement and graduation by transferring stu-dents. These problems are especially pronounced forstudents with special needs (Hall, 2008).
Nevertheless, the available evidence suggests that mil-itary children typically function as well as or even betterthan civilian children on most indices of health, well-being,and academic achievement. They have similar or lowerrates of childhood psychopathology, lower rates of juveniledelinquency, lower likelihood of alcohol or drug abuse,better grades, and higher median IQs than do their civiliancounterparts (Jensen, Xenakis, Wolf, & Bain, 1991; Kenny,1967; Morrison, 1981). According to a large-scale surveyof military adolescents (Jeffreys & Leitzel, 2000), militarychildren are in general healthy, have good peer relation-ships, are engaged in school and community, do well atschool, and are satisfied with life. On average, militarychildren report high optimism and positive self-images(Watanabe, 1985).
Compared with civilian children, military childrenhave greater respect for authority and are more tolerant,resourceful, adaptable, responsible, and welcoming of chal-lenges, and they have a greater likelihood of knowing andbefriending someone who is “different” (Hall, 2008); theyengage in fewer risky behaviors (Hutchinson, 2006); theyexhibit greater self-control (Watanabe, 1985); and theyshow lower levels of impatience, aggression, and disobe-dience and higher levels of competitiveness (Manning,Balson, & Xenakis, 1988). Most military children arehappy to embrace the term military brat and one or anotherof its backronyms such as “brave, resilient, adaptable, andtrustworthy.”1
Difficult life events do not automatically lead to prob-lems in children. In some cases, challenges provide anopportunity to grow. For instance, relocation can be apositive experience. Children and families have the oppor-tunity to meet new people and make new friends, to visitdifferent places, and to experience diverse cultures(O’Connell, 1981).
If families have positive attitudes toward relocation,social support, previous relocation experience, and activecoping styles, they do better when they move (Feldman &Tompson, 1993; Frame & Shehan, 1994). As stressful asparental separation can be, military children are affordedthe opportunity to take on responsibilities and to be moreindependent and mature. Although the inherent hierarchyand structure of military culture can produce resentmentamong some military children and decrease their indepen-dent thinking, it can also foster discipline. Furthermore,military values that emphasize service, sacrifice, honor,teamwork, loyalty, sense of purpose, sense of community,and pride can work as resilience factors to overcome thedifficulties of military life (Paden & Pezor, 1993).
During WarThe major challenge for military children and familiesduring war is a lengthy deployment of the uniformed fam-ily member to a combat zone. Children not only miss thedeployed parent, but they also experience obvious uncer-
tainty surrounding his or her safety, especially in single-parent or dual-career families. There are other issues aswell. Children may be asked to take on greater responsi-bilities, and daily routines may change (Pincus, House,Christenson, & Adler, 2001). Families may move to becloser to other relatives. Unlike relocation during times ofpeace, war-time relocation of families may require them tomove off base into the civilian community where they losethe existing military support system (MacDermid, 2006).
Nearly 900,000 U.S. children have had at least one oftheir parents deployed since 2001, and currently 234,000children have one or both parents at war (Zoroya, 2009).Long and frequent deployments of service members putmilitary children and families at risk for psychosocial prob-lems (American Psychological Association, PresidentialTask Force on Military Deployment Services for Youth,Families, and Service Members, 2007). According to U.S.Department of Defense data, between 2003 and 2008 thenumber of military children receiving outpatient mentalhealth care doubled, and during that period inpatient visitsby military children increased by 50%, with a 20% jumpfrom 2007 to 2008 (“Department of Defense Reaches Outto Children of Soldiers,” 2009). This indicates potentially acumulative toll of parental deployments on military chil-dren and urgent needs for proper mental health services forthis population.
Although scarce, several studies have looked at theimpact of parental deployment on children during currentwars. Although military children and families cope rela-tively well with shorter separations (less than six months),longer and multiple deployments create measurable distress(Chandra et al., 2010; Flake et al., 2009). Parental deploy-ment can affect physical health, academic performance,behavior problems, depression, and anxiety of militarychildren. Adolescent children of deployed parents showsignificantly higher levels of stress, systolic blood pressure,and heart rate than their civilian counterparts (Barnes,Davis, & Treiber, 2007). Children of deployed servicemembers also show decreases in their academic perfor-mance, school engagement, and overall school adjustment(Engel, Gallagher, & Lyle, 2010). More than one third ofschool-age children showed high risk for psychosocial dif-ficulties during parental deployment, 2.5 times the nationalnorm (Flake et al., 2009). Children of deployed parents,especially older youth and girls, reported more problemswith school, family, and mental health. The longer theparental deployment is, the greater these problems are,during and after deployment (Chandra et al., 2010).
Risk factors exacerbating the negative effects of de-ployment on military children and families include a his-tory of family problems, younger families, less educatedfamilies, foreign-born spouses, families with young chil-dren, those with lower pay grades or reduced income, thosewithout a unit affiliation such as National Guard and Re-
1 The origin of the term military brat is not agreed on, although somehave traced it to an acronym for British Regiment Attached Traveler (i.e.,a soldier’s child).
67January 2011 ● American Psychologist

serve families, families with children who have disabilities,families with pregnancies, single-parent families, and fam-ilies with mothers in the military (American PsychologicalAssociation, Presidential Task Force, 2007).
Although military deployment poses risks, especiallyfor some families, it is equally important to remember thatmany military children and families show resilience andgrowth. During the deployment of a family member, par-ents report that their children are closer to family andfriends, and that they are more responsible, independent,and proud. Seventy-four percent of the spouses of servicemembers report personal growth, despite also reportingincreased loneliness, stress, and anxiety (U.S. Departmentof Defense, Defense Manpower Data Center, 2009b).
Resilience plays an important role in all phases ofdeployment. Resilience mitigates stress and improves ad-justment to deployment by children and families. Familiesthat function most effectively are active, optimistic, self-reliant, and flexible (Jensen & Shaw, 1996; Wiens & Boss,2006). Families that function well find meaning in militarylife and identify with the work of their uniformed familymember (Hammer, Cullen, Marchand, & Dezsofi, 2006;Marchant & Medway, 1987). Family preparedness for de-ployment as well as community and social support lead tobetter adjustment (Wiens & Boss, 2006).
Huebner (2010) found that adolescents who adaptedwell during parental deployment showed the ability to putthe situation in perspective; positive reframing; the embrac-ing of change and adaptation as necessary; effective copingskills; and good relationships with family, friends, andneighbors. For example, one adolescent reported, “I havereally good neighbors that understand the situation goingon. And I’m always welcome at my neighbors” (Huebner,2010, p. 14).
During deployment, the well-being of military chil-dren needs to be approached not just at the level of theindividual child but also in terms of larger social systems—the extended family, neighborhoods, schools, and commu-nities. The community environment affects children’s ad-justment and coping during wartime deployment, andparental stress strongly relates to a military child’s psycho-social functioning during deployment (Flake et al., 2009;Huebner, Mancini, Bowen, & Orthner, 2009). The chal-lenges faced by military children are exacerbated by familyand community inability to recognize and provide propersupport and assistance. If the family as a whole adjusts wellto deployment, then so do children. If we care about mil-itary children’s well-being, it is imperative to ensure familywell-being because they are so closely connected.
All things considered, military families on averagehave done well and show resilience during peace and evenwar. Problems of course exist for some military families,but rarely to a greater extent than among civilian families.Contrast this conclusion with the notion of the militaryfamily syndrome, which refers to a constellation of out-of-control offspring, authoritarian fathers, and depressedmothers (Lagrone, 1978). This alleged syndrome has beenrefuted repeatedly by relevant evidence (e.g., Jensen, Gor-don, Lewis, & Xenakis, 1986; Jensen et al., 1991; Morri-
son, 1981), but it seems to be as resilient as the healthymilitary family that it fails to acknowledge. The fact thatmilitary families overall have done well in the past de-serves greater dissemination in the present than seems tooccur in today’s popular media. If nothing else, the histor-ical strength of the military family can serve as a source ofpride and inspiration.
Strengths-Based ApproachesMilitary children and families often do well, but they arenot invulnerable (Cozza, Chun, & Polo, 2005). Rather, theydo well because they have compensating strengths andassets (Bowen, Mancini, Martin, Ware, & Nelson, 2003:Palmer, 2008). It behooves us to identify what these maybe, to enhance them, and to use what is learned to designinterventions for all military children and families, thosewith or without problems. As noted, one way to prevent orsolve problems is to base interventions on what is goingwell.
The previous section reviewed the strengths and assetsof military children and families. More family supportprograms that address strengths as well as problems areneeded. Existing programs need not be replaced but ex-panded. A focus on what goes well does not mean that whatgoes poorly should be ignored. Indeed, strengths-basedinterventions complement and extend problem-focused in-terventions (Park, 2004, 2009; Park & Peterson, 2006,2008; Park et al., 2009; Peterson & Park, 2003). A com-prehensive approach to the support of military families maybe more effective than a problem-focused strategy, and itwould certainly reduce the stigma that surrounds the seek-ing of “mental health” care.
Programs and resources, formal and informal, alreadyexist in both military and civilian sectors to support mili-tary children and families. Targeted programs and servicesare helpful, but we need further assistance, support, andengagement of the broader community.
The Military Child Education Coalition (MCEC) pro-grams to support military children are worthy of attention.They embody the strengths-based focus advocated here.MCEC has been working directly with different branchesof the military, school districts, and parents to facilitatetransition of transferring military children (MCEC, 2001).MCEC offers regular training for school counselors andteachers, involves civilian students in their programs, andmakes available relevant information to schools as well asparents. Underlying all of the MCEC programs is theassumption that military families are resilient and resource-ful, but that accessible information, consistent school rules,and support help reduce the annoyances associated withstudent relocation.
The Student 2 Student program of MCEC is a uniquestudent-led, school-based program for transitioning stu-dents from military families. This program provides socialas well as instrumental support for students relocating toand from different schools. A team of advisors, volunteerstudents, and school liaison officers from each school aretrained to develop and implement specific plans that fittheir particular school setting and to implement, recruit,
68 January 2011 ● American Psychologist

and train others at their school. These programs benefit alltransitioning students, military connected or not.
As another example, MCEC’s initiative “Living in theNew Normal: Helping Children Thrive through Good andChallenging Times” engages and empowers the wholecommunity. It is designed to reach everyone involved withmilitary-connected children. It provides resources andtrains adults to help children with deployment-related chal-lenges to develop resilience. Further, the program bringstogether all sectors of the community to identify the uniqueassets of that community and to develop specific plans toutilize those assets to provide sustained support not only formilitary children and families but also for all communitymembers. The MCEC programs stand in contrast to manyother interventions for military families, which are oftenbrief and highly targeted, because they involve larger socialunits (schools and communities) on an ongoing basis.
Issues and RecommendationsThere is a significant shortage of evidence-based programs.Indeed, many programs for military children and familiesare not evaluated at all. In the absence of evidence for theireffectiveness, they are but well-intended interventions.When resources are limited and demands are great, it iseven more critical to identify programs that are effectiveand efficient, and to understand the active ingredients thatmake programs successful (Lester, McBride, Bliese, &Adler, 2011). Following appropriate evaluation, successfulprograms can be disseminated with confidence, and inef-fective programs can be modified or eliminated. A betterjob needs to be done coordinating and disseminating infor-mation about existing programs, increasing their accessi-bility to the entire military community, and reducingstigma associated with seeking mental health care.
More generally, the research literature on militarychildren and families is too scant, especially in light ofcontemporary concerns with their well-being while theUnited States is at war. Several observations about thisliterature are offered, followed by recommendations forfurther research and interventions.
Much of the relevant research on military families isnot methodologically rigorous. Studies are often hamperedby small and nonrepresentative samples and often lackappropriate comparison groups. They are often cross-sec-tional and starkly descriptive. Potential confounds are oftennot measured and thus cannot be taken into account, leav-ing studies inconclusive.
Studies of military children need to use multiple in-formants. Studies usually depend on what the nonmilitaryparent says and may reflect a reporting bias. Consider thatone investigation found greater problems among militarychildren than among civilian children according to parentalreport but not according to the direct report of the children(Jensen et al., 1991). Chandra et al. (2010) noted similardiscrepancies between conclusions based on parental reportand child report.
The lack of explicit theory is conspicuous, althoughthere is an important exception: the cycle of deploymentmodel, which distinguishes different phases through which
military families pass when a family member is deployed:(a) predeployment (from notification to departure), (b) de-ployment (from departure to return), (c) reunion (termedredeployment in the military), and (d) postdeployment.Each phase has its own characteristics and requirements(Pincus et al., 2001).
Research on the effects of deployment on militarychildren and families usually focuses only on the period ofactual deployment. Redeployment and postdeployment arepoorly understood and in need of greater explication. Al-though reunion can be joyous, it also requires changes andadjustments in roles and routines for all family members,and these can be stressful and confusing (American Psy-chological Association, Presidential Task Force, 2007).Furthermore, many families have to start preparing for thenext deployment again. For both families and service mem-bers alike, the postdeployment stage is particularly longand complex (MacDermid, 2006). Many returning servicemembers experience combat-related mental health prob-lems, injuries, and disabilities. These can burden childrenand families. There is simply not enough research about thelong-term effects on children and families of living with aparent who is experiencing such difficulties and how tohelp them. Longitudinal studies are needed.
Also, a developmental perspective should be utilizedin understanding the effect of deployment on children inorder to provide developmentally appropriate services.Children at various developmental stages face differentdevelopmental tasks and have different levels of cognitive,emotional, and social skills. As a result, children mayrespond quite differently at each deployment cycle depend-ing on their developmental stages (Paden & Pezor, 1993).
As already noted, most military family studies assumea traditional family and thus do not adequately sample therelevant populations. Considering the diversity of militaryfamily types, future studies should examine the impact ofmilitary life, especially deployment, on children from dif-ferent types of families. Future studies should also comparethe effects on children of maternal versus paternal deploy-ment.
Although studies have been done spanning differentmilitary eras, they rarely use the same measures or proce-dures, precluding strong conclusions about similarities anddifferences among different military cohorts (e.g., thoseserving during Vietnam, Somalia, Desert Storm, and Op-eration Iraqi Freedom/Operation Enduring Freedom versusthose serving during more peaceful times). Military fami-lies, no less than their civilian counterparts, are complex.The challenges they face are likely not across the board butrather are influenced by a host of interacting factors—branch of service, age, education, ethnicity, pre-existingproblems and assets, community integration (e.g., living onbase or off base), exposure to combat, and number ofdeployments—that are rarely studied in terms of their in-teractions.
Studies making direct comparisons across branches ofthe service are also rare, although those studies that do existoften find differences in family functioning across Army,Navy, Air Force, Coast Guard, and Marines. Another ne-
69January 2011 ● American Psychologist

glected contrast related to family functioning is whether theuniformed family member is active duty or Reserve orNational Guard. As is well known, a large number ofReserve and National Guard members currently serve; al-most 700,000 members of the Reserve and National Guardhave been activated since 9/11, parents of about 35% ofmilitary children (U.S. Department of Defense, DefenseManpower Data Center, 2009a). Reserve and NationalGuard families live off base among civilians and are lessintegrated into a military community, factors that limit theiraccess to military support systems and programs. Manyhave either left or put on hold their civilian careers becauseof their “suddenly military” status. The effects on childrenand families are largely unknown, although one suspectsthat they include notable instability and stress.
Recent reports suggest that Reserve children and fam-ilies may be at greater risk for mental health and adjustmentissues (Chandra et al., 2008; Mental Health Advisory Team6, 2009). Children from Reserve families report a lack ofunderstanding and support from their peers and teachersmore than children from active-duty families. And whatabout the children and families of civilian contractors andFederal Agency employees serving in war zones, soheavily relied upon during the current wars? No study hasaddressed the challenges they face.
There are members of the military family who areoften neglected in research and intervention. Siblings canplay an important role in bolstering the well-being andresilience of military children and deployed service mem-bers. Sibling relationships in general are among the mostcrucial in a person’s life (Bank & Kahn, 1982). Increasedattention to military children who do or do not have sib-lings would be important. Given frequent relocations, sib-lings may be even more important for military childrenthan for civilian children, providing stability, familiarity,and support not readily available elsewhere.
Another glaring absence in the literature is consider-ation of the brothers and sisters of service members. Thesiblings of service members are of course affected by thedeployment, injury, or death of those who serve, but vir-tually nothing is known about challenges they face and howto help them. Studies of civilians make clear that siblingloss adversely affects health and well-being. Survivingsiblings often experience anxiety, guilt, sadness, and anger(Bank & Kahn, 1982). They report health that is evenworse than that of surviving spouses (Hays, Gold, &Pieper, 1997).
“Siblings of troops often are forgotten mourners” (He-fling, 2009). According to a recent report, there are severalthousand surviving siblings from current wars. Many are intheir 20s or 30s (Hefling, 2009), but considering that manyservice members who have lost their lives were young, alarge number of surviving siblings are also in their teens oreven younger—children themselves. When a service mem-ber dies, the spouse, the children, and the parents aregenerally expected to be most affected. Sibling death maybe overlooked as a significant loss (Moss, Moss, & Hans-son, 2001). As a result, siblings may not receive the supportthey need.
Finally, more research is needed to understand theimpact of deployment and grief on military parents andgrandparents (Rando, 1986). Their coping and adjustmentare important for their own sake as well as in terms of theimpacts on the health and well-being of all other familymembers (Fry, 1997).
CSF Program for Military FamilyMembersCurrently, a major effort is under way to extend the CSFprogram to all Army family members. Psychologists andthe U.S. Army are collaborating to enhance the resilienceand well-being of military family members. This project isbased on the premise that family members play an impor-tant role in the soldier’s performance, resilience, and well-being. Parallel to the CSF for soldiers, the family CSFprogram will include both assessment and program mod-ules built on a strengths-based approach.
The Global Assessment Tool for families, now underdevelopment, measures a person’s strengths and problemsin four life domains: emotional, social, familial, and spir-itual (Peterson et al., 2011). The contents of assessment andtraining modules for families are designed to address bothcommon personal and family-related issues with specialattention to unique challenges and experiences faced bymilitary families. The assessment tool is planned to beavailable through a military website for family members,and the outcome will be confidential. Upon completion ofthe survey, participants will receive instant feedback onstrengths and issues in each life domain. Depending on theresults, tailored information and various training modules,from self-development online programs to more intensivegroup or personal interventions, will be made available.
At this early stage of the project, the target partici-pants are adults in the military family—spouses or care-takers of military children. Strengths and problems amongmilitary children will be measured by the caretaker’s re-port, and separate training modules are planned to provideadults with tools to promote the resilience and well-beingof military children. A larger community of military familymembers will be reached in an efficient and cost-effectiveway with computer technology in conjunction with otherstrategies to deliver assessment and programs (Gottman etal., 2011). The family component of the CSF program hasjust begun. The initiative will be revised on the basis of theresults of ongoing research and evaluation. It is conceiv-able that in the future, additional direct assessment andprograms for military children will be added to the CSFprogram.
ConclusionThroughout history, military children and families haveshown great capacity to adapt to and grow from challenges,during peace or during war. However, with U.S. involve-ment in current wars, military families face multiple chal-lenges that put them at high risk of distress and mentalhealth problems. Their needs are greater than ever. Thewell-being of military children and families is desirable in
70 January 2011 ● American Psychologist

its own right and as a means to many other valued ends, forindividuals and the larger society.
There is an urgent need for better understanding ofboth the challenges and the strengths and assets of militarychildren and families to help them not only survive but alsothrive. Studies and programs need to take a comprehensiveapproach that is strengths based and problem focused.Studies and programs must focus not just on the individualbut also on larger social contexts. We need more high-quality research and more evidence-based programs. Pro-grams need to be rigorously evaluated and better dissemi-nated to reach all those who are in need. Current efforts toexpand the CSF program to military family members areanother example of a systematic collaboration betweenpsychology and the military to achieve the goal of ahealthy, resilient, and productive military community.
Psychology as a field is in a unique position to ac-complish all of these goals (Seligman & Fowler, 2011).Military children and families deserve sustained attentionfrom psychology. One hopes that more psychologists willjoin and indeed help lead this worthy endeavor. About onethird of the population has a direct relationship with some-one in the military, and virtually everyone has an indirectrelationship (Black, 1993). Military families live in ourneighborhoods. Their children go to our schools. Much canbe learned from them. Building and sustaining healthy,resilient, and thriving military children and families willbring benefits not just to them but ultimately to all Amer-icans. The military family is the American family.
REFERENCES
Amato, P. R., Booth, A., Johnson, D. R., & Rogers, S. J. (2007). Alonetogether: How marriage in America is changing. Cambridge, MA:Harvard University Press.
American Psychological Association, Presidential Task Force on MilitaryDeployment Services for Youth, Families, and Service Members.(2007). The psychological needs of U.S. military service members andtheir families: A preliminary report. Washington, DC: American Psy-chological Association.
Bank, S., & Kahn, M. (1982). The sibling bond. New York, NY: BasicBooks.
Barnes, V. A., Davis, H., & Treiber, F. A. (2007). Perceived stress, heartrate, and blood pressure among adolescents with family membersdeployed in Operation Iraqi Freedom. Military Medicine, 172, 40–43.
Black, W. G. (1993). Military-induced family separation: A stress reduc-tion intervention. Social Work, 38, 273–280.
Bowen, G. L., Mancini, J. A., Martin, J. A., Ware, W. B., & Nelson, J. P.(2003). Promoting the adaptation of military families: An empirical testof a community practice model. Family Relations, 52, 33–44. doi:10.1111/j.1741-3729.2003.00033.x
Chandra, A., Burns, R. M., Tanielian, T., Jaycox, L. H., & Scott, M. M.(2008). Understanding the impact of deployment on children and fam-ilies: Findings from a pilot study of Operation Purple Camp partici-pants [Working paper]. Santa Monica, CA: Rand Corporation.
Chandra, A., Lara-Cinisomo, S., Jaycox, L. H., Tanielian, T., Burns,R. M., Ruder, T., & Han, B. (2010). Children on the homefront: Theexperience of children from military families. Pediatrics, 125, 16–25.
Conroy, P. (1991). Introduction. In M. E. Wertsch, Military brats: Leg-acies of childhood inside the fortress (p. xix–xxvii). St. Louis, MO:Brightwell.
Cornum, R., Matthews, M. D., & Seligman, M. E. P. (2011). Compre-hensive soldier fitness: Building resilience in a challenging institutionalcontext. American Psychologist, 66, 4–9. doi:10.037/a0021420
Cozza, S. J., Chun, R. S., & Polo, J. A. (2005). Military families and
children during operation Iraqi Freedom. Psychiatric Quarterly, 76,371–378. doi:10.1007/s11126-005-4973-y
Croan, G. M., Levine, C. T., & Blankinship, D. A. (1992). Familyadjustment to relocation (Technical Report No. 968). Alexandria, VA:U.S. Army Research Institute for the Behavioral and Social Sciences.
Department of Defense reaches out to children of soldiers. (2009, October22). U.S. Medicine. Retrieved from http://www.usmedicine.com/articles/Department-of-Defense-Reaches-Out-to-Children-of-Soldiers.html
Engel, R. C., Gallagher, L. B., & Lyle, D. S. (2010). Military deploymentsand children’s academic achievement: Evidence from Department ofDefense education activity schools. Economics of Education Review,29, 73–82.
Feldman, D. C., & Tompson, H. B. (1993). Expatriation, repatriation, anddomestic geographical relocation: An empirical investigation of adjust-ment to new job assignments. Journal of International Business Stud-ies, 24, 507–529. doi:10.1057/palgrave.jibs.8490243
Flake, E. M., Davis, B. E., Johnson, P. L., & Middleton, L. S. (2009). Thepsychosocial effects of deployment on military children. Journal ofDevelopmental and Behavioral Pediatrics, 30, 271–278. doi:10.1097/DBP.0b013e3181aac6e4
Frame, M. W., & Shehan, C. (1994). Work and well-being in the two-person career: Relocation stress and coping among clergy husbands andwives. Family Relations, 43, 169–205. doi:10.2307/585323
Fry, P. S. (1997). Grandparents’ reactions to the death of a grandchild: Anexploratory factor analysis. Omega: Journal of Death and Dying, 35,119–140.
Gottman, J. M., Gottman, J. S., & Atkins, C. (2011). The ComprehensiveSoldier Fitness program: Family skills component. American Psychol-ogist, 66, 52–57. doi:10.1037/a0021706
Hall, L. K. (2008). Counseling military families: What mental healthprofessionals need to know. New York, NY: Routledge.
Hammer, L. B., Cullen, J. C., Marchand, G. C., & Dezsofi, J. A. (2006).Reducing the negative impact of work-family conflict on militarypersonnel: Individual coping strategies and multilevel interventions. InC. A. Castro, A. B. Adler, & T. W. Britt (Eds.), Military life: Thepsychology of serving in peace and combat (Vol. 3, pp. 220–242).Westport, CT: Praeger Security International.
Hays, J. C., Gold, D. T., & Pieper, C. F. (1997). Sibling bereavement inlate life. Omega: Journal of Death and Dying, 35, 25–42.
Hefling, K. (2009). Siblings of troops often are forgotten mourners.Retrieved October 21, 2009, from http://www.armytimes.com/news/2009/09/ap_military_grieving_siblings_092409/
Huebner, A. J. (2010, January). Impact of deployment on children andfamilies: Recent research updates. Presentation at the National GuardProfessional Development Conference: Family Program ProfessionalDevelopment, Orlando, FL.
Huebner, A. J., Mancini, J. A., Bowen, G. L., & Orthner, D. K. (2009).Shadowed by war: Building community capacity to support militaryfamilies. Family Relations, 58, 216–228. doi:10.1111/j.1741-3729.2008.00548.x
Hutchinson, J. W. (2006). Evaluating risk-taking behaviors of youth inmilitary families. Journal of Adolescent Health, 39, 927–928. doi:10.1016/j.jadohealth.2006.05.015
Jeffreys, D. J., & Leitzel, J. D. (2000). The strengths and vulnerabilities ofadolescents in military families. In J. A. Martin, L. N. Rosen, & L. R.Sparacino (Eds.), The military family: A practice guide for humanservice providers (pp. 225–240). Westport, CT: Praeger.
Jensen, P. S., Gordon, G. A., Lewis, R. L., & Xenakis, S. N. (1986). Themilitary family in review: Context, risk, and prevention. Journal of theAmerican Academy of Child Psychiatry, 25, 225–234. doi:10.1016/S0002-7138(09)60230-2
Jensen, P. S., Grogan, D., Xenakis, S. N., & Bain, M. W. (1989). Fatherabsence: Effects on child and maternal psychopathology. Journal of theAmerican Academy of Child and Adolescent Psychiatry, 28, 171–175.doi:10.1097/00004583-198903000-00004
Jensen, P. S., & Shaw, J. A. (1996). The effects of war and parentaldeployment upon children and adolescents. In R. J. Ursano & A. E.Norwood (Eds.), Emotional aftermath of the Persian Gulf War: Veter-ans, families, communities, and nations (pp. 83–109). Washington, DC:American Psychiatric Press.
Jensen, P. S., Xenakis, S. N., Wolf, P., & Bain, M. W. (1991). The
71January 2011 ● American Psychologist

“military family syndrome” revisited: “By the numbers.” Journal ofNervous and Mental Disease, 179, 102–107. doi:10.1097/00005053-199102000-00007
Kenny, J. A. (1967). The child in the military community. Journal of theAmerican Academy of Child Psychiatry, 6, 51–63. doi:10.1016/S0002-7138(09)61289-9
Lagrone, D. M. (1978). The military family syndrome. American Journalof Psychiatry, 135, 1040–1043.
Lester, P. B., McBride, S., Bliese, P. D., & Adler, A. B. (2011). Bringingscience to bear: An empirical assessment of the Comprehensive SoldierFitness program. American Psychologist, 66, 77–81. doi:10.1037/a0022083
MacDermid, S. M. (2006). Multiple transitions of deployment and reunionfor military families. Retrieved from the Military Family ResearchInstitute, Purdue University website: http://www.cfs.purdue.edu/mfri/DeployReunion.ppt
Manning, D. T., Balson, P. M., & Xenakis, S. N. (1988). Prevalence oftype A behavior in American combat soldiers and their children. Mil-itary Medicine, 153, 358–360.
Marchant, K. H., & Medway, F. J. (1987). Adjustment and achievementassociated with mobility in military families. Psychology in theSchools, 24, 289–294. doi:10.1002/1520-6807(198707)24:3�::AID-PITS2310240315�3.0.CO;2-A
Mental Health Advisory Team 6. (2009, November 6). Mental HealthAdvisory Team (MHAT) 6 Operation Enduring Freedom 2009 Afghan-istan (Report chartered by the Office of the Command Surgeon USForces Afghanistan (USFOR-A) and Office of the Surgeon GeneralUnited States Army Medical Command). Retrieved from http://www.armymedicine.army.mil/reports/mhat/mhat_vi/MHAT_VI-OEF_Redacted.pdf
Military Child Education Coalition. (2001). United States Army secondaryeducation transition study. Arlington, VA: Military Family ResourcesCenter.
Morrison, J. (1981). Rethinking the military family syndrome. AmericanJournal of Psychiatry, 138, 354–357.
Moss, M. S., Moss, S. Z., & Hansson, R. O. (2001). Bereavement and oldage. In M. S. Stroebe, R. O. Hansson, W. Stroebe, & H. Schut (Eds.),Handbook of bereavement research: Consequences, coping, and care(pp. 241–260). Washington, DC: American Psychological Association.doi:10.1037/10436-010
O’Connell, P. V. (1981). The effect of mobility on selected personalitycharacteristics of ninth and twelfth grade military dependents (Unpub-lished doctoral dissertation). University of Wisconsin, Milwaukee.
Paden, L. B., & Pezor, L. J. (1993). Uniforms and youth: The militarychild and his or her family. In F. W. Kaslow (Ed.), The military familyin peace and war (pp. 3–24). New York, NY: Springer.
Palmer, C. (2008). A theory of risk and resilience in military families.Military Psychology, 20, 205–217. doi:10.1080/08995600802118858
Park, N. (2004). Character strengths and positive youth development.Annals of the American Academy of Political and Social Science, 591,40–54. doi:10.1177/0002716203260079
Park, N. (2009). Building strengths of character: Keys to positive youthdevelopment. Reclaiming Children and Youth, 18, 42–47.
Park, N., & Peterson, C. (2006). Moral competence and character
strengths among adolescents: The development and validation of theValues in Action Inventory of Strengths for Youth. Journal of Adoles-cence, 29, 891–910.
Park, N., & Peterson, C. (2008). Positive psychology and characterstrengths: Application to strengths-based school counseling. Profes-sional School Counseling, 12, 85–92.
Park, N., Peterson, C., & Brunwasser, S. M. (2009). Positive psychologyand therapy. In N. Kazantzis, M. A. Reinecke, & A. Freeman (Eds.),Cognitive and behavioral theories in clinical practice (pp. 278–306).New York, NY: Guilford Press.
Peterson, C., & Park, N. (2003). Positive psychology as the evenhandedpositive psychologist views it. Psychological Inquiry, 14, 141–146.
Peterson, C., Park, N., & Castro, C. A. (2011). Assessment for the U.S.Army Comprehensive Soldier Fitness program: The Global AssessmentTool. American Psychologist, 66, 10–18. doi:10.1037/a0021658
Pincus, S. H., House, R., Christensen, J., & Adler, L. E. (2001). Theemotional cycle of deployment: A military family perspective. Journalof the Army Medical Department, 4/5/6, 615–623.
Rando, T. (1986). Death of the adult child. In T. Rando (Ed.), Parentalloss of a child (pp. 221–238). Champaign, IL: Research Press.
Rohall, D. E., Segal, M. W., & Segal, D. R. (1999). Examining theimportance of organizational supports on family adjustment to militarylife in a period of increasing separation. Journal of Political andMilitary Psychology, 27, 49–65.
Segal, D. R., & Segal, M. W. (2004). America’s military population.Population Bulletin, 59, 1–40.
Seligman, M. E. P., & Fowler, R. D. (2011). Comprehensive SoldierFitness and the future of psychology. American Psychologist, 66, 82–86. doi:10.1037/a0021898
Shaw, J. A. (1979). Adolescents in the mobile military community. InD. X. Freedman et al. (Eds.), Adolescent psychiatry (Vol. 7, pp. 191–198). Chicago, IL: University of Chicago Press.
Shinseki, E. K. (2003). The Army family (White paper). Retrieved fromhttp://www.whs.mil/library/Dig/AR-M620U_20080912.pdf
U.S. Department of Defense, Defense Manpower Data Center. (2008).The changing profile of the Army 1985-2008. Alexandria, VA: Author.
U.S. Department of Defense, Defense Manpower Data Center. (2009a).Reserve components: Noble Eagle/Enduring Freedom/Iraqi Freedom.Alexandria, VA: Author.
U.S. Department of Defense, Defense Manpower Data Center. (2009b).2008 surveys of military spouses: Impact of deployments on spousesand children. Alexandria, VA: Author.
Watanabe, H. K. (1985). A survey of adolescent military family members’self-image. Journal of Youth and Adolescence, 14, 99–107.
Wertsch, M. E. (1991). Military brats: Legacies of childhood inside thefortress. St. Louis, MO: Brightwell.
Wiens, T. W., & Boss, P. (2006). Maintaining family resiliency before,during, and after military separation. In C. A. Castro, A. B. Adler, &T. W. Britt (Eds.), Military life: The psychology of serving in peace andcombat (Vol. 3, pp. 13–38). Westport, CT: Praeger Security Interna-tional.
Zoroya, G. (2009, June 25). Troops’ kids feel war toll. USA Today.Retrieved from http://www.usatoday.com/news/military/2009-06-24-military-kids_N.htm
72 January 2011 ● American Psychologist

Screening for ACEs at Walter Reed
Our pediatric medical home screens for ACEs! Over the past year, we screened 38% of 4 year-olds at well-child visits. Over the next academic year, the Red and Blue team clinic PI project goal is to increase screening rates to 75% AND expand screening to include 2- and 3-year well-child visits.
Here's how to complete the screen for your patients:
1. The family should receive the following ACE-Q handout at check-in. The familywrites down the number of adverse events the child has experienced.
2. Add the total of the numbers recorded in the two boxes. This is the ACE score.3. Your screener should document the ACE score in the vitals section along with
hearing and vision screen. Be sure to review the hard-copy questionnaire if thescore is >1 or is not documented in the vitals section.
4. Management of ACE score is as follows:a. Score 0
i. Continue with regular well child check anticipatory guidance
b. Score 1-3
i. Ask if the parent is concerned about or sees any relationship
between the ACEs they have identified and their child’s mental or
physical health.
1. Yes - Code 'Problem related to upbringing, unspecifiedZ62.9' in A/P and refer to Dr. Elmore (WRB Pediatrics ClinicHealth Psychologist)
a. Order consult: 'Behavioral Health MTF BE'. In 'Reasonfor Request' specify that patient is referred toDr. Elmore. Consider including 'positive ACE screen' inyour referral comment.
2. No – Ensure ACE score documented in vitals section andcontinue with regular well child check anticipatory guidance
c. Score ≥4
i. Code 'Problem related to upbringing, unspecified Z62.9' in A/Pii. Refer to Dr. Elmore as aboveiii. CONSIDER: Social Work and Case Management Consults
iv. Ensure ACE score is recorded in vitals section
A note: Using this screen, it is not necessary for them to disclose which events have been experienced. Families should always be invited to discuss further, however a desire for privacy should not prevent an appropriate referral to Dr. Elmore to provide appropriate support.

CYW Adverse Childhood Experiences Questionnaire (ACE-Q) Teen Self-Report
CYW ACE-Q Teen SR (13-19 yo) © Center for Youth Wellness 2015
Today’s Date: _____________________________________
Your Name: ______________________________________________________ Date of birth: _____________________________________
Many children experience stressful life events that can affect their health and development. The results from this questionnaire will assist your doctor in assessing your health and determining guidance. Please read the statements below. Count the number of statements that apply to you and write the total number in the box provided.
Please DO NOT mark or indicate which specific statements apply to you.
1) Of the statements in section 1, HOW MANY apply to you? Write the total number in the box.
2) Of the statements in section 2, HOW MANY apply to you? Write the total number in the box.
Section 1. At any point since you were born…
§ Your parents or guardians were separated or divorced
§ You lived with a household member who served time in jail or prison
§ You lived with a household member who was depressed, mentally ill or attempted suicide
§ You saw or heard household members hurt or threaten to hurt each other
§ A household member swore at, insulted, humiliated, or put you down in a way that scaredyou OR a household member acted in a way that made you afraid that you might bephysically hurt
§ Someone touched your private parts or asked you to touch their private parts in a sexual waythat was unwanted, against your will, or made you feel uncomfortable
§ More than once, you went without food, clothing, a place to live, or had no one to protect you
§ Someone pushed, grabbed, slapped or threw something at you OR you were hit so hard thatyou were injured or had marks
§ You lived with someone who had a problem with drinking or using drugs
§ You often felt unsupported, unloved and/or unprotected
Section 2. At any point since you were born…
§ You have been in foster care
§ You have experienced harassment or bullying at school
§ You have lived with a parent or guardian who died
§ You have been separated from your primary caregiver through deportation or immigration
§ You have had a serious medical procedure or life threatening illness
§ You have often seen or heard violence in the neighborhood or in your school neighborhood
§ You have been detained, arrested or incarcerated
§ You have often been treated badly because of race, sexual orientation, place of birth,disability or religion
§ You have experienced verbal or physical abuse or threats from a romantic partner (i.e.boyfriend or girlfriend)
To be completed by Patient

Toxic Stress and Adverse Childhood Experiences Continuity Module Quiz
1. Define the following:
● Positive stress response
Positive stress responses are a normal and essential part of healthy development. It is
characterized by brief increases in heart rate and blood pressure, as well as mild elevations in
hormonal levels. When children are exposed to a stressor as part of their development, such as
the first day of daycare or receiving vaccines, the presence of a caring relationship with an adult
provides a protective effect that helps them cope with the stressor after the initial activation.
The physiological stress response shuts down through negative feedback once the child is no
longer exposed to the stressor.
● Tolerable stress response
It involves exposure to a non-normative experience that presents a greater magnitude of
adversity or threat (ex. death of an immediate family member, involvement in a natural disaster).
The magnitude and duration of the stress response is reduced when the child is supported by
caring adults, which allows the child to return to baseline status.
● Toxic stress response
Toxic stress responses occur with intense, frequent, or prolonged adversity. Disruption of brain
architecture and other organ systems can be seen during these responses, and can lead to an
increased risk of stress related disease and cognitive impairment.
2. What are the 7 adverse childhood experiences assessed in the ACEs study?
● Abuse
○ Psychological
○ Physical
○ Sexual
● Neglect
○ Physical
○ Emotional
● Household dysfunction
○ Substance abuse
○ Mental illness
○ Parent treated violently
○ Criminal behavior in household
○ Divorce/separation

3. Name some military-specific adverse childhood experiences.
○ PCS moves
○ Deployment
○ Wounded warrior parent
○ Parental death during deployment
4. What does toxic stress do the developing brain?
Our stress response is developed for short term threats
requiring brief bursts of energy. An over-activated HPA
response can develop secondary to chronic stressors,
which can then lead to many long term consequences
affecting both the brain and gene expression, and can
also lead to future risky behaviors and chronic disease.
Toxic stress can negatively impact processing of
emotions, working memory, active learning, decision
making, impulse control, and judgement.
It can also cause epigenetic changes that can be
passed down from generation to generation. These
changes can be reversible if interventions are made
early.
A child who experiences toxic stress may be more
reactive to even mildly adverse experiences and less capable of effectively coping with future
stress.
5. The ACEs study showed that the consequences of toxic stress are not limited to mental
health issues. What are some examples of these lifelong effects of toxic stress?
● Mental Health
● Obesity
● Drug and alcohol use
● Smoking
● Heart disease
● Cancer
● Stroke
● Diabetes
● Chronic bronchitis and emphysema

6. How can you prevent the consequences of adverse childhood experiences and toxic stress?
● Screening and early intervention
● Creating stable and caring relationships with adults
● Resiliency
7. What is resiliency?
● Process by which the child moves through a traumatic event, utilizing various protective
factors for support, and returning to “baseline” in terms of an emotional and physiologic
response to the stressor
● Protective factors include parental resilience, social connections, concrete/tangible help
in times of need, parent knowledge of child development, and social and emotional
competence of the child

Toxic Stress and Adverse Childhood Experiences Continuity Module Cases
1. Annalise is a 13 year old female who has two older brothers and two younger sisters.
Her mother started using drugs and alcohol when Annalise was 4 years old and her father is not
in the picture. Oftentimes Annalise would have to ask her friends at school for food because her
family didn’t have enough food at home to feed everyone. She and her two younger sisters
were recently placed in a foster home this month.
Identify the ACE risk factors in this child’s situation:
● Maternal drug use
● Food insecurity
● Foster home stay
● Single parent home
What can her foster family do to help build resiliency in Annalise?
● Build strong positive relationships with a supportive parent, caregiver, or other adult
● Mobilize sources of faith, hope, and cultural traditions
2. You are seeing three siblings, ages 12, 7, and 3 years, as new patients in your practice.
They come to the office with their mother who reports that they all need physicals to start at a
new school. When you take their social history, their mother tearfully reports that it’s been a
difficult year. She and the children left their physically abusive father several months ago. They
have moved several times to stay with friends, and have just moved to town to stay with her
sister. She reports that she has had difficulty finding work, and that money is tight. She has had
difficulty finding childcare for her youngest child, and she is worried about the older children
starting at a new school in the middle of the academic year. She asks what advice you can give
to help them with the transition.
What age-appropriate manifestations of stress might you see in each child?

What are some resources in the military that you can offer to their mother?
Fleet and Family Services
Army Community Services
Family Advocacy Program
School Liaison Officer
Crisis Support
Clinical Counseling
http://www.militaryonesource.mil/
Behavioral Health consult
Social Work consult
3. You see a 2 year old male, Adrian. He is your last patient of the day. He is accompanied by
his mother and grandmother and this is his first time in the Pediatrics Clinic. He and his mother
recently moved into his grandmother’s home due to conflict between his mother and father. He
was born to a 20 year old active duty Army mother. He was born at 35 weeks EGA and
weighed 1.9kg at birth (SGA). You look through his medical record and notice that his
immunizations are only up to date until 6 months. His mother and father are married and his
active duty Army father recently returned from deployment about six months ago. His father was
recently arrested last month for drug possession. His mother reports that she has been very
withdrawn lately and does not have the motivation to take care of Adrian, so Adrian’s
grandmother has been stepping in more to help out.
What effects might the stressors in Adrian’s home have on his brain development?

What are some lifelong health consequences that Adrian is at risk for?
How do you think the stressors in Adrian’s home affected his mother’s ability to parent?
It has had a negative impact on her ability to parent. It has made his mother more withdrawn or
distracted and which has gotten in the way of her taking him in to the pediatrician to get Adrian’s
immunizations completed.
How can Adrian’s pediatrician intervene to help prevent these lifelong consequences on
Adrian’s health?
Screening for toxic stress at all well child visits
Referral to local resources, behavioral health, family counseling
Establishing a caring and open relationship with parent and child
Educating Adrian’s mother on adverse childhood experiences and toxic stress and its
negative impact on Adrian’s health going forward

4. Two siblings, a 4 year-old boy and 8 year-old girl, are in your office for well-child exams. After
their exams, their father mentions that the children’s mother will be deploying to Afghanistan in a
month. This will be her second deployment in three years, and she is expected to be overseas
for 9 months. The father says that younger child does not remember his mother’s last
deployment, but that his older daughter was very anxious and had difficulty starting school. The
father is concerned about how this upcoming deployment may affect his children, and he asks
what he can do at home to reduce the stress of separation.
Do you think this situation represents positive, tolerable, or toxic stress? Why? What
factors might change how this stressful situation is experienced by the children?
It could be any of the three! It most likely represents a tolerable stressor, as a non-normative
experience with the child receiving guidance in coping with stress from a trusted adult. If the
family lives and is well-connected in a large military community, this could even be considered a
normative experience within a community that provides many supports for stress-management.
This situation also has the potential to represent toxic stress to these children, depending on
how their father and other trusted adults help them to respond to physiologic manifestations of
stress. If support is lacking, the children may experience toxic stress.
How might the 4 year-old boy react to separation from his mother? What advice can you
offer to reduce the stress of deployment?
Approximately 1/3 of school-age children show psychosocial difficulties during parental
deployment (2.5 times the rate of civilian populations). Older youth and girls are more likely to
report problems with school, family, and mental health. Evidence suggests that multiple and
prolonged deployments are more likely to negatively affect children. Some potential effects
include:
- poor academic performance
- behavior problems
- symptoms of depression
- symptoms of anxiety
What advice can you offer to help her cope with this separation?
Families that function most effectively are active, optimistic, self-reliant, and flexible. Encourage
the father to frame the challenges of separation as positively as possible. Help the child to
identify reliable friends, neighbors, and family members who understand the situation and can
provide emotional support. For the older child, especially, this presents an opportunity to take on
household responsibilities, develop a degree of independence, and demonstrate maturity.
Encourage the father to specifically acknowledge these actions as the child’s role in the whole
family’s service to the country, fostering a sense of purpose and pride.
Images from this module can be found in Center For Youth Wellness ACE-Q User Guide for Health Professionals and the American Academy of
Pediatrics SOPT’s Advocacy Campaign’s Partnering for Resilience: Learn, Empower, and Connect to Address Toxic Stress Resident Presentation