Musculoskeletal Pain and Pregnancy
Transcript of Musculoskeletal Pain and Pregnancy

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 1/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 1
Musculoskeletal pain and pregnancy
Eugen Ancuta
MD, PhD, MSC
Research Department„Cuza-Voda” Obstetrics and Gynecology Hospital
Iasi, Romania
I. Musculoskeletal conditions during pregnancy
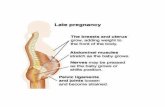
As many women gain weight during the third trimester of pregnancy there is an increase in
force on joints and soft tissues resulting in musculoskeletal pain. It has been suggested that
this pains will continue and may be aggravated by prolonged postures or even daily
activities.
Repetitive injury to the disc can compromises spinal integrity. A conglomerate of anatomical
changes including hyperlordosis, hyperextension of the knees and a hyperkyphosis can be
noted.
Estrogen, progesterone and relaxin cause global relaxation to the ligaments and muscles in
the pregnant women. Many times the increase in ligament mobility and loss of muscle tone
that creates hypermobility in the spinal segment can irritate an existing condition or develop
a injury to the ligaments muscles.
Causes of musculoskeletal pain include: auto accidents, fractures, sprains, dislocations orpostural strain, repetitive movements, prolonged immobilization etc.
Pregnancy is a time of changes in the musculoskeletal system. These changes can develop a
variety of problems including: low back pain, pelvic pain, leg cramps, carpal tunnel
syndrome, de Quervain tenosynovitis or transient osteoporosis. Therefore, preexisting
musculoskeletal problems such as rheumatoid arthritis or previous low back pain also
contribute to the musculoskeletal symptoms of pregnancy but with greater frequency.
The reported incidence of these conditions is less than 70 % of pregnant women.
Low back pain is not correlated with maternal weight or fetal size.
Changes in sacroiliac joints and pubic symphysis width less than 1 cm have been considerednormal in pregnant women.
Rupture of the pubic symphysis (diastasis) can be associated with severe pain.
Treatment includes acetaminophen 0.5 to 1 gram orally, 6-hourly as necessary, up to
maximum dose of 4 grams daily.
Also pelvic pain can occur up to several years and the treatment of posterior pelvic pain,
diastasis or persistence of sacroiliac joint is predominantly conservative. Surgical fixation in
diastasis greater than 3 cm can be used.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 2/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 2
Leg cramps is often exacerbated in the second and third trimester and occur in up to 30% of
pregnant women.
Pre-pregnancy fitness and maintaining adequate hydration may be beneficial.
Treatment options include calcium carbonate 1.5 grams (elemental calcium 600 mg) orally,
daily. Also magnesium supplements can be used with no significant benefit.
Carpal tunnel syndrome has been reported in up to 20% cases of pregnant women. It occurs
more commonly later in life, especially around menopause. Injections of corticosteroid may
provide symptomatic relief in pregnancy but can be used only if the symptoms are severe
during breastfeeding. Decompressive surgery during pregnancy should be avoided if
possible.
De Quervain tenosynovitis mostly occurs in postpartum than in pregnancy and usually affect
the tendons of abductor pollicis longus and extensor pollicis.
Local infiltration of 1 ml of lignocaine (1%) premixed with corticosteroid(methylprednisolone or betamethasone) can be used during breastfeeding. Resting the
thumb is effective to reduce pain but is difficult at this time. Moreover, the use of NSAID
drugs may be effective temporary.
Transient osteoporosis of pregnancy can occur in the third trimester and usually affects the
hip. The reported incidence of this condition is reduced than the asymptomatic physiological
loss of bone mass that occurs during pregnancy and lactation.
Pregnant women with significant hip pain should be referred for rheumatologist
assessment. Bisphosphonates should be avoided in pregnancy.
II. Postpartum depression and fatigue
Mother with postpartum depression may be at an increased risk of spinal injury. Those who
had a career find that they may lose touch with collegues and social calendar events.
Therefore clinicians can suggest them to stay active in their health.
Women with downward head tilt, a flexed cervical spine and rounded shoulders can give
way to recognize a potentially depressed subject.
Patients who are primiparid may find that after cesarean delivery they have had to resume
their regular activities. Postpartum depression can also be associated with issues of weight.
Clinicians can guide them to join healthy weight loss program that will restore health and
aid in weight management. As a support for weight control they should be referred to their
physician for full blood chemistry to include a thyroid panel and cancer.
The most important aspect to recovery is the assistance of family and friends.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 3/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 3
Moms should be advised to supplement their diet with multivitamins and essential fatty
acids vitamins because nutritional compromise can cause fatigue or exacerbate an existing
condition of fatigue. Other nutritional support may be indicated to prevent fatigue (anemia
or thyroid dysfunction): B-Complex vitamin, Co Q10 supplements and Iron supplements.
Patients should be advised to acquire as much sleep as possible.
As the re-setting of hormones to a non-gravid state for new mothers, the patient may
experience low back and sacral pain, but the most profound affect can be to the thoracic
spine.
There are factors that contribute to postpartum musculoskeletal pain including: engorged
breast tissue, rounded shoulder position and ergonomic compromises seen with lifting or
carrying newborn.
Also phone use while carrying the newborn causes excessive contraction of the muscles of
the cervical spine. These postural changes cause cervical pain. Patients should be educated
to switch arms or can use many devices available at stores that are designed to support
proper ergonomics to mothers.
III. Prevention and enhanced care
Mothers/Caregivers who engage in the repetition of removing the entire car seat with child
is exposed to biomechanical stress to the spine. Educate patients to remove the infant
within the car seat. At this time they should pull the seat as close as possible to their body.
Removing the newborn from the baby bathtub can create postural compromises that can
insult the integrity of the lumbar and thoracic spine. To avoid musculoskeletal pain the
newborn should be held close to the body. Employ mothers to take the time to do
rehabilitative exercises. These can assist in the reduction of the disc, zygapohyseal joint and
muscular injury.
Patients can also use play pens when them needs to be „hand -free”. Outward stretchedarms can compromise the thoracic spine. To accommodate the extra weight the child is
place down into the play pens while the mother is in a flexed position. To avoid back
injuries, the adult caregiver can lowering one of the side bars. This create a repetitive strain
on the upper and middle trapezious muscle rhomboids and levator scapular muscles. Viable
alternatives exist for caregivers in order to maintain joint mobility and spinal integrity. To
accommodate the extra weight check for leg inequality, hypertonic erector spinae muscles
trigger points in the quadratus lumborum muscles, myofascial trigger points and hypertonic
rhomboids, levator scapulae and cervical muscles. Chronic shortening of the lumbar muscles
with an increase in the lumbar lordosis in pregnancy should be receiving as much attention.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 4/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 4
Talking wireless phone while carrying a child, parents are free to move about and
accomplish tasks around the house. In addition, focused history can turn into an educational
consult.
Advise patients to opt for the carrier that maximizes spinal integrity and to look for a stroller
with handles that are high enough in order to avoid hunching.
IV. Women physiology and its concern to physical exercise
Recreational physical fitness such as running and varied aerobics help to facilitate the goal
of muscle tone. There are some differences between men and women: they have a
comparably smaller sized thorax, cardiac muscle and the total red cells, hemoglobin and
hematocrite concentration average are approximately 6%, 10% respectively and peak bone
density is less than the bone density seen in men of the same age. All these factors may
hinder exercise performance. Therefore, weight equipment has been designed to
accommodate a male physique.
V. Knees, shoulders and foots injuries
Imbalance between quadriceps and hamstring muscles, altered biomechanics from an
increased quadriceps angle and pronation or improper shoes are the foundation to these
injuries.
Clinically, mothers can present limb and spinal mal-alignment. Restoration of kinesiology
should include orthotics, strengthening of the quadriceps, stretching and strengthening the
hamstrings and correction of foot alignment.
Ligament laxity affect female during pregnancy and has been suggested as predisposing
them to injury. Injury rates to the knees have been found to be greater in women with wide
pelvis, increased femoral anteversion and increased valgus of the knees.
Footwear with high heels can accentuate pressure on the metatarsal heads and inter-
segmental spinal dysfunctions can appear. Clinically these patients should complain of low
back pain, neck or hip pain. Orthotic foot wear would be recommended.
Pregnant women involved in excessive exercise can developed shoulder injuries. These
exercise may be accomplish by upward and anterior migration of the humeral head in the
fossa with not enough space in forward flexion. Simple remedies to these habits would be to
encourage women to join a rehabilitative program that includes gleno-humoral joint and
cervical spine.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 5/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 5
As well as female change physiologically and anatomically during pregnancy, clinicians
should encourage them to maintain proper posture as often as possible. Educating pregnant
women regarding posture may prevent myofascial pain and spinal joint dysfunction. Women
should pay attention to bend their knees or hold the child close to the body when lifting
weights.
Researchers also noted a direct relationship between excessive foot pronation and injury of
the anterior cruciate ligament.
IV. Management of the rheumatic illnesses during pregnancy
The clinical management of pregnancy complicated by rheumatic illnesses as systemic lupus
erythematosus, antiphospholipid syndrome, rheumatoid arthritis, scleroderma, juvenile
idiopathic arthritis or spondyloarthropathy depends on both fetal and maternal factors.
Clinicians have suggested that assessment of anti-DNA, antiphospholipid, anti-SSA/Ro, anti-
SSB/La, RNP antibodies and ESR level can be used. Also, in antiphospholipid syndrome
measurements of anticardiolipin antibodies (high titer >40 IU of IgM or IgG), anti-beta2-
glycoprotein1 (present for at least 12 weeks), lupus anticoagulant test, proteinuria and
thrombocytopenia may be usefull.
A diagnosis of rheumatoid arthritis, scleroderma or juvenile arthritis depends on clinical
grounds alone.
Systemic lupus erythematosus during pregnancy can include musculoskeletal manifestations
as arthralgia or myalgia and vascular, hematological, renal or myocardial disorders. The
injuries sites are located in proximal interphalangeal joints, metacarpal phalangeal joints
and the knees. Patients can often suffer from cramping, diarrhea or vomiting resultant
mostly from vasculitis of the intestines. Also can suffer from sudden death, arrhythmias or
cardiac failure from pericarditis. Other clinical signs may include pleurisy or pleural effusion.
The re-setting of hormones to a non-gravid state can reduce musculoskeletal pain, fatigue
and other signs.
When diagnosing SLE, there are certain criteria that must be met. Most important to the
pregnant women is to adopt a multidisciplinary approach.
Patients should be referred to their gynecologist and rheumatologist for evaluation.
Monitoring of SLE consists of ultrasound evaluation of the fetal growth rate and placental
volume. Establishing a diagnosis of SLE flare requires a new or increasing of anti-dsDNA
antibody.
A diagnosis of neonatal lupus syndrome include a high-titer anti-Ro/SSA or anti-La/SSB
antibodies in neonates. Mothers may develop severe preeclampsia or HELLP syndrome.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 6/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 6
Diagnosing congenital complete heart block requires ultrasonography between 18 and 24
weeks of gestation. Monitoring fetal heart rate show spontaneous bradycardia, reduced
placental volume, decreased amniotic fluid or fetal death.
V. Treatment options in SLE during pregnancy
Corticosteroids may increase risk of pregnancy-induced diabetes, hypertension or
premature rupture of membranes as maternal complications and slight increase in cleft
palate or fetal growth restriction as fetal complications.
Hydroxycholoquine discontinuation during pregnancy can result in a flare of SLE.
ACE inhibitors and angiotensin receptor blockers may increased risk of oligohydramnios,
fetal growth restriction or fetal renal dysfunction in second and third trimester. Also there is
a direct relatioship between teratogenesis and ACE inhibitors or angiotensin receptor
blockers.
Evidence indicates that pregnant women with SLE are better treated with anticoagulants in
stead of anti-inflammatory drugs. Heparin or aspirin lower doses may be protective against
fetal death in SLE(antiphospholipid syndrome). Anticoagulant therapy during pregnancy is
successful and can ameliorate the discomfort associated with SLE.
Low dose aspirin has been used in order to improve pregnancy outcome by preventing
preeclampsia, hypertension, preterm birth, intrauterine growth restriction or perinatal
death (women with historical risk factors). The administration of low dose aspirin duringpregnancy is significantly related to fetal survival in patients with renal lupus. Also low dose
aspirine in the first trimester does not increase the risk of congenital malformations and in
the second and third trimester do not increase fetal side effects.
Management SLE during pregnancy include: no increase more than 25% in serum creatinin;
normal arterial blood pressure; no increase in proteinuria (more than 1g/24h); no
symptoms/signs of active SLE; normal C3 and C4 and negative anti-DNA; normal uterine and
ombelical artery doppler ultrasound at 24 weeks of gestation. Stop low dose aspirin at the
end of the 36 weeks, continue LMWH until delivery and resume warfarin after delivery, if no
obstetrical contraindications.
There is no contraindication to vaginal delivery related to SLE or treatment.
Women who took low dose aspirin during pregnancy have a lower risk of preterm delivery
than did those treated with placebo.
VI. Options for female contraception in women with SLE
Contraception includes intrauterine device, oral pill, depot medroxyprogesterone, subcutaneous
implants. Combined hormonal contraception should be avoided in female with previous thrombosisor Apl.

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 7/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 7
The need for contraception should be periodically assessed with the counselling of a dedicated team
of rheumatologists and obstetricians. The team gives the patient the opportunity to adequately
modify her treatment and to achieve a good pregnancy outcome.
VII. Cancers during pregnancy
On very rare situation, metastatic disease (breast, thyroid, cervical, kidney cancer) can also
affect the pregnant women. Patients may present musculoskeletal dysfunction. If the
musculoskeletal pain is not abated by treatment be sure to refer to an oncologist.
Selective references
1. Dahm KT, Brurberg KG, Jamtvedt G, Hagen KB.Advice to rest in bed versus advice to stay active
for acute low back-pain and sciatica.Cochrane Database Syst Rev 2010;(6):CD
2. Buchbinder R, Hayden JA, Pransky G(eds.).Back pain and non-infammatory spinal disorders (
whole journal ).Best Practice & Research Clinical Rheumatology 2010;24(2):147-298.
3. Ostensen M, Forger F.Management of RA medications in pregnant patients.Nat Rev Rheumatol
2009;5(7):382-90.
4. Marshall S, Tardif G,Ashworth N.Local corticosteroid injection for carpal tunnel
syndrome.Cochrane Database Syst Rev 2007;(2):CD001554.
5. Roux CH, Brocq O, Brevil V, Albert C, Fuller-Zeigler L.Pregnancy in Rheumatology patients
exposed to anti-tumour necrosis factor(TNF)-alpha therapy.Rheumatology (Oxford)2007;46(4):695-8.
6. Gur C, Diav-Citrin O, Shechtman S, Arnon J, Ornoy A.Pregnancy outcome after first trimester
exposure to corticosteroids: a prospective controlled study.Reprod Toxicol 2004;18(1):93-101.
7. Austalian Acute Musculoskeletal Pain Guidelines Group.Evidence-based management of acute
msculoskeletal pain: a guide for clinicians. Bowen Hills, Old:Australian Academic Press;2004.
8. Peters S, Stanley I, Rose M, Kaney S, Salomon P, A Randomized Controlled Trial of Group Aerobic
Exercise in Primary Care Patients with Persistent and Unexplained Physical Symptoms, Family
Practice Oxford University Press 2002, Vol. 19, No. 6, pp. 665-674.
9. Nicassio P, Moxham E,, Schuman C, Gevirtz R, The Contribution of Pain, reported Sleep Quality,
and Depressive Symptoms to Fatigue and Fibromyalgia, International Association for the Study
of Pain, 2002 Dec; 100 (3): 271-9
10. Ardent EA, Common Musculoskeletal Injuries in Women. Phys Sports Med. 1996; 24 (7) : 39-48
11. Fauci A., Braunwald E., Isselbacher K. Wilson J. Martin J. Kasper D. Hauser S, Longo D. Harrison’s
Principles of Internal Medicine; 14th
Edition; McGraw-Hill, Health Professions Division; 1998;
pp.562-570, 1872-1873, 2409-2419
12. Schneider M. Tender Points/Fibromyalgia Pain Syndrome: A Need for Clarity in Terminology and
Differential Diagnosis, Journal of Manipulative Physiologi cal Therapeutics, Vol. 18, No. 6, Jul/Aug
1995, pp. 398-405
13. Betz R., et al, Scoliosis and Pregnancy, The Journal of Bone and Joint Surgery Incorporated,
January 1987, Vol.69-A, No.1, pgs 90-95

7/27/2019 Musculoskeletal Pain and Pregnancy
http://slidepdf.com/reader/full/musculoskeletal-pain-and-pregnancy 8/8
April 1, 2012 E. ANCUTA, MUSCULO-SKELETAL PAIN AND PREGNANCY
Page | 8
14. Ranzi, A., Use of Complementary Medicines and Therapies Among Obstetric
Patients, Obstetrics and Gynecology 2001, April 1997 (4 suppl ): s4
15. Carli G, Suman A, Biasi G, Marcolongo R, Reactivity to Superficial and Deep Stimuli in Patients
with Chronic Musculoskeletal Pain, International Association of the Study of Pain Management,
2002 Dec; 100 (3): 259-69
16. Diakow, P., D.C., et al, Back Pain During Pregnancy and Labor, Journal of Manipulative and
Physiological Therapeutics, Vol. 14, Number 2, February 1991
17. Cohen K Chiropractic Treatment of the Musculoskeletal System During Pregnancy, Journal of the
American Chiropractic Association/May 1997
18. Seidel H., Ball J., Dains J., Benedict G. Mosby’s Guide to Physical Examination Third Ed. 1995; pp.
444-466