Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
-
Upload
kenia-lopez -
Category
Documents
-
view
218 -
download
0
Transcript of Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
-
8/13/2019 Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
1/5
Mayo Clin Proc. March 2007;82(3):351-355 www.mayoclinicproceedings.com 351
NONSURGICAL MANAGEMENT OF HYPERPARATHYROIDISM
For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.
CONCISE REVIEW FOR CLINICIANS
From the Department of Family Medicine (B.F., R.J .P.) and Division of Endocri-nology (T.J .M.), Mayo Clinic College of Medicine, Jacksonville, Fla. Dr Farfordis now at the Keesler Air Force Base, Miss. Dr Moraghan is now with theUniversity of North Dakota School of Medicine, Grand Forks.
A question-and-answer section appears at the end of this article.
Address reprint requests and correspondence to R. John Presutti, DO, Depart-ment of Family Medicine, Mayo Clinic College of Medicine, 4500 San PabloRd, Jacksonville, FL 32224 (e-mail: [email protected]).
2007 Mayo Foundation for Medical Education and Research
Nonsurgical Management of Primary Hyperparathyroidism
BRYANFARFORD, DO; R. JOHNPRESUTTI, DO; ANDTHOMASJ. MORAGHAN, MD
Primary hyperparathyroidism is the most common cause of hyper-calcemia in the outpatient sett ing and is typically caused by asingle benign parathyroid adenoma. Most patients with hyper-parathyroidism are postmenopausal women. Patients can beasymptomatic or minimally symptomatic. Parathyroidectomy isthe definitive cure for primary hyperparathyroidism, and no medi-cal therapies have been approved by the Food and Drug Adminis-tration for this disorder. Guidelines for surgery have been estab-lished by a National Institutes of Health consensus panel, butmany patients do not meet these guidelines or have comorbidconditions that prohibit surgery. This review describes alternativetreatment options for patients who decide against or are unable toproceed with surgery.
Mayo Clin Proc. 2007;82(3) :351 -355
Primary hyperparathyroidism is a leading cause of hy-percalcemia in the outpatientsetting.The typical patientis a postmenopausal woman older than 50 years (mean age,
55 years).In the United States, the incidence of primary
hyperparathyroidism is 2 to 3 per 1000 women and ap-
proximately 1 per 1000 men.1,2The diagnosis of primary
hyperparathyroidism has increased during the past 30 years
with the development and use of automated blood analyz-
ers to monitor serum calcium levels, but the incidence of
cases has been declining since the mid 1980s.3Because of
advances in radiographic and surgical techniques, the clas-
sic presentation of primary hyperparathyroidism with com-
plications of nephrocalcinosis, nephrolithiasis, and osteitisfibrosa cystica is rare today.1,2 Findings in patients with
primary hyperparathyroidism include persistent hypercalce-
mia and elevated serum parathyroid hormone (PTH) levels.
Malignancy, the second most common cause of hypercalce-
mia, is distinguished from primary hyperparathyroidism by
constantly low or suppressed PTH levels. In rare cases,
patients may have higher PTH levels that are attributable to
ectopic PTH secretion, coexisting primary hyperpara-
thyroidism, or PTH resistance. Although surgery is the de-
finitive treatment for patients with symptomatic primary
hyperparathyroidism, many patients do not meet established
surgical criteria or have comorbid conditions that prohibit
surgery. This article reviews the management of primary
hyperparathyroidism in patients who qualify as surgical
candidates but decline or have contraindications to surgery.
SYMPTOMS OF PRIMARY HYPERPARATHYROIDISM
A National Institutes of Health consensus panel recog-
nized 2 forms of primary hyperparathyroidism: asymp-
tomatic and symptomatic.2,4 Patients with asymptomatic
primary hyperparathyroidism account for 75% to 80% of
cases and usually have serum calcium levels that are no
more than 1.0 mg/dL higher than the normal range of 8.9
to 10.1 mg/dL; however, these levels may be as high as
12.0 mg/dL in younger healthy patients.1,2,5,6Symptomatic
primary hyperparathyroidism has no specific clinical pre-
sentation, but several nonspecific symptoms may be
found by eliciting a thorough medical history. Patients
may have weakness, mild depression, fatigue, anorexia,
and often increased absence from work. Patients with
symptomatic hyperparathyroidism usually have a serum
calcium level higher than 12 mg/dL, and nearly all pa-
tients with levels exceeding 14 mg/dL are symptomatic.1
The signs and symptoms of hyperparathyroidism (Table
1) largely reflect the effects of hypercalcemia and may
involve multiple organ systems.1,2,4,5
TYPES OF PRIMARY HYPERPARATHYROIDISM
The pathogenesis of sporadic primary hyperparathyroidism
involves abnormal tissue in the parathyroid gland. Ap-
proximately 80% to 85% of patients with primary hyper-
parathyroidism have benign parathyroid adenomas, and the
remainder have hyperplasia (parathyroid carcinomas are
rare, occurring in approximately 1% of cases).1,2,7Heredi-
tary disorders, including familial hyperparathyroidism,
multiple endocrine neoplasia syndrome (type 1 and 2A),
and hyperparathyroidism-jaw tumor syndrome, account for
approximately 10% of patients with primary hyperparathy-roidism.1Primary hyperparathyroidism is associated with
hypercalcemia and inappropriately high PTH levels (after
adjusting for the level of serum calcium). However, mea-
surement of calciotropic hormones during skeletal evalua-
tion has led to identification of normocalcemic individuals
with elevated PTH levels. This condition called incipient or
eucalcemic primary hyperparathyroidism may represent
the earliest manifestation of primary hyperparathyroidism.8
-
8/13/2019 Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
2/5
Mayo Clin Proc. March 2007;82(3):351-355 www.mayoclinicproceedings.com352
NONSURGICAL MANAGEMENT OF HYPERPARATHYROIDISM
For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.
Benign familial hypocalciuric hypercalcemia is charac-terized by hypercalcemia and relative hypocalciuria. This
autosomal dominant disorder is distinguished from primary
hyperparathyroidism by a calcium clearancecreatinine
clearance ratio [(24-hour urinary calcium serum creatininelevel)/(24-hour urinary creatinine level serum calcium)]
cutoff of 0.01. Familial hypocalciuric hypercalcemia is
present at birth; thus, a previously documented normal se-
rum calcium level excludes this diagnosis.1
SURGICAL TREATMENT GUIDELINES
No medical therapies have been approved by the Food and
Drug Administration for the treatment of primary hyper-parathyroidism, and parathyroid surgery is the only defini-
tive cure.1,2,4,5,9,10A National Institutes of Health consensus
panel on primary hyperparathyroidism recently revised
parathyroid surgery guidelines for asymptomatic patients
(Table 2).4The panel confirmed the recommendation of
parathyroidectomy for any patient with symptomatic hy-
perparathyroidism involving target organs, such as those
with nephrolithiasis, severe bone disease, or neuromuscu-
lar dysfunction.4However, many patients with asymptom-
atic primary hyperparathyroidism do not meet the criteria
recommended for surgery. In addition, many patients
(symptomatic or asymptomatic) voluntarily defer surgery
or have comorbid conditions that preclude surgery.4,7
INITIAL EVALUATION
The initial evaluation of a patient with symptomatic pri-
mary hyperparathyroidism includes measuring the serum
calcium and PTH levels. These values should be mea-
sured simultaneously because of variations that occur
with respect to time, blood volume, and dietary intake.
Elevated PTH production in the presence of persistent
hypercalcemia confirms the diagnosis of primary hyper-
parathyroidism. 2
INPATIENT MANAGEMENT
Symptomatic patients should be hospitalized if they
present with severe hyperparathyroidism-induced hyper-
calcemia, dehydration, or cardiovascular or neurologiccomplications. Initial treatment with intravenous saline so-
lution gradually replaces lost fluids and increases urinary
calcium excretion. However, saline solution rarely amends
serum calcium concentrations in patients with moderate to
severe hypercalcemia. Once fluid repletion is accom-
plished, a loop diuretic may be administered to inhibit
sodium reabsorption at the ascending limb of the loop of
Henle, reduce the passive reabsorption of calcium, and
increase urinary calcium excretion.11 Patients must be
closely monitored for complications caused by aggressive
diuresis, including hypokalemia, hypomagnesemia, and
acute renal insufficiency. Drugs such as intravenous
bisphosphonates or subcutaneous calcitonin may be admin-istered to decrease bone resorption during acute hypercal-
cemia. Although zolendronate has been recommended11for
lowering serum calcium levels during malignancy-induced
hypercalcemia and may be beneficial for patients with
primary hyperparathyroidism, it is not approved by the
Food and Drug Administration for such use. Etidronate,
clodronate, and pamidronate are first-generation bisphos-
phonates that may be used, but they are relatively weaker
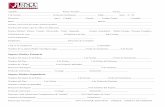
TABLE 1. Signs and Symptomsof Primary Hyperparathyroidism1,2,4,5
NeurologicInability to concentrateConfusionDepression
AnxietyFatigue
CardiovascularHypertensionLeft ventricular hypertrophyProlonged QT intervalBradycardiaValvular calcificationArrhythmia
GastrointestinalAnorexiaNauseaConstipationVomitingAbdominal painPancreatitisPeptic ulcer disease
RenalNephrolithiasisRenal insufficiencyNephrocalcinosisPolydipsiaPolyuria
Musculoskeletal or rheumatologicOsteopeniaOsteoporosisGoutPseudogoutBone or joint painCystic bone lesionsChondrocalcinosis
TABLE 2. National Institutes of Health Guidelines forParathyroidectomy in Asymptomatic Patients With
Primary Hyperparathyroidism4
Serum calcium 1.0 mg/dL above the upper limit of normal
24-h urinary calcium >400 mg
Creatinine clearance reduced by 30%
Bone mineral density T score less than 2.5 SD at any site
Age
-
8/13/2019 Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
3/5
Mayo Clin Proc. March 2007;82(3):351-355 www.mayoclinicproceedings.com 353
NONSURGICAL MANAGEMENT OF HYPERPARATHYROIDISM
For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.
inhibitors of bone resorption compared with zolendronate.
Calcitonin is also a relatively weak agent. It increases renal
calcium excretion and decreases bone resorption by inter-
ference with osteoclast maturation, but its efficacy is lim-
ited to the first 48 hours, even with repeated doses.11After
acute complications of primary hyperparathyroidism havebeen addressed, the possibility of parathyroidectomy
should be considered.
OUTPATIENT M ANAGEM ENT
All management strategies outlined in this section pertain
to patients with symptomatic hyperparathyroidism who
are not surgical candidates because of medical contraindi-
cations or who have elected not to undergo parathyroidec-
tomy for the treatment of primary hyperparathyroidism.
These strategies may also be applied to patients with
asymptomatic primary hyperparathyroidism who decline
surgery.
M ONITORINGClose monitoring is critical during outpatient management.
Although no method is available to predict the timing of
disease progression in an individual patient, 27% of pa-
tients with asymptomatic primary hyperparathyroidism
who initially do not meet surgical criteria develop at least 1
surgical indication during 10 years of follow-up.12If sur-
gery is not recommended or is declined, patients should be
informed of the signs of worsening disease and the critical
need for regular follow-up visits throughout their lifetime.
Recommendations for monitoring include measuring se-rum creatinine levels and bone density (lumbar spine, hip,
and forearm) once a year and measuring serum calcium
levels twice a year. To establish the patients baseline
health profile, abdominal ultrasonography or radiography
should be performed to identify renal stones. Urinary cal-
cium and creatinine clearance should also be measured. If
no renal involvement is detected, baseline studies do not
need to be repeated.7
DIETANDL IFESTYLEM ODIFICATIONSPatients with primary hyperparathyroidism should not
overly restrict their dietary intake of calcium. In fact, a low-
calcium diet may increase PTH secretion, leading to furthercomplications of bone disease. In contrast, a calcium-rich
diet may exacerbate the hypercalemia.10Vitamin D defi-
ciency may increase PTH secretion and bone resorption.10
Therefore, patients should maintain a moderate daily el-
emental calcium intake of 800 to 1000 mg and a vitamin D
intake appropriate for their age and sex (400 IU/d for
women >50 years, 600 IU/d for women >75 years, and 400
IU/d for men >65 years).7,9,10
PHARMACOTHERAPY
Bisphosphonates. Bisphosphonates are analogues of
inorganic pyrophosphate that inhibit osteoclast-mediated
bone resorption.13,14 Symptomatic primary hyperparathy-
roidism leading to parathyroidectomy is frequently associ-
ated with a decrease in cortical bone density and relativepreservation of trabecular bone density,15and bisphospho-
nates are a promising group of medications for the treatment
of bone loss. This finding is interesting because administra-
tion of a bisphosphonate with teriparatide (recombinant hu-
man parathyroid hormone) blunts the improvement in bone
mineral density attained with teriparatide alone.16,17
Alendronate, the most widely studied bisphosphonate,
markedly improved bone mineral density at the lumbar
spine (6.9% increase) and hip (3.7% increase) in patients
with asymptomatic primary hyperparathyroidism after 2
years of therapy.15However, this study found no change
from baseline measurements in serum calcium, PTH, or
urine calcium levels. A separate 2-year study of 32 patients
with primary hyperparathyroidism also showed clear im-
provement of bone mineral density at the lumbar spine
(4.0% increase) after alendronate treatment but failed to
show improvement at the hip or mid radius.18Serum cal-
cium and PTH levels were unchanged from baseline mea-
surements at the end of the study. Chow et al13 reported
similar results, with considerable improvement of bone
mineral density at the lumbar spine and femoral neck. They
also observed a reduction in serum calcium levels but no
change in PTH levels after 1 year. The most commonly
reported adverse effect was mild dyspepsia, but it was not
severe enough to discontinue therapy.13,15,18
Because alen-dronate improves bone mineral density and appears to have
few adverse effects, it should be considered as an alterna-
tive nonsurgical treatment for patients with primary hyper-
parathyroidism-related osteoporosis.15
Risedronate, a potent oral bisphosphonate, reduced fast-
ing serum calcium levels and markers of bone turnover (ie,
alkaline phosphatase, N-telopeptide, osteocalcin) in a study
of 19 patients with primary hyperparathyroidism.14 How-
ever, serum calcium levels increased after the introduction of
an oral calcium load. Additional studies are required to eval-
uate the efficacy of risedronate before such treatment can be
recommended for patients with hyperparathyroidism.
Calcimimetics.Calcimimetic agents increase the sensi-tivity of calcium-sensing receptors in parathyroid chief
cells. Patients with hyperparathyroidism are not as respon-
sive as healthy people to changes in serum calcium concen-
trations and often have increased secretion of PTH in re-
sponse to elevated calcium levels.7Cinacalcet directly low-
ers PTH secretion by enhancing receptor sensitivity.7,19
Shoback et al7reported reductions in serum calcium and
PTH concentrations after oral administration of cinacalcet.
-
8/13/2019 Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
4/5
Mayo Clin Proc. March 2007;82(3):351-355 www.mayoclinicproceedings.com354
NONSURGICAL MANAGEMENT OF HYPERPARATHYROIDISM
For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.
Serum calcium levels decreased after 1 day of treatment and
remained within the reference range for the rest of the study,
and PTH levels decreased by 20%. Patients tolerated the
cinacalcet well and reported few adverse events. The most
common adverse effect, paresthesia, was noted in 9 of the 22
patients. Peacock et al8found similar results in a 52-weekrandomized, double-blind, placebo-controlled study that in-
vestigated the long-term efficacy and safety of cinacalcet for
reducing serum calcium and PTH in patients with mild or
moderate primary hyperparathyroidism. They reported that
73% of cinacalcet-treated patients and 5% of placebo-treated
patients achieved normocalcemia (serum calcium
-
8/13/2019 Manejo Medico Hiperpoara Primario Mayo Clinic 2007 (1)
5/5
Mayo Clin Proc. March 2007;82(3):351-355 www.mayoclinicproceedings.com 355
NONSURGICAL MANAGEMENT OF HYPERPARATHYROIDISM
For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.For personal use. Mass reproduce only with permission fromMayo Clinic Proceedings.
alendronate or raloxifene. If the benefit outweighs the risk,
estrogen replacement is another treatment option. Although
no medical treatment has been approved for primary hyper-
parathyroidism, calcimimetics may reduce serum calcium
and PTH levels. Finally, percutaneous alcohol ablation of the
parathyroid gland may be a suitable treatment for patientswho are unwilling or unable to undergo parathyroidectomy.
REFERENCES1. Kearns AE, Thompson GB. Medical and surgical management of hyper-
parathyroidism [published correction appears inMayo Clin Proc. 2002;77:298].Mayo Clin Proc.2002;77:87-91.
2. Taniegra ED. Hyperparathyroidism.Am Fam Physician.2004;69:333-339.3. Wermers RA, Khosla S, Atkinson EJ, Hodgson SF, OFallon WM, Melton
LJ III. The rise and fall of primary hyperparathyroidism: a population-basedstudy in Rochester, Minnesota, 1965-1992.Ann Intern Med.1997;126:433-440.
4. Bilezikian JP, Potts JT Jr, El-Hajj Fuleihan G, et al. Summary statementfrom a workshop on asymptomatic primary hyperparathyroidism: a perspec-tive for the 21st century.J Bone Miner Res.2002;17(suppl 2):N2-N11.
5. Fuleihan Gel-H. Clinical manifestations of primary hyperparathyroid-ism. In: Rose BD, ed. UpToDate. Waltham, Ma; 2005.
6. Bilezikian JP, Silverberg SJ. Clinical practice: asymptomatic primary
hyperparathyroidism.N Engl J Med.2004;350:1746-1751.7. Shoback DM, Bilezikian JP, Turner SA, McCary LC, Guo MD, PeacockM. The calcimimetic cinacalcet normalizes serum calcium in subjects withprimary hyperparathyroidism.J Clin Endocrinol Metab.2003;88:5644-5649.
8. Peacock M, Bilezikian JP, Klassen PS, Guo MD, Turner SA, Shoback D.Cinacalcet hydrochloride maintains long-term normocalcemia in patients withprimary hyperparathyroidism.J Clin Endocrinol Metab.2005;90:135-141.
9. Utiger RD. Treatment of primary hyperparathyroidism. N Engl J Med.1999;341:1301-1302.
10. Agus ZS. Management of asymptomatic primary hyperparathyroidism.In: Rose BD, ed. UpToDate. Waltham, Ma; 2005.
11. Agus ZS, Savarese DMF, Berenson, JR. Treatment of hypercalcemia. In:Rose BD, ed. UpToDate. Waltham, Ma; 2005.
12. Silverberg SJ, Shane E, Jacobs TP, Siris E, Bilezikian JP. A 10-yearprospective study of primary hyperparathyroidism with or without parathyroidsurgery [published correction appears inN Engl J Med. 2000;342:144].N EnglJ Med. 1999;341:1249-1255.
13. Chow CC, Chan WB, Li JK, et al. Oral alendronate increases bonemineral density in postmenopausal women with primary hyperparathyroidism.J Clin Endocrinol Metab.2003;88:581-587.
14. Reasner CA, Stone MD, Hosking DJ, Ballah A, Mundy GR. Acutechanges in calcium homeostasis during treatment of primary hyperparathyroid-ism with risedronate.J Clin Endocrinol Metab.1993;77:1067-1071.
15. Khan AA, Bilezikian JP, Kung AW, et al. Alendronate in primaryhyperparathyroidism: a double-blind, randomized, placebo-controlled trial.JClin Endocrinol Metab.2004;89:3319-3325.
16. Black DM, Greenspan SL, Ensrud KE, et al, PaTH Study Investigators.The effects of parathyroid hormone and alendronate alone or in combination inpostmenopausal osteoporosis.N Engl J Med. 2003;349:1207-1215.
17. Finkelstein JS, Hayes A, Hunzelman JL, Wyland JJ, Lee H, Neer RM.The effects of parathyroid hormone, alendronate, or both in men with os-teoporosis.N Engl J Med. 2003;349:1216-1226.
18. Parker CR, Blackwell PJ, Fairbairn KJ, Hosking DJ. Alendronate in thetreatment of primary hyperparathyroid-related osteoporosis: a 2-year study.JClin Endocrinol Metab.2002;87:4482-4489.
19. Cinacalcet. EFacts. 2005. Available at: www.formchecker.com/Fac/servlet/MonoViewer?sys=1&id=503&sec=3&set=g5n73. Accessed Septem-ber 22, 2005.
20. Raloxifene. EFacts. 2005. Available at: www.formchecker.com/Fac
/servlet/MonoViewer?sys=1&id=309&sec=3&set=7ci0b. Accessed September22, 2005.21. Zanchetta JR, Bogado CE. Raloxifene reverses bone loss in postmeno-
pausal women with mild asymptomatic primary hyperparathyroidism. J BoneMiner Res.2001;16:189-190.
22. Rubin MR, Lee KH, McMahon DJ, Silverberg SJ. Raloxifene lowersserum calcium and markers of bone turnover in postmenopausal women withprimary hyperparathyroidism.J Clin Endocrinol Metab.2003;88:1174-1178.
23. Bennedbaek FN, Karstrup S, Hegedus L. Percutaneous ethanol injectiontherapy in the treatment of thyroid and parathyroid diseases.Eur J Endocrinol.1997;136:240-250.
24. Harman CR, Grant CS, Hay ID, et al. Indications, technique, and efficacyof alcohol injection of enlarged parathyroid glands in patients with primaryhyperparathyroidism.Surgery.1998;124:1011-1019.
25. Karstrup S, Hegedus L, Holm HH. Ultrasonically guided chemical par-athyroidectomy in patients with primary hyperparathyroidism: a follow-upstudy. Clin Endocrinol (Oxf).1993;38:523-530.
26. Ives HE. Diuretic agents. In: Katzung BG, ed. Basic and Clinical Phar-macology. 7th ed. Stamford, Conn: Appleton and Lange; 1998:251.
27. Potts JT Jr. Diseases of the parathyroid gland and other hyper- andhypocalcemic disorders. In: Kasper DL, Braunwald E, Fauci AS, Hauser SL,Longo DL, Jameson JL, eds.Harrisons Principles of Internal Medicine. Vol2. 16th ed. New York, NY: McGraw-Hill Medical Publishing Division;2005:2256.
Questions About Nonsurgical Management of
Primary Hyperparathyroidism
1. Which oneof the following is the most commoncauseof hypercalcemia in the outpatient setting?
a. Malignancyb. Primary hyperparathyroidismc. Sarcoidosisd. Thiazide diureticse. Iatrogenic
2. Which oneof the following is nota National Institutesof Health guideline for parathyroid surgery in asymp-tomatic patients with primary hyperparathyroidism?
a. Serum calcium levels 1.0 mg/dL above the upperlimit of normal
b. 24-hour urinary calcium greater than 400 mgc. Creatinine clearance reduction of 30%d. Bone mineral density T score less than 2.5 SD at
any sitee. Age older than 50 years
3. Which oneof the following is part of the initialevaluation of a patient with clinical signs andsymptoms of primary hyperparathyroidism?
a. Chest radiographyb. Electrocardiographyc. Parathyroid hormone leveld. Complete blood cell counte. Bone mineral density determination
4. Which oneof the following agentsincreasesthesensitivity of calcium-sensing receptors inparathyroid chief cells?
a. Cinacalcetb. Estrogenc. Risedronated. Raloxifenee. Alendronate
5. Which oneof the following medications may inducehypercalcemia?
a. Risedronateb. Penicillinc. Lithium carbonated. Diltiazeme. Furosemide
Correct answers:1. b, 2. e, 3. c, 4. a, 5. c