Liver function tests
-
Upload
rishabh-gupta -
Category
Health & Medicine
-
view
179 -
download
2
Transcript of Liver function tests

Liver Function Tests
Moderator – Dr. Saroj JaswalSubmitted by 51-60

GROSS ANATOMY •Two lobes (falciform ligament) • Blood supply : Hepatic artery(oxygen)& Portal vein(nutrients)• veinous supply : hepatic veins , inferior vena ceva •microscopic units lobules functional units of liver •Each lobule is a hexagonal centrally located vein with portal triads

BIOCHEMICAL FUNCTIONS The liver performs four major functions : Excretion / secretion Metabolism Detoxification Storage
1. Synthetic functions : Plasma proteins – albumin(osmotic pressure) , carrier
proteins ( transport of elements Fe Cu) , globulins , coagulation factors.
Cholestrol – precursor of steroid hormones , bile acids and 7-dehydrocholestrol.
Bile acids- to absorb lipid nutrients from the gut , includes fatty acids and fat soluble vitamins .

METABOLISM Carbohydrate metabolism :Liver is an important homeostatic regulator
of blood glucose . It can either produce glucose or store glucose
. By the following processes :1. Glycogenesis – by converting glucose into
glycogen for storage .2. Glycogenolysis – ATP is required , glycogen
is again converted back into glucose .3. Gluconeogenesis – formation of glucose
from non precursor carbohydrates such as lactate , glucogenic amino acid and propinyl CoA .

AMINO-ACID METABOLISM PROTEINS get breakdown in the intestine into
amino acids and reach liver by portal vein ; utilized to form different proteins like globulin , albumin , coagulation factors …………………..
LIPID METABOLISM : Fatty acids catabolised to release CoA – used for TCA
cycle and ETC to release energy . Acetyl CoA converted to ketone bodies – acetone ,
acetoacetate and hydroxybutyric acid . Liver synthesis apoprotein part of lipoproteins –
transportation of lipids into circulation .

PROTECTIVE FUNCTION & DETOXIFICATION
Exogenous substances : It detoxify toxic substances – hydrolysis , hydroxylation ,oxidation , reduction and demethylation .
More soluble in water and easily excreted through urine .
Drugs – metabolised by P450 enzyme system of liver , convert drugs into more soluble form which in due course conjugate with sub. Like glycine , glucouronic acid to get excreted in urine .
Endogenous substances – Kupffer cells perform phagocytosis to eliminate foreign cmpds . For eg. NH3 is detoxified urea and metabolism of xenobiotics ( detoxification )

WHAT IS PURPOSE OF LFTS?
LFTs alone do not give the physician full information, but used in combination with a careful history, physical examination (particularly ultrasound and CT Scanning), can contribute to making an accurate diagnosis of the specific liver disorder.
Different tests will show abnormalities in response to liver inflammation liver injury due to drugs, alcohol, toxins, viruses Liver malfunction due to blockage of the flow of bile Liver cancers

CLASSIFICATION OF LFT’SSynthetic function of liver-a. Serum proteins – albumin,globulin,ceruloplasmin haptoglobin , alpha
fetoprotein , alpha 1 antitrypsin levelsb. Prothrombin time
Serum Enzymes(liver enzyme panel)c. Indicating hepatocellular damage- ALT , ASTd. Indicating obstruction- ALP, GGT
Based on detoxification functione. Blood ammonia f. Hippuric acid test
Hepatic excretory function-g. serum- bilirubin levels, conjugated and unconjugated h. Urine – bile pigments , bile salts and urobilinogen

TEST BASED ON SYNTHETIC
FUNCTION OF LIVER

1)SERUM ALBUMIN LEVEL Normal Value- 3.5 to 5 g/dl Albumin is major protein- responsible for OSMOTIC
pressure in vascular system Half life: 20 days, low level in all chronic diseases of
liver Normal A/G ratio is 1.2 to 1.5 :1 Reverses in case of cirrhosis due to
hypoalbuminemia and hypergammaglobulinemia.

2) SERUM GLOBULIN
• Alpha and beta globulins synthesized by liver and immunoglobulin by lymphocytes
• Normal value - 2.5 to 3.5 g/dl • Cirrhotic liver cannot clear bacteria, antibodies against intestinal
bacteria seen.• Ig A –Inc. in alcoholic liver disease
Ig M - ↑↑ Primary biliary cirrhosis..
Ig G - ↑↑ Auto immune hepatitis.

3) PROTHROMBIN TIME
Prothrombin is synthesized by liver Half life – 6 hrs so it indicate – present function of liver PT :blood test, time taken by blood to clot Normal value : 10 to 15 sec. PT is Prolonged - liver losses 80% of reserve capacity Commonly PT is used for detecting liver coagulopathies Note : Vit K deficiency Prolongs PT time But In case of LIVER diseases : PT remains prolonged
even after parenteral administration of Vit. K

4) 1-ANTITRYPSIN (AAT)
• Most abundant 1-globulin and acute phase reactant• Inactivates : serum proteases • Normal values : 90 to 200 mg/dl• It has multiple alleles , individuals possessing PiZZ allele :
deficient activity of this enzyme : Liver cirrhosis
Low levels Neonatal cholestasis, emphysema
High levels acute trauma, infection

5) HAPTOGLOBIN• Another major 2 protein synthesised in liver.• Normal values: 30- 200 mg/dl• Function – transports free Hb in the plasma to reticuloendothelial
system (RES)• Low levels – lead to ppt of free Hb in kidneys and cause damage
• Turnover rates are less than albumin – used to Identify recent changes in the liver.
Low levels Severe hepatocellular diseases (deficient synthesis), hemolytic disease(rapid degradation)
High levels Inflammatory processes , myocardial infarction

6) -FETOPROTEIN
Normal component of fetal blood., disappears after few weeks of birth.
Normal range-up to 1 year of age < 30ng/ml adults(M and non pregnant F) < 15ng/ml Tumor marker
Maternal serum AFP level Inc. in fetal open tube neural defect and dec. in foetal down syndrome
Mild Inc. Chronic hepatitis or cirrhosis
Drastic Inc. hepatocellular carcinoma, germ cell tumour and teratoma of ovary

7) CERULOPLASMIN
Synthesized by Hepatic parenchymal cells and small part by lymphocytes
Transport : Cu Normal levels: males 22- 40mg/dl
females 25-60mg/dl
pregnancy 30-120 mg/dl
Low levels
Wilson's hepatolenticular degeneration
High levels
Acute Hepatitis, hemochromatosis, obstructive biliary disease

8)TRANSTHYREITN (PRE-ALBUMIN) Produced by liver Transport thyroxine and triidothyronine Half life 2 days , hence useful parameter to assess
hepatic function early in course of liver disorders.

TEST BASED ON SERUM ENZYMES
A. Enzymes indicating Hepatocellular Damage
Alanine amino transferase (ALT) Serum Glutamate Pyruvate transaminase (SGPT) Source - liver, cardiac muscle , skeletal muscle. Increased – when cells of the liver have been inflamed or
necrosed. Normal serum level : male- 13-35 U/L female – 10-35 U/L
SGPT PLP

Abnormal levels
Only ALT are elevated in:-1. AMI rise within 6-8 hrs and remain upto 5 days
2. Pulmonary embolism
Aspartate amino transferases (AST) Serum glutamate oxaloacetate transaminase (SGOT) Source- more liver specific
Moderate 50 - 100 Chronic liver diseases,hepatitis C, NASH(non alcoholic steatohepatitis )
Very high 300-1000
Acute hepatitis , toxic or viral in origin
ASTPLP

Normal level : 8-20 U/L
Normal AST: ALT ratio – 0.8
ratio > 2 AST is higher
Alcoholic hepatitis, hepatitis with cirrhosis , NASH , erythromycin treatment
Ratio < 0.8ALT is higher
Acute hepatocellular injury, toxic exposure ,extra hepatic obstruction
elevated liver diseases, myocardial infarct, muscle disease

B. Markers of obstructive liver disease Alkaline Phosphatase (ALP) Source: liver, bone, placenta and intestine. ALP is a hydrolase enzyme responsible for removing
phosphate groups from many types of molecules, including nucleotides and proteins.
phosphomonoester ALP alcohol + phoshate ion Normal level: 40-125 U/L Levels are significantly higher in children and pregnant
women.
Moderate increase
2-3 times Hepatic diseases includes infective hepatitis,hepatocellular carcinoma
Very high levels 10-12 times Obstructive jaundice (gall stones)
Drastically high levels
More than 12 times
Not related to liver disease but Bones disease such as rickets, osteomalacia

ISOENZYMES OF ALP Iso enzyme location Increased in
Alpha 1 ALP Epithelial cells of biliary canaliculi
Obstructive jaundice
Alpha 2 heat labile ALP
Hepatic cells
Alpha 2 heat stable ALP
Placental origin (regan iso enzyme)
Pregnancy and inhibited by phenylalanine
Pre beta ALP Bone origin Pagets disease, rickets osteomalacia
Gamma ALP Intestinal cells Ulcerative colitis5’- NucleotidaseNormal range 2-17 U/LFunction ; hydrolysis of nucleoside 5’ phosphate estersClinical significance
Sensitive and specific for hepatobiliary disorders (HBD), obstructive biliary diseases Normal pregnancy, bone growth and bone diseases do not affect 5' NTIn pts with HBD, changes in ALP are usually followed by similar changes in 5' NT

GAMMA GLUTAMYL TRANSFERASE (GGT)1. Function – Glutathione + amino acid GGT glutamyl peptide +
cysteinylglycine regulate glutathione levels
2.Source - liver, kidney, pancreas, intestinal cells absent in bone
3.Normal serum levels : 10-30 U/L4. Diagnostic signicficance hepatic microsomal enzyme GGT elevation differentiate ALP increase
levels ,seen in biliary tract diseases In alcoholic liver disease GGT levels may be parallel to
alcohol intake , even when other LFT’s are in Normal range.diseases pancreatic disease , MI ,pulmonary disease
Drugs warfarin , antidepressants


TEST BASED ON DETOXIFICATIOMBlood ammonia level Normal level: 10-50 mcg/dl Index of urea synthesis by liver, marker of hepatic
encaphlopathy Ammonia is converted to urea by liver Increased levels 1. cirrhosis
2. portocaval anastomoses
Hippuric acid test Benzoyl glycine Reaction benzoic acid+glycine = hippuric acid Ingestion of sodium benzoate thn hourly excretion hippuric
acid is constant Decreases when the liver fails to detoxify

Oral Glucose tolerance test Glucose tolerance: ability of person to metabolise
a given load of glucose Glucose load : 75g in 250-300ml of water. Urine
samples are taken

EXCRETORY FUNCTIONS OF LIVER

TESTS BASED ON EXCRETORY FUNCTION
1.Serum bilirubin2.Urine bilirubin3.Urine and faecal urobilinogen4.Urine bile salts

SERUM BILIRUBIN

What is bilirubin?
•Bilirubin is a linear tetrapyrrole structure.
•It is the end product of heme catabolism.
•It is yellowish in colour and found in bile.
•Produced by reticuloendothelial system

Since the bilirubin is a waste product, hence
it has to be excreted from the body
For this it has to be first conjugated by the
hepatocytes to make it water soluble to be
removed from the body.


CONJUGATION OF BILIRUBIN

EXCRETION OF BILIRUBIN
Water soluble bilirubin Mixed with the bile
Reaches the Intestine Deconjugated by the bacterial flora
Free Bilirubin
Reduced
Urobilinogen (UBG) (Tetrapyrrole structure)
reduction of vinyl substituent groups
Stercobilinogen (SBG)


NORMAL VALUES
Total Bilirubin 0.2 to 0.8
mg/dl
Conjugated bilirubin 0 to 0.2
mg/dl
Unconjugated Bilirubin 0.2 to
0.6mg/dl

HYPERBILIRUBINEMIAS
These can be grouped in two ways1. Conjugated or Unconjugated2. Congenital and aquired

CONGENITAL HYPERBILIRUBINEMIAS
Crigler Najjar Syndrome- Deficiency of UDP glucuronyl transferase
Gilbert Syndrome-Defective uptake of bilirubin by the liver
Dubin Johnson Syndrome-Defective excretion of conjugated bilirubin
Rotor Syndrome

AQUIRED HYPERBILIRUBINEMIAS
Physiological Jaundice in new borns Breast Milk Jaundice

URINE UROBILINOGEN


Bilirubin in Urine:Normally bilirubin is absent in urine.Conjugated bilirubin being water soluble is excreted in urine in obstructive jaundice.
This can be detected by Fouchet’s test
Urine urobilinogen - normally trace amounts is present.
In obstructive jundice no urobilinogen is present in urine.

because bilirubin cannot enter intestine.
Note: Presence of bilirubin in urine and absence of urobilinogen in urine is seen in obstructive jaundice.
In hemolytic jaundice increased production of bilirubin causes increased formation of urobilinogen which appears in urine.
Note: Increased urobilinogen in urine and absence of bilirubin in urine is seen in hemolytic jaundice.

Fecal urobilinogen - Normal about 300mg.
Increased in Hemolytic jaundice in which color of feces is dark.
In Obstructive jaundice urobilinogen is not excreted through feces and the color is the feces is pale.

BILE SALTS

SYNTHESIS OF BILE SALTS
Cholesterol hydroxylated at 3/7/12 positions
Removal of 3-carbon unit, to make it 24 C
Conjugation with glycine
Secretion into intestinal canal
In the intestine, deconjugation and removal of hydroxyl groups.

Normally bile salts (sodium salts of taurocholic acid and glycocholic acid) are present in the bile; but are not seen in urine. Bile salts in urine are detected by Hay’s test.
Positive Hay’s test indicates the obstruction in the biliary passages causing regurgitation of bile salts into the systemic circulation leading to its excretion in urine.

Jaundice

• Jaundice is yellowish discoloration of the skin, sclera and mucous membranes due to hyperbilirubinemia and deposition of bile pigments .
• Equilibrium between bilirubin production and clearance is disturbed .
• Serum bilirubin level greater than 2mg/dL
• Jaundice is NOT a disease, but rather a sign that can occur in many different diseases.
What is Jaundice?

TYPES OF JAUNDICE
PRE HEPATIC HEPATIC POST HEPATIC
Excessive amount of bilirubin is presented to the liver due to excessive hemolysis
Impaired cellular uptake, defective conjugation or abnormal secretion of bilirubin by the liver cell
Impaired excretion due to mechanical obstruction to bile flow
Elevated unconjugated bilirubin in serum
Both conjugated and unconjugated bilirubin may be elevated in serum
Elevated conjugated bilirubin in serum

TYPES OF JAUNDICE
PRE HEPATIC
HEPATIC POST HEPATIC
Hemolytic Anemia
Hepatitis, cirrhosis, Crigler-Najjar Syndrome, Dubin-Johnson Syndrome, Rotor’s Syndrome
Gallstone, malignancy, inflammation

There are other types of Jaundice : Pathologic
JaundicePathologic jaundice can occur in children and adults and is diagnosed when jaundice presents a health risk. Several forms of hepatitis, cirrhosis of the liver and other liver diseases, bile duct blockage, along with infections and medications, can also cause pathological jaundice. Gilbert Syndrome Jaundice
Gilbert's syndrome is a harmless hereditary condition that results in mild jaundice. During times of illness or stress, people with Gilbert's syndrome will experience low levels of some bilirubin-processing enzymes in their livers, according to LabTestsOnline.com. Once diagnosed, Gilbert's syndrome does not require further medical treatment.

Neonatal Jaundice
•Jaundice is clinically detectable in the newborn when the serum bilirubin levels are greater than 85 μmol/L. This occurs in approximately 60% of term infants and 80% of preterm infants.
•Neonatal jaundice first becomes visible in the face and forehead. Blanching reveals the underlying colour. Jaundice then gradually becomes visible on the trunk and extremities.


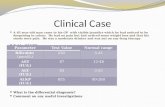
Function test Pre-hepatic Jaundice Hepatic Jaundice Post-hepatic Jaundice
Total bilirubin Normal / Increased Increased
Conjugated bilirubin Normal Increased Increased
Unconjugated bilirubin Normal / Increased Increased Normal
Urobilinogen Normal / Increased Increased Decreased / Negative
Urine Color Normal Dark (urobilinogen + conjugated bilirubin)
Dark (conjugated bilirubin)
Stool Color Normal Normal/Pale Pale
Alkaline phosphatase levels
Normal
Increased
Alanine transferase and Aspartate transferase levels
Increased
Conjugated Bilirubin in Urine Not Present Present
Splenomegaly Present Present Absent
Table of diagnostic tests

VAN DEN BERGH TEST
Van den bergh test is specific for bilirubin. Normal serum gives a positive van den bergh reaction.
Principle of the reaction:REACTION
Bilirubin + diazotized sulphanilic acid
Purple coloured azobilirubin

VAN DEN BERGH TEST
Direct Positive:
conjugated bilirubin gives a purple color immediately on addition of the reagent.
Indirect Positive:Purple color develops only when the reagent and methanol are added.
Unconjugated bilirubin gives color only when methanol is added.
Hence conjugated bilirubin is also called direct bilirubin and unconjugated called indirect bilirubin

VAN DEN BERGH TEST
BiPhasic:Purple color develops immediately on addition of reagent.Addition of methanol intensifies the color.Elevation of both unconjugated and conjugated bilirubin.

VAN DEN BERGH TEST
RESULTSIndirect Positive Hemolytic jaundiceDirect Positive Obstructive
jaundiceBiphasic Hepatic
jaundice

SCHLESINGER’S TEST
The bilinogens form complexes with zinc ions which exhibit brilliant green fluorescence.
It is negative in normal urine.

EHRLICH’S TEST
Bilinogens react with Erlich’s aldehyde reagent i.e. Para dimethyl amino benzaldehyde to form red colour.


HAYS TEST
Hay's test, also known as Hay's sulphur flower test, is a chemical test used for detecting the presence of bile salts in urine

THANK YOU