Liver Function Tests
Click here to load reader
-
Upload
kamal-jaoni -
Category
Documents
-
view
34 -
download
4
Transcript of Liver Function Tests

1
Liver Function Tests
Shannon Jenkins, M.D.
•The diagnosis can be established noninvasively in the vast majority of patients with abnormal Liver Function Tests.
•Appropriate testing can be guided by the pretest probability of specific forms of liver disease
•The majority of patients in whom the diagnosis remains unclear after obtaining a history and laboratory testing will have alcoholic liver disease, fatty liver, or NASH
• Enzyme tests–Aminotransferases–Alkaline phosphatase–Gamma glutamyl transpeptidase
• Tests of synthetic function–Albumin–Prothrombin time
• Tests of hepatic transport capability–Serum bilirubin
Aminotransferases
• Alanine aminotransferase (ALT or SGPT), Normal 10-40 IU/L
• Aspartate aminotransferase (AST or SGOT), Normal 10-40 IU/L

2
Serum AminotransferaseLevels > 500
• Acute viral hepatitis• Wilson’s disease• Severe chronic active hepatitis• Common Bile Duct Stone• Budd-Chiari and Veno-occlusive Disease• HELLP
Serum AminotransferaseLevels > 10,000
• Ischemic liver/hepatic shock
• Acetominophen overdose
Minimal Elevation or NormalSerum Aminotransferases
• Hemochromatosis• Jejunoileal bypass• Chronic HCV• NASH
Common Causes of Mildly Elevated Liver Transaminases
Drug-induced hepatitis
• NSAIDS• Antibiotics• Statins• Antiepileptic drugs• Antituberculous drugs• Acetominophen
Alcoholic Hepatitis
• AST:ALT ratio > 2• Both levels < 300• GGT elevated 2x normal

3
Alcoholic Hepatitis
• [(Prothrombin time-control) x 4.6] + serum bilirubin = Discriminant Function Value
• If Discriminant Function Value > 32, mortality of pt > 50% within 2 years
• Treat with steroids or pentoxyphillin
Hepatitis B
• Parenteral drug use• Areas of high disease prevalence (Southeast
Asia, China and sub-Saharan Africa)
• Check: – Hepatitis B surface antigen – Hepatitis B surface antibody – Hepatitis B core antibody
Hepatitis C
• Parenteral exposure (blood transfusions, intravenous drug use, occupational)
• Cocaine use• Tattoos• High risk sexual behavior.
Hepatitis C
• Check Hepatitis C antibody
• Hepatitis C RNA by PCR
Hemochromatosis
• Increased Iron saturation (serum iron/TIBC)– > 45%, obtain serum ferritin
• Increased Ferritin (> 400 ng/mL men, > 300 ng/mL in women)
• Check genetic studies: HFE genetic mutation
• Liver biopsy
Hemochromatosis and Cirrhosis
• Unlikely to develop cirrhosis, if:– < 40 years of age– Absence of hepatomegaly– Normal ALT and AST– Serum ferritin < 1000

4
Non-Alcoholic Steatohepatitis (NASH)
• Mild elevations in aminotransferases (2-4 fold increase only)
• AST/ALT ratio < 1• Mild increase in ALP• Normal albumin, INR and bilirubin
Non-alcoholic Steatohepatitis (NASH)
• Common in women, DM and obesity• May be asymptomatic• Symptoms: fatigue, RUQ discomfort/pain• U/S, CT scan or MRI reveals fatty
infiltration of the liver
Liver biopsy for Non-alcoholic Steatohepatitis
• Peripheral stigmata of chronic liver disease • Splenomegaly • Cytopenia • Abnormal iron studies • Diabetes and/or significant obesity in an
individual over the age of 45 with elevated ALT
“Unexplained” ALT Elevations
• Muscle Disease or Injury• Celiac Disease• Adrenal Insufficiency• Thyroid Disease
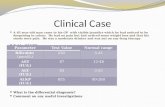
Case 1
• Patient is a 42yo female• PMH significant only for HTN for which
she takes no medications• NKDA• SH: no tobacco, no illicits, “social” drinker• Works at a drycleaners
Case 1
• WBC 7,000
• H/H 9/27
• Platelets 101,000
• AST 88, ALT 41

5
What is the likely cause of her elevated liver enzymes?
• A. Etoh hepatitis
• B. Shock liver
• C. Halothane toxicity
• D. Hemochromatosis
Case 1
• The same patient returns 1 month later with complaint of headaches and fatigue.
• AST 2650 • ALT 3900
What is the likely cause of her elevated liver enzymes?
• A. Etoh hepatitis
• B. Shock liver
• C. Acetominophen toxicity
• D. Hemochromatosis
Case 2
• Patient is an 81yo male admitted secondary to AMI
• PMH significant for CAD, s/p MI and CHF with EF of 25%
• Patient had syncopal episode witnessed by nursing
Case 2
• AST 19,524, ALT 16,233
• WBC 6,000, no bandemia
• Troponin 0.4, CK 220
What is the likely cause of his elevated liver enzymes?
• A. Etoh hepatitis
• B. Shock liver
• C. Acetominophen toxicity
• D. Hemochromatosis

6
Case 3
• Patient is a 58yo male• Admitted secondary to generalized
weakness and vague abdominal pain• PMH: none• Meds: none• NKDA
Case 3
• SH: Mild MR. Lives with his brother since the death of his parents.
• Occasional Etoh and tobacco
• No environmental exposures
Case 3
• Glucose 240
• AST 170, ALT 157
What is the likely cause of his elevated liver enzymes?
• A. Etoh hepatitis
• B. Shock liver
• C. Acetominophen toxicity
• D. Hemochromatosis
Case 4
• Patient is a 28yo G2P1001 at 26 weeks EGA presenting to the ED with jaundice
• PMH: diagnosed with TB 4 weeks prior• Meds: INH, Rifampin, Ethambutol,
Pyridoxine• NKDA
Case 4
• SH: Immigrated from Equador 7 months prior, no tobacco, Etoh or illicits
• BP 128/77, HR 80, R 12, Afebrile• ALT 601, AST 319, ALP 251• Tbili 2.7• LDH 246

7
What is the likely cause of her elevated liver enzymes?
• A. HELLP
• B. Cholestasis of pregnancy
• C. Drug induced hepatitis
• D. Hemochromatosis
What is your next step
• A) Discontinue all anti-tubercular medications
• B) Liver biopsy• C) Uric acid, platelets, 24 hour urine for
protein, Ca+• D) Continue current course of therapy
Rare Causes of Elevated Transaminases
• Autoimmune hepatitis
• Wilson’s disease
• Alpha-1 antitrypsin deficiency
Autoimmune Hepatitis
• Primarily young to middle-aged women• Associated with arthralgias, fatigue,
anorexia, pruritus• Often co-existence of other autoimmune
diseases• Increased IgG on SPEP • Elevated Anti-nuclear antibodies (ANA) &
anti-smooth muscle antibodies (SMA)
Wilson’s Disease
• Genetic disorder of biliary copper excretion
• Typically age 5-25, but consider the dx in age < 40
• Adolescents present with liver disease
• Adults present with mental status change

8
Wilson’s Disease
• Decreased ALP• Decreased uric acid• Elevated AST and ALT, > 500 IU/L• Initial screen: serum ceruloplasmin• Opthalmologist for Kayser-Fleischer
rings
Alpha-1 Antitrypsin Deficiency
• Uncommon• Chronic liver disease• Decreased alpha-1 antitrypsin level• Alpha-1 antitrypsin phenotype• Suspect in patient with early emphysema
Elevated Alkaline Phosphatase
Alkaline Phosphatase
• Normal = 30-120 IU/L
• Check GGT to determine if elevated ALP is secondary to hepatic source
• Mild elevations may be seen post-prandial
Sources of Alkaline Phosphatase
• Liver• Bone• Small intestines• Placenta/Pregnancy• Regan isoenzyme (lung teratoma)
Causes of Elevated ALP
• Pregnancy• Pancreatic
Cancer• Paget’s disease• Primary biliary
cirrhosis
• Cholestasis• Sarcoid• Amyloid• Hyperthyroid• Hypernephroma• Hodgkin’s
disease

9
Intrahepatic Cholestasis
– Viral hepatitis– Etoh hepatitis– EBV– Anabolic
steroids, Contraceptives
– CMV– TPN– Primary biliary
sclerosis– Primary
sclerosing cholangitis
Extrahepatic Cholestasis
• Choledocholithiasis• Pancreatic or Gallbladder CA• Cholangiocarcinoma • Primary sclerosing cholangitis• Stricture due to chronic pancreatitis• AIDS cholangiopathy
Primary Biliary Cirrhosis
• 95% of patients with PBC are women• Onset between 30-65 years of age.• May be asymptomatic• Symptoms: Fatigue, pruritus,
hyperpigmentation, arthralgias
Primary Biliary Cirrhosis
• Elevated Alkaline phosphatase levels• Elevated bilirubin• Mildly elevated transaminases• + Antimitochondrial antibodies• + Antinuclear antibodies (ANA)
Case 5
• Patient is 34yo female admitted to the psychiatric ward
• You are consulted due to elevated liver enzymes on admission labs.
• Patient with tremor, confusion
Case 5
• ALT 1620, AST 1550, ALP22
• Na 122
• Uric acid 1.1 mg/dL (normal 1.9-7.5mg/dL0

10
What is the likely cause of this patient’s elevated liver enzymes?
• A. Pancreatic Cancer
• B. Wilson’s disease
• C. Primary biliary cirrhosis
Case 6
• 58yo female with fatigue and pruritus• No significant PMH• No medications• NKDA
Case 6
• ALP 423• Total bilirubin 10.2• AST 110, ALT 133• GGT 55 (normal < 30)
What is the likely cause of this patient’s elevated liver enzymes?
• A. Pancreatic Cancer
• B. Wilson’s disease
• C. Primary biliary cirrhosis
• D. Autoimmune hepatitis
What test would you order now?
• A. Liver biopsy• B. Antimitochondrial antibodies• C. Alpha-1 antitrypsin• D. Antinuclear antibodies
Case 7
• 60yo female presenting to the ED with jaundice, fatigue and midepigastric ache that radiates to her back.
• Pain has been present for approximately 4 months, since she was hospitalized for MI
• 25 lb weight loss

11
Case 7
• Glucose 199• AST 156 ALT 144• ALP 155• Total bilirubin 1.1 mg/dL• Direct bilirubin 0.3 mg/dL
What is the likely cause of this patient’s elevated liver enzymes?
• A. Pancreatic Cancer
• B. Wilson’s disease
• C. Primary biliary cirrhosis
Case 8
• Patient is 38yo female presenting with arthralgias
• AST 9800, ALT 8600• Total protein 9.0• Albumin 3.5• Total bilirubin 0.7 (normal)• ALP 110
What is the likely cause of this patient’s elevated liver enzymes?
• A. Pancreatic Cancer
• B. Wilson’s disease
• C. Primary biliary cirrhosis
• D. Autoimmune hepatitis
Case 9
• 71yo male with several month history of back pain
• PMH: CAD s/p CABG 9 years prior, HTN, hypercholesterolemia
• Meds: ASA, lopressor, lisinopril, pravachol• NKDA
Case 9
• ALP 772 IU/L• Total bilirubin 0.4 mg/dL• AST 35 IU/L• ALT 28 IU/L• GGT 15

12
What is the likely cause of this patient’s elevated liver enzymes?
• A. Pancreatic Cancer
• B. Wilson’s disease
• C. Primary biliary cirrhosis
• D. Paget’s disease
Tests of Synthetic Function
• Albumin (normal = 3.5-4.8 g/dL)– Low level suggests chronic process (cancer or
cirrhosis)– Normal level couples with abnormal
transaminases suggests acute process (viral hepatitis or choledocholithiasis)
• Prothrombin time (normal = – Elevated in Vitamin K deficiency– Elevated with hepatocellular dysfunction
Causes of Low Serum Albumin and Total Protein
• Malnutrition• Liver disease• Nephrotic syndrome• Protein losing enteropathy (Sprue,
Crohn’s)
Causes of Low Serum Albumin with High/Normal Total
Protein• Multiple myeloma• Autoimmune hepatitis• HIV• Etoh hepatitis• Primary biliary cirrhosis
Elevated Indirect Serum Bilirubin
• Normal level < 1
• Gilbert’s/Crigler-Najjar• Blood Loss/Hemolysis• Liver Disease (hepatitis, cirrhosis)• Hepatic congestion secondary to CHF
Elevated Direct Bilirubin
• Normal level < 2
• Dubin-Johnson Syndrome• Hodgkin’s lymphoma• Biliary obstruction• Hepatocellular disease

13
Elevated Serum Ferritin
• Hemochromatosis• Hepatocellular necrosis• Hodgkin’s disease• Leukemia• Hyperthyroid• Uremia• NASH
Elevated Lactate Dehydrogenase(Normal 50-150)
• MI• Pneumocystis Pneumonia• Hemolytic Anemia• Pancreatitis• Mononucleosis
• LDH 1-2 = Cardiac, RBC• LDH 3 = Pulmonary• LDH 4-5 = Muscle, Liver
• LDH 1 > 2 = MI or hemolytic anemia• LDH 5 > 4 = Liver disease (cirrhosis,
hepatitis, hepatic congestion)
Evaluation of Chronic MILD Elevation of Aminotransferases
• Review possible link to medications, herbal therapies or recreational drugs
• Screen for alcohol abuse (screening instruments, AST/ALT ratio >2:1)
• Obtain serology for hepatitis B and C (HBsAg, HBsAb, HBcAb, HCV Ab)
• Screen for hemochromatosis (FE/TIBC >45 percent)
• Evaluate for fatty liver (AST/ALT usually < 1, obtain a RUQ ultrasound)
• Exclude muscle disorders (obtain creatinine kinase or aldolase)
• Obtain thyroid function tests (TSH if hypothyroidism is suspected otherwise obtain a full set of thyroid function tests)
• Consider celiac disease (especially in patients with a history of diarrhea or unexplained iron deficiency - serum anti endomysial IgA or anti tissue transglutaminase IgA antibodies are reasonable screening tests)
• Consider adrenal insufficiency

14
• Consider autoimmune hepatitis particularly in women and those with a history of other autoimmune disorders (check serum protein electrophoresis, obtain ANA and ASMA if positive)
• Consider Wilson's disease in those <40 (check ceruloplasmin, evaluate for Kayser Fletcher rings)
• Consider alpha-1-antitrypsin deficiency especially in patients with a history of emphysema out of proportion to their age or smoking history (obtain alpha-1-antitrypsin phenotype)
References
• Pratt, DS, Kaplan, MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med 2000; 342:1266.
• Polson J, Lee WM. AASLD position paper: the management of acute liver failure. Hepatology 2005 May; 41 (5): 1179-97.
• American Gastoenterological Association medical position statement: evaluation of liver chemistry tests. Gastroenterology 2002 Oct;123(4):1364-6.
• Chopra S, Griffin PH: Laboratory tests and diagnostic procedures in evaluation of liver disease. Am J Med 1985;79:221-230.
• Seth SG, Gordon FD, Chopra S. Nonalcoholic steatohepatitis. Ann Intern Med 1997; 126: 137-145.• Pratt DS. Approach to the patient with abnormal liver function tests. UpToDate 2005; volume 11.2.