Laparoscopic Sacral Colpopexy - Hysteropexy.com Lap Sacral Colpopexy Surg Tech... · If cystotomy...
Transcript of Laparoscopic Sacral Colpopexy - Hysteropexy.com Lap Sacral Colpopexy Surg Tech... · If cystotomy...
GynecologySURGICAL TECHNOLOGY INTERNATIONAL XVII
Laparoscopic Sacral ColpopexyROBERT D. MOORE, D.O.
CO-DIRECTOR OF UROGYNECOLOGY & RECONSTRUCTIVE PELVIC SURGERY
ATLANTA CENTER FOR LAPAROSCOPIC UROGYNECOLOGY
ATLANTA UROGYNECOLOGY ASSOCIATES
ATLANTA, GA
JOHN R. MIKLOS, M.D.
CO-DIRECTOR OF UROGYNECOLOGY & RECONSTRUCTIVE PELVIC SURGERY
ATLANTA CENTER FOR LAPAROSCOPIC UROGYNECOLOGY
ATLANTA UROGYNECOLOGY ASSOCIATES
ATLANTA, GA
ABSTRACT
Sacral colpopexy is the gold standard for vaginal vault suspension throughout the literature. The opera-
tion is considered to be invasive yet very effective. The laparoscopic approach to the sacral colpopexy is
not only effective but can have minimal morbidity in the correct surgeon's hands. The authors have per-
formed more than 500 sacral colpopexy via laparoscopy with minimal morbidity and thus share their tech-
nique with the reader.
- 195 -
Laparoscopic Sacral Colpopexy
MOORE, MIKLOS
Figure 1. Vaginal vault prolapse.
if bowel injury occurs. Two days priorto surgery, the patient is placed on a fullliquid diet (shakes, pudding, and so on),and the day prior to surgery only clearliquids are allowed. The afternoon priorto surgery, the patient drinks 8 oz ofmagnesium citrate to clean out thebowels. We also do not recommend theuse of nitrous oxide for an anesthetic
agent during laparoscopy because thiscan cause bowel distention during theprocedure and increase the risk ofbowel injury.
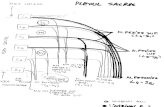
Port placement is based on the surgeon's preference, skill, and acquiredtechnique. We use a 10-mm suturingport in the left paramedian region, andtwo 5-mm ports, one in the suprapubicregion and the other in the right paramedian region (Fig. 2). The surgeonstands on the patient's left side andcompletes all needle passing, suturing,needle retrieving, and knot tying bythemselves using the left paramedianand suprapubic port. The assistantstands on the patient's right side anddrives the camera, using the right lowerport for retraction, suction /irrigation,and so on. Once the operative portshave been placed, the vagina is elevatedwith an EEA ™ sizer (Ethicon, NewBrunswick, NJ) and the peritoneumoverlying the vaginal apex is dissectedanteriorly, exposing the apex of thepubocervical fascia (Fig. 3a). If the edgeof the bladder is difficult to identify secondary to scar tissue, the bladder can beretrograde filled through the three-wayFoley catheter with sterile water andthen carefully dissected off the anteriorsegment. We take this dissectionapproximately one third to one half theway down the anterior wall.
Next, we dissect out the spacebetween the rectovaginal fascia and therectum. This dissection opens the rectovaginal space, and the dissection is takendown to within 3 cm of the perinealbody (Fig. 3b). If bleeding is encountered, it can be stopped with bipolarelectrocautery or surgical clips. A separation between the rectovaginal andpubocervical fascia confirms an enterocele at the apex (Fig. 4).7 If a small enterocele is present, it should be repairedin a site-specific fashion by imbricatingthe stretched vaginal epitheliumbetween the apical edges of the pubocervical and rectovaginal fascia.8 A permanent suture can be used in a
continuous purse-string fashion or in aninterrupted fashion. A large enterocele
Superficialcircumflex
iliac artery
Femoral
artery
Superficialepigastric
artery
1
SURGICAL TECHNIQUE
The patient is taken to the operatingroom and is placed in the dorsallithotomy position with adjustable Allen stirrups. A three-way 16-Fr Foley catheteris placed for gravity drainage. Inflatablesequential compression devices areplaced on the patient's lower extremities for deep vein thrombosis (DVT)prophylaxis. A 48-hour bowel preparation is used for all of our laparoscopicpatients. This preparation helps decompress the bowel for better visualizationand helps minimize the risk of infection
•
Rectusmuscle
fA
•External
iliac
artery
Inferior
epigasrticartery
Figure 2. Laparoscopic port placement.
Uterosacral
ligament
Abdominal sacral colpopexy remainsone of the most successful operations forthe treatment of vaginal vault prolapse(Fig. 1) with excellent results on longterm follow-up. 1-3 The laparoscopicapproach is used in an attempt to minimizethe size of the abdominal incision and thus
the patient's morbidity.4--6If the surgeonuses laparoscopy as a means of surgicalaccess and performs the sacral colpopexyin the same manner as in the open abdominal approach, the operative cure rateshould theoretically be equivalent.
INTRODUCTION
- 196 -
(Figs. 5a & 5b) should be resected (Fig.5c) and the cuff re-approximated withabsorbable sutures so the excessive vaginal epithelium is not used as a point ofmesh attachment. Theoretically, suturing the mesh to the enterocele sacinstead of the more supportive pubocervical and rectovaginal fascia may predispose the patient to an increased riskof mesh erosion, suture pullout, or surgical failure.
Attention is then directed to the
sacral promontory and the presacralspace. The peritoneum overlying thesacral promontory is incised longitudinally and this peritoneal incision isextended to the cul-de-sac (Figs. 6a &6b). A laparoscopic dissector is used toexpose the anterior ligament of thesacral promontory through blunt dissection (Fig 6c). The peritoneum on thesidewall is incised and freed up beneaththe ureter so that the mesh can be
retroperitonealized at the end of theoperation. Hemostasis is achieved usingeither coagulation or surgical clips.
A 12 cm X 4 cm polypropylenemesh graft is fashioned into a "Y" shapeso there is an anterior and posterior leafof the mesh. Typically, the anterior leafis approximately 3 cm to 4 cm long andthe posterior leaf is longer at 5 cm to 6cm so that it can be brought downdeeper into the rectovaginal space. Themesh is then introduced into the
abdominal cavity through a 10-cm or12-cm port. The posterior leaf issutured back to the tail of the mesh to
keep it out of the way, and the anteriorleaf is sutured in place first. The vaginalapex is then directed anterior andcephalad, exposing the pubocervical fascia for application of the surgical graft.The anterior leaf of the mesh is then
sutured to the pubocervical fascia withthree pairs of 2-0 nonabsorbable suturesbeginning distally and working towardthe rectovaginal fascia apex (Fig. 7). Weuse nonabsorbable sutures and tie extra
corporally with a closed-loop knotpusher, which is time-saving and efficient.
The first suture is placed through themesh and then through the pubocervicalfascia, being careful to avoid the bladderedge. Once the anterior leaf is suturedin place, the posterior leaf is thenreleased and sutured in place in a similar fashion. The most distal suture is
typically placed through the vagina first(being careful to avoid the rectum),then brought through the mesh, and
GynecologySURGICAL TECHNOLOGY INTERNATIONAL XVII
~!
Figure 3. lal Exposing the pubocervical fascia at the vaginal apex. (bl Exposing the rectovaginal septum atthe vaginal apex.
Peritoneum
Figure 4. Enterocele· peritoneum in direct contact of vaginal epithelium with no intervening fascia.
- 197 -
Laparoscopic Sacral ColpopexyMOORE, MIKLOS
Figure 5. (a). Large enterocele. (b) Large enterocele. Ie) Dissecting and removing the large enterocele sac.
then tied down into position. Theremaining sutures are taken through themesh and the vagina, typically all atonce, and a total of six to eight suturesare used to suture the posterior leafinto place (Fig. 8). The surgeon shouldattempt to take stitches through theentire thickness of the vaginal wall,excluding the vaginal epithelium.
If a hysterectomy is completed at thetime of the surgery, the cuff is reapproximated in the normal fashion priorto mesh placement and the procedure isthen completed in the identical fashionas described previously. Some have suggested the use of a double-layer closureof the vaginal cuff to help decrease therate of mesh erosion, but we do not
routinely do this and have seen noincreased rate of cuff erosion.9 Howev
er, we do feel it is very important tokeep the sutures that are being placed tohold the mesh in place away from thevaginal cuff, as suturing the mesh rightinto the cufTcan lead to an extrusion inthe suture line.
The vagina is then elevated into itsnormal natural position in the pelvis, andthe surgeon sutures the free end of the Yshaped mesh to the anterior longitudinalligament of the sacrum using two No. 0nonabsorbable sutures (Fig. 9). Themesh should be attached with minimal
tension on the vagina (Figs. lOa & lOb).After reducing intra-abdominal pressureand inspecting the presacral space forhemostasis, the peritoneum is reapproximated with 2-0 polyglactin sutures (Fig.11). The most important aspect ofretroperitonealizing the mesh is not necessarily to cover over all the mesh but isto eliminate the open space between themesh and the right pelvic side wallwhere the bowel could potentiallybecome entrapped and obstructed orischemic. Once the repair is completed,cystoscopy is completed to ensureureteral patency and to ensure that thereis no suture penetration into the bladderor damage to the bladder from dissectionor suture placement.
Lower Urinary Tract InjuriesPotential injuries can occur to the
ureters or to the bladder during therepair. The ureters should be identifiedat the beginning of the operation.Clearly, the right ureter is at more risk
Enterocelesac
Pubocervical
faSCI\,
Vaginalmucosa
Peritoneum
Pubocervica
fascia
- 198 -
GynecoloBYSURGICAL TECHNOLOGY INTERNATIONAL XVII
Figure 7. Suturing the mesh to the anterior vaginal pubocervical fascia.
Figure 6. (al. Incisions of peritoneum over sacral promontory. (bl Incisions of peritoneum over sacralpromontory. (cl Exposingthe anterior ligament of the sacrum.
Peritoneumelevated and/ incised
,./I
-
Cut edge ofperitoneum
! //7./
b
Anterior sacral
ligament
'Aortic bifurcation
c
a
Bladder
Middle sacralvessels
Posterior leafmesh
of injury, secondary to the placement ofthe mesh on the sacrum on' the rightside of the colon. The right ureter isidentified at the pelvic brim prior todissection down into the presacralspace. As this space is opened and theincision is extended down into the
pelvis on the right side wall, the uretershould be clearly visualized throughoutthe dissection and is actually releasedaway from the operative field with thedissection. The ureters could also
potentially be compromised duringsuture placement of the mesh arms ontothe anterior and posterior vagina,specifically the most distal lateralsutures on the anterior wall near the
edge of the bladder where the uretersare entering into the bladder (a gooddissection will help avoid this dangerarea) and the lateral sutures of the posterior leaf near the uterosacral ligaments .
Cystoscopy is performed at the endof the procedure to ensure ureteralpatency. If ureteral obstruction is identified, the suture causing this must beidentified and removed and ureteral
patency confirmed. If any evidence ofcompromise or injury is identified tothe ureter, a ureteral stent should beplaced and left in place for 14 days to 21days. If a suture is seen penetrating thebladder, it must be removed (laparoscopically) and replaced away from thebladder and no further treatment is nec
essary. If cystotomy occurs during theoriginal dissection of the bladder off ofthe vagina, this should be repairedlaparoscopically with a double-layer closure with delayed absorbable sutures.The procedure can still be completedand mesh placed, but care should betaken to try to keep the mesh away fromthe suture line in the bladder. The bladder should be drained for an extended
period of time with this type of aninjury (7 days to 10 days) to ensureproper drainage and healing. Overall,the risk of lower urinary tract injury islower with sacral colpopexy than withother vault suspensions, such asuterosacral ligament suspension.
Bowel InjuryThe bowel can be injured with the
lysis of adhesions or with the dissectionof the rectum off of the posterior wallof the vagina. A proper 48-hour bowelpreparation described previously is vitalto help decrease the risk of bowelinjury, as this actually deflates the small
- 199 -
Laparoscopic Sacral Colpopexy
MOORE, MIKLOS
Attachment of
posterior leaf mesh
Figure 8. Suturing the mesh to the posterior vaginal rectovaginal fascia.
Figure 9. Suturing the mesh to the anterior ligament of the sacrum.
Bladder
Anterior leamesh
Graft attachmentto anterior
sacral ligament
- 200 -
and large bowel and makes it much easier to get the bowel out of the pelvis andhave it stay in the upper abdomen andout of the surgical field. Additionally,the use of nitrous oxide should be
avoided as well as an anesthetic agent,as this will cause the bowel to become
distended and inflated, increasing therisk of injury. If a small bowel injuryoccurs, primary repair laparoscopicallyis recommended and if a proper bowelpreparation was completed, the meshsacral colpopexy can be completed.However, antibiotic coverage should becompleted for 1 week postoperatively.If the rectum or large bowel is injuredduring the dissection into the rectovaginal space, primary repair can be completed if proper bowel preparation wascompleted. However, the mesh is notrecommended to be placed following alarge bowel injury. Certainly, antibioticcoverage is warranted postoperatively aswell.
Vascular InjuriesAs with any advanced pelvic surgical
procedure, a thorough knowledge ofthe pelvic anatomy and vasculature isrequired prior to attempting laparoscopic sacral colpopexy. The overall riskfor bleeding is actually quite low; however, if it does occur it can be a lifethreatening event. Our average bloodloss in over 500 cases over the past 4years has been less than 75 cc, and wehave not had to give any blood transfusions for intra-operative bleeding andonly one blood transfusion postoperatively. The average blood loss forlaparoscopic reconstruction is actuallymuch less than with laparotomy secondary to more precise dissection andbetter visualization with laparoscopy,with the benefit of also eliminating thebleeding encountered with a largeabdominal wall incision. There is actu
ally minimal risk of bleeding or majorvasculature injury with the dissection ofthe vaginal cuff. This area can be quitevascular, especially down in the rectovaginal space, but it is typically venousin nature and can be easily controlledwith cautery or surgical clips.
One should always identify andknow the location of the ureters priorto any cauterization or clipping. However, dissection into the presacral spacehas the potential for catastrophic bleeding. The patient is placed in deep Trendelenburg positioning with a left tilt sothe bowel may be placed in the upper
Gynecolo8YSURGICAL TECHNOLOGY INTERNATIONAL XVII
a Inferior mesenteric artery b
Figure 10. lal Minimal tension is used when attaching the mesh to the sacrum. (bl Minimal tension is used when attaching the mesh to the sacrum.
Figure 11. Reapproximating the peritoneum over the sacral colpopexy mesh.
- 201 -
abdomen and the rectum will fall off to
the patient's left side. The right common iliac artery and vein are identified,as is the ureter. The peritoneum is tented using fine graspers and the peritoneum incised over the sacral
promontory. The presacral space iscarefully dissected until the presacralligament is reached, and this area iscarefully cleaned with a laparoscopicKittner dissector until the white of the
ligament is seen. The middle sacralartery is identified and the surgeon isensured of finding a vessel-free area tosuture or attach the mesh. One must becareful, as on occasion the left commoniliac vein can traverse this area as well.
If bleeding is encountered during thedissection or down in the sacral hollow,it can be life-threatening and rapid conversion to laparotomy should be considered and prepared. Bipolarelectrocautery, surgical clips, or hemostatic sutures may be used laparoscopically to try to control the bleeding, butagain the position of the ureter must beidentified to ensure it is away from thesurgical field. Thrombin gel agent maybe used laparoscopically and can behelpful in controlling both arterial andvenous bleeding. We have utilized this
Laparoscopic Sacral Colpopexy
MOORE, MIKLOS
material in several incidences and havehad excellent clinical results, and todate have not had to convert any patientto laparotomy.
If bleeding cannot be controlled, aconversion to laparotomy is requiredand packing/pressure should be placedimmediately to control bleeding,restore volume, and the patient givenblood products if necessary. Thumbtacks with bone wax have been used in
the sacral hollow to control bleedingvessels that have retracted into the
sacrum, and again hemostatic agentssuch as thrombin gel may be used tohelp obtain hemostasis as well.
CONCLUSION
Laparoscopy should only be considered a mode of surgical access, whichshould not significantly change the technique of operative reconstructivesurgery. Laparoscopy benefits the surgeon by improving visualization,decreasing blood loss, and magnifying
the pelvic floor defects that must berepaired. Other advantages - including less postoperative pain, shorter hospital stays, shorter recovery time, andearlier return to a better quality of life- have also been described in the liter
ature to date. Disadvantages often citedin the literature include increased operative time and associated increased
costs. The authors' personal experienceis the operative time is similar and inmany cases reduced, especially forpatients with a high body mass index.However, complex operativelaparoscopy is associated with a steepand lengthy learning curve, after whichoperative time can be significantlyreduced based on the surgeon's experience and laparoscopy skills as well asthe quality of the operative team. WI
REFERENCES
1. Maher C, Baessler K, Glazener C, et al.Surgical management of pelvic organ prolapseis women. Cochrane Database Syst Rev 2007JulyI8;(3): CD004014.
- 202 -
2. Higgs P, Goh J, Krause H, et al. Abdominal sacral colpopexy an independent prospective long-term follow-up study. Aus NZ JObstet Gyenaecol 2005 Oct;45(5):430--4.3. Limb J, Wood K, Weinberger M, et al.Sacral colpopexy using mersilene mesh inthe treatment of vaginal vault prolapse.World JUral 2005 Feb;23(1)55-60. Epub, 11 Nov 2004.4. Rozet F, Mandr'on E, Arroyo C, et al.Laparoscopic sacral colpopexy approach forgenito-urinary prolapse: experience with 363cases. Eur Ural 2005 Feb;47(2):230~6.5. Casson M, Rajabally R, Bogaert E, et al.Laparoscopic sacrocolpopexy, hysterectomyand burch colposuspension: feasibility andshort-term complications of 77 procedures. JSac Lap Surg 2002;6(2):115-9.6. Wattiez A, Canis M, Mage G, et al.Promontofixation for the treatment of prolapse. Ural Clin N Amer 2001 ;28: 151~7.7. Richardson AC. The anatomic defects inrectocele and enterocele. J Pelvic Surg1995;1:214---21.8. Miklos JR, Kohli N, Lucente V, Saye WB.Site-specific fascial defects in the diagnosis andsurgical management of enterocele. Am JObstet GynecoI1998;179:1418~23.9. Brizzolara S, Pillai-Allen A. Risk of Mesherosion with sacral colpopexy and concurrenthysterecomty. Obst5t Gynecol 2003; 102(2):306-10.