2016 Arizona Institute on Leadership and Politics Orientation Guide
IRONMAN ARIZONA MEDICAL ORIENTATION 2013
-
Upload
dr-david-carfagno -
Category
Health & Medicine
-
view
539 -
download
0
Transcript of IRONMAN ARIZONA MEDICAL ORIENTATION 2013

David Carfagno D.O., C.A.Q.
Scottsdale Sports Medicine Institute
Mass Sporting Event : Sports Medicine

OUTLINE
1. PREPARATION OF THE EVENT2. Swim3. Bike4. Run

PREPARATION1. Course set up2. Resources3. Staff4. Yourself

Medical Tents
Swim South Side Main Medical North Side Warming
Transition Men’s and Women’s Change Tent
Main Medical Finish 72 bed MASH unit Teams comprised of 3-4 staff per 6 bed
section Evaluation/oral suport/IV
support/Meds/Istat 2 ALS ambulances and PM staff

Medical Tent The Medical tent serves a
large role in the Ironman and thus organization of the medical team is important and takes shape nearly 5 months before each race every year.
The Medical team is comprised of doctors, nurses, paramedics, EMT’s, medical students, athletic trainers, and other personnel such as IV technicians and communications, security, and supply volunteers.

Personnel
Catchers are placed at the finish line. They are educated on cooling down the athlete and escorting those that need medical care.
At the beginning of the tent, we have a computer check-in. Personnel will take the athlete’s chip and the athlete is checked in.

SHIFTS Swim Medical 5:30-9:00 am South Main Tent (Swim Exit) Hasan Chaudry MD/Gina Ferguson RN Joe Garcia MD/Susan Girard RN Alex Espinoza MD/Kelley Deeny RN/Terra Marr RN Lainie Yarris MD/Sue White RN/Brad Williams PM Jeff Jaco PA/Michelle Nelson RN/Mary Ellen Quinn NPEMT
Finish/Catching Rodney Schnuelle EMT/Katie Sidesinger RN/Milica Mcdowell DPT/Conrad Hilton/Scott Simpson
North Medical Tent Michelle Miller RN/Billy Burnett EMT/Brian Byars EMT Main Medical Setup 8:00-10:00 am
Nicole Barreda ND/Maria Santander MD Al Valle CPU/Craig Wolchover CPU/Alex Zdvorak CPU
Transition Medical 8:00-10:00 am Brian Crowder RN/Jocelyn Mayes RN Robyn Crowder/Paul Herberger
Transition Medical 12:00-5:30 pm Men’s Tent: Savas Petrides MD (Sarah Petrides)/Bob Nelson MD Ignacio Marquez EMT/Kenneth Zurcher/Michael Bishop PM Women’s Test: Bridget Haga RN/Katie Hoodjer RN Jim West PM/Sarah West RN/Lisa Sherry-Kulow RN/Sana Shuttari NP/Angela Tetschner RN/Lori Vega RN

SHIFTS Main Medical 12:00-3:00 pm CPU: Jordan Ahern/Kali Bayes A: Liz Dinsmoor RN/Mark Ford EMT B: Ann Kelly RN/Judy Lynn PM/Deborah Ackerman RN C: Tanya Marvin PA/Clare Ryan RN NP
Main Medical 3:00-6:00 pm CPU: Jordan Ahern/Mikayla Jaraczewski/Jennifer Light A: Liz Dinsmoor RN/Carly Fellhoelter CAN B: Lyle Edwards PM/Praise Gunadi RN C: Terra Marr RN/Jennifer Quint RN D: Robert Ziltzer MD/Amy Turano RN/Rachel Dickman EMT
Run Medical 3:00-6:00 pm Steven Cho/Jason Lee Dina Utter RN/Praise Gunadi RN

SHIFTS Main Medical 6:00-9:00 pm CPU: Jordan Ahern/Darrin Anderson/Joseph Baxter/Samantha Calvin/Bonnie and Danny Kissinger/Sue Pierson/Annette Paris A: Ryan Coates DO/Dan Leon PM/Roger Chopelas RN/Andrew Bliss EMT B Dennis Scribner MD/Lisa Banyasz RN/Richard Alamo PM C: Benjamin Johansen DO/Cliff Bailey RN/Rodney Schnuelle EMT E: Amish Shah MD/Tara Peters RN/Dane Morrissey PM/Mark Thornberry PM F: Mikyong Hand MD/Kimberli Haas RN//Tommy Roads/Kimberly Hansen ATC G: Donn Hogan MD/Rachael Roberts RN/Desiree Hart-Wilson RN/Pamela Pimentel RN H: Andrew Utter MD/ /Anna Lipa RN/Loren Swensen EMT I: Lyle Edwards PM/Neil Martin PM/Kathy Brown RN/David Jordan PM
Walking Wounded: Jay Mellen MD/Brian Moore MD/Carol Holliday RN/ Terra Marr RN/Charles Brown PM/Jennifer Sheneman RN Donovan Adendorf DC/Megan Cook/Jackie English/Carly Fellhoelter Crna/Cyntia Hurtado/Mikayla Jaraczewski/Bret Jones/Neal
Mckimpson/Leonor Medina/Anna Pastorino/Scott Simpson/Conrad Hilton/Josh Hendrix Catcher Assist: Ted McCarthy MD/Mike Pierson MD/Marita Mcgoldrick NP/Eric Loiland PT/Sarah Kellerhals/Yoonha Kim/ Matthew
Petterson/Sarah Rubenstein/Amber Sandoval-Menendez Run Medical 6:00-9:00 pm Patrick Weldon MD/Gary Young RN/Jude Carza RN/Raiza Carza RN Charting: Gregg Bassett/Sam Fleischer Assist: Joanne Donnelly Crna/James Fernandes PTATC/Jose Fonseca PT
Main Medical 9:00-12:30 am CPU: Jordan Ahern/Cassie Beard/Tamara Brown/Michelle Drietz A: Mike Brown DO/Lisa Austin RN/Brad Eppelheimer ATC B: Matthew Duke DO/Zelda Carson RN/Brianna Foote RN C: Savas Petrides MD (Sarah Petrides)/Carly Fellhoelter crna/Nathan Hill EMT D: Richard Ernst MD/Yiselle Gonzalez RN/Chris Murray PM E: Dana Jamison MD/Melissa Kay ATC F: Amish Shah MD/Terra Marr RN
Walking Wounded: Dennis Scribner MD/ Maya Davidow MD/Peggy Thornhill RN Tracy Lee/Chung-Kai Liu/ Catcher Assist: Ted McCarthy MD/ Kelsey Picha ATC/Sharon Plummer ND
Run Medical 9:00-12:30 am Amy Wiser MD/Vicky Tippett MD/Kortney Parman RN Evan Wolff/Russell McWilliam/Tina Rossi/Gillian Hansen

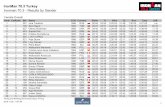
0
50
100
150
200
250
300
350
400
450
# of Athletes
Until 5pm 5pm-6pm 6pm-7pm 7pm-8pm 8pm-9pm 9pm-10pm 10pm-11pm 11pm+Time of Day
Ironman Average Finish Time
Run:

SWIM 1. Drowning / Near-drowning Swim-Induced Pulmonary Edema (SIPE) Asthma Hypothermia / Hyperthermia Swim Combat / Exit Trauma Anxiety Corneal Abrasion

S.I.P.E.
Swimming Induced Pulmonary Edema
Secondary Causes
•Wetsuit compression, compression calf/arm•Pre Race hydration•Stimulants•Cold Water-Dive Reflex

Hypothermia
• Compensatory Mechanisms:– Shivering (which occurs from 37 to 32 degrees)– Autonomic Nervous system (occurring from 37
to 32 degrees, includes bradycardia and vasoconstriction)
– Extrapyramidal stimulation of skeletal muscles– Adaptive Behavioral responses

HYPOTHERMIA
TREATMENT• Treatment: Focus on diminishing heat loss
• Use of heating devices. This includes
heaters within the tents , warm baths • Removal of wet clothes. Wet clothing
leads to heat dissipation five times• Cover and keep patient insulated.
Aluminum foil blankets efficient than wool blankets
• Warm IV Fluids • Serious hypothermia , follow Marine
Corps Marathon Hypothermia algorithm

BIKE
Head Injury Fractures Road Rash Repetitive Motion Medical Issues

RUN
Cardiac Arrest, Heat Stroke, and Exercise-Associated Hyponatremia.
Initial Approach to the unresponsive athlete: Initial Evaluation (VS) / C-A-B Elevate the legs Assess Mental Status Assess Volume Status Fluid Replacement Continuous Monitoring

Steps to Approach the Collapsed Athlete Initial Evaluation/ C-A-B
Compressions-Airway-Breathing (check back of bib for Medical Information)
Elevate the Legs This will help any conscious athletes that are light-headed
Assess Mental Status AMS often presents with Heat Stroke and Exercise-Associated
Hyponatremia Assess Volume Status
Fluids consumed, vomit/diarrhea, urinated during race, orthostatic pulse
Fluid Replacement Fluids w/electrolytes such as Sports Drink or Chicken broth An IV may be started based on clinical judgment
Continuous Monitoring Any athlete needing to go to the hospital MUST be seen by the
Medical Director

1. Exercise Associated Collapse (EAC) Heat Exhaustion- more common in warmer environments During race blood vessels maximally dilated in legs for
cooling and delivery of O2 to working muscles Adrenaline released to regulate BP and maintain cardiac
output When athlete stops pump action is lost and adrenaline no
longer released Vessels remain dilated leading to pooling of blood in lower
extremity
TREATMENT Have athlete continue “cool down” walk after race Lie the athlete down and elevate the legs If no nausea present offer PO fluids or possible IV

2. Volume Depletion
During exercise runners often sweat >1.5 L/Hr while maximally absorbing approximately 1 L (negative fluid balance)
With as little as 3% loss of body weight a marathon runner performance is impaired
Volume depletion leads to hyperthermia due to the limiting of blood shunted to the skin
Runners present: Hypotension, tachycardia, weight loss, decreased skin turgor,
hypernatremia
TREATMENT Oral fluids such as sports drink or chicken broth IV NS, first w/500 ml bolus, then 500 ml over 30-60 min Any sign of AMS must have electrolytes drawn

3. Exercise-Associated Hyponatremia Most common mechanism due to over-hydration Trained athletes should have calculated fluid loss during
exercise Risk factors for developing EAH
Finish under 4 hrs, inexperience, small stature, female gender Hallmark for EAH: AMS or unusual neurologic complaint
Recognizing Hyponatremia Stage 1: dizziness, nausea, vomiting, headache (Na+ 130-135
mEq/L) Stage 2: mental status changes (confusion, disorientation) (Na+ 125-130
mEq/L) Stage 3: altered consciousness (delirium, seizures, coma) (Na+ <125
mEq/L)

On Course Management EAH Stage 1
If vitals stable, fluid restriction (4oz max) and observe until urination Fluid replacement: add 3 salt packs (3/8 tsp) to half cup electrolyte
drink, this will provide 1 g Na or a 3%saline solution Should athlete continue fluid restriction of 4oz max/ mile adding salt
as above
Stage 2/Stage 3 Consider transferring to ER Give 3% oral saline solution, if can tolerate PO fluids Transport via EMT/Paramedics, advise NO IV fluids until hyponatremia
excluded ALL runners w/EAH must receive discharge from Medical director

Medical Tent Management EAH Stage 1
Draw blood for Na+ concentration and give no IV fluids Limit fluid to 4oz (preferably broth) or 3% saline or salty snacks
Stage 2 Draw blood for Na+ concentration, if >125 mEq/L offer PO broth Oral hypertonic saline: 4 cubes of bouillon in 4oz hot water for a 9%
solution Limit fluid to 4oz, continue observation until they urinate If not improved 15-20 min repeat oral solution or give 100 ml bolus
3%NaCl Begin cardiac monitoring and pulse oximetry A 2nd IV bolus given 10-15 min later Any signs of neuro must go to ER, transport on IV=3%NaCl at 1 ml/min
Stage 3 Draw blood for Na+ concentration, if <125 or delirium present must go to
ER Begin cardiac monitoring and pulse oximetry Give 100 ml bolus 3% NaCl and a 2nd in 10-15 min Both Valium and Ativan for IV injection are available to treat seizures

4. Heat Stroke With a core temp >104°F organ/brain cells begin to die Goal is Rapid cooling to < 104°F within 30 min Athlete presents w/CNS changes, altered
cognition/behavior If oral reading >100.5°F, then rectal temp should be taken
Early Warning signs Irritability, confusion, apathy, belligerence, emotional instability,
irrational behavior, giddiness , vomiting, numbness ,tingling, collapse, seizures, coma
Paradoxical chills and goose bumps signal shutdown of peripheral circulation
Follow Mantra: “cool first, transport second”

“Cool First, Transport Second” Cool First
Rapid cooling by placing athlete into ice-water submersion tub (immerse trunk, both arms and both legs) has 100% survival rate when athlete immersed within 10 min of collapse (key to maximal cooling is constant stirring of the ice)
May also cold water douse the body while patient lying on porous stretcher, while massaging major muscle groups w/ice bags
May also place wet ice towels over entire body, rotate w/cooler towels every 2 min
Check rectal temp/vitals/CNS status every few min At athlete can be cooled from 108-110°F to 102°F within 15-30 min,
average rate of cooling drop is 1°F every 3 min Transport Second
Once temp reaches 102°F, remove from immersion tub Observe for 30-60 min to ensure drinking fluids, normal vitals, good
cognition Physicians recommended to follow up and evaluate patients w/sever
hyperthermia If rectal cannot be measured, cold water immersion for 10-15 min then
transport to ER

7. Cardiac Arrest Usually occurs near the finish, theory is increased
adrenaline release precipitates arrhythmia, when runner sees finish line and sprints to improve position
Any athlete w/Cardiac arrest should prompt notification Medical Command and activate 911 system and initiate ambulance
TREATMENT Good quality chest compressions Early defibrillation when AED available Follow the Marine Corps Marathon algorithm for Emergency Cardiac
Care

Cardiac Arrest during Long-Distance Running RacesJonathan H. Kim, M.D. for the Race Associated Cardiac Arrest Event Registry
(RACER) Study GroupN Engl J Med 2012; 366:130-140January 12, 2012DOI: 10.1056
1. 10.9 million runners, 59 (mean [±SD] age, 42±13 years; 51 men) had cardiac arrest 0.54 per 100,000 participants; interval and among (men 0.90 per 100,000, women 0.16).
2. Cardiovascular disease accounted for the majority of cardiac arrests. The incidence rate was significantly higher during marathons (1.01 per 100,000) than during half-marathons
3. Of the 59 cases of cardiac arrest, 42 (71%) were fatal (incidence, 0.39 per 100,000).
4. Among the 31 cases with complete clinical data, initiation of bystander-administered cardiopulmonary resuscitation and an underlying diagnosis other than hypertrophic cardiomyopathy were the strongest predictors of survival.

5. Exertional Rhabdomyolysis Most important factor pre-disposing to this condition is
hypovolemia Damage to skeletal muscle and release CK-MM, myoglobin
and aldolase into circulation High levels of myoglobin can cause acute renal failure,
DIC, lactic acidosis and cardiac dysrhythmias Symptoms
myalgias, muscular swelling, tenderness, dark colored urine, lower back or abdominal pain
Risk Factors Poor fitness level, high temp/humidity, sickle cell trait, viral illness, hx
of myopathies, prior renal insufficiency
TREATMENT Fluid replacement, maintain good urine output, transport to Hospital

6. Hypoglycemia Check athlete for Hx of Diabetes
Exercise acts like regular insulin and this must be calculated
In non-diabetics may occur due to complete depletion of glycogen stores
Symptoms Fatigue, dizziness, tachycardia, nausea, vomiting, impaired mental status *Any of these symptoms a “finger stick” glucose should be checked
TREATMENT (if glucose <55) PO glucose if no nausea or vomiting Bolus of D50 IV ER transport for those who fail to respond or remain hypoglycemic

8. GUT Science Exercise=Sympathetic Nervous System Digestion= Parasympathetic Nervous System Athletes must train their guts to digest on the run Under ideal conditions the gut can process 1.5 L/hr
Many novice runners will over-feed or over-hydrate, and gut cannot handle this volume leading to nausea/vomit
Symptoms Diarrhea (possible osmotic diarrhea), nausea, vomit, abdominal pain *Be cautious w/abdominal pain, during exercise 70% of splanchnic
circulation is shunted to working muscles, this can result in ischemia and eventually necrosis of intestinal lining cells

9. Respiratory Problems 15% of general population and 40% athletes w/allergies
will develop Exercise-Induced bronchospasm If patient has true asthma, number rises to over 70%
Common on days w/ increased pollutants such as smoke, dust, pollen
TREATMENT Replacing volume, administer breathing treatments w/inhaled
bronchodilators Albuterol is effective as rescue inhaler

10. Muscle Cramps
Treatment is two fold: addressing metabolic issues and mechanical stretching of injured muscle
First begin IV and check serum sodium and magnesium
TREATMENT EAH? Draw iSTAT 2-4 g Magnesium sulfate give slow IV push while watching reflexes
and respirations Ativan 0.5 mg IM or IV 2-4 g Magnesium sulfate can be added to 1 L IV NS and run at 500-
1,000 ml/hr Sickle cell trait can produce muscle ischemia and should be treated
w/O2 and IV fluids, transport to ER Use of the Massage therapist may be helpful

12. Skin Care Remember sunburned skin does not sweat well, SPF >30 should be
used Avoid waterproof products which block pores and reduce sweating
Abrasions should be cleaned w/Hydrogen peroxide or Hibiclens Betadyne retards wound healing
Small, intact blisters that are minimally painful usually don’t need any treatment. Cover it with a small bandaid, and triple antibiotic ointment.
Larger or painful blisters that are intact should be carefully drained, without removing the skin. clean the skin over the blister with rubbing alcohol or soap and water. sterilized needle or pin, puncture a small hole at the edge of the blister. Drain the fluid with gentle pressure and apply a bandaid with some triple antibiotic
ointment. Keep it clean and dry for 2-3 days, changing the dressing daily. You may then begin
to carefully trim away the dead skin. Use second skin, or blister pads for protection, until the new skin matures.

Charting TIME IN: ____________ TIME OUT: ___________ Arrived from: Ambulance Massage Finish Line Other
___________________________ Finisher? Yes No DQ? Yes No
CHIEF COMPLAINT Altered Mental Status Seizures
Exhaustion Short of Breath Vomiting Diarrhea ABD Cramps Muscle
Cramps Dizziness Syncope Nausea Headache Trauma Other
_______________ PHYSICAL FINIDINGS Dehydration Hypotension Edema Confusion Hyperthermia Hypothermia Other
_____________________________ DIAGNOSIS Exhaustion Dehydration Trauma
Hyponatremia Hyperthermia Hypothermia Other _____________________________
OUTCOME Resume Race Discharge Transport to Hospital
COMMENTS _____________________________________________________________________________________________________
M.D. ______________________________________________ R.N. ___________________________________________________

DISHCARGE
HOME CARE Stretch tight muscles, and ice sore tendons and
joints. Anti-inflammatory medications, such as ibuprofen or
naproxen may help speed recovery. Eat a light diet with foods that are easy to digest,
such as pasta, rice, or potatoes. Adding some protein actually helps your muscles recovers faster.
Drink plenty of fluids. It is a good idea to salt your food or use a Sports Drink to replace the electrolytes (such as sodium) you have lost. Avoid drinking large quantities of water.

DISCHARGE
SEEK MEDICAL ATTENTION IF YOU EXPERIENCE: Severe leg or calf pain not improved with elevation Abdominal pain with or without vomiting or diarrhea Persistent temperature over 100.50 F (37.80 C) orally Blood in vomit or stool (even dark red or black stool) Unusual weakness, dizziness or fainting Decreased urine output, bloody or very dark urine Unusual chest pain, muscle cramping or edema
[puffiness] Coughing, trouble breathing, colored or bloody phlegm Severe headache, vision changes or confusion